Roux-en-Y-Gastric Bypass Surgery | Procedure & Cost
PACE Hospitals is recognized as the best hospital for gastric bypass surgery in Hyderabad, India, offering advanced bariatric care with a focus on the Roux-en-Y gastric bypass procedure. Our skilled bariatric surgeons provide personalized treatment to manage obesity, metabolic disorders, type 2 diabetes, hypertension, and related complications.
With modern technology and a patient-focused approach, we ensure safe surgery, quicker recovery, and lasting results. We also offer clear guidance on gastric bypass surgery cost, helping patients make informed decisions with confidence.
Book an Appointment for Gastric-Bypass Surgery
Gastric Bypass Surgery Appointment
Why Choose PACE Hospitals for Gastric-Bypass Surgery?
Expert Bariatric Surgeons Delivering Safe & Effective Gastric Bypass Outcomes
Gastric Bypass with Faster Recovery & Sustained Long-Term Weight Loss
Gastric Bypass Surgery with Transparent Costs, Insurance Support & Cashless Options
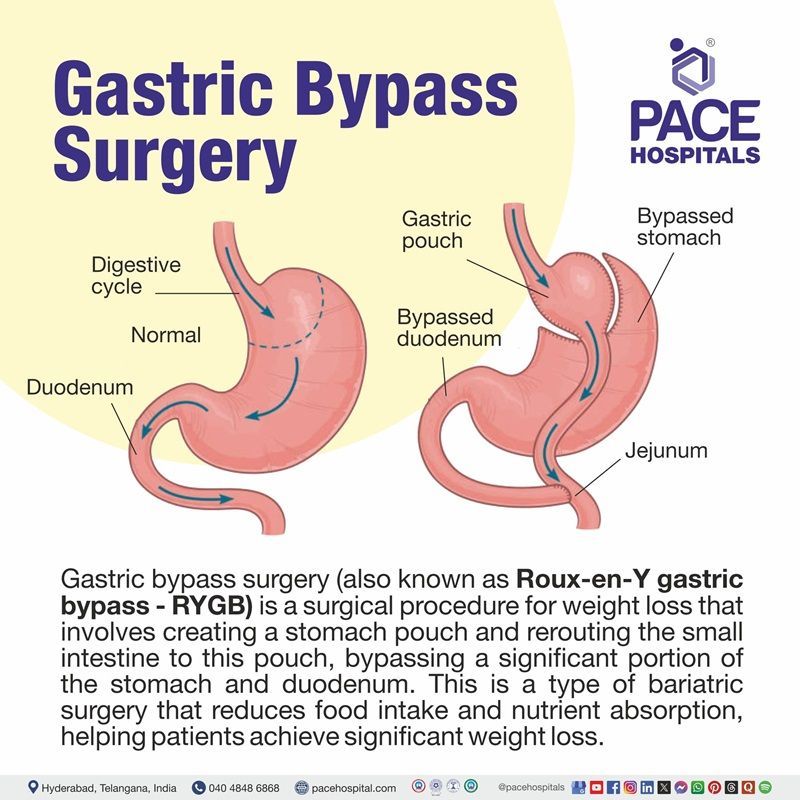
Roux en y gastric bypass definition
The laparoscopic Roux-en-Y gastric bypass surgery (LRYGB) is widely considered as the gold standard in bariatric surgery; achieving superior weight-loss with acceptable complication rates. Bariatric surgery is a surgical procedure which evolved as one of the most effective methods of treatment for morbid obesity. The laparoscopic Roux-en-Y gastric bypass surgery is a type of bariatric surgery.
LRYGB is also a metabolic procedure as it results in significant improvements of diabetes mellitus, hypertension, dyslipidaemia and sleep apnea, along with a subsequent reduction in overall mortality. Though the technique is now well-defined, controversies continue to exist at certain aspects of the configuration.
In the 1960s, gastrointestinal surgeons Mason and Ito first devised this method. The gastric bypass was predicated on the weight reduction observed in ulcer patients who underwent partial stomach resection. Using a Roux-en-Y intestinal limb, the gastric bypass has evolved into its current form over several decades.
Why it is called the Roux-en-Y gastric bypass?
The Roux-en-Y gastric bypass is named after Swiss surgeon César Roux (1857-1934), who served as Chief of Surgery at Lausanne County Hospital and was the first Professor of External Pathology and Gynecology at the new University of Lausanne, which opened in 1890.
How does Roux-en-Y gastric bypass work?
This procedure lowers the size of the upper stomach to a little egg-sized pouch by cutting the top portion of the stomach decreasing the amount of food that can be consumed. This pouch is directly connected to the Roux limb, a portion of the small intestine resulting in a "Y" shape.
The meal subsequently skips the remainder of the stomach and the top portion of the small intestine. This decreases the fat and calorie absorption from the meals consumed. Additionally, it also diminishes the quantity of vitamins and minerals absorbed from diet.
Indication for Roux-en-Y gastric bypass
Understanding of obesity and metabolic–bariatric surgery (MBS) has evolved significantly since the NIH’s original 1991 guidelines, backed by long-term evidence demonstrating safety, efficacy, and durable weight-loss outcomes. Based on the 2022 American Society of Metabolic and Bariatric Surgery (ASMBS) and International Federation for the Surgery of Obesity (IFSO) updated recommendations, the following are the current indications. The indications for MBS include:
- Adults with BMI ≥35 kg/m²
- Adults with BMI ≥30 kg/m² with type 2 diabetes
- Adults with BMI 30–34.9 kg/m² who fail nonsurgical weight-loss therapies
- Consideration of different BMI thresholds across populations (like Asian populations)
- Children and adolescents (with different BMI and major comorbidity)
- No upper age limit based on physical fitness
- High-risk surgical candidates benefit improving metabolic status and reducing long-term systemic risk.
- Patients requiring other specialty surgeries (Joint arthroplasty, Abdominal wall hernia repair)
- Failure of all nonoperative measures in maintaining weight loss for > 6 months.
- Commitment to long term follow up (can be assessed by preoperative weight loss)
Contraindications
Relative contraindications can include patients suffering from various ailments such as:
- Patients with Crohn disease (inflammatory bowel disease affecting the lining of digestive tract) and severe esophagitis are contraindicated as Roux-en-Y bariatric surgery can enhance its development.
- Patients with psychosocial disorders including drug or alcohol use disorders cannot undergo bariatric surgery.
- Patients with significant intellectual impairment are unlikely to be viable candidates because a high level of patient comprehension of the risks and lifestyle consequences of surgery is required.
- Patients with epilepsy should have their medicines reviewed because bypass surgery affects absorption. As a result, preoperatively, thorough decision making with the cooperation of pharmacists and neurologists should be sought.
Absolute contraindications include:
- Pregnancy
- Any terminal renal illness
- Unstable coronary artery disease
- Severe heart failure
- Liver cirrhosis
- Portal hypertension
- Active malignancy
Benefits of gastric bypass
Roux-en-Y gastric bypass is considered one of the most effective and well-studied bariatric procedures. Below given are key benefits:
- Significant long-term weight loss: RYGB leads to substantial and durable weight reduction, often maintained for many years.
- High remission rates for type 2 diabetes: RYGB frequently results in partial or complete remission of type 2 diabetes, often occurring early due to hormonal and metabolic changes.
- Improvement in obesity-related conditions: Conditions such as hypertension, dyslipidemia, obstructive sleep apnea, and fatty liver disease commonly improve after RYGB.
- Lower recurrence of weight regain: Compared to restrictive procedures, RYGB shows better long-term maintenance of weight loss due to its dual restrictive and metabolic mechanisms.
Considerations of the surgeon before the procedure
The surgeons undergo rigorous study and training, honed with years of experience, to pay keen attention even to minute details in the surgical technique of laparoscopic Roux-en-Y procedure as it is fundamental to avoid complications both in the short and long term.
Roux-en-Y procedure has profound effects on dietary and nutritional intake, as it is both malabsorptive (limits food absorption) as well as a restrictive (limits food intake) bariatric surgery which is the reason that it affects the absorption of micronutrients.
There is a serious risk of malnutrition if the patient is unable to comply with the nutritional guidelines, follow-up and aftercare. This is why the doctors always emphasise on explaining the outcomes of the procedure and the eligibility of the patient through the lens of preoperative weight loss.
Patients who underwent Roux-en-Y-gastric-bypass may be at risk of protein malnutrition which again brings the necessity of preprocedural explanation by the healthcare professionals to the patients.
The surgeons take special care in treating patients with pre-existing mental health conditions and their medication, as some medicines may be associated with increased appetite and thirst.
The other patients who need special support are:
- Pregnant and/or nursing women
- Women suffering from menorrhagia (iron deficiency anaemia)
- Patients on proton pump inhibitors
- Patients with B12 deficiency
- Patients who have had duodenal switch surgery
- Patients with co-existing malabsorptive conditions, such as celiac disease, tropical sprue, inflammatory bowel disease (IBD)
- Patients with renal impairment or with a single kidney, kidney stones
- Patients with high cardiovascular risk
Pre-operative Weight loss and its principle
Apart from other evaluatory pathways, pre-operative weight loss has been used as a screening tool for predicting success in surgical candidates. It is accepted that patients who weigh less have decreased risk with surgery and less weight-related comorbidity.
- Thinner patients generally require less rigorous pre-operative clearance than their heavier counterparts due to a lower burden of obesity-related disease.
- It is technically easier to operate on someone thinner due to improved exposure and accessibility.
- Pre-operative programs to decrease BMI would theoretically reduce perioperative and postoperative complications such as bleeding, wound infection, etc.
- In addition, shorter operative times and hospital stays could occur.
- In addition to the hypothetical risk improvement with pre-operative weight loss, many medical providers theorized that patients who demonstrate pre-operative weight loss are more severe and motivated about adhering to postoperative diet and exercise recommendations.
Steps for Pre-Operative Weight Loss
Most pre-operative weight loss programs and appointments include several meetings with nutritionists, physicians, psychiatric assessments and weigh-in calculation.
In these and other meetings, the bond between the patient and healthcare providers strengthens, which is necessary for a low attrition rate during the postoperative phase.
If the patients cannot show adequate weight loss or miss appointments, they may be forced to start over or, in extreme cases, are even refused surgery.
Patient Selection Criteria
Overall, the surgeons opt for Roux-en-Y gastric bypass for patients with the following traits. The counselling and education during the entirety of the pre-operative journey are designed to prepare the patients and cultivate the following traits in them.
- Well-informed, motivated individuals
- Acceptable operative risks
- Able and willing to comply with long-term follow-up
- Psychological stability
- Free from drug and alcohol abuse
- Demonstrated previous weight loss attempts
- A clear and realistic understanding of the lifestyle changes needs lifelong before and after surgery.
Roux-en-Y Gastric Bypass Procedure
The preparation for surgery may start months before the actual procedure. A preoperational weight loss procedure plan is presented to the patients, and is expected to stick with it. Apart from various other advantages, the preoperational weight loss procedure plan provides discipline to the patient, which helps restrict food after surgery.
The doctor explains to the patient that although Roux-en-Y gastric bypass is an effective bariatric surgery, it may not work over the long term if the patient fails to change their habits and lifestyle.
- Once the patients sign the consent form, they will be started on a two-week milk diet for reducing the liver size, resistance and constraints on the movement of laparoscopic instrument.
- The patient may receive venous thromboembolism prophylaxis on the day of the surgery.
- In some vulnerable individuals Thrombo-embolic deterrent (TED) stockings or intermittent pressure calf compression devices are applied.
Pre-operative evaluations
Pre-operative evaluations are necessarily done once the patient demonstrates substantial pre-operative weight loss. These evaluations include:
- Allergy evaluation
- Cardiac evaluation
- Nutritional evaluation
- Anaesthetic evaluation
- Sleep apnoea evaluation
- Psychological evaluation
- Obesity Hypoventilation evaluation
- Upper gastrointestinal anatomy evaluation
- Pulmonary evaluation is usually for pulmonary embolism and venous thromboembolis
Informed Consent
After undergoing all the aforementioned evaluations, the new information about the patient's overall candidacy for surgery is re-evaluated, considering the result of pre-operative weight loss. This new information may change the benefit-risk equation discussed at the patient’s initial evaluation.
If the patient is deemed suitable for bariatric surgery, the next question is about the type of surgery. Once Roux-en-Y gastric bypass surgery is confirmed, the patient is provided with all the information about the surgery required to make an informed decision.
The language associated with consent is in simple terms. The consent process, theoretically and ideally, should be a focused discussion reinforcing the personalized risks and benefits to the specific patient, which usually varies from case to case. The patient is provided with ample opportunities to ask any questions.
Ultimately, the patient and the caregivers/family should fully understand the therapy and the risks associated with the treatment.
Commencement of surgery is done only after the informed consent form is signed.
During Roux-en-Y gastric Bypass Surgery
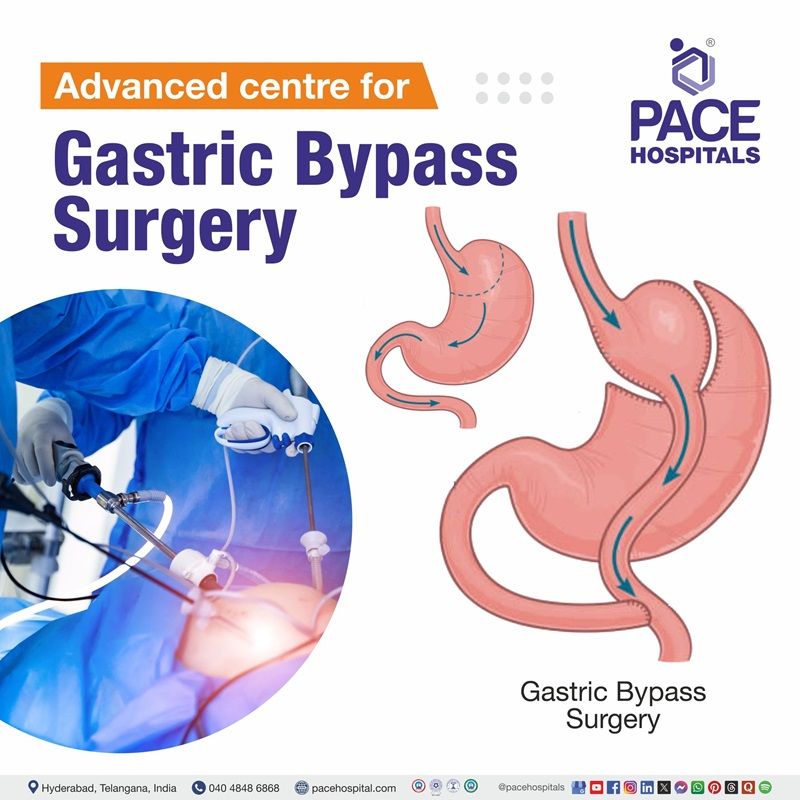
Laparoscopic techniques vary between surgeons, and there is no established standardization. The steps of Roux-en-Y-gastric bypass (RYGB) include 1) gastric pouch creation, 2) creation of biliopancreatic limb, 3) jejunojejunostomy creation, and 4) creation of gastrojejunostomy.
Laparoscopic procedures differ from one surgeon to the next, and there isn’t any particular school of recognised standards. Roux-en-Y gastric bypass (RYGB) procedures include
- The formation of a gastric pouch
- The formation of a biliopancreatic limb
- The formation of a jejunojejunostomy
- The formation of a gastrojejunostomy.
General anaesthesia is provided and the patient made to lie down with legs spread wide to establish a pneumoperitoneum (inflated abdomen).
- Commonly, the Veress needle is injected into the right hypochondrium, and 4-5 cm above the umbilicus, an optical trochar is inserted.
- Additional 12 mm ports are inserted in the left upper quadrant and right upper quadrant.
- To retract the liver, a 5 mm port and Nathanson retractor attached to Martin's arm are inserted.
The formation of a gastric pouch
- Patient is placed in reverse Trendelenburg position to expose the gastroesophageal junction.
- Dissection begins at the angle of His exposing the left crus of the diaphragm and gastrohepatic ligament.
The formation of biliopancreatic limb
- The biliopancreatic limb (afferent limb consisting of the duodenum and proximal jejunum) remains with the remnant stomach.
- The limb gets digestive enzymes from hepatobiliary tract, pancreas and the stomach.
Formation of jejunojenuostomy
- The biliopancreatic limb is connected to the last segment of jejunum at this point to create side-to-side jejunojejunostomy (JJ anastomosis).
Formation of gastrojejunostomy
- The Roux limb of the middle part of intestine is brought up and a side-to-side gastrojejunostomy is created by a linear stapling device.
Leak test
- Before the completion of the surgery, an upper endoscopy leak test is performed keeping the gastrojejunostomy in view.
After Roux-en-Y gastric bypass surgery
- The patients need to have overnight stay as research showed that same-day discharge brought increased mortality and morbidity.
- The patients will be taken into a recovery room or post-anesthesia unit once their vital signs (heart rate, respiration rate, and blood pressure) are stabilized.
- Appropriate hydration and pain and nausea control are initiated.
- During the in-hospital stay, patients are observed for signs of leak or bleeding, such as tachycardia (increased heart rate), tachypnoea (increased respiration), or fever.
- Anti-embolic stockings and intermittent sequential compression devices are removed as soon as the patient is ready to walk.
Complications of Roux-en-Y Gastric Bypass Surgery
The mortality of Roux-en-Y gastric bypass is roughly 0.2%, higher than that of sleeve gastrectomy and gastric banding combined.
Early Complications:
- Anastomotic leaks: A potentially fatal complication which could be seen within 24 hours in 3% of cases. An intraoperative leak test can reduce the odds.
- Hemorrhage: Usually due to anastomoses and staple lines. Usually resolves on its own but till that time the patient may need transfusion.
- Deep vein thrombosis or pulmonary embolism: One of the commonest causes of death after gastric bypass. Prevention is necessary and the patient may be prescribed given compression stockings, and post-operative medication for at least one-week minimum.
Late Complications
- Internal herniation: Hernias can occur in up to 7% of cases. Three types of hernias can be seen.
- A Petersen's hernia - bowel herniation between the jejunal mesentery of the alimentary limb and the colon.
- The other two hernias may be seen at the JJ anastomosis and through the mesocolic defect.
- Micronutrient deficiency: Lifelong mineral/vitamin supplementation is necessary as these deficits are caused due to malabsorption. Common deficiencies include vitamin B12, thiamine, iron, zinc, folate, and vitamin D.
- Gallstone formation: Rapid weight loss could signify the odds of gallstones occurring in 30% of patients. Cholecystectomy is performed to remove them.
- Dumping syndrome: Quick movement of sugar from the stomach into the duodenum due to gastric emptying, altering diet and decreasing the size of meals can help.
Questions that the patients can ask the healthcare team about Roux-en-Y gastric bypass surgery?
- Can I have an online consultation for follow-up, or should I be present there?
- Now that I am eating less compared to earlier, won't I feel weak and tired?
- When can I start riding my bike or driving my car after surgery?
- How much time does it take to fully heal the surgical cuts?
- How many months will the follow-up is going to be?
- How many times should I come for a follow-up?
- How can I manage pain after surgery?
- When can I start exercising again?
- How do I care for my incisions?
- What should my diet plan be?
- When can I return to work?
Does jejunojejunostomy induce vulnerability in Roux-en-Y gastric bypass procedure?
Abdominal pain, especially postprandial abdominal pain could be seen among 22–30% of patients who underwent Roux-en-Y gastric bypass.
Despite being scanned with abdominal computer tomography (CT), correct pathology may not be identified. Thus, a diagnostic laparoscopy is usually done in such patients in the absence of significant radiological findings.
Of all the other complications, the adhesions and kinking jejunojejunostomy takes the top place. Adhesions and kinking at the jejunojejunostomy partially obstruct as evidenced by postprandial pain in conjunction with nausea and complex hypoglycemia (low blood sugar).
A 2021 retrospective analysis demonstrated the efficiency of laparoscopic revisional surgery in these patients. Either adhesiolysis or total revision of the jejunojejunostomy is done among 115 patients suffering from postprandial pain due to adhesions and kinking jejunojejunostomy after Roux-en-Y gastric bypass procedure. The study resulted in 38% of patients experiencing a complete and lasting resolution of symptoms following revisional surgery. Another 28% reported lasting improvement but were substantially not entirely free from symptoms. A 13% experienced no lasting improvement, and 14% underwent gastric bypass reversal due to persisting symptoms.
Reduction of diabetes after Roux-en-Y Gastric Bypass
Roux-en-Y gastric bypass is a therapeutic option for severely obese adults associated with type 2 diabetes. The weight loss induced by Roux-en-Y gastric bypass is superior to that of nonsurgical management.
Nevertheless, a potent anti-diabetes effect was also observed in few cases. This anti-diabetic effect may extend beyond the period of perioperative caloric restriction, which demonstrates an independent effect of the surgery affecting glucose metabolism.
A 2005 study demonstrated that the changes in insulin resistance following Roux-en-Y gastric bypass supported with documentation of marked falls in plasma insulin levels within days of gastric bypass.
In this study insulin resistance is measured using an Intravenous Glucose Tolerance Test (IVGTT) both before and after Roux-en-Y gastric bypass surgery (after 6 days later). The IVGTTs clearly demonstrate substantial loss of insulin resistance within 6 days following surgery, thus concluding the reduction of diabetic condition in the patients.
Roux-en-Y Gastric Bypass vs Sleeve Gastrectomy
A large, Swedish-Norwegian, multicenter randomized clinical trial was published in 2024 which analysed the difference in the of perioperative complications between two different groups who underwent either sleeve gastrectomy and Roux-en-Y gastric bypass.
Both sleeve gastrectomy and Roux-en-Y gastric bypass surgeries are bariatric surgeries which are done in patients with extreme obesity. The results are as follows:
| Parameters | Sleeve gastrectomy | Roux-en-Y gastric bypass |
|---|---|---|
| Mean operating time | 47.3 minutes | 67.7 minutes |
| Adverse event occurred in | 40 of 878 patients (4.6%) | 54 of 857 patients (6.3%) |
| Serious adverse events | 15 of 878 patients (1.7%) | 23 of 857 (2.7%) |
| Small bowel obstruction | 0 of 872 patients (0%) | 6 of 850 (0.7%) |
| Subsequent readmissions | 27 of 873 (3.1%) | 34 of 851 (4.0%) |
Although serious adverse events within 30 days was higher in the Roux-en-Y gastric bypass group when compared with the sleeve gastrectomy group, it was not statistically significant. The study concluded that perioperative morbidity was low and was insignificant between the groups. The authors suggested that the perioperative risk should be of limited focus in case of choosing between sleeve gastrectomy and Roux-en-Y gastric bypass surgery.
Roux-en-Y gastric bypass revision surgery
Roux-en-Y gastric bypass surgery (RYGB) is one of the most common procedures in the world between the years 2014–2018. While traditionally, Roux-en-Y gastric bypass surgery has been the gold standard bariatric procedure, but like any other procedure, revisional or conversional surgeries may be required, due to weight regain or failure of weight loss.
Weight regain is defined in 40.7% of studies as an Excess Weight Loss (EWL) less than 50% from the original pre-operative weight.
Up to 40% of patients may not have any anatomical reason for weight loss failure. In most cases, however, weight loss failure may occur due to anatomical abnormalities such as:
- Dilated gastro-jejunal anastomosis (GJA) - Possible weight regain due to decreased distension of the gastric pouch and therefore a reduction in satiety stimulation.
- Dilated gastric pouch – The proximal gastric pouch gets enlarged with a post-procedural capacity exceeding the normal of 15-20 mL.
- Gastro-gastric fstula - Opening an abnormal communication between the excluded gastric remnant and the neo gastric pouch.
- Non-anatomical reasons for weight loss failure include nutritional concerns, abnormal behaviour, and polyphagia may be also essential causes.
Endoscopic revision of Roux-en-Y gastric bypass surgery
Gastro-jejunal anastomosis greater than 15 millimeters is considered an indication for endoluminal revision in failed Roux-en-Y gastric bypass surgery. The technical endpoint is to achieve a stoma diameter between 4 and 9 mm. There are some reports that believe a correlation between stoma diameter (mostly greater than 2 cm in diameter) and weight regain and weight loss failure after the primary operation.
There are several endoscopic procedures for revision of failed Roux-en-Y gastric bypass surgery including
- Restorative Obesity Surgery Endoscopic
- Endoscopic gastro-jejunostomy revision
- Transoral outlet reduction (TORe), and
- Endoscopic gastric plication with StomaphyX.
Gastric Bypass Surgery Cost in Hyderabad, India
The cost of Roux-en-Y Gastric Bypass (RYGB) in Hyderabad generally ranges from ₹2,10,000 to ₹4,80,000 (approx. US $2,500 – US $5,760).
The exact cost varies depending on the patient’s BMI, severity of obesity, associated metabolic disorders (diabetes, hypertension, sleep apnea, fatty liver), need for preoperative investigations, hospital stay, surgeon expertise, and facilities — including cashless insurance, TPA corporate tie-ups, and support with medical insurance documentation wherever applicable.
Cost Breakdown According to Type of Bariatric Treatment & Care
- Bariatric Surgeon Consultation + Preoperative Assessment – ₹1,000 – ₹2,500 (US $12 – US $30)
- Preoperative Tests (CBC, LFT, RFT, Thyroid Profile, ECG, Echo, Chest X-ray) – ₹3,500 – ₹7,500 (US $42 – US $90)
- Endoscopy (If Required Before Surgery) – ₹2,000 – ₹4,500 (US $24 – US $54)
- Anesthesia Evaluation – ₹1,000 – ₹2,500 (US $12 – US $30)
- Roux-en-Y Gastric Bypass Surgery – ₹2,10,000 – ₹4,20,000 (US $2,500 – US $5,040)
- High-BMI / Complex Case Surcharge – ₹15,000 – ₹45,000 (US $180 – US $540)
- Hospital Stay (2–4 Days) – ₹15,000 – ₹45,000 (US $180 – US $540)
- Postoperative Medications & Supplements – ₹4,000 – ₹12,000 (US $48 – US $144)
- Dietitian & Lifestyle Counselling – ₹1,500 – ₹4,000 (US $18 – US $48)
- Follow-up Investigations (Blood tests, Vitamin Levels) – ₹1,500 – ₹5,000 (US $18 – US $60)
Frequently Asked Questions (FAQs) on Gastric-Bypass Surgery
How does gastric bypass work?
The procedure helps to reduce stomach size, reroutes the intestine, and brings hormonal changes that support weight loss and improved metabolism. These changes help limit food intake, enhance satiety, and improve insulin sensitivity, which benefits individuals with obesity and diabetes like metabolic disorders.
Which Is the best hospital for Roux-en-Y Gastric Bypass in Hyderabad, Telangana, India?
PACE Hospitals, Hyderabad, is one of the most trusted centers for bariatric and metabolic surgery.
We have highly experienced team of experts’ bariatric surgeons, endocrinologists, nutritionists, anesthesiologists, and physiotherapists provide comprehensive care for:
- Severe obesity
- Type 2 diabetes requiring metabolic surgery
- Hypertension and dyslipidemia
- Obstructive sleep apnea
- NAFLD/MASLD and obesity-related liver disease
- PCOS-associated weight gain
- Failed weight-loss attempts through lifestyle measures
We provide minimally invasive laparoscopic surgery, advanced ICU care, structured patient education, and long-term follow-up programs, PACE Hospitals ensures safe, precise, and patient-focused outcomes — supported by cashless insurance, TPA tie-ups, and documentation assistance.
How long does gastric bypass surgery take?
Most procedures take about 1.5 to 3 hours, depending on the patient's anatomy and the surgical approach used. Laparoscopic techniques have shortened surgery times and improved outcomes in most cases.
What are 3 common long-term complications of gastric bypass?
Common long-term issues include marginal ulcers; iron, B12, and calcium deficiencies; and internal hernias. Some individuals may also experience low blood sugar episodes or weight regain over time. Regular follow-up helps detect and manage these conditions early to avoid future complications.
Is gastric bypass safe?
Gastric bypass is considered safe when performed by trained bariatric surgeons, with complication rates continuing to decline as techniques improve. Long-term health benefits often outweigh the risks for individuals with severe obesity or metabolic disease.
What is the cost of gastric bypass surgery in hyderabad at PACE Hospitals?
At PACE Hospitals, Hyderabad, the cost of Roux-en-Y Gastric Bypass typically ranges from ₹1,95,000 to ₹4,50,000 and above (approx. US $2,350 – US $5,400), offering an affordable and specialized option for bariatric and metabolic surgery. However, the final cost depends on:
- BMI, surgical complexity, and comorbidities
- Need for endoscopy or additional imaging
- Type of anesthesia and operative duration
- Need for robotic assistance
- Length of hospital stay
- Advanced comorbidity management (diabetes, sleep apnea, fatty liver)
- Postoperative supplements and long-term follow-ups
- Nutritional and metabolic counseling requirements
Patients with fewer comorbidities and shorter recovery duration fall at the lower range, whereas individuals with high BMI, complex anatomy, or extended postoperative care fall toward the higher range.
After evaluation, blood tests, imaging, and multidisciplinary consultation, our bariatric team provides a personalized surgical plan and a transparent cost estimate based on the patient’s health needs.
What can you never eat again after gastric bypass?
There is no single food that is permanently "forbidden," but certain items become not consumable because the altered stomach pouch and bypassed intestine change digestion impressively. Foods extremely high in sugar, carbonated drinks, fried foods, and tough meats often triggers abdominal discomfort, dumping syndrome, or rapid blood sugar shifts. Most of research-oriented studies emphasize lifelong avoidance of highly processed, sugary foods because they interfere with nutrient absorption and weight maintenance after surgery.
How to know if there's something wrong with gastric bypass?
If an individual gets warning signs such as persistent vomiting, abdominal pain that worsens over time, dehydration, rapid heartbeat, fever, difficulty swallowing, or blood in stool, they require immediate medical evaluation. Moreover, if a patient faces complications such as anastomotic leaks, strictures, internal hernias, and nutritional deficiencies weeks to months after surgery, so they should not ignore it as may relate to something wrong with gastric bypass.
Is gastric bypass reversible?
Reversal process is technically possible, but it is complex work and carries higher risks than the original procedure. Reversal is usually considered only for severe problems such as long-term ulcers, malnutrition, or complications that cannot be managed with standard treatment.
Is blood stool normal after gastric bypass?
Blood in stool is not expected usually and should be evaluated promptly. It may indicate existing of an ulcer, anastomotic bleeding, or irritation in the digestive tract. Early medical assessment helps prevent serious complications such as anemia, ongoing bleeding or any such complications
Will heartburn go away with gastric bypass surgery?
Many individuals experience relief from reflux after gastric bypass because the procedure reduces acid exposure and diverts bile away from the stomach pouch. Some may still develop symptoms due to ulcers or pouch irritation, making follow-up important.
Does insurance cover gastric bypass?
Yes. In India, many major health insurance companies cover gastric bypass surgery when it is medically required for treating obesity and related health problems arised by it. However, approval usually depends on meeting certain criteria such as a high BMI, long-standing obesity, and conditions like type 2 diabetes, sleep apnea, hypertension, PCOS, or joint disorders. Most insurers follow India's bariatric surgery coverage norms, which require medical documentation, diagnostic reports, and evidence of supervised weight-loss attempts.
Coverage may be provided as cashless if the hospital is empaneled with the insurer, or as reimbursement in other cases. Some policies may have waiting periods or require specific preauthorization before the surgery. Checking individual policy terms and TPA requirements is important, as rules may vary across Indian insurers.
Where is the stomach located after gastric bypass?
The surgery leaves a small stomach pouch at the upper portion of the stomach, which receives food directly. The remaining larger portion stays in place but is bypassed and continues to produce digestive enzymes that join food further down the intestine.
How to qualify for gastric bypass?
Eligibility generally includes a BMI of 40 or above, or a BMI of 35 or above with obesity-related conditions such as diabetes or sleep apnea. Documentation of previous attempts at weight loss and ability to commit to long-term follow-up are also important criteria.
Why choose PACE Hospitals?
- A Multi-Super Speciality Hospital.
- NABH, NABL, NBE & NABH - Nursing Excellence accreditation.
- State-of-the-art Liver and Kidney transplant centre.
- Empanelled with all TPAs for smooth cashless benefits.
- Centralized HIMS (Hospital Information System).
- Computerized health records available via website.
- Minimum waiting time for Inpatient and Outpatient.
- Round-the-clock guidance from highly qualified super specialist doctors, surgeons and physicians.
- Standardization of ethical medical care.
- 24X7 Outpatient & Inpatient Pharmacy Services.
- State-of-the-art operation theaters.
- Intensive Care Units (Surgical and Medical) with ISO-9001 accreditation.