Live-donor Liver Transplant at Govt. Institute during #COVID
Live-donor liver transplant at Osmania hospital during #COVID. The logistics for a liver transplant during the current lockdown in a government setup is a huge task, kudos to Dr. CH Madhusudan, the OGH anaesthesia and GI team for rising up to the challenge. 1 week later both donor and recipient are doing well. A 10 hour operation in the present high risk covid environment not with standing, team voluntary work helping the poor HPB patients at both Osmania and Gandhi (Hyderabad's premier govt institutes) is something he found extremely satisfying in past 5 years.
Mr. AK 50 year male 135 kg with comorbidities uncontrolled diabetes Hypertension, COPD and sleep apnea.
Mr. AK 50 year male. BMI 44. 135 kg with comorbidities uncontrolled diabetes Hypertension, COPD and sleep apnea. Underwent Minigastric bypass. Post procedure doing great with 45 kg weight loss and completely cured of his type 2 diabetes, Hypertension and sleep apnea.
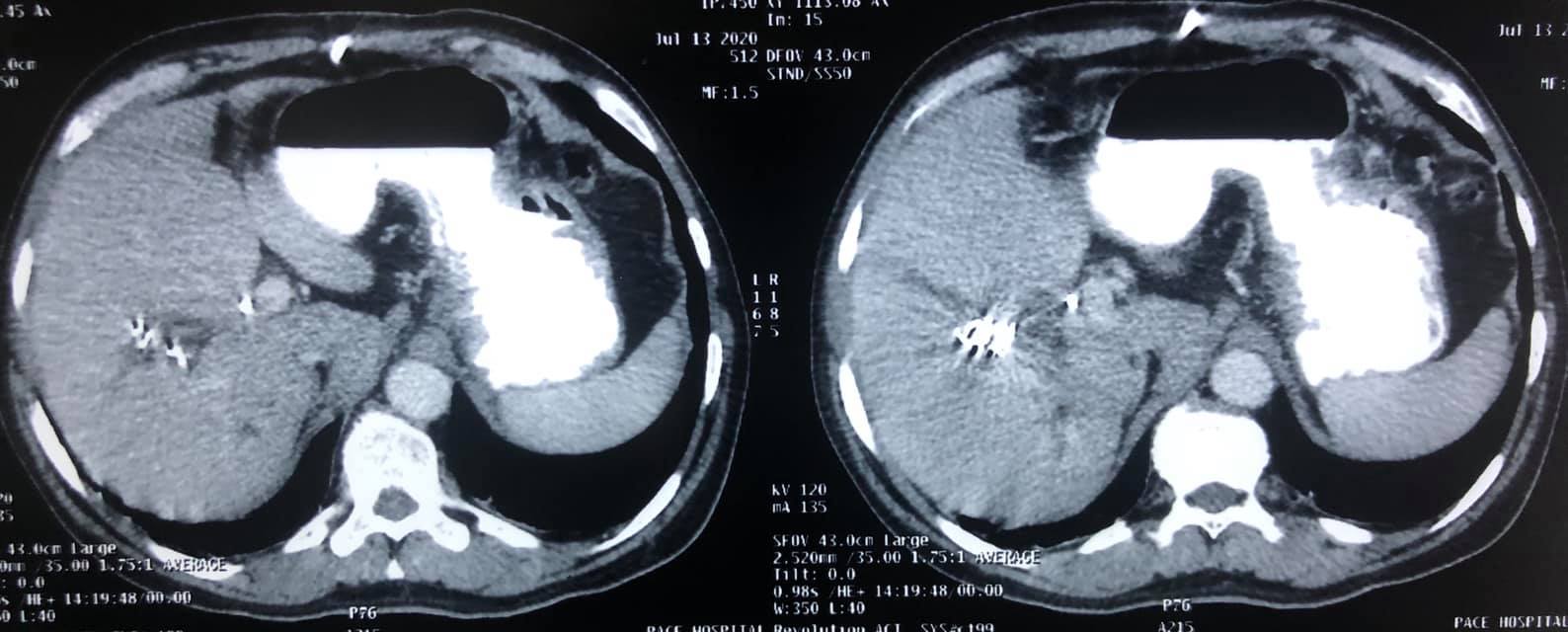
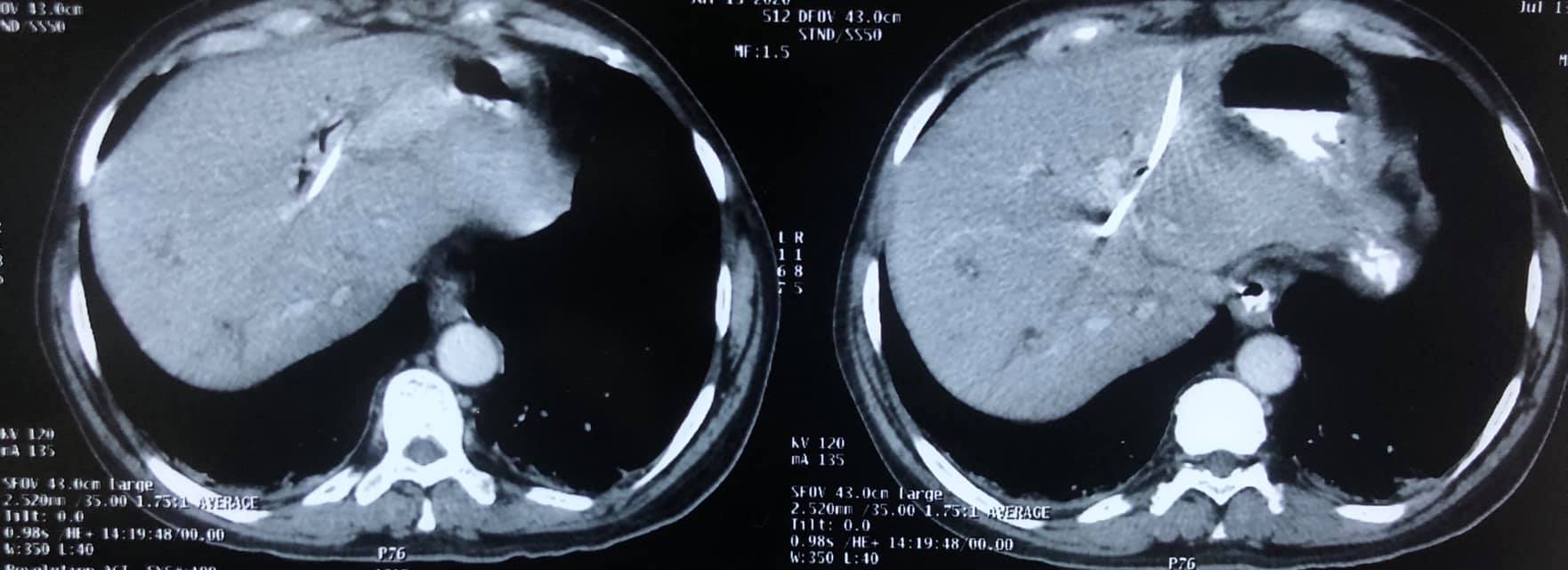
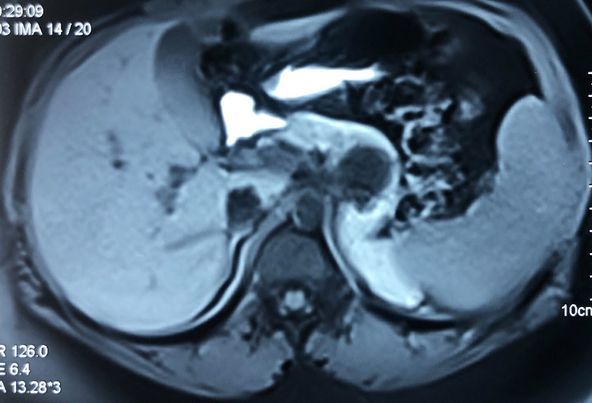
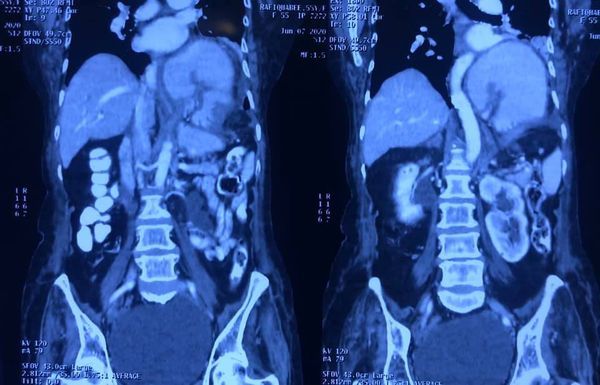
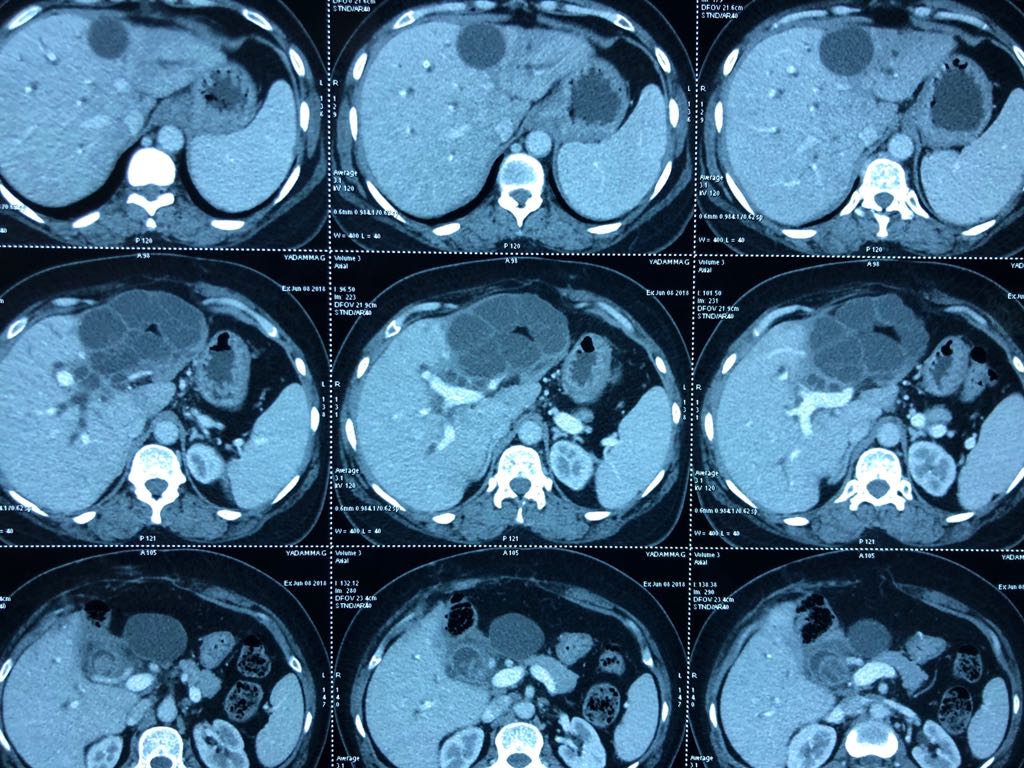
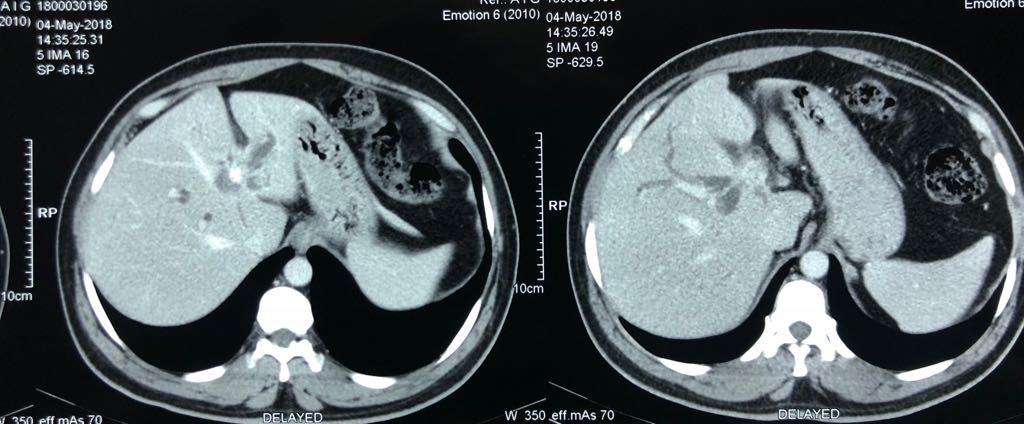
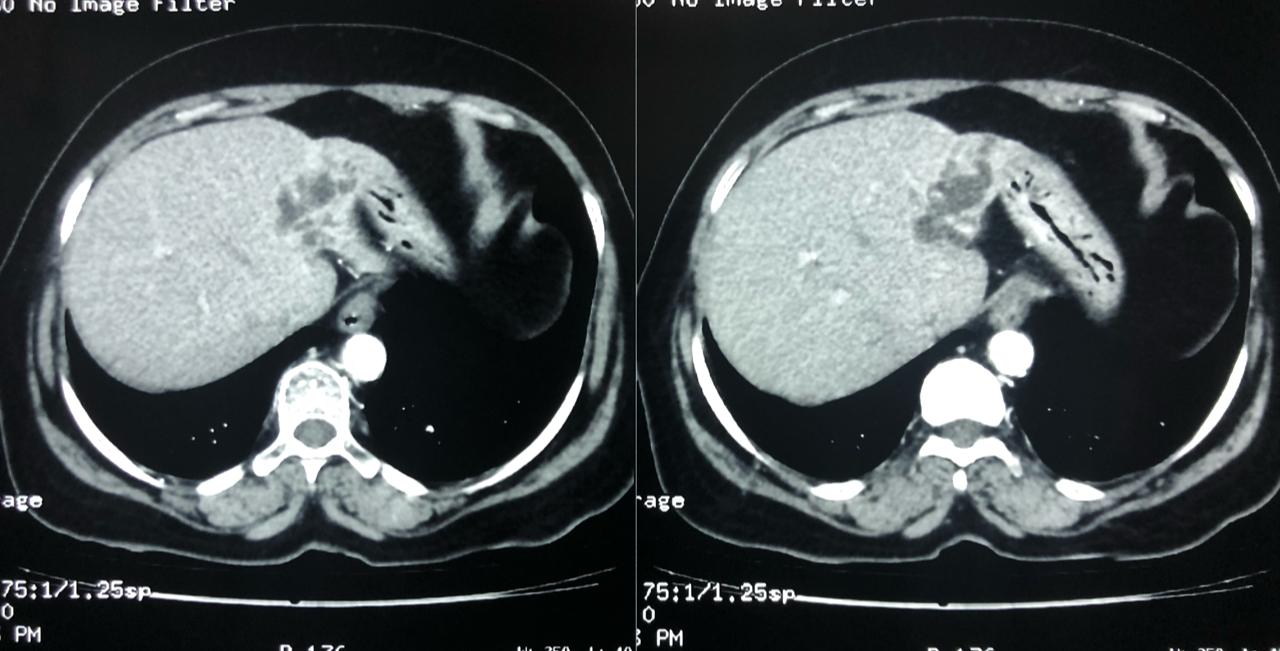
65 years of man type 3A hilar cholangiocarcinoma (complex hepatobiliary malignancy) with deep jaundice
SIX STEPS TO SUCCESS IN A ROLLER COASTER COVID CHALLENGE
- STEP 1: Left PTBD (to bring down jaundice)
- STEP 2: portal vein embolisation to allow growth of the small remnant left liver
- STEP 3: Right sided anterior and posterior PTBD to control persistent fever after initial intervention.
- STEP 4: admitted for surgery COVID positive CT CO-RADs 5 managed medically
- STEP 5: after 3 weeks waiting and repeat COVID PCR negative (couldn’t wait longer for risk of catheter dislodgement while waiting) underwent an Extended Rt hepatectomy with caudate lobectomy bile duct excision Left hepaticojejunostomy
- STEP 6: despite all the trials& tribulations and 7 hr surgery patient had a smooth recovery discharged by D6. An extremely satisfying result in a very difficult malignancy and a super motivated patient.
5 years old young girl with chronic pancreatitis with rupture in the pancreatic tube
5 years old young girl with suffering from chronic pancreatitis. In addition to chronic pancreatitis she had a rupture in the pancreatic tube causing a mass & swelling in the tail of pancreas. Due to intractable pain and sitophobia (fear of food) for more than an year with severe malnutrition she had stopped stepping out to play and never been to a school in past 2 years. After arranging funds thru CMRF and welfare workers. We performed a distal pancreatic resection with LPJ (pancreatic drainage procedure). As they are from a village she was lost to follow up after a couple of early post op visits. Now 3 years later they heard about warangal visit and came for follow up. Very happy to see that she is completely pain free and doing well. She has transformed to a very active and playful girl who is her class topper and when I asked her said she wishes to be a doctor when she grows up. God bless her with great life.
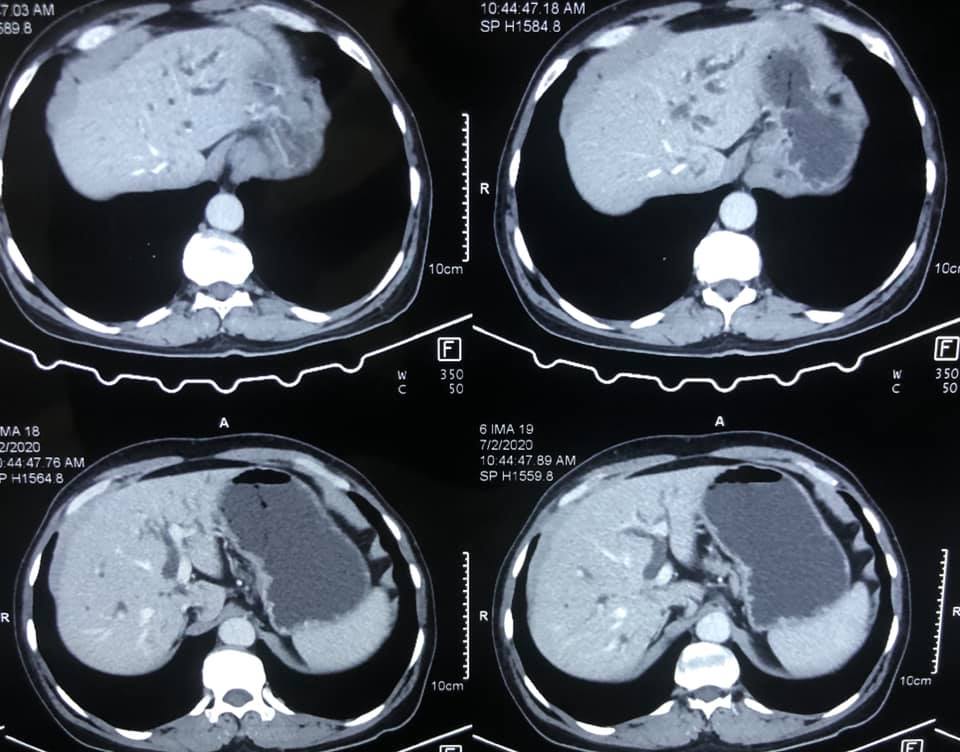
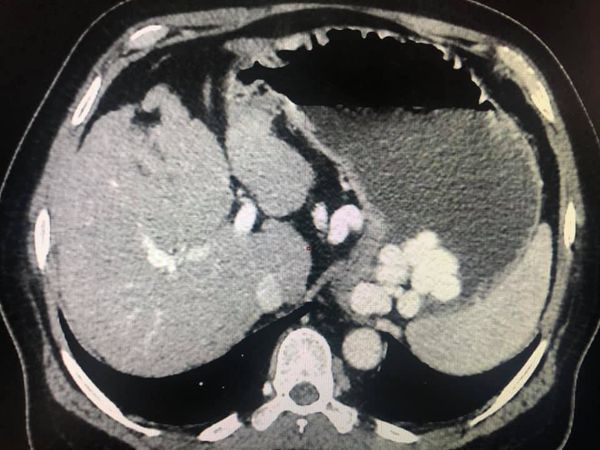
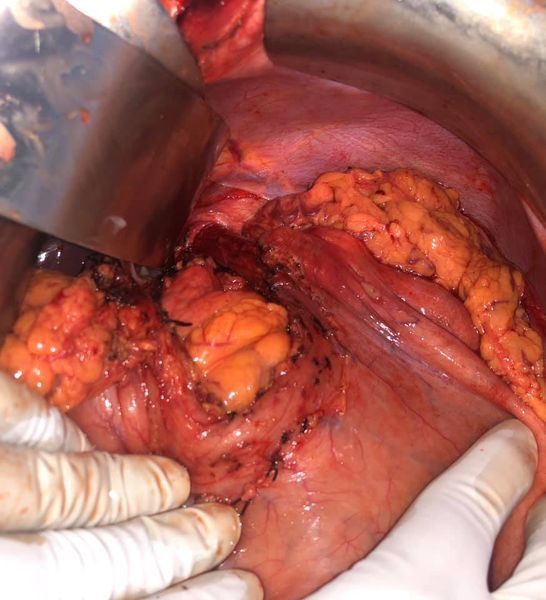
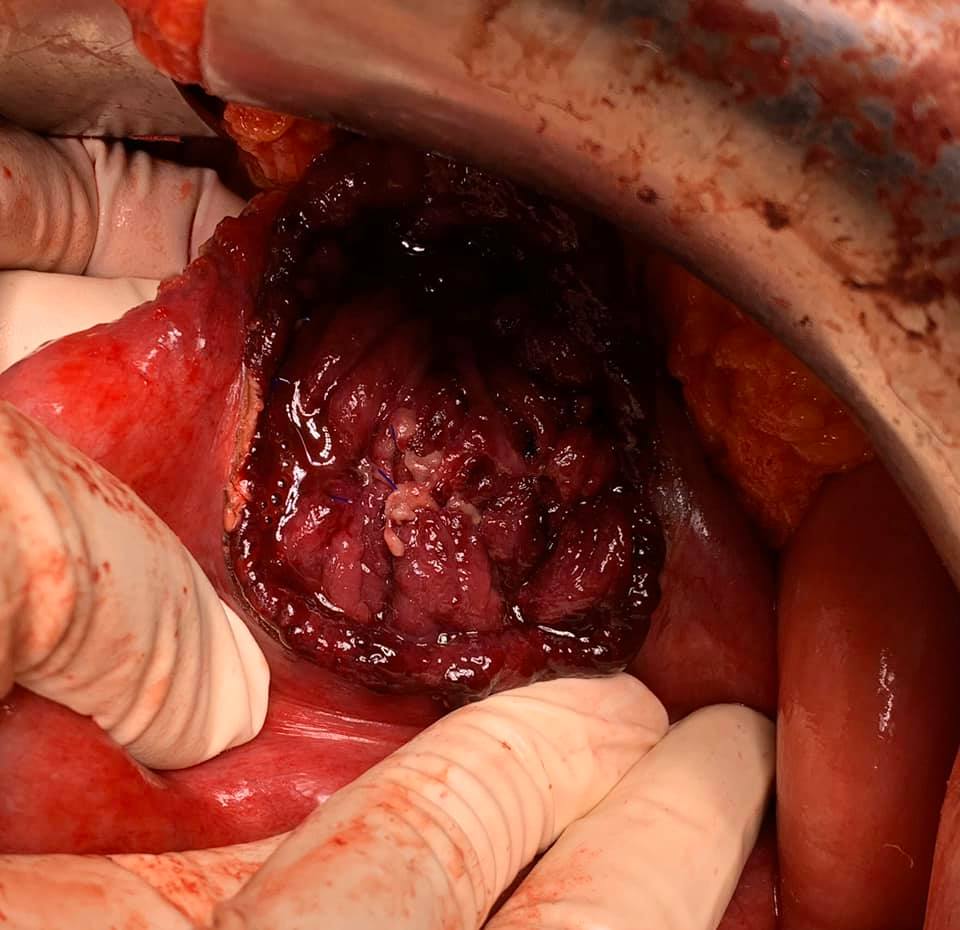
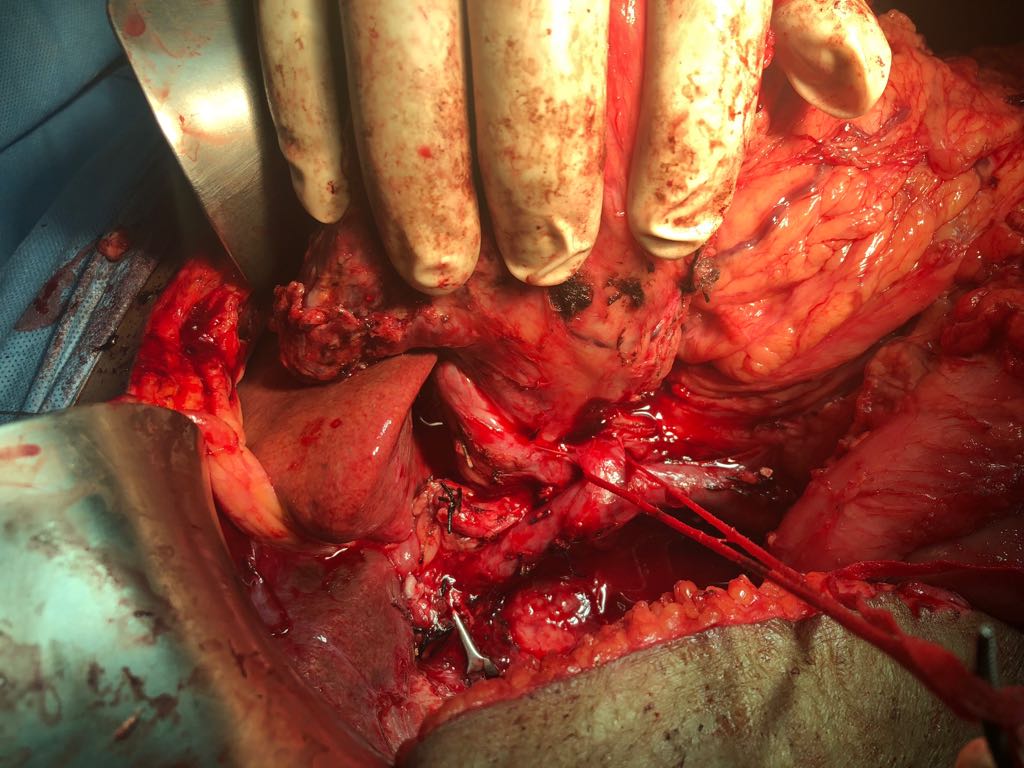
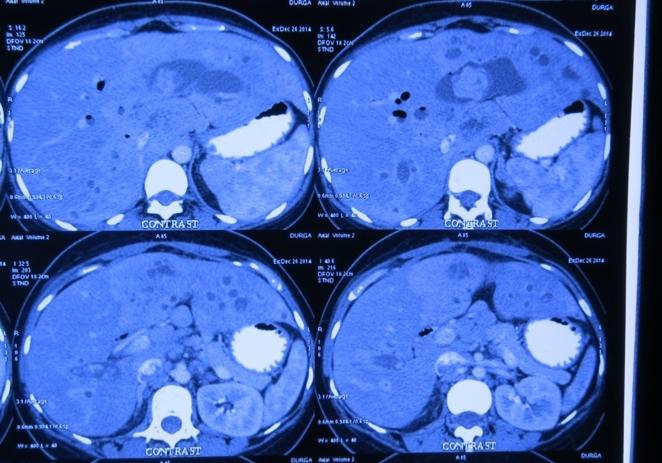
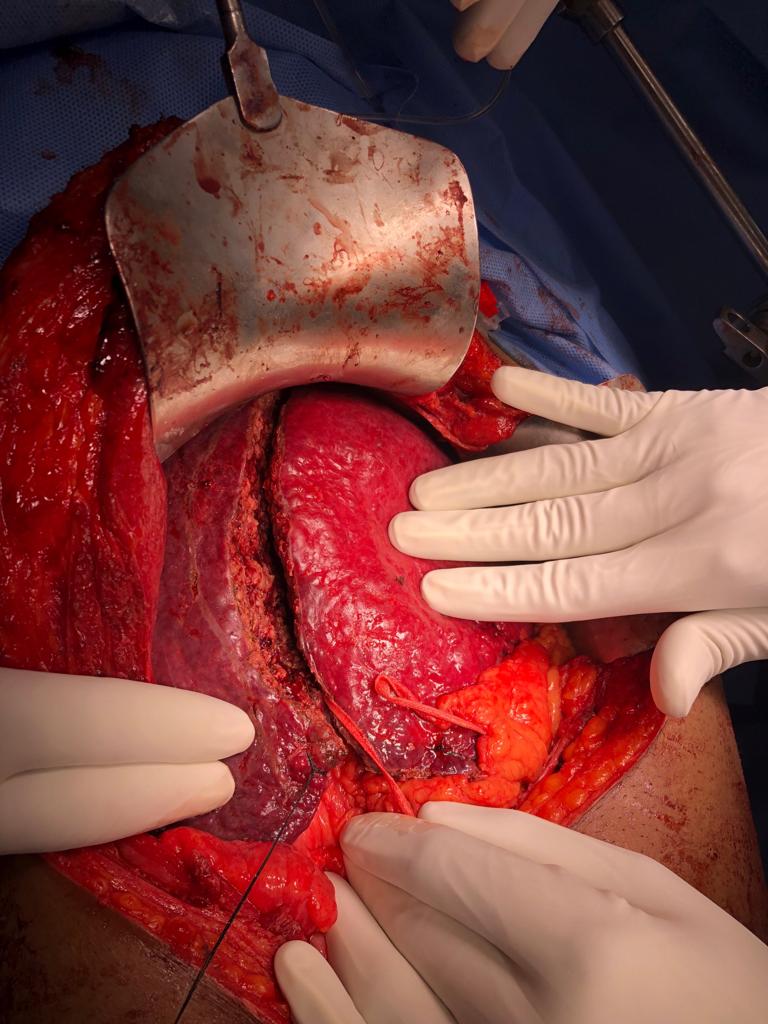
Challenging emergency during the COVID: Child’s A CLD with HUGE gastric varices uncontrolled
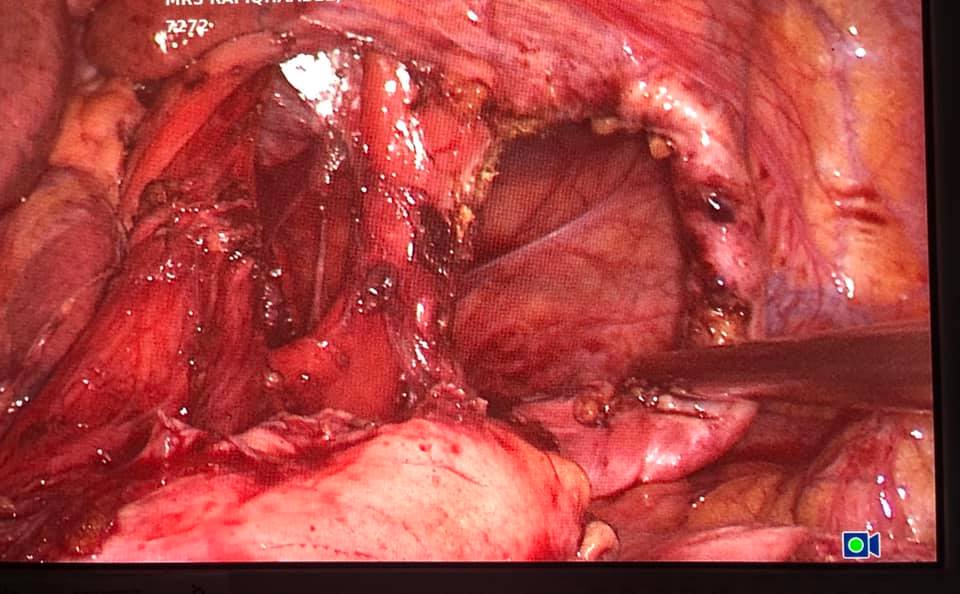
Child’s A CLD with HUGE gastric varices uncontrolled by Endoscopic glue and attempted EUS coiling. One salvage option would be TIPSS with balloon vascular occlusion but due to logistics we went for modified sugiura procedure. Splenectomy + Gastro esophageal devascularisation with anterior Gastrotomy and overseeing of gastric varices with pyloroplasty. Images show 1 CECT showing large gastric fundal varices. 2,3,4 Gastro Esophageal devasc 5, 6 Large fundal varices before and after oversewing. 7. Anterior gastrotomy 8. Pyloroplasty. Postoperative recovery was uneventful.
Cystic neoplasm of Pancreas
Middle aged female patient came with complaints of chronic upper abdominal pain since 6 months. The pain was mild to moderate, dull aching, non-radiating and not related to meals or defecation. It was not associated with vomiting, jaundice or abdominal lump. CT Abdomen suggested a cystic lesion in the distal body of pancreas of size 3x3 cm without communication with PD. Endoscopic Ultrasound guided Fine-needle aspiration (FNA) was performed and aspirated fluid suggested elevated CEA levels to 1168 with elevated amylase and lipase with mucin stain positive. Patient underwent laparoscopic spleen preserving distal pancreatectomy (Warshaw's technique). The resected specimen suggested mucinous cystadenoma of pancreas. The patient is asymptomatic now.
Morbid obesity with weight 170 kg and BMI 62 with COPD, severe OSA
Before - after Mrs. SF aged 41 sufferers from morbid obesity weight 170 kg BMI 62 with COPD and severe OSA for which she was on home BIPAP. Her Diabetes was uncontrolled and was suffering from bilateral osteoarthritis. Due to all these factors she became almost fully armchair bound at young age. She is now at post gastric bypass with a weight loss of 90 kg with complete resolution of DM and OSS leading active and productive life.
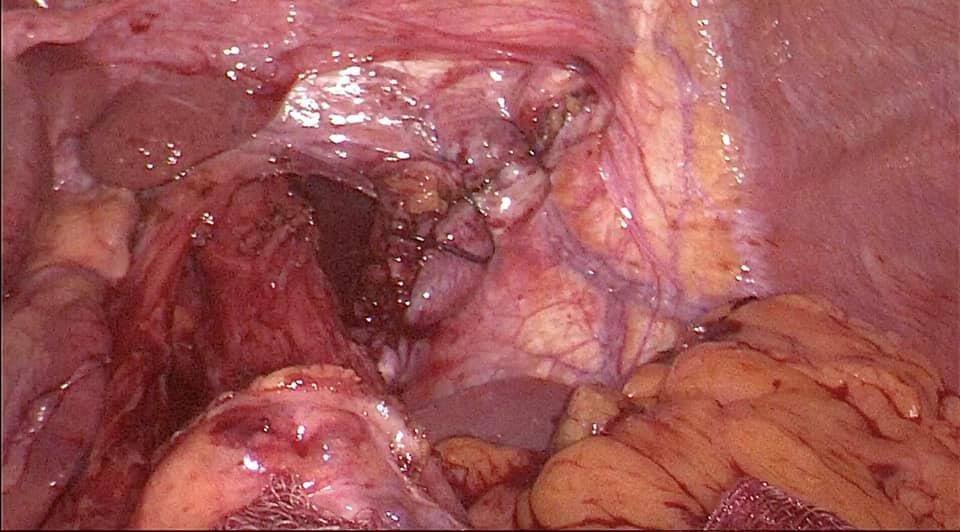
Laparoscopic spleen preserving distal pancreatectomy (WARSHAW TECHNIQUE) for 35 yr old morbidly obese patient
Laparoscopic spleen preserving distal pancreatectomy (WARSHAW TECHNIQUE) 35 yr old morbidly obese patient with a 4 cm mucinous cyst of pancreas confirmed by EUS cytology and CEA level. Planned for a laparoscopic spleen preserving distal pancreatectomy At surgery as the tumor was posterior and densely adherent to splenic artery and vein we opted for the warshaw technique. In this the short gastrics are preserved and a segment of splenic vessels (art & vein) along the resected pancreas are excised removing them at body and again at splenic hilum (as depicted in video). This way spleen is preserved with blood supply based on the short gastrics avoiding the sequela of asplenia such as thrombocytosis and OPSI. The patient had a smooth postoperative recovery.
55 years male suffering with chronic constipation since 10 years
55 years old NRI patient from Germany came with history of chronic constipation since 10 years in the form of hard stools, straining, feeling of incomplete evacuation and h/o finger evacuation of stools.
All the neccessary investigations were done and were normal. Ileo-colonoscopy done suggested a sessile polyp in sigmoid colon of size 1x1cm. Endoscopic submucosal resection was performed. Procedure was uneventful. Biopsy suggested adenomatous polyp with low grade dysplasia.
REVISION BARIATRIC SURGERY Before - After
Miss PM 30 Years, a gifted artist and painter presented to us 3 years ago at 168 kg after a failed sleeve gastrectomy (weight regain post procedure). She underwent a Revision bariatric procedure - her failed Sleeve was converted Minigastric bypass. 3 years post procedure she has shed 80 kgs plus of excess weight to become 84 kg with marked improvement in mobility and breathing difficulties and a renewed focus on her career.
A beautiful case: Left sided Bochdalek Hernia
51 yr old patient with recurrent vomiting and dyspepsia and left sided chest pain. CT, Barium showed fundus and body of stomach in thoracic cavity with Mesentroaxial Volvulus. (image 1-4) Pre-OP thought to be a large sliding paraesophageal hernia operative findings revealed a posterior defect separate from hiatus suggestive of Bochdalek diaphragmatic hernia with a small hiatal hernia. Repair of Bochdalek defect with Crural repair was performed with mesh reinforcement. A 270 degree fundoplication was added (instead of a 360 as Manometry could not be performed preoperatively) (image 6-10) postoperative recovery was smooth (preop-postop xrays image 11-12).
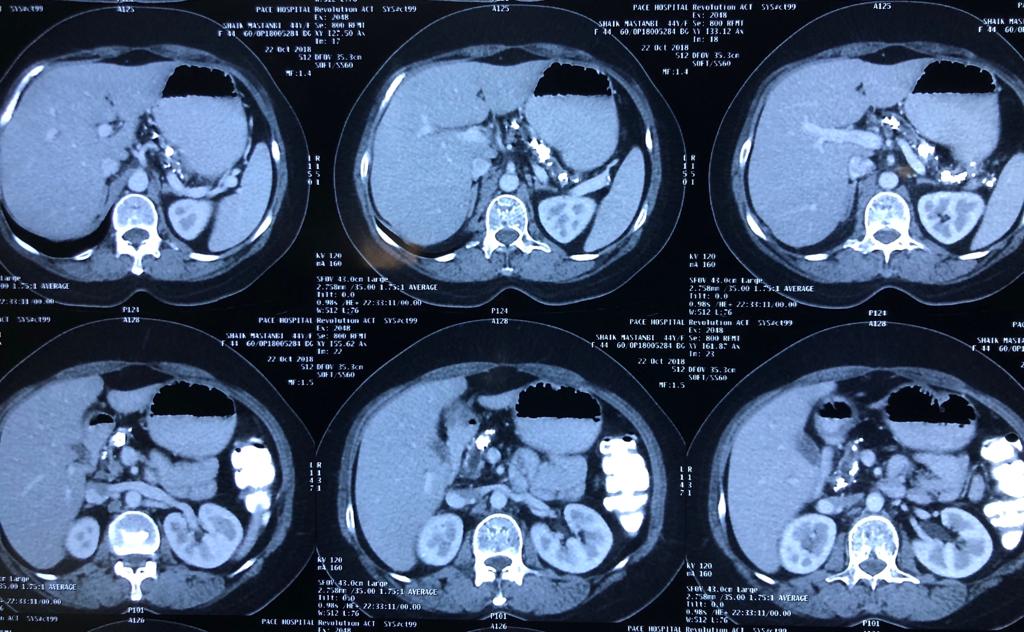
With chemotherapy improved survival with quality of life for Stage 4 cancer patient
Interesting Images March 2019 : Patient came with an early stage carcinoma rectum, underwent Hemicolectomy surgery then lost to follow-up. Later after 9 month patients presented to us with Stage 4 disease (Carcinoma colon with Liver secondaries). Then we started her on treatment with Chemotherapy along with Monoclonal antibodies with six cycle of above said treatment patient achieved near complete remission. We could achieve very good results with chemotherapy even in patients with Stage 4 disease (Carcinoma colon with Liver secondaries).
270 degree toupet fundoplication for GERD with hiatus hernia
270 degree toupet fundoplication for GERD with hiatus hernia. Most patients with intractable GERD and hiatus hernia undergo 360 degree Nissan fundoplication. However all patients undergo high resolution Manometry prior to procedure to assess esophageal body peristalisis. This patient was found to have ineffective peristalisis in lower half of esophagus , doing a Nissens would relieve reflux but lead to dysphasia due to ineffective peristalsis. Therefore such patients we do a 270 degree toupet fundoplication.
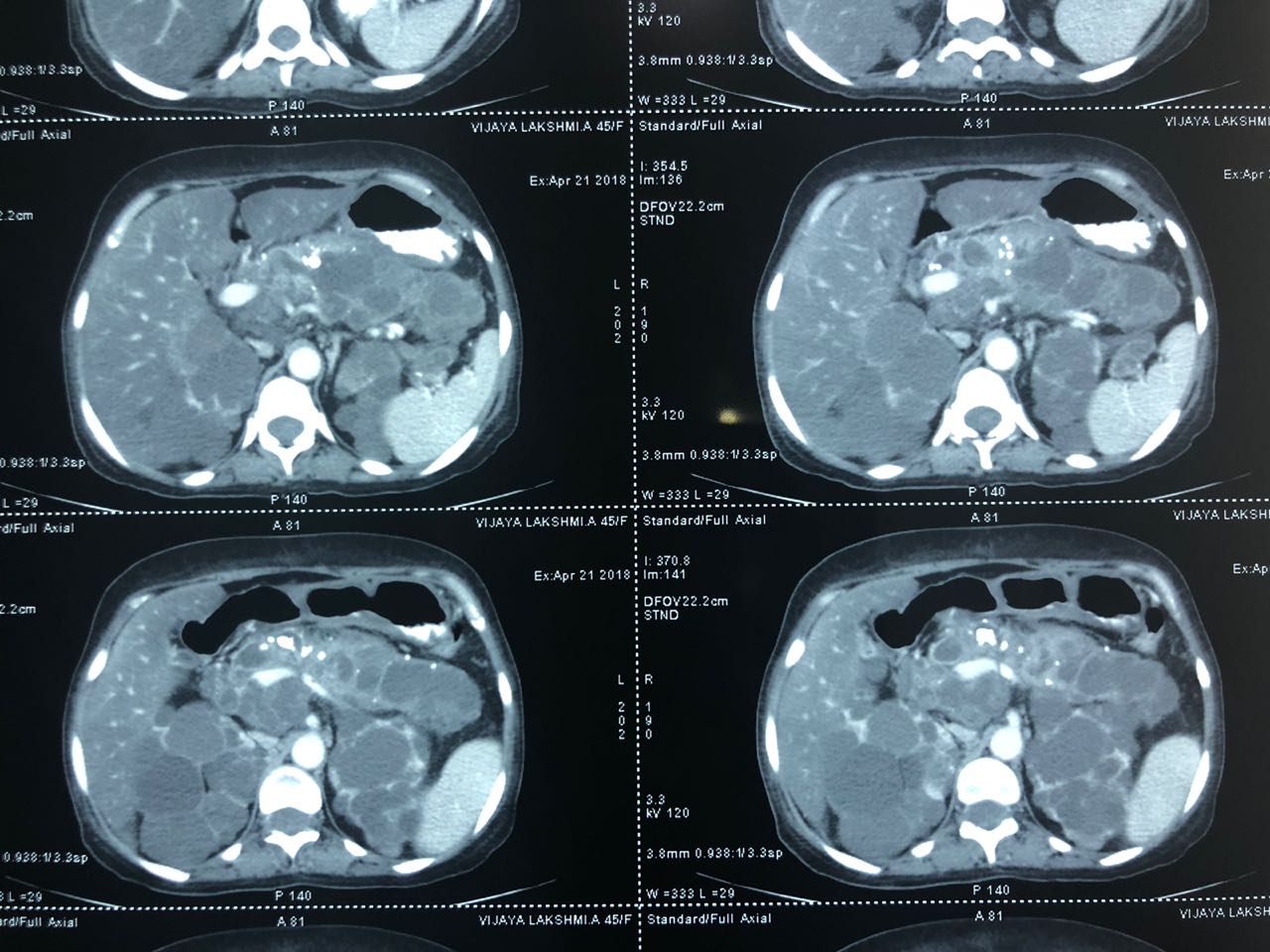
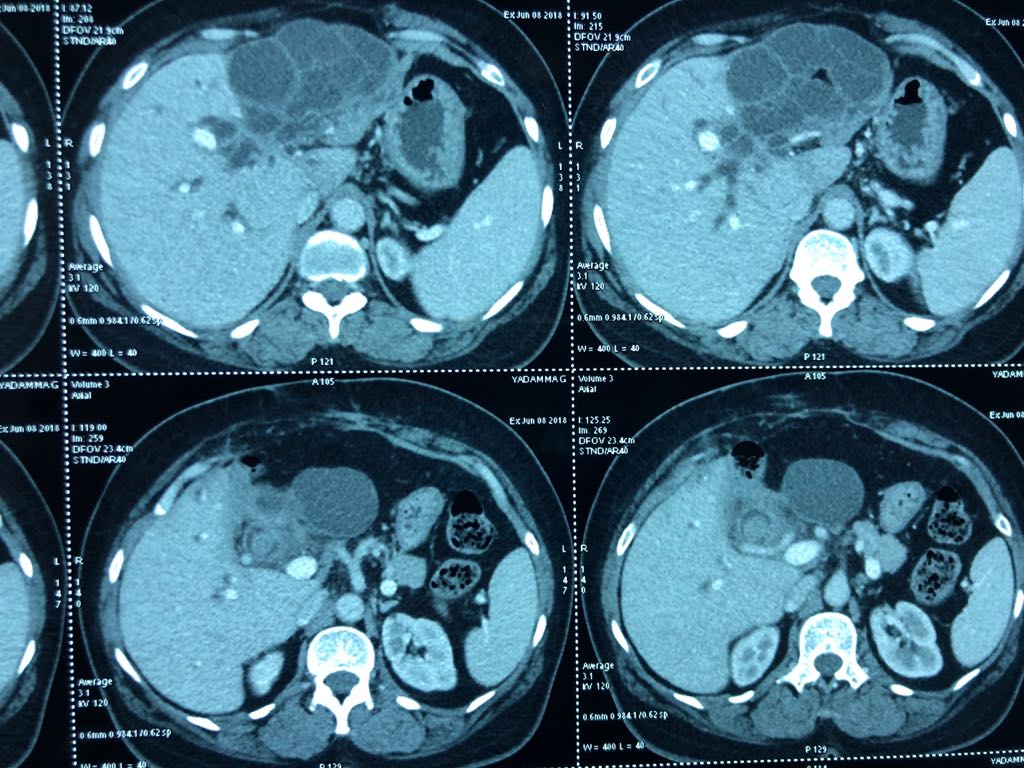
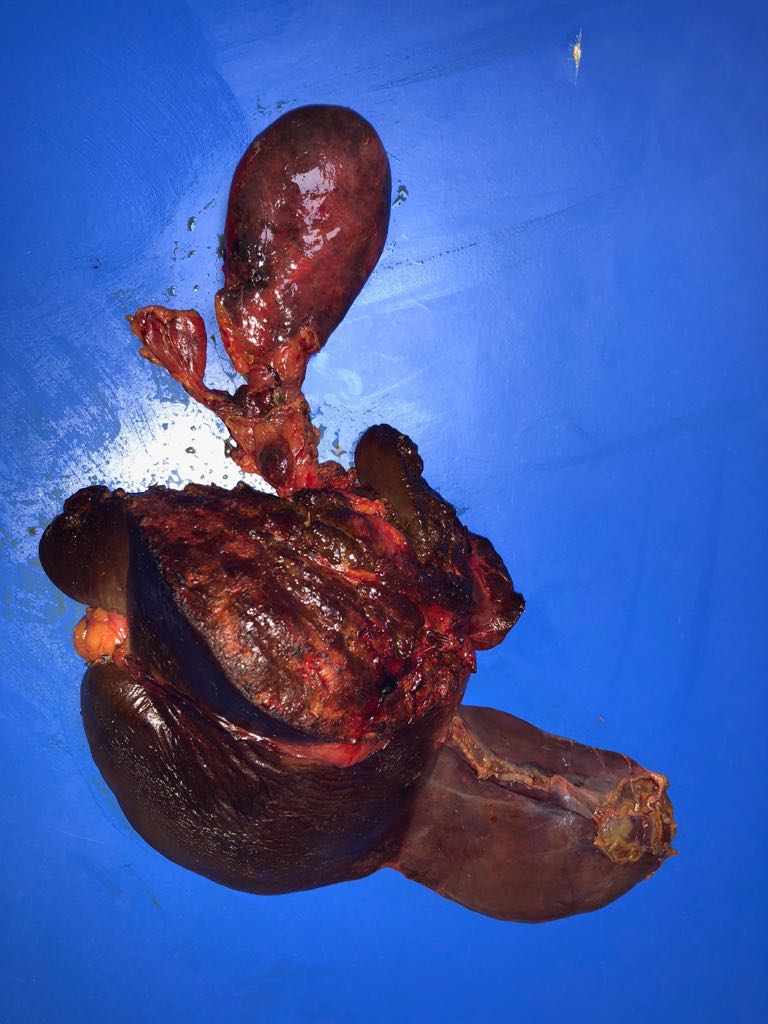
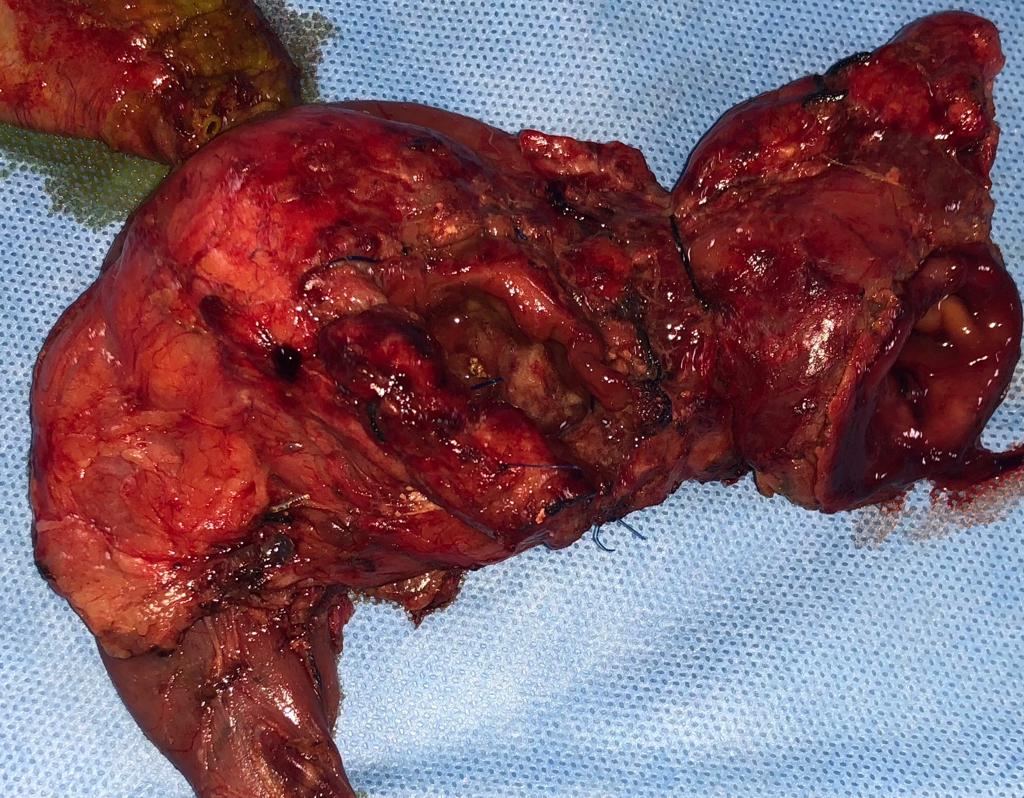
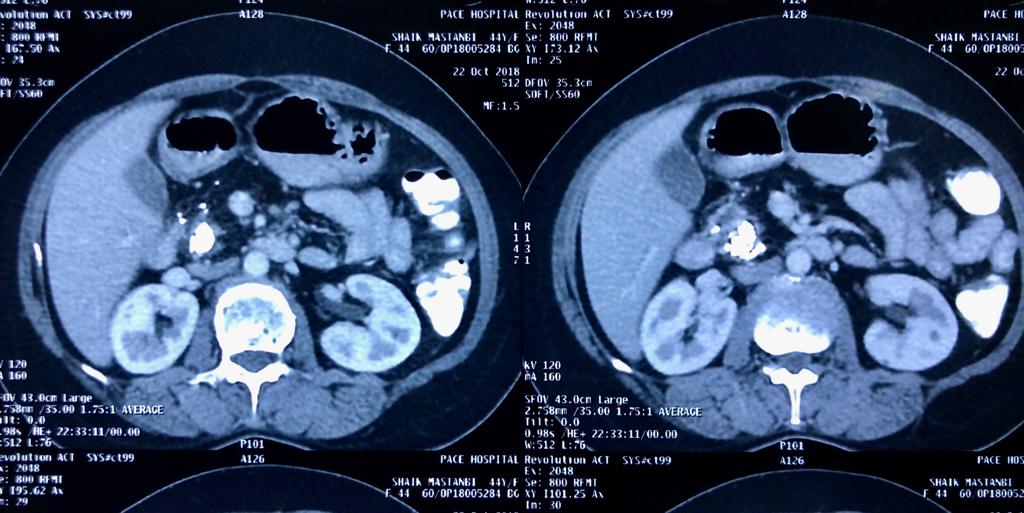
Total pancreaticoduodenectomy with splenectomy done for a 45 yr female with main duct
Total pancreaticoduodenectomy with splenectomy done for a 45 yr female with main duct IPMN with invasive mid-body cancer with bilateral polycystic kidneys. Her EUS, ERCP and fluid cytology , fluid CEA, serum CA19 -9 were all suggestive and a PET showed high uptake in her solid .She is doing well post op but planned for adjuvant CT Rt as had breached capsule and encased splenic vein. Total pancreaticoduodenectomy was frowned upon as a high morbidity surgery due to severe exocrine and endocrine insufficiency with brittle diabetes and ulcerogenicity due to complete loss of pancreatic bicarbonate secretion. But in recent years with easy availability of enzyme supplements, CGM (continuos glucose monitoring devices), insulin pens and long acting PPI the long term QoL of these patients is comparable with partial pancreatectomy patients
Misleading diagnosis - A 50 year old lady presented with a jaundice and pain abdomen
A 50 year old lady presented with a jaundice and pain abdomen. She was previously operated thrice for hydatid cyst of left liver over the past decade. Her CT showed a large recurrent multiloculated left lobe lesion along with a daughter cyst in the bile duct. We did not have the biopsy from previous surgery but with a diagnosis of recurrent hydatid cyst we performed a Left hepatectomy with CBD exploration of the daughter cyst. Post operative recovery was in eventful. Final histopathology was suggestive of biliary cystadenoma. Surprisingly the histology of the daughter cyst we removed from CBD also revealed biliary afenomatous hyperplasia. Biliary cystadenomas present with imaging suspiciously similar to complex hydatid / or even simple cyst. They have a high propensity for recurrence and even chance for malignant transformation . When suspected based on preoperative imaging or intraoperative frozen resection is the best approach.
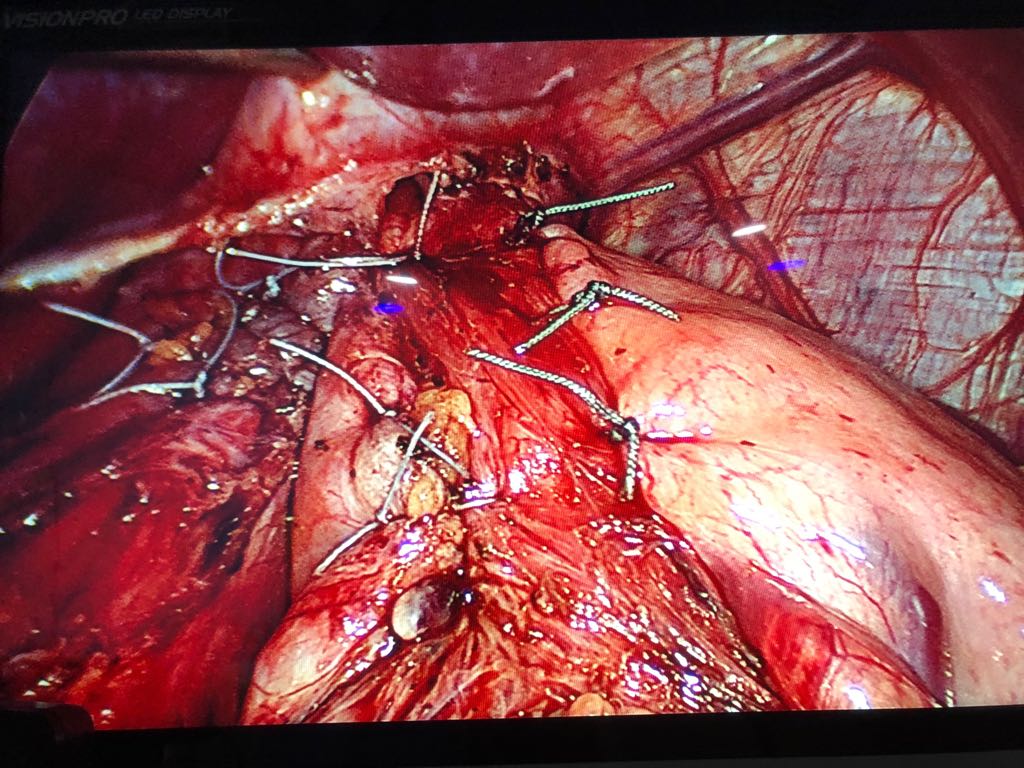
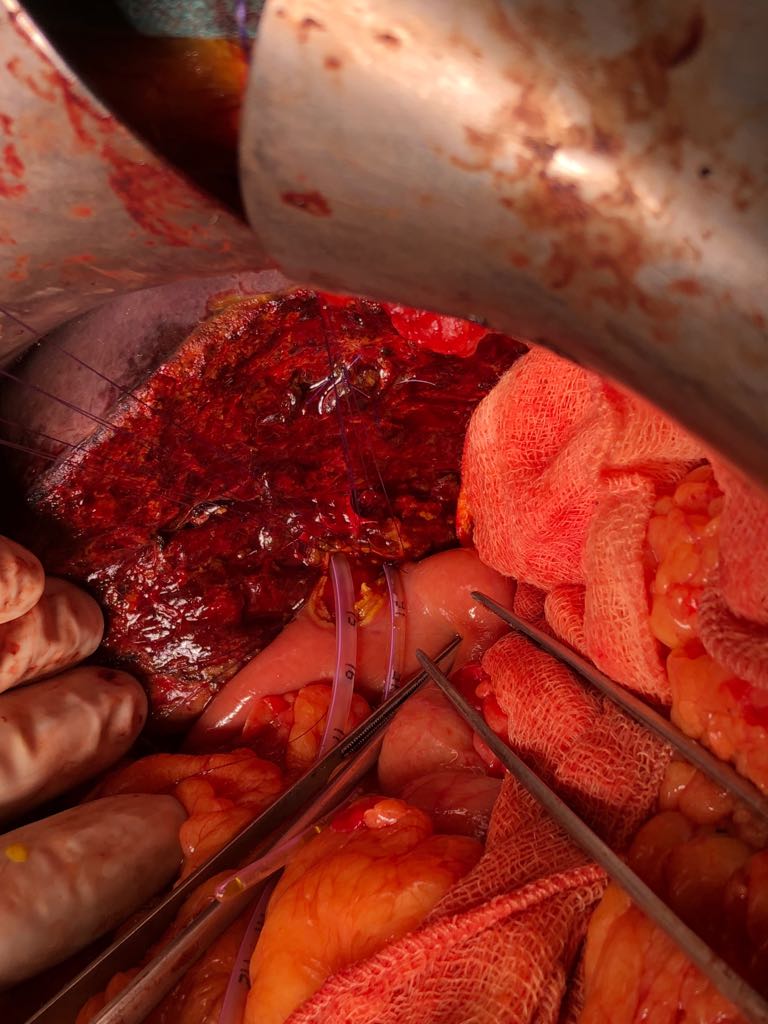
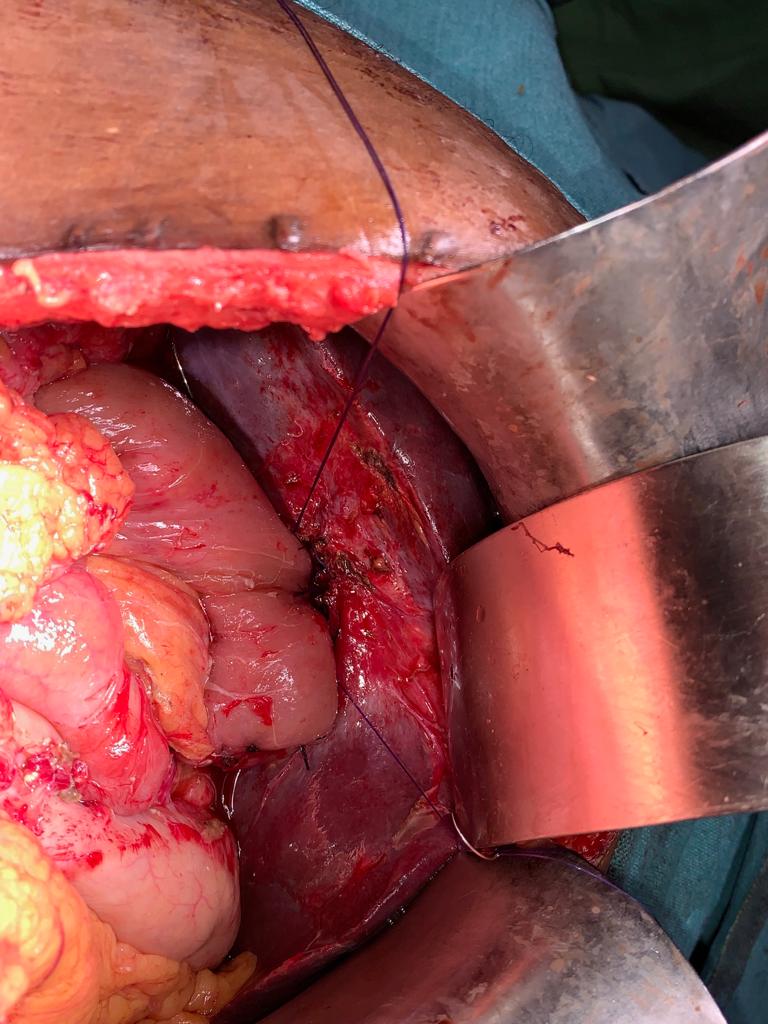
Patient with Type - 3 B hilar cholangiocarcinoma was admitted with obstructive jaundice
Patient with Type - 3 B hilar cholangiocarcinoma was admitted with obstructive jaundice. His bilirubin was 15 mg%. He had an attempted ERCP outside which failed so underwent a Rt PTBD. He was readmitted for surgery after 3 weeks with a bili of 2 mg%. At diagnostic lap he had evidence of PtBD catheter displacement with bile leak but as patient was not septic he went ahead with an extended left hepatectomy with enbloc caudate lobectomy and bile duct excision and right hepaticojejunostomy to separate Rt anterior and Rt posterior.
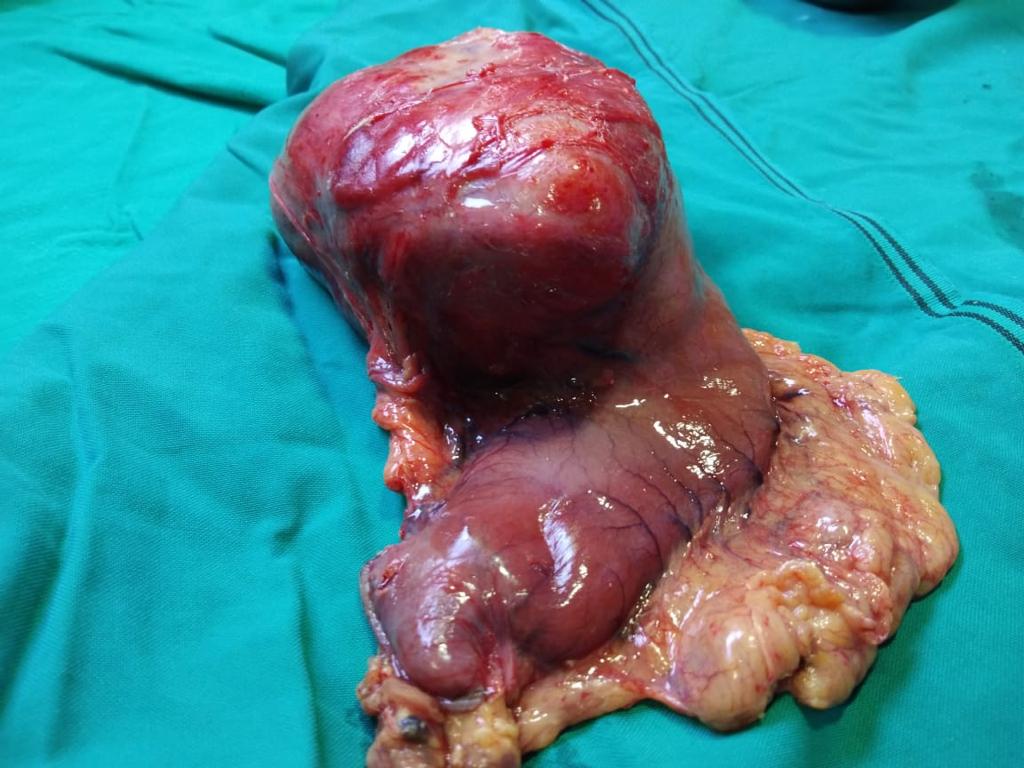
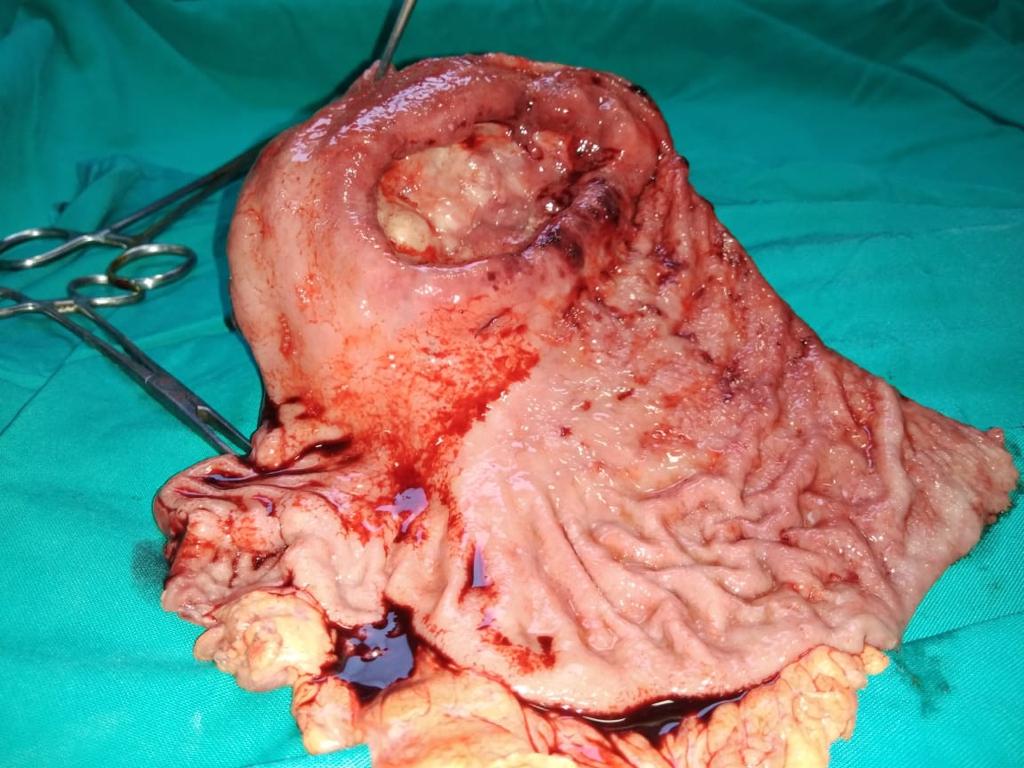
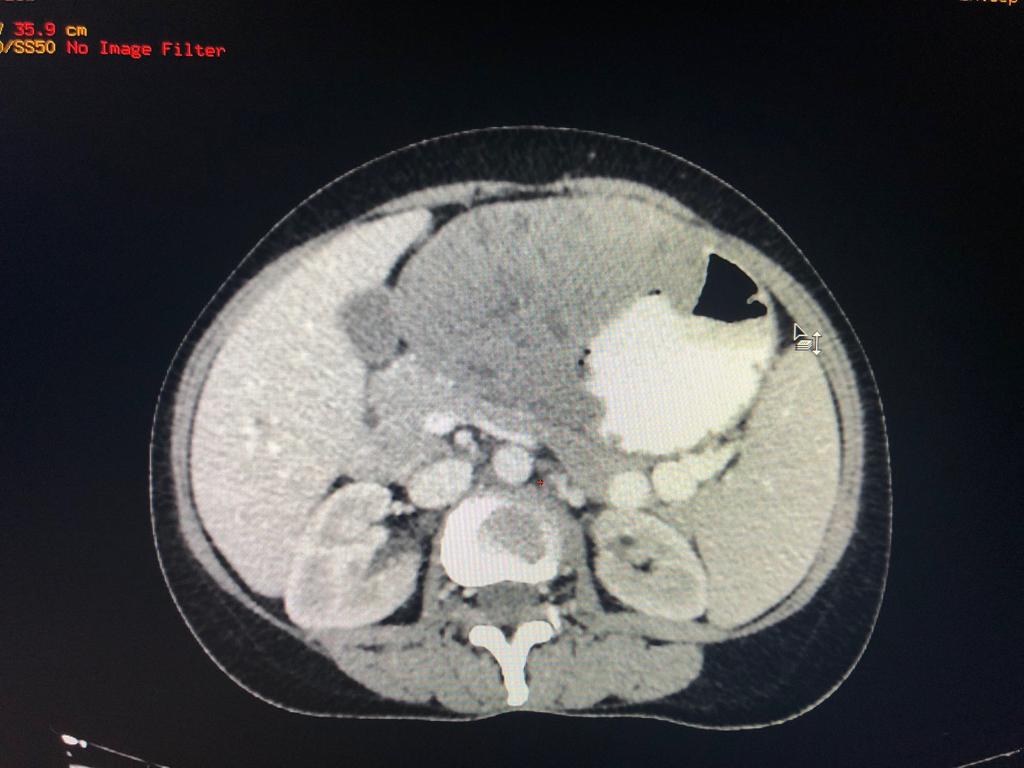
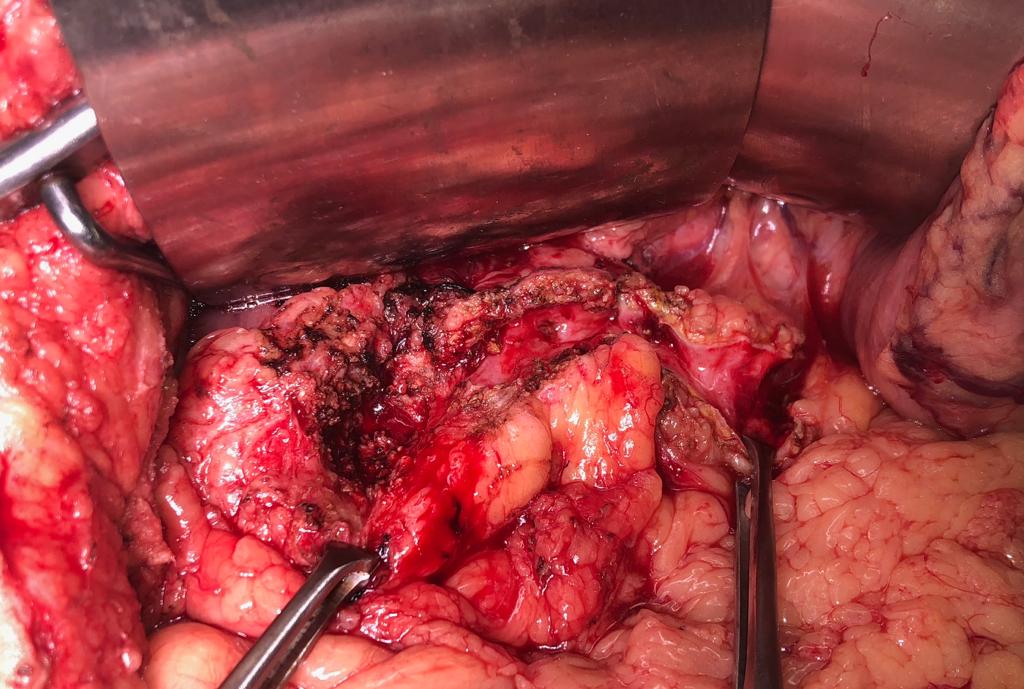
A rare case of gastric schwannoma masquerading as a GIST - 52 year old lady presented with massive GI bleed
A rare case of gastric schwannoma masquerading as a GIST. 52 year old lady presented with massive GI bleed and severe anemia Hb 5.0 gm. Her CT scan and endoscopy revealed a exophytic lesion 10 x 12 cmof gastric body with a ulceration in stomach. She underwent a lap assisted subtotal gastrectomy with a diagnosis of a GIST. Post operative immunohistochemistry revealed a gastric schwannoma. Gastric schwannoma is a very rare mesenchymal tumor arising from the nerve plexus of gastric wall . Unlike gastric GIST of this size >10 cm which are usually the rare malignant schwannoma are entirely benign with excellent long term prognosis.
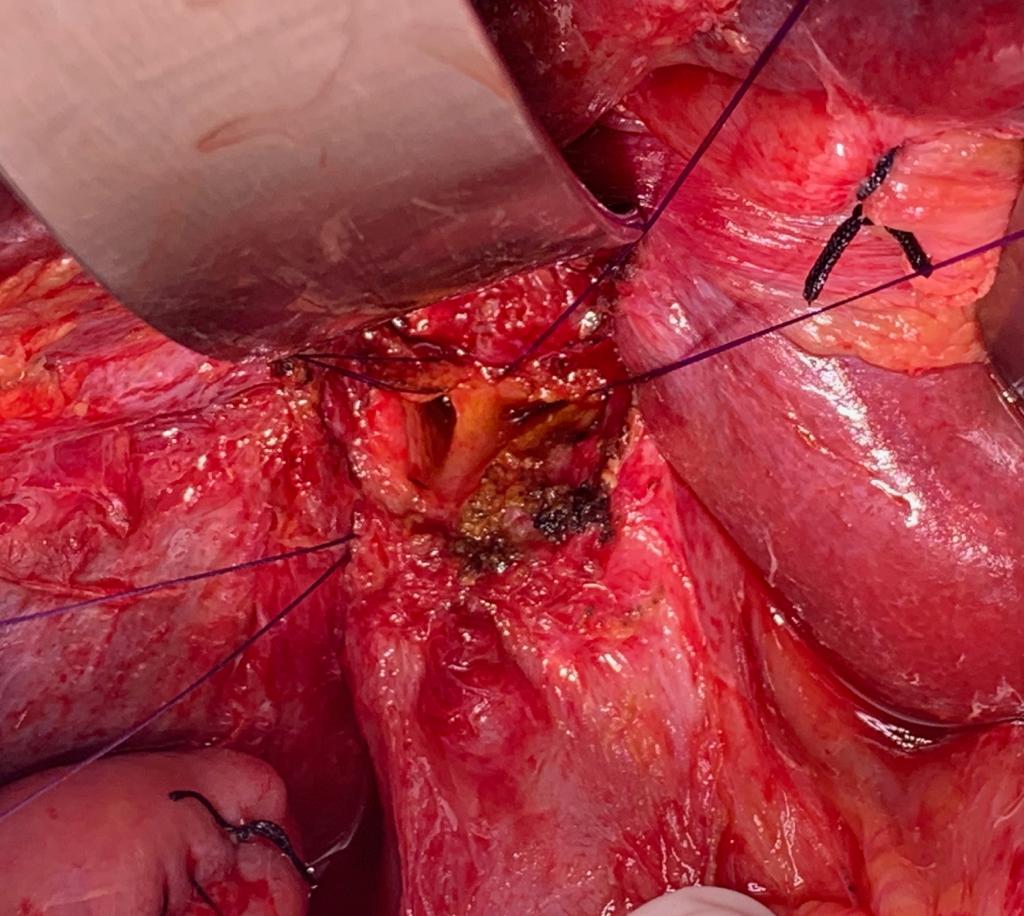
45 yrs old lady with classical presentation of tropical / idiopathic chronic calcific pancreatitis
45 year old lady with classical presentation of tropical /idiopathic chronic calcific pancreatitis presented with reccurant pain 6 months. Her CT scan showed dilated PD 12 mm with large calculi. CA 19-9 was normal, no evidence of biliary obstructuon,there was no evidence of a mass on CT scan. Underwent a freys LPJ with head coring (image 2,3) Day 3 the intraoperative biopsy came as adenocarcinoma. Normally with preoperative suspision intraoperative frozen would have been done but as it was unsuspected only biopsy was done. Once biopsy confirmed Patient was taken up for whipples procedure on D5 after a detailed discussion of risks and benefits and staging CT Chest. Unciante was compeltely removed baring SMA and sparing accesory right hepatic artery (images 4) Reconstruction was done by LPJ to remnant pancreas, HJ and antecolic GJ. This case highlights the high incidence of malignancy in 'tropical pancreatitis" and importance of sending head biopsies even in patients where malignancy is unsuspected preoperatively. Wether a frozen needs to be done routinely is debatable considering the costs and logistics.
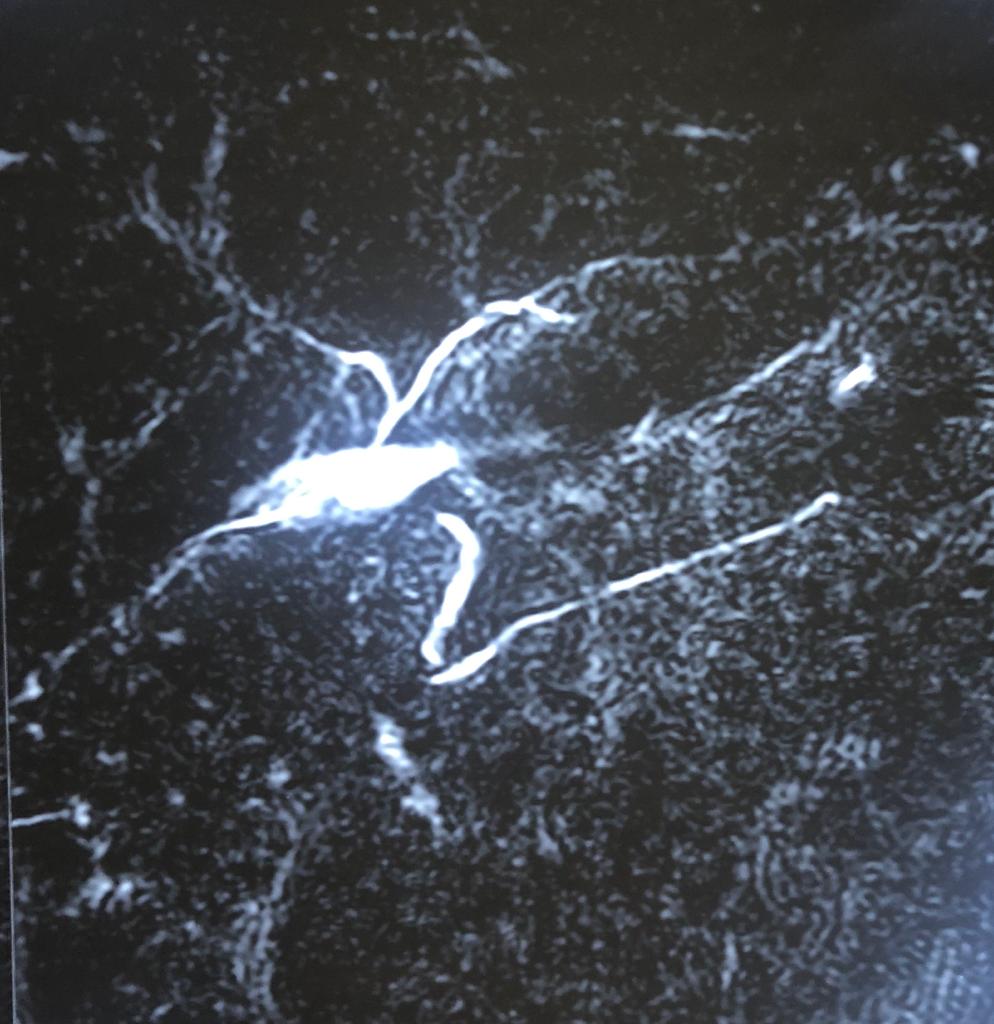
Recurrent pyogenic cholangitis (RPC) - 67 yr old Bangladeshi lady presented with recurrent episodes of jaundice, fever and pain for past 1 year
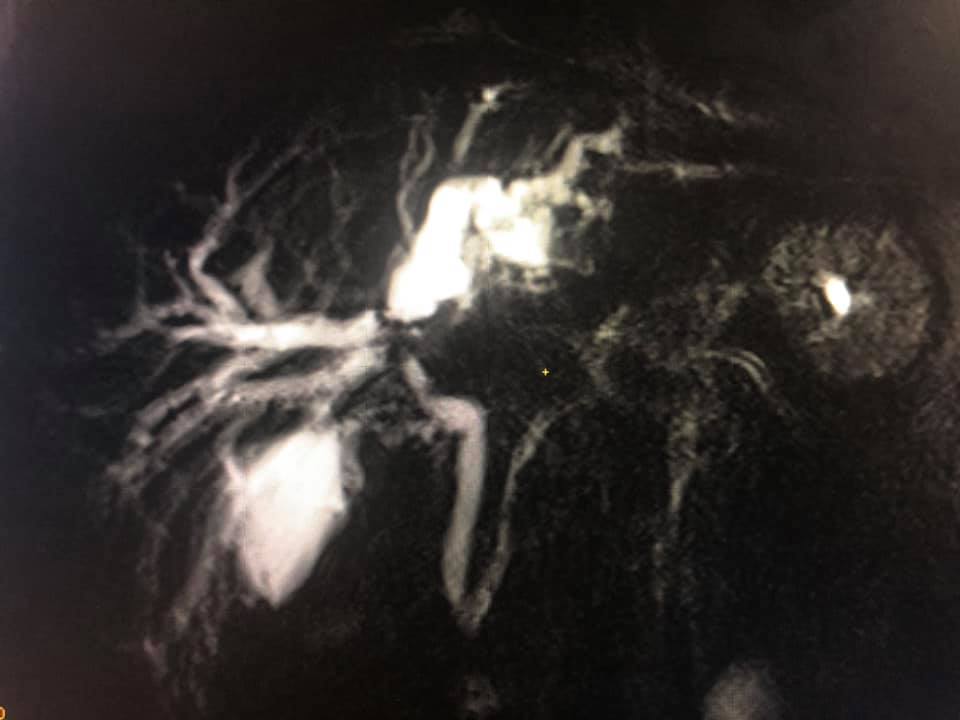
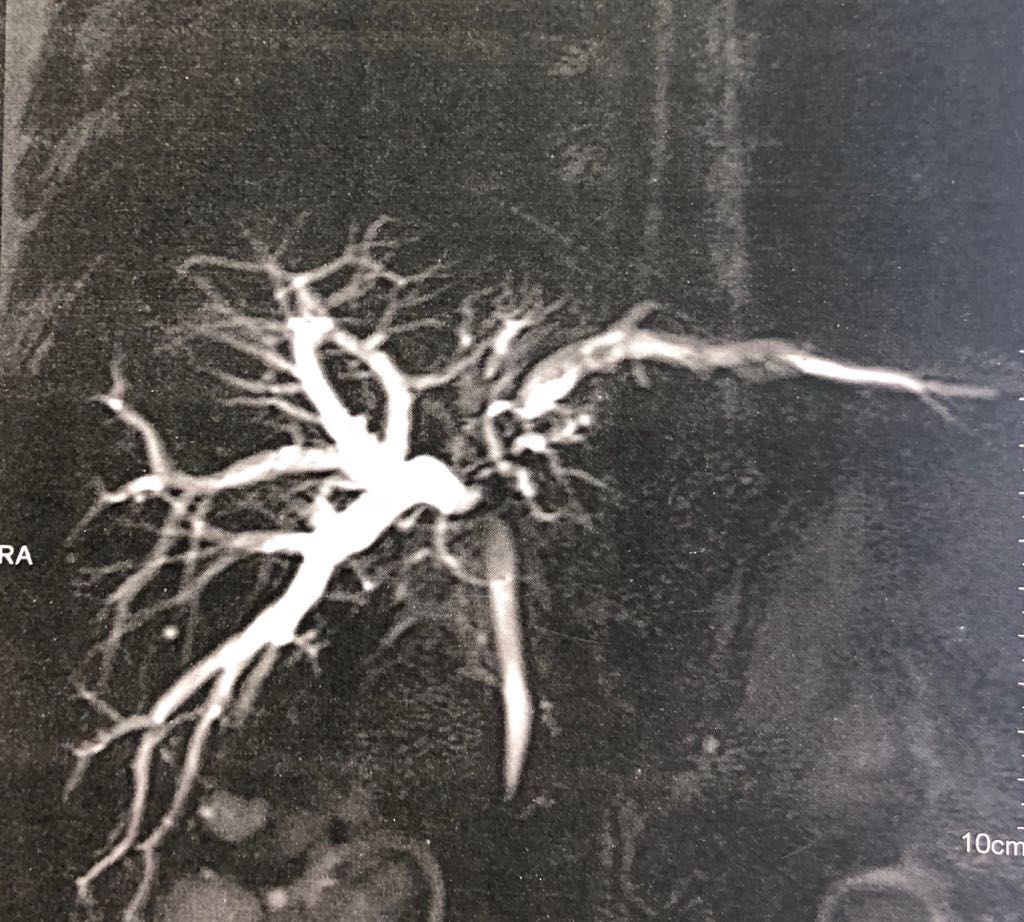
Interesting images: Recurrent pyogenic cholangitis (RPC) 67 yr old Bangladeshi lady presented with recurrent episodes of jaundice fever and pain for past 1 year. MRCP and CT scan showed left duct stricture with left sided IHBRD and CBD stones and atrophy of left lateral segment. As she 4 duct was also involved we did a left hepatectomy with hepaticoduodenostomy . Reccurant pyogenic cholangitis is a disease charecterised by multiple instances of biliary bacterial infection, hepatic abcesses , multiple stricturing of bile ducts with pigment stone formation in the intrahepatic and extrahepatic biliary tree. This can cause reccurant episodes of cholangitis, chronic illness ultimately leading to liver failure. It is more common in the far east population. Management includes long term biiary drainage with liver resections for segmental disease and liver transplantation in patients with end stage liver failure . The last CT scan shows another CT scan another similar patient with huge intrahepatic stones and abscesses managed successfully by surgery and long term PTBD.
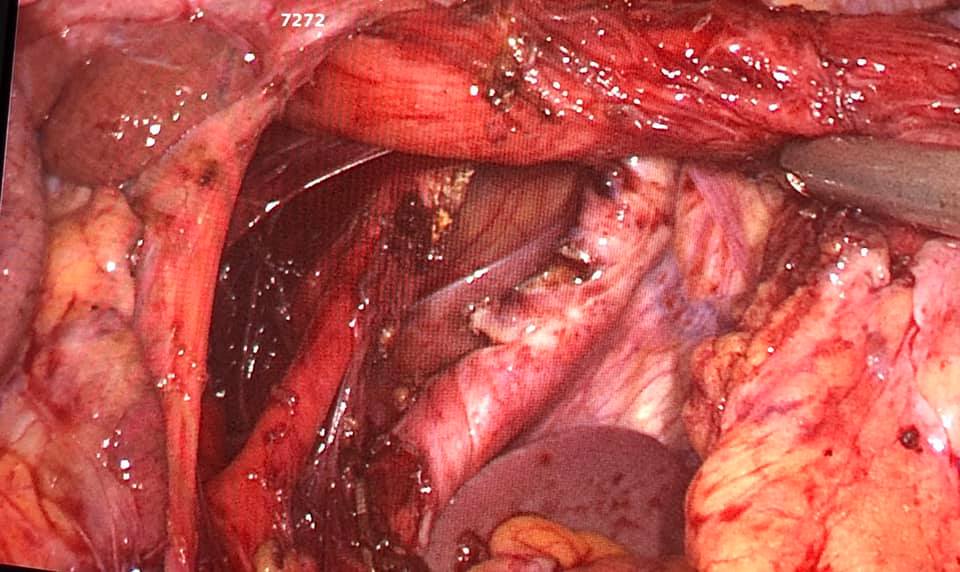
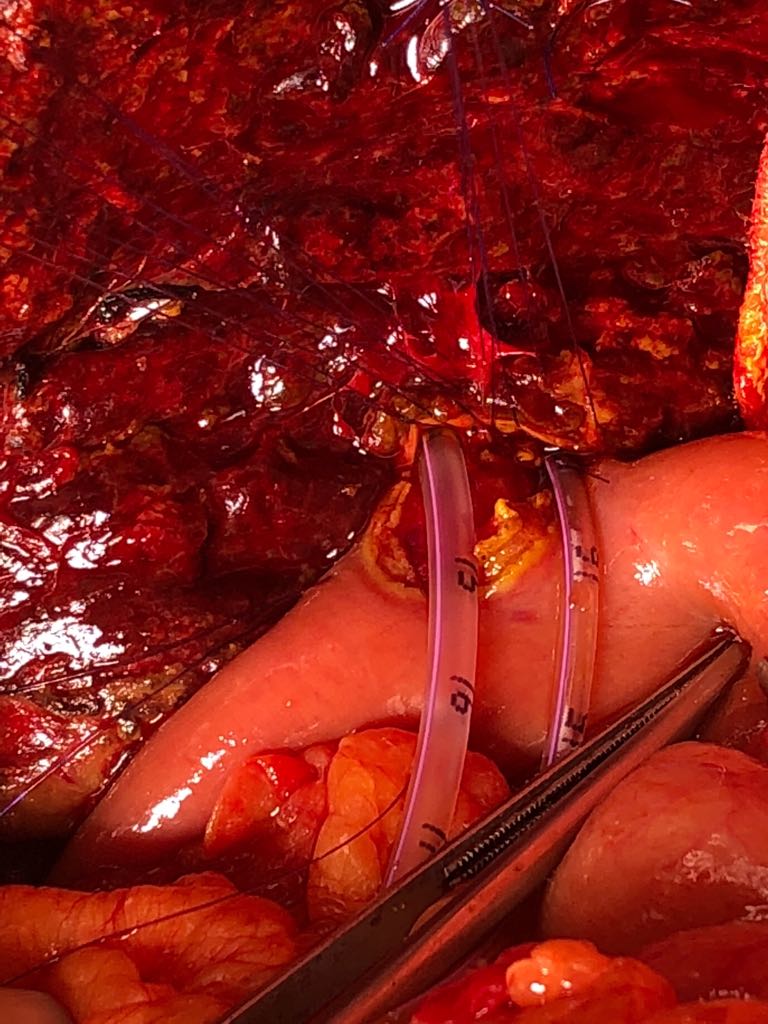
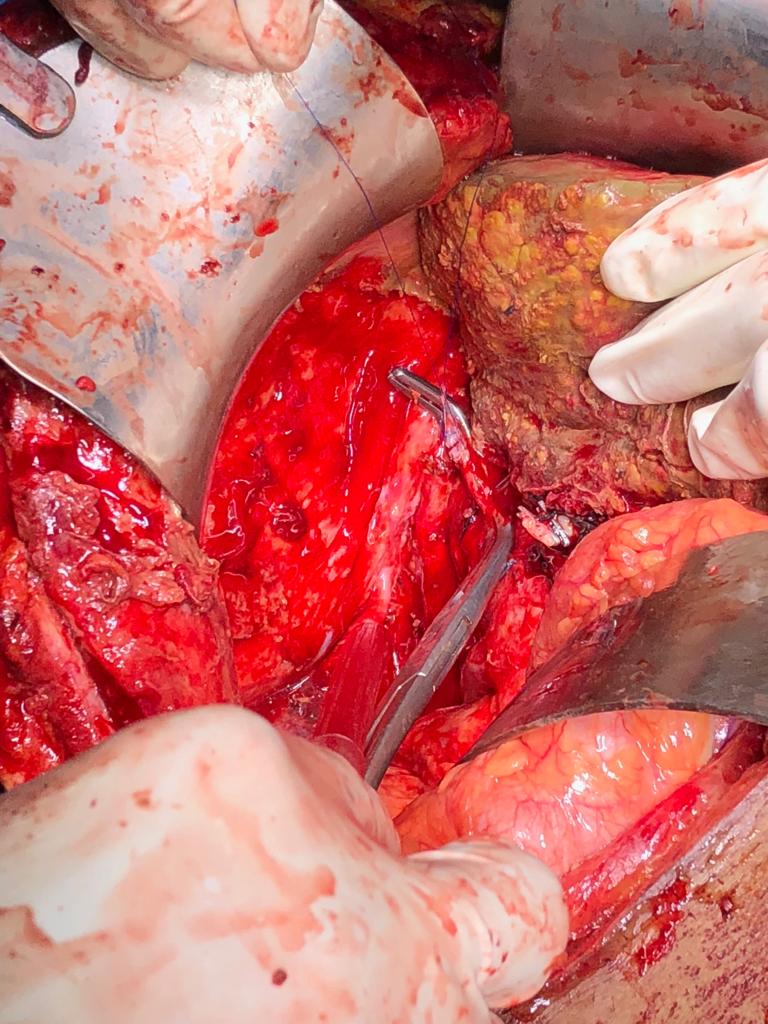
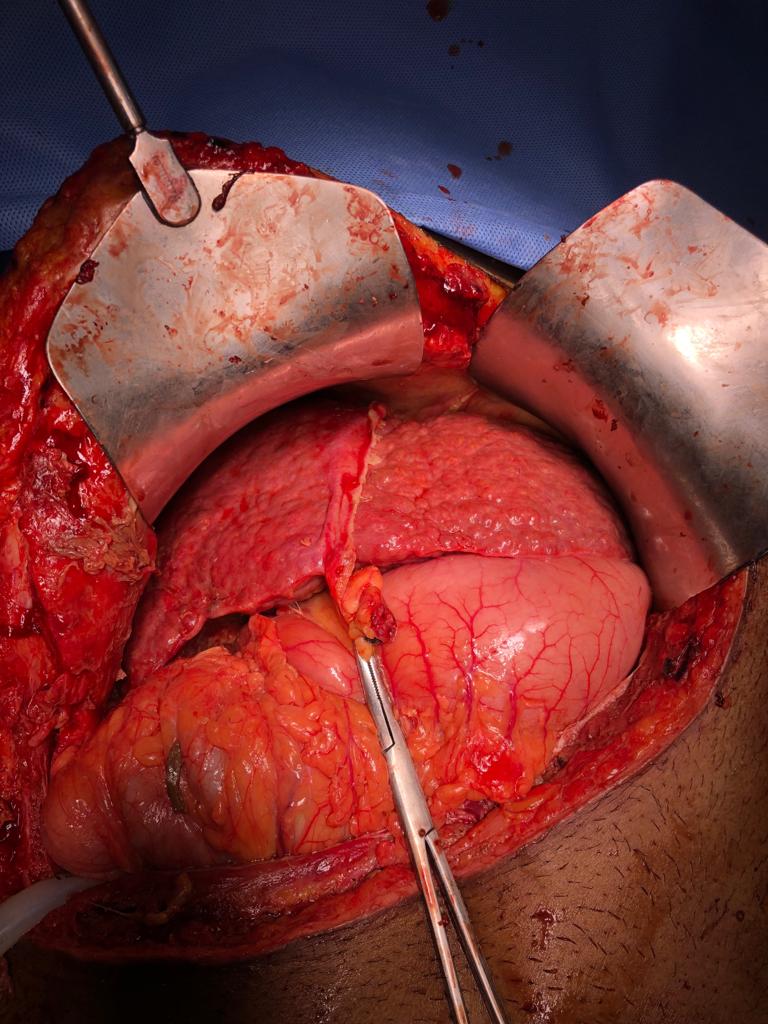
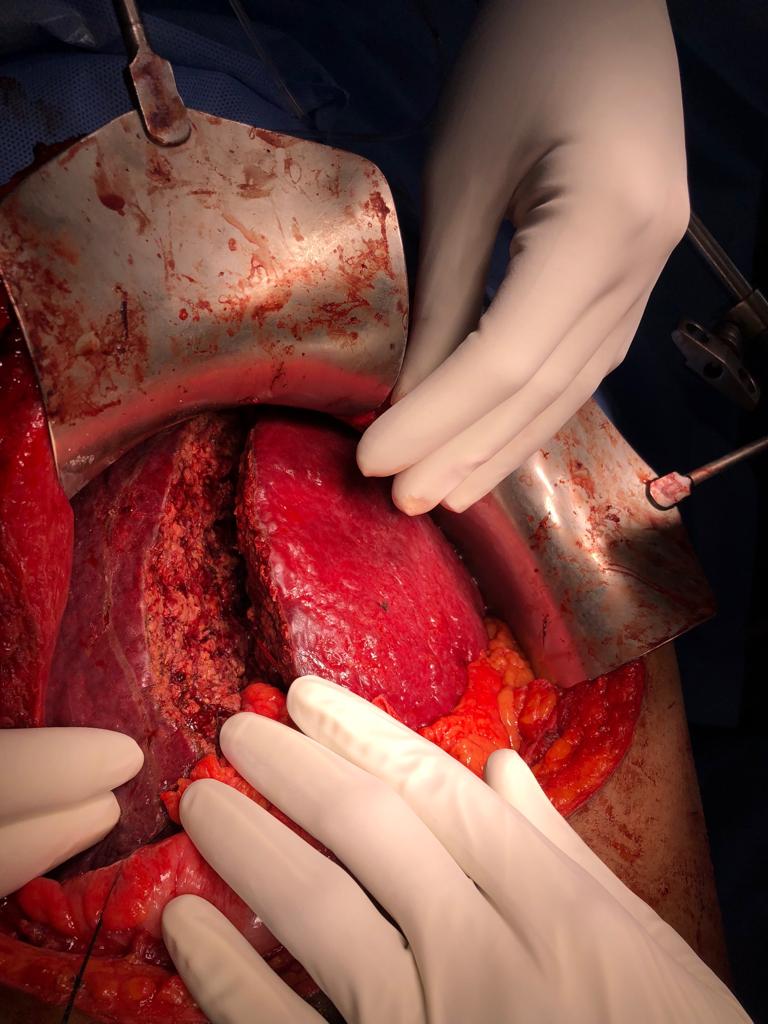
ALLPS hepatectomy 45 year old child’s A cirrhosis with normal LFT and no portal hypertension.
Interesting images October: ALLPS hepatectomy 45 year old child’s A cirrhosis with normal LFT and no portal hypertension. Planned for a right hepatectomy however intraoperative portal vein pressure was 13 mm ( preferably less than 8 mm) so altered strategy and did ALLPS (Associating Liver Partition and Portal vein Ligation for Staged hepatectomy) In ALLPS stage 1 we ligate portal vein, transect parenchyma fully by hanging and mobilise the right lobe fully. (Image 1,2 and 3) 7 to 10 days (8th day in our Pt)later depending on LFT trend we document the hypertrophy on CT scan and do the completion hepatectomy (pics . Although it has its own shortcomings in selected patients (like in our case ) it has been proven to achieve better degree of hypertrophy compared to Portal vein embolisation / portal vein ligation. Ideally useful for trisectionectomies.
Bariatric surgery on a 29 yrs old male with 220 kg weight, completely bedridden for past 3 months
After completing a successful gastric bypass on a 200 kg adult Pace team broke the barrier yet again in super obese by performing bariatric surgery on a 29 year old male with 220 kg weight (BMI 75 Kg/m2) completely bedridden for past 3 months and admitted with obesity related congestive cardiac failure and type 1 respiratory failure . optimisation of cardiac status with diuretics and BiPaP for 2 weeks,we performed a sleeve gastrectomy as a stage 1 procedure following which 2 months patient has now become 180 kg and is ambulant , off oxygen he is planned for a stage 2 gastric bypass after a couple of months. Bariatric surgery on these super obese is a challenging exercise not only for surgeons , but more importantly from a cardiac, Anesthetist, critical care and nursing rehabilitation point of view so Kudos to the Pace team for pulling it off safely and successfully in an extreme high risk Patient.
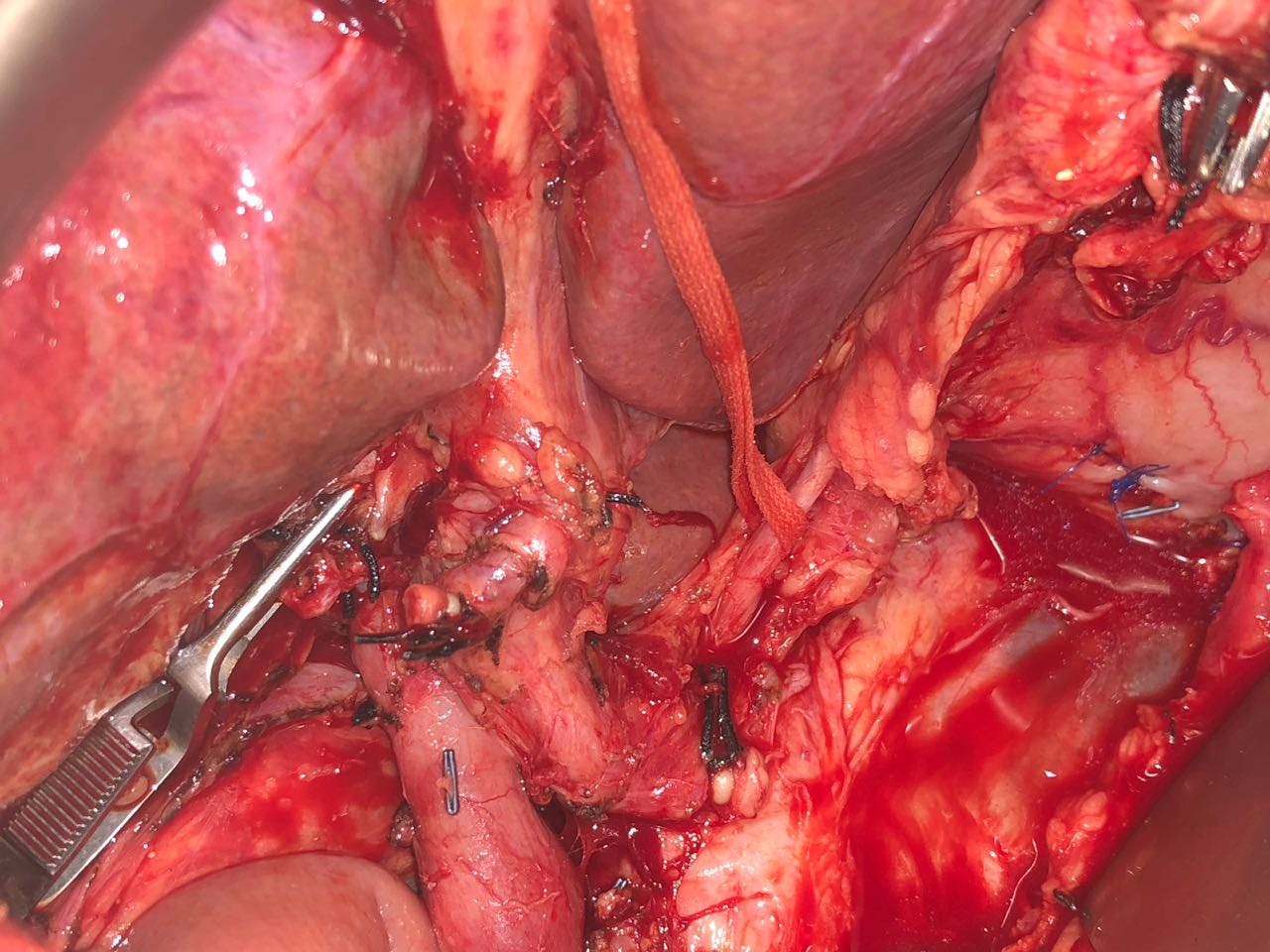
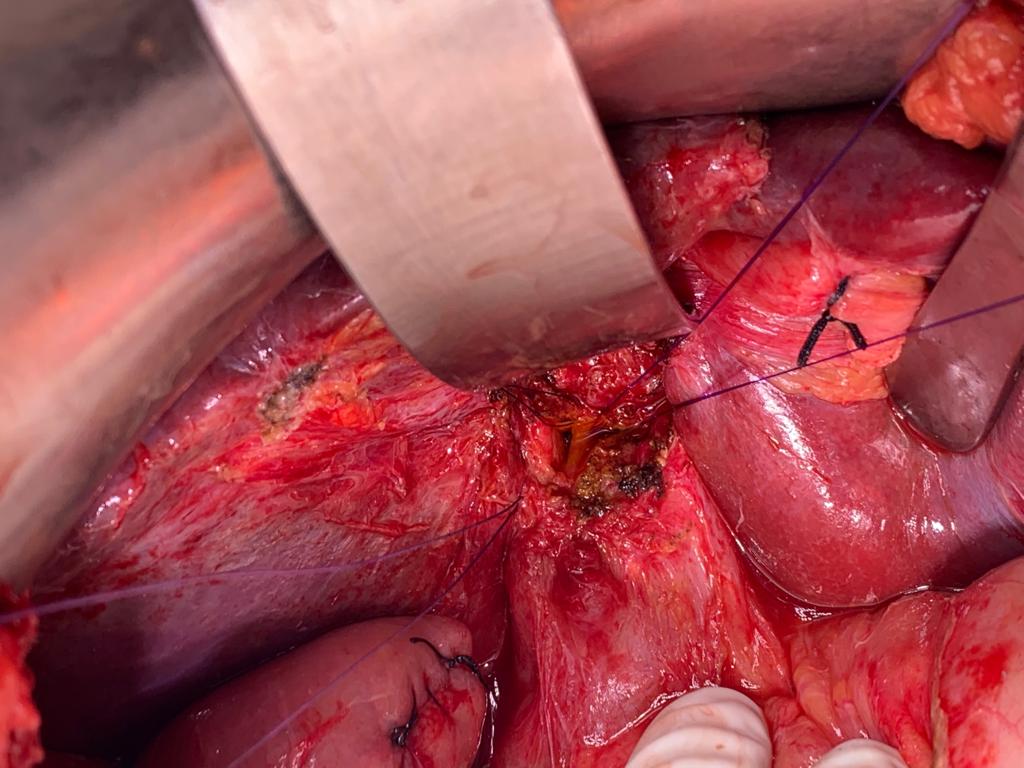
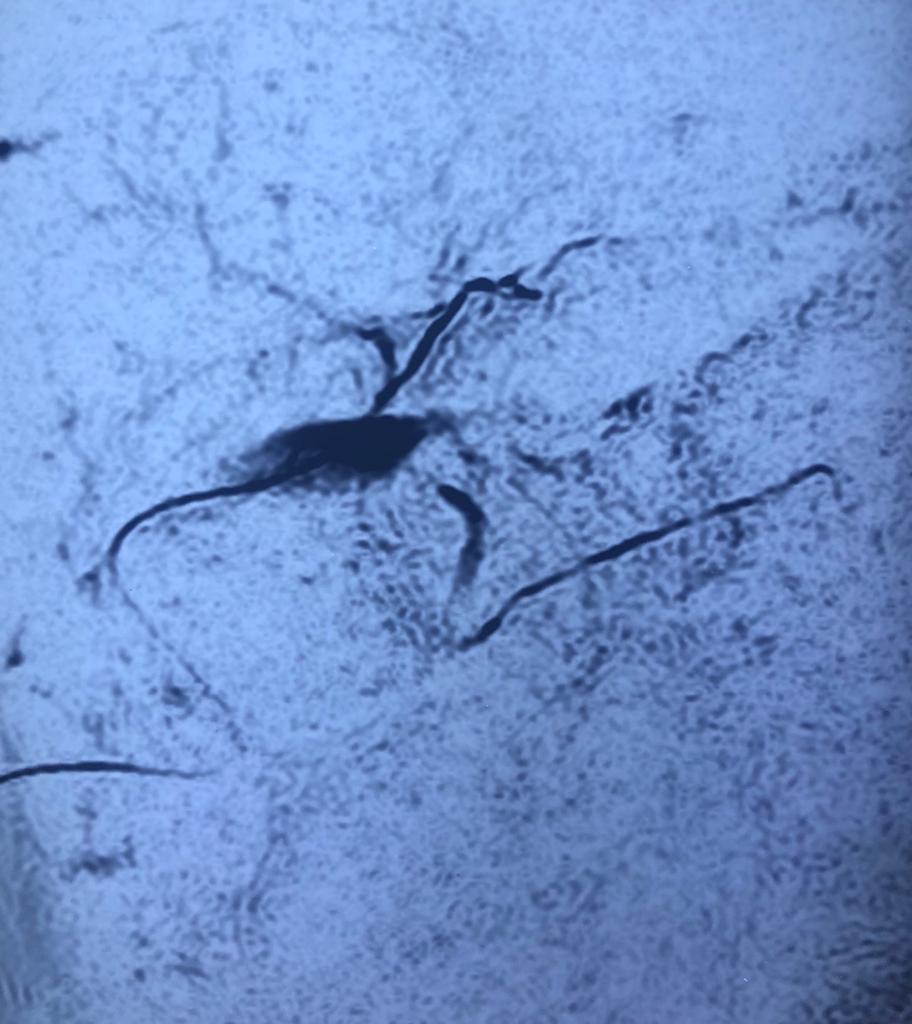
Case of post cholecystectomy biliary stricture with complete cutoff and external biliary fistula
Interesting images December: Case of post cholecystectomy biliary stricture with complete cutoff and external biliary fistula.Pt was 6 months after injury He was refused surgery elsewhere and told to wait for fistula to close as there was no biliary dilatation. After a complete cutoff the the external biliary fistula mostly closes over a period of time by fistulizing into duodenum. However after 2- 3 month waiting period presence of a persisting fistula there is no need to wait forever. By the hepp- couinad approach the anastomosis is a side to side anastomosis to the extrahepatic left duct which is abt 3-4 cm in length and as you can see in the images despite the apparent lack of dilatation on MRCP we could achieve a wide 3 cm side to side anastomosis to the confluence and left duct. The anastomosis is by a standard parachuting blumgart kelly technique. The lack of biliary dilatation is not a contraindication to reconstructive surgery after BDI after an adequate waiting period.
Awards & Recognition
Over the years, PACE Hospitals has been recognized by numerous organizations for its commitment to exceptional patient outcomes, leadership, innovations and excellence. PACE stands at par with most progressive and advanced standards of health and healthcare delivery and has received the 2015 awards for :-
Awarded Best Gastroenterology Hospitals in South India
Awarded Best Nephrology and Urology
Hospitals in South India
Hospitals in South India