Pancreatic Cancer Treatment in Hyderabad, India
At PACE Hospitals, team of best gastroenterologist doctors in Hyderabad are experienced in handling complex cases of pancreas related diseases and its complications such as acute pancreatitis, chronic pancreatitis, pancreatic cancer.
We have team of the best doctor for pancreatic cancer in India, they are having extensive experience in providing medical and surgical treatment for pancreatic cancer.
Request Appointment for Pancreatic Cancer Treatment
Pancreatic Cancer Treatment - appointment
Why Choose PACE Hospitals for Pancreatic Cancer Treatment?
250+ Patients treated from Pancreatic cancer
Equipped with Latest Technology, ERCP & SpyGlass Cholangioscopy System
Team of the Best Pancreatic Cancer Doctors with 35 + years of expertise
CGHS, ECHS and All insurance accepted for cashless treatment
Pancreatic Cancer Diagnosis
While there are various pancreatic cancer tests for the diagnosis, it must be understood that not all of them will be used for every suspected patient. The oncologist takes into consideration the following before selecting the appropriate tests for diagnosis:
- The presented signs and symptoms
- Age, family history and general health of the suspected patient
- The results of previous medical tests
- The type of cancer suspected
Before delving into the various diagnostic paths intended to establish and confirm pancreatic cancer in the patient, the oncologist / gastroenterologist considers the patient's history and physical examination. The physical examination for pancreatic cancer usually involves the presentation of:
- Abdominal pain (sometimes described as a “boring-like” pain).
- Weightloss with or without jaundice and sometimes accompanied by low back pain.
- The pain could increase during food consumption or lying flat on the back.
- The stool colour could be light coloured from the absence of bile.
- Jaundice (increased level of bilirubin in the blood resulting in yellow discolouration of skin and eyes), depression, pruritis (itchy skin).
- Hepatomegaly (abnormal enlargement of the liver) and splenomegaly (enlarged spleen)
The history and symptoms of pancreatic cancer noted by the doctor could direct the patient to refer for imaging tests for the detection and conformation of the tumour.
The various tests for the diagnosis of pancreatic cancer include:
- Hepatobiliary tests
- Serum amylase and/or lipase levels
- Tumour markers
- Germline mutations
- Molecular, or biomarker, testing of the tumour
- Computed tomography scanning
- Transcutaneous ultrasonography
- Endoscopic ultrasonography
- Magnetic resonance imaging
- Endoscopic retrograde cholangiopancreatography
- Positron emission tomography scanning
The aforementioned tests can be divided into haematological, genetic and imaging tests.
Pancreatic Cancer Stages
After an imaging modality has assisted in establishing a likely pancreatic cancer diagnosis, the next question is whether surgery can be performed to treat pancreatic cancer. Based on CT and/or EUS criteria, pancreatic masses are staged as resectable, unresectable, or borderline resectable. The TNM stages of pancreatic cancer include:
| Staging | T (tumour) | N (node) | M (metastasis) |
|---|---|---|---|
| Stage 0 | Tis | N0 | M0 |
| Stage IA | T1 | N0 | M0 |
| Stage IB | T2 | N0 | M0 |
| Stage IIA | T3 | N0 | M0 |
| Stage IIB | T1-3 | N1 | M0 |
| Stage III | T4 | Any N | M0 |
| Stage IV | Any T | Any N | M1 |
Differential diagnosis of pancreatic cancer
Before the attempt of imaging and biopsy tests could be made, the differential diagnosis (symptoms closely resembling) of pancreatic cancer could include:
- Acute pancreatitis
- Chronic pancreatitis
- Cholangitis
- Cholecystitis
- Choledochal cyst
- Peptic ulcer disease
- Cholangiocarcinoma
- Stomach cancer
Considerations and goals of an oncologist before planning a pancreatic cancer treatment
Shared decision-making: Before the oncologist even considers treating the patient, the concept of shared decision-making must be introduced to the patient. Shared decision-making includes carefully and diligently explaining all the pancreatic cancer treatment options available to the patient and their caregivers. In case of any unclear issues, all must be resolved.
Once the pancreatic cancer treatment options are well explained, the patients, the caregivers and the team of doctors sits and discuss the best treatment option that fits the goals of care. Shared decision-making is the discussion among clinicians and patients which involves the choosing of optimal decision when exposed with the best available evidence to achieve informed preferences.
The doctor must emphasise the possibility of biliary tract obstruction (and the subsequent risk for sepsis from the biliary tree) during the staging of pancreatic cancer. The proposal for a stent, which can be placed to relieve jaundice and pruritus, must be dealt with caution as:
- Stent blockage and stent-induced pancreatitis can occur.
- The occurrence of infection due to stent could be possible, but antibiotics can help.
Nevertheless, it must be understood that in the case of early surgical intervention, the doctors may not think placing the stent could be necessary. Patients with pancreatic cancer are often hypercoagulable (increased affinity to form blood clots within a blood vessel) and frequently have thrombophlebitis (blood clots blocking veins, usually in the legs) as well as deep vein thrombosis with pulmonary emboli (a frequent cause of death).
Therefore, apart from pancreatic cancer treatment medications and techniques, the patient must undergo prescribed appropriate examinations to understand the status of thromboses. Analysing the data, the routine workup can be modified to implement appropriate management.
Pancreatic cancer is more likely to be effectively treated if found early. However, there are also medicines (palliative care for pancreatic cancer patients) that can help individuals with advanced pancreatic cancer control their disease and live longer and more comfortably.
Pancreatic Cancer Treatment
Treating pancreatic cancer symptoms and side effects is crucial to cancer care. The pancreatic cancer treatment options and recommendations depend on several criteria, including the type and stage of pancreatic cancer, the patient's preferences and overall health, and the possibility of adverse effects. The most prevalent therapies for pancreatic cancer are:
- Surgery
- Radiation Therapy
- Chemotherapy
- Targeted Therapy
- Immunotherapy
Pancreatic cancer treatment involves a multidisciplinary team of doctors creating a tailor-made pancreatic cancer treatment and overall care plan by combining various supportive and curative therapies. The interdisciplinary team involves multiple healthcare professionals, such as:
- Oncologists
- Physician assistants
- Nurse practitioners
- Oncology nurses
- Patient navigators
- Social workers
- Clinical pharmacists
- Patient counsellors
- Dietitians
The types of treatment for pancreatic cancer
- Surgery - Whipple Procedure (Pancreaticoduodenectomy), Central pancreatectomy, Distal pancreatectomy, Total pancreatectomy
- Radiation therapy - External beam radiation therapy such as Traditional radiation therapy, Stereotactic body radiation (SBRT) or cyberknife and Proton beam therapy; Other types of radiation therapy
- Therapies using medications - Chemotherapy such as 1st line therapy, 2nd line therapy and Off label; Targeted therapy, Immunotherapy
- Palliative therapy - Palliative chemotherapy, Relieving bile duct or small intestine blockage, Improving digestion and appetite, Controlling diabetes, Relieving pain and other side effects
Pancreatic cancer surgery
If surgery is being considered, a consultation with an oncologic surgeon must be done soon as possible, as it could decide the application or abandonment of the stent.
Depending on the site and size of the pancreatic tumour, surgery for pancreatic cancer may involve the removal of the entire pancreas or a portion of it. Most pancreatic cancers are detected after the disease has already spread, making surgery an option for just about 20% of patients. It is usual to practise to obtain a second opinion from a skilled surgical oncologist for diseases such as pancreatic cancer that are less prevalent.
Strategies for Resection
The types of pancreatic cancer surgeries include:
- Whipple procedure (pancreaticoduodenectomy)
- Central pancreatectomy
- Distal pancreatectomy
- Total pancreatectomy
The search for distant metastases is the first stage of the operation. The liver and peritoneal surfaces are checked for pancreatic cancer implants.
Whipple procedure (pancreaticoduodenectomy) - If the pancreatic cancer is seen only in the head of the pancreas, this primary pancreatic cancer treatment is performed. The surgeon separates the head of the pancreas, the duodenum (the starting part of the small intestine), the bile duct, the stomach, or sometimes just a portion of the stomach. Whipple technique variants include:
- standard
- pylorus-preserving
- radical pancreaticoduodenectomy
Central pancreatectomy: A conservative procedure that preserves the spleen and pancreatic parenchyma and is done as an alternative to distal pancreatectomies. Compared to a distal pancreatectomy, a central pancreatectomy preserves endocrine and exocrine pancreatic function better, but the primary disadvantages of this procedure include significant morbidity, especially in elderly and obese diabetic patients.
Distal pancreatectomy: the surgeon removes the pancreatic tail and body, as well as the spleen if the pancreatic cancer is located on the left side of the pancreatic tail.
Total pancreatectomy: is done if pancreatic cancer has expanded to multiple sections of the pancreas or has spread across the pancreas. A complete pancreas, a portion of the small intestine, a part of the stomach, the common bile duct, the gallbladder, and the spleen are removed during a total pancreatectomy. Lesions in the body and tail require distal pancreatectomy and occasionally central pancreatectomy.
Pancreatic cancer symptoms that diminish a patient's quality of life are frequently treated with palliative operations and supportive surgeries. To reduce jaundice, nausea and vomiting, and tumor-related pain, palliative therapies and surgeries may include bypass operations, stent placements, and nerve blocks.
Radiation therapy for pancreatic cancer
Utilising high-energy x-rays or other particles, a radiation oncologist performs radiation treatment to destroy pancreatic cancer cells. External-beam radiation therapy is the most frequent form of radiation therapy, in which radiation is delivered from a machine outside the body.
External-beam radiation therapy for pancreatic cancer is the most common form of radiation therapy. Radiation therapy can be administered in a variety of ways:
- Traditional radiation therapy (also known as standard or conventional fraction radiation therapy for pancreatic cancer or simply radiation for pancreatic cancer): consists of daily treatments of reduced radiation doses per fraction or day administered over 5-6 weeks.
- Stereotactic body radiation (cyberknife): shorter, higher-dose radiation therapy treatments administered for five days. This radiation therapy can deliver more localised care in fewer sessions but is less effective than conventional radiation therapy, which may not be suitable for some patients.
- Proton beam therapy: This proton beam therapy for pancreatic cancer is actually a radiation therapy which employs protons instead of x-rays for treatment as protons with a high energy level can damage pancreatic cancer cells. Additionally, it reduces the quantity of healthy tissue exposed to radiation. Proton beam therapy may be administered for a conventional or shorter duration.
Radiosensitisation: The process of administering chemotherapy with radiation therapy amplifies the effects of radiation therapy, thus aiding in tumour shrinkage sufficient for surgical removal.
Side effects of radiation therapy could include fatigue, moderate skin responses, nausea, upset stomach, and loose stools, which usually disappear after treatment.
Chemotherapy for pancreatic cancer
Chemotherapy for pancreatic cancer uses either a drug or a combination of medications given in scheduled cycles to destroy pancreatic cancer cells, usually by keeping the pancreatic cancer cells from growing, multiplying, and making more cells.
The combination is based on the following:
- specific diagnosis
- stage of disease
- treatment history
- genetic makeup
- side effects
- the overall health of the patient
The chemotherapy could be:
First-line chemotherapy: Given to patients with either locally advanced or metastatic pancreatic cancer without any prior treatment.
Second-line chemotherapy: patients can be given a second-line and third-line treatment showing considerable promise when refractory phase or primary resistance or secondary or acquired resistance is encountered.
- Refractory cancer: 1st line treatment does not work or stops working to control pancreatic cancer growth, or the patient does not show any response
- Primary resistance: 1st-line treatment does not work at all
- Secondary or acquired resistance: Treatment may work well for a while and then stop being effective later, which is sometimes called
Off-label use: The administration of a medicine for a condition not stated on its Food and Drug Administration (FDA) approved label is its off-label use. This indicates:
- The medicine is not being administered for the condition approved by FDA.
- The medicine being administered is contrary to the label's directions.
Off-label medicine is only recommended when there is solid evidence that it may be effective for an illness not listed on the label. This evidence may include previously published studies, promising outcomes from ongoing research, or results from tumour biomarker testing, all of which indicate that the treatment may be effective.
Targeted therapy for pancreatic cancer
A treatment targeted specific genes, proteins, or the tissue environment that promotes the growth and survival rate of pancreatic cancer by inhibiting the growth and spread of pancreatic cancer cells while minimising damage to healthy cells.
Every pancreatic cancer doesn't need to have the same targets. The doctor performs tests to determine the genes, proteins, and other variables from the tumour to provide the most effective treatment.
Side effects vary for each drug. The general side effects could include skin rash like acne, diarrhoea, loss of appetite, fatigue, taste changes, etc.
Immunotherapy for pancreatic cancer (biological therapy)
This therapy is intended to strengthen the body's natural defences against cancer by endogenous substances (produced within the body) or in a laboratory to enhance, target, or restore immune function.
Immune checkpoint inhibitors, such as anti-PD-1 antibodies, can treat pancreatic cancer with high microsatellite instability (MSI-H) or deficient mismatch repair (dMMR). About 1-1.5% of pancreatic tumours are associated with high MSI-H levels.
Currently, immunotherapy is now being researched in conjunction with chemotherapy. Different forms of immunotherapy may result in distinct adverse effects.
Palliative Therapy for Pancreatic Cancer
Palliative care (supportive care) focuses on enhancing the quality of life of patients undergoing treatment by addressing their non-medical needs and controlling their pancreatic cancer symptoms. Patients who receive palliative care in conjunction with pancreatic cancer therapy frequently report less severe pancreatic cancer symptoms, a higher quality of life, and greater treatment satisfaction.
Hospice care shouldn't be confused with palliative care, administered when a cure is unlikely or when the patient is in their final months of life. The various palliative therapies include:
Palliative chemotherapy: Any chemotherapy regimen may alleviate pancreatic cancer symptoms, such as reducing pain, boosting a patient's energy and appetite, and halting or stymieing weight loss. This method is utilised when pancreatic cancer has spread and cannot be cured, but chemotherapy can alleviate pancreatic cancer symptoms. Palliative chemotherapy discussion between the patient and the physician is crucial as the advantages against the potential adverse effects can be assessed.
Therapy for improving digestion and appetite: In the case of a non-functioning pancreas partially or destroyed, a particular diet, medicines, and specially prescribed enzymes can be given, which may improve digestion. A dietitian or nutritionist can be consulted by patients suffering from weight loss and poor appetite. Daily exercise is strongly suggested, and the doctor can develop an effective routine for Improving digestion and appetite.
Therapy for controlling diabetes: Insulin is typically prescribed to pancreatic cancer patients as endogenous production (production within the body) is hampered. This is more common after a total pancreatectomy.
Therapy for relieving pain and other side effects: Opioid analgesics are frequently prescribed for pain relief. Specialised nerve blocks (anaesthetic and/or anti-inflammatory injection targeted for a certain nerve or group of nerves to treat pain, providing long-lasting pain relief) could also be administered.
- A celiac plexus block: is a form of nerve block that relieves abdominal or back discomfort.
- Percutaneous (through the skin) or endoscopic ultrasonography can perform a nerve block.
- Radiation therapy is occasionally utilised to alleviate pain depending on the tumour's location.
Pancreatic Cancer Treatment by Stages
Potentially curable pancreatic cancer (resectable and borderline resectable pancreatic cancer)
- Surgery
- Treatment before surgery, also called neoadjuvant therapy
- Treatment after surgery, also called adjuvant therapy
Locally advanced pancreatic cancer
- 1st line therapy
- 2nd line therapy
Metastatic pancreatic cancer
- 1st line therapy - Maintenance therapy
- 2nd line therapy
Pancreatic Cancer Treatment Cost in Hyderabad, India
The cost of Pancreatic Cancer Treatment in Hyderabad generally ranges from ₹2,000 to ₹6,50,000 and above (approx. US $24 – US $7,800).
The exact cost depends on the stage of cancer, type of treatment (surgery, chemotherapy, radiotherapy, targeted therapy), diagnostic tests (CT, MRI, PET-CT, biopsy), specialist consultation, hospitalization, and hospital facilities including cashless insurance, TPA corporate tie-ups, and complete support with medical insurance wherever applicable.
Cost Breakdown According to Type of Pancreatic Cancer Treatment
- Oncologist / Gastro Surgeon Consultation – ₹1,000 – ₹2,000 (US $12 – US $24)
- Blood Tests (CBC, LFT, Tumor Markers CA 19-9) – ₹1,000 – ₹3,000 (US $12 – US $36)
- Ultrasound Abdomen – ₹1,200 – ₹2,500 (US $14 – US $30)
- Contrast CT Abdomen – ₹4,500 – ₹9,000 (US $54 – US $108)
- MRI Abdomen – ₹4,500 – ₹10,000 (US $54 – US $120)
- PET-CT Scan – ₹18,000 – ₹32,000 (US $215 – US $385)
- Endoscopic Ultrasound (EUS) – ₹8,500 – ₹18,000 (US $100 – US $215)
- Biopsy (EUS-guided or CT-guided) – ₹7,000 – ₹15,000 (US $85 – US $180)
- Chemotherapy (Per Cycle) – ₹12,000 – ₹48,000 (US $145 – US $575)
- Radiation Therapy (Complete Course) – ₹40,000 – ₹1,20,000 (US $480 – US $1,440)
- Targeted Therapy / Immunotherapy – ₹25,000 – ₹1,50,000 (US $300 – US $1,800)
- Whipple Surgery (Pancreaticoduodenectomy) – ₹1,80,000 – ₹3,50,000 (US $2,160 – US $4,200)
- Palliative Care & Pain Management – ₹5,000 – ₹25,000 (US $60 – US $300)
- Hospitalization (3–7 Days) – ₹12,000 – ₹45,000 (US $145 – US $540)
Frequently Asked Questions (FAQs) on Pancreatic Cancer
Is pancreatic cancer rare?
No. Pancreatic cancer is not rare.
Pancreatic cancer is the 7th greatest cause of cancer-related death in developed nations. According to GLOBOCAN 2018 estimates, pancreatic cancer was the 11th most prevalent cancer in the world in 2018, with 4.5% of all cancer-related fatalities. The incidence and death of pancreatic cancer increase with age and are slightly more prevalent among men than women.
Which Is the best hospital for Pancreatic Cancer Treatment in Hyderabad, India?
PACE Hospitals, Hyderabad, is widely recognized as one of the most trusted centres for pancreatic cancer diagnosis and treatment, offering advanced evaluation and multi-disciplinary cancer care.
We handle complicated cases by experienced team members including medical oncologists, surgical gastroenterologists, hepatobiliary specialists, interventional radiologists, and critical care experts, providing comprehensive management for:
- Early-stage pancreatic tumors
- Locally advanced pancreatic cancer
- Metastatic pancreatic cancer
- Pancreatic cystic neoplasms
- Pancreatic neuroendocrine tumors
- Bile duct obstruction and jaundice related to tumors
- Cancer-associated pain or weight loss
With PET-CT, EUS, CT/MRI, advanced biopsy techniques, Whipple surgery, chemotherapy, radiation therapy, supportive care, and 24/7 critical care backup, PACE Hospitals ensures precise diagnosis, timely treatment, and patient-centric cancer care — supported by cashless insurance, TPA tie-ups, and end-to-end documentation assistance.
What is the difference between pancreatitis and pancreatic cancer?
Pancreatitis and pancreatic cancer are afflictions of the pancreas, but there are vast differences between them. Pancreatitis is just an inflammation of the pancreas, which is not as fatal as pancreatic cancer. The symptoms of pancreatitis can be easily detected, but the symptoms of pancreatic cancer cannot be detected early.
How long does it take for pancreatic cancer to spread?
It takes an average of 7 (seven) years for the initial cancer cell to multiply into the billions of cells that comprise a malignant tumour of the size of a plum, after which at least one cell within the tumour has the potential and capability to migrate to other organs. Patients survive an average of 2.5 years following this metastasis.
What Is the cost of Pancreatic Cancer Treatment at PACE Hospitals, Hyderabad?
At PACE Hospitals, Hyderabad, the cost of pancreatic cancer treatment typically ranges from ₹1,800 to ₹6,25,000 and above (approx. US $22 – US $7,500), making it a comprehensive and advanced yet competitively priced option for cancer care. However, the final cost depends on:
- Stage and type of pancreatic cancer
- Need for CT, MRI, PET-CT, and biopsy
- Type of treatment: surgery, chemo, radiation, targeted therapy
- Whether Whipple surgery or palliative care is required
- Number of chemotherapy cycles
- Duration of hospitalization
- Nutritional support, pain management, and follow-up care
- Presence of complications (jaundice, weight loss, liver involvement)
Early-stage pancreatic tumors treated with basic investigations and medical care fall at the lower range, while advanced cancer requiring PET-CT, Whipple surgery, chemotherapy, and prolonged hospitalization falls at the higher end.
After specialist consultation, imaging, and biopsy evaluation, our oncology team will provide a personalised treatment plan and a transparent cost estimate based on the stage and type of pancreatic cancer.
How long does pancreatic cancer take to show symptoms?
Typically, early pancreatic malignancies do not manifest any symptoms. By the time they manifest symptoms, they have frequently developed to a substantial size or spread beyond the pancreas.
Early detection of pancreatic cancer is very difficult because of the presentation of only a few symptoms and the insensitivity of current imaging tools to detect pancreatic cancer at that stage. Before traditional testing can discover numerous cases of pancreatic cancer, there is a lag in time.
Can pancreatitis lead to cancer?
Yes, there is an increased risk (2-3%) of chronic pancreatitis, which can lead to pancreatic cancer. Chronic pancreatitis (long-term inflammation of the pancreas) can cause scarring and severe pain in the abdomen and lower back.
The symptoms of pancreatic cancer and chronic pancreatitis overlap, especially in the blockage of the pancreatic duct, due to which the reach of digestive enzymes produced by the pancreas is hindered in digesting food.
What is the survival rate of pancreatic cancer?
Earlier, pancreatic cancer survival rate was difficult to detect as most patients are asymptomatic and only show symptoms once they hit the advanced stages. However, with established, specialised screening tests which emerged by the turn of the century, many studies have investigated the survival rate. The pancreatic cancer survival rate is expressed in terms of 5 years.
- If the pancreatic cancer is localised (i.e., the tumour is found only in the pancreas), then the 5-year rate is 39.4%.
- In the case of regional pancreatic cancer (i.e., pancreatic cancer had spread to nearby lymph nodes outside the pancreas), the 5-year rate is 13.3%.
- In the case of metastatic pancreatic cancer (i.e., the spread of pancreatic was seen in other organs such as the liver or lung), the 5-year rate is 2.9%.
By concluding
all the stages, overall, the survival rate of pancreatic cancer is 10%.
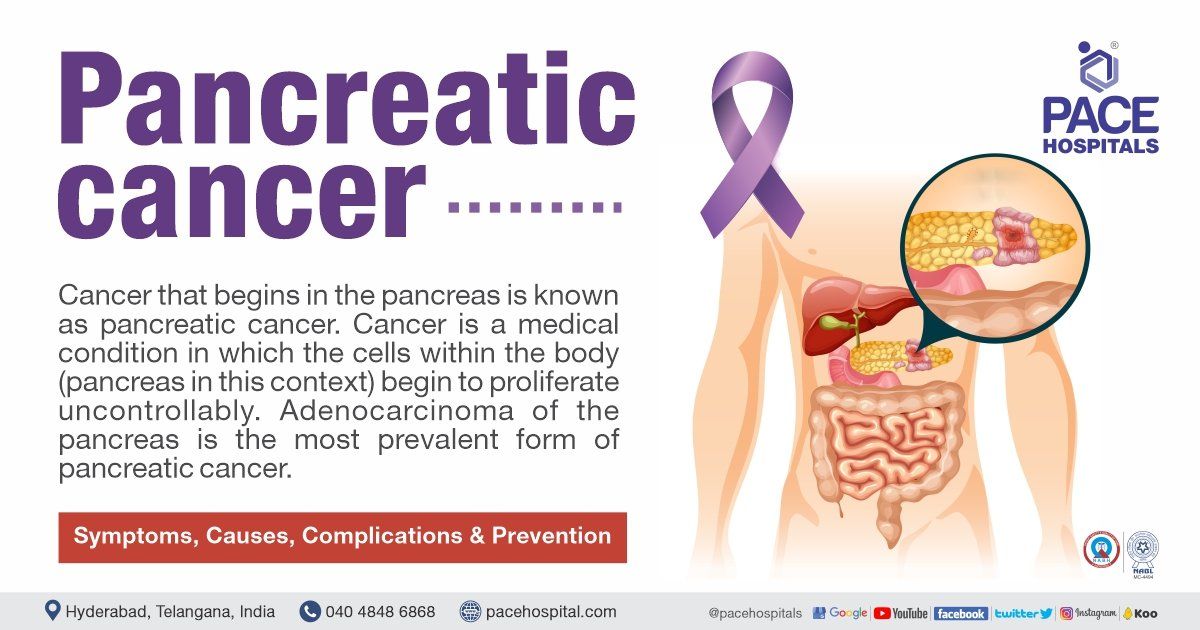
What causes pancreatic cancer?
Genetic mutations to the DNA are the fundamental causes of pancreatic cancer. These DNA mutations can occur through 3 ways. They are:
- Inherited Mutations: Most individuals with an inherited cancer syndrome inherit one mutant copy from any one of the parents. It must be understood that not everyone with an inherited mutant cancer will get pancreatic cancer, but the risk is greater.
- Mutation with Behaviour: The patients' behaviour can cause damage to DNA, such as cigarette smoking can cause pancreatic cancer-inducing chemicals in cancer-associated genes in the pancreas, which can grow into pancreatic cancer.
- Caused by Chance: DNA can be damaged by chance during the process of copying itself. Occasional mistakes during the copying of DNA can lead to mutation, which can increase the risk of pancreatic cancer.
What are the symptoms of pancreatic cancer?
The pancreatic cancer symptoms are the same in both men and women. They include:
- Ascites (distended abdomen) - due to the spread of pancreatic cancer in the abdominal cavity
- Abdominal and back pain - tumour pushing against the surrounding organs and nerves
- Bone pain-due to pancreatic cancer spread
- Cachexia - (general weight loss and muscle wasting) is usually due to metastasis (pancreatic cancer spread).
- Chills - due to infection and obstruction of the bile ducts by the increased size of the pancreas
- Diabetes - due to impaired insulin secretion by the pancreas
- Fatigue –Pancreatic cancer causes malnutrition and anaemia, which causes fatigue
- Fever - due to bile ducts obstruction, leading to infection of bile ducts and liver.
- Hair thinning and hair loss - due to chemotherapy
- Jaundice - due to obstruction in the bile duct, bile backs up into the liver and enters the bloodstream.
- Anorexia (loss of appetite)- due to pancreatic cancer blocking the gut or the effects of therapy.
- Stool discolouration - The bile duct and pancreatic duct are joined in the back of the head of the pancreas and open into the duodenum. Due to blockage, the bile is released into the bloodstream. The stool becomes light or clay-coloured as bile does not enter the digestive tract.
- Thrombophlebitis (inflammation and clotting of veins) - the body's response to pancreatic cancer or the direct spread of pancreatic cancer to blood vessels
- Urine discolouration - due to the accumulation of bile in the urine, makes it appear darker than usual.
- Weight loss - Almost all pancreatic cancers are associated with weight loss. Normal cells and malignant cells battle for nutrients. In addition, pancreatic cancers frequently impede digestion, which further adds to weight loss.
- Yellowing of skin or eyes - due to increased bile in the bloodstream.
How does pancreatic cancer affect the body?
Pancreatic cancer can affect the body in various ways. Pancreatic cancer ultimately causes death, often due to progressive inanition (exhaustion caused by lack of nourishment). The metabolic consequences of pancreatic cancer include a few of the following:
- Jaundice
- General malaise
- Depression
- Alopecia
- Pancreatic Insufficiency
- Bile Duct Obstruction
- Stomach Obstruction
- Small Intestine Obstruction
- Diabetes etc
Why do you get pancreatic cancer?
You can get pancreatic cancer if you:
- smoke
- consume alcohol
- have an increased BMI
- are diabetic
- suffer from chronic pancreatitis
- have familial history of pancreatic cancer
- have familial cancer syndromes
- suffer from medical conditions such as inflammatory bowel disease, periodontal disease, peptic ulcer disease
Also, the chances of cancer seem to increase in coal gas and aluminium workers from occupational exposure.
What are the pancreatic cancer surgery complications?
During the initial few weeks following pancreatic cancer surgery, patients may experience weakness, fatigue, and pain. Other negative effects of pancreatic removal include trouble digesting food and diabetes due to the pancreas' inability to make insulin. Before undergoing surgery, discuss with doctor the potential adverse effects of the procedure and how they will be addressed.
What are the side effects of chemotherapy for pancreatic cancer?
Chemotherapeutic side effects generally include poor appetite, nausea, vomiting, diarrhoea, gastrointestinal problems, rash, mouth sores, hair loss, and a lack of energy. They depend mainly on the drugs prescribed.
Interestingly, it was noticed that various patients have different side effects despite administering the same drug.
Chemotherapy could also induce leukopenia (low white blood cell count), anaemia and thrombocytopenia, risking the patients for infections, bruising and easy bleeding. Most side effects end with a chemotherapeutic regimen, but few can be long-lasting and worsen with treatment continuation.
What is the prognosis for pancreatic cancer?
The prognosis depends on the stage of diagnosis. At the moment of diagnosis, the prognosis for pancreatic cancer varies on the size and type of the tumour, lymph node involvement, and degree of metastasis (spread of cancer).
The improvement of prognosis is largely fruitful if the pancreatic cancer is discovered earlier and treated. Unfortunately, pancreatic cancer typically displays few or no symptoms until it has advanced and spread. Consequently, most cases (up to 80%) are diagnosed later, at more challenging stages.
Can pancreatic cancer be mistaken for pancreatitis?
Yes. Chronic pancreatitis shares numerous symptoms with pancreatic cancer, such as: extreme abdominal pain or digestive issues. These are recurrent, progressive, and extremely severe episodes. Mild pain may also be experienced between bouts, particularly in those who continue to consume alcohol. The other symptoms include:
- Recurring nausea and vomiting
- Weight loss
- Loss of appetite
- Increased frequency of urination
- Jaundice
As chronic pancreatitis and pancreatic cancer symptoms are similar, a CT scan and an endoscopic ultrasound test with biopsy can make a distinction.
Does a dilated pancreatic duct mean cancer?
No. As per the study, dilated pancreatic duct does not mean cancer, any degree of dilatation of the main pancreatic duct could be a sign of high risk for pancreatic cancer. In these cases, a total systemic examination of the patient is necessary for the early detection of pancreatic cancer.
What does pancreatic cancer feel like?
The most common feeling of pancreatic cancer includes a recurring dull pain in the upper abdomen (belly) and/or middle or upper back. This is likely caused by a tumour that has grown in the pancreatic body or tail and is pressing on the spine.
Some individuals report mid-abdominal pain that radiates to the back. Often, pain can be alleviated by bending forward when lying down. Pain caused by pancreatic cancer might vary from person to person; therefore, you should address any new pain-related pancreatic cancer symptoms with the doctor.
What is the most effective treatment for pancreatic cancer?
Surgery is a potentially successful therapy accessible to approximately 20% of pancreatic cancer patients. When surgery isn't an option, radiation therapy can be used to treat early-stage pancreatic cancer.
Can smoking cause pancreatic cancer?
Yes. Smoking releases carcinogens which cause mutation in DNA. Mutation in DNA can cause an increased risk of various cancers. Pancreatic cancer is one such malignancy.
The likelihood of developing pancreatic cancer is around double for smokers compared to those who have never smoked.
Approximately 25% of pancreatic cancers are attributed to cigarette smoking. Smoking cessation can help in the reduction of chances of cancer.
Does high bilirubin mean pancreatic cancer?
No, high bilirubin does not always mean pancreatic cancer. There are various other differential diagnoses for high levels of bilirubin, such as:
Intrinsic to the ductal system
- Jaundice - a liver disease in which bile is released into the system
- Gallstones - a small, hard crystalline abnormal mass in the gall bladder or bile ducts from bile pigments, calcium salts and cholesterol.
- Surgical strictures
- Infection
- Intrahepatic malignancy – cancer in the liver
- Cholangiocarcinoma - bile ducts cancer
Extrinsic to the ductal system
- Extrahepatic malignancy (pancreas, lymphoma)
- Pancreatitis – inflammation of the pancreas
What is pancreatic cancer treatment cost in India?
Pancreatic cancer treatment cost in India ranges from ₹ 4,75,000 to ₹ 7,65,000 (US$ 5750 - US$ 9250) (INR four lakh seventy-five thousands to seven lakh sixty-five thousands). Treatment of pancreatic cancer cost in India depends upon the multiple factors such as the patient's age, stage of pancreatic cancer, complications associated and types of pancreatic cancer treatment such as Chemotherapy, Whipple Procedure, Central Pancreatectomy, Distal Pancreatectomy, Total Pancreatectomy and Radiation Therapy
It must be understood that the damage to the pancreas is permanent. Nevertheless, right time and early diagnosis can help in treating the causes and further any additional pancreas impairment must be avoided to slow the prognosis.
Are pancreatic cancer treatment covered by insurance in India?
Yes, pancreatic cancer treatment is covered by insurance in Hyderabad, India. Person need to cross-check with their respective health insurance companies and corporates about the partial or complete cashless treatment eligibility to get the benefits.
Why choose PACE Hospitals?
- A Multi-Super Speciality Hospital.
- NABH, NABL, NBE & NABH - Nursing Excellence accreditation.
- State-of-the-art Liver and Kidney transplant centre.
- Empanelled with all TPAs for smooth cashless benefits.
- Centralized HIMS (Hospital Information System).
- Computerized health records available via website.
- Minimum waiting time for Inpatient and Outpatient.
- Round-the-clock guidance from highly qualified super specialist doctors, surgeons and physicians.
- Standardization of ethical medical care.
- 24X7 Outpatient & Inpatient Pharmacy Services.
- State-of-the-art operation theaters.
- Intensive Care Units (Surgical and Medical) with ISO-9001 accreditation.