Pancreatic cancer - Symptoms, Causes, Complications and Prevention
PACE Hospitals
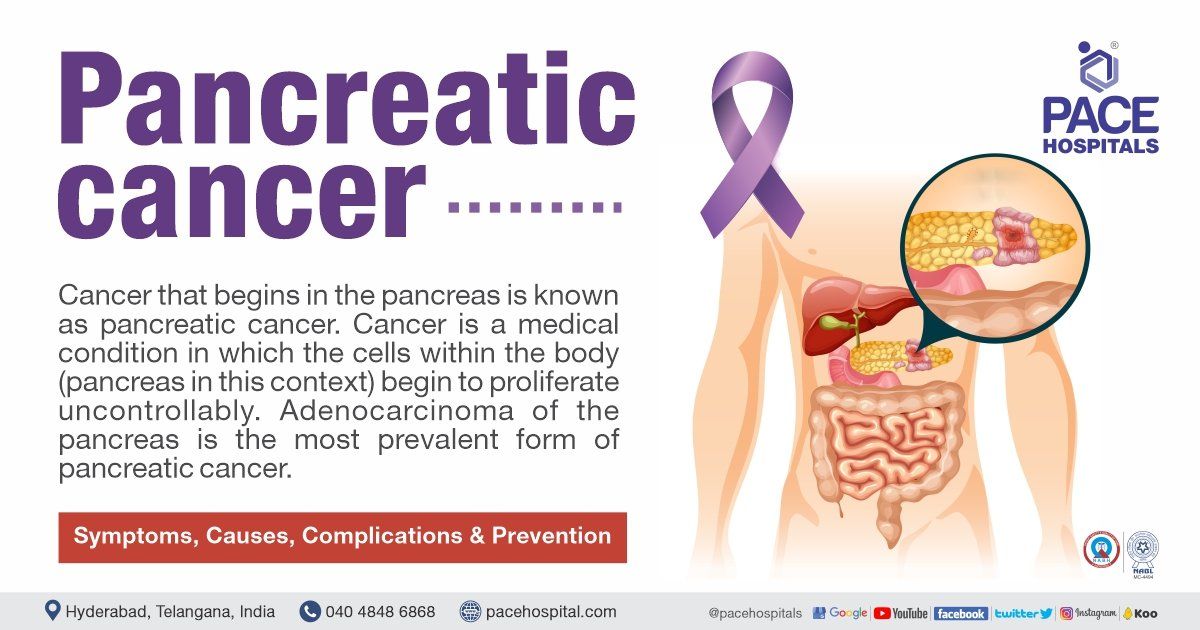
Cancer that begins in the pancreas is known as pancreatic cancer. Cancer is a medical condition in which the cells within the body (pancreas in this context) begin to proliferate uncontrollably. Adenocarcinoma of the pancreas is the most prevalent form of pancreatic cancer.
Types of Pancreatic cancer
There are numerous forms of pancreatic cancer, which are distinguished primarily by origination of tumour: the exocrine or endocrine component.
Exocrine tumours. This is the most prevalent kind of pancreatic cancer. Most people simply refer to this malignancy as pancreatic cancer. Adenocarcinoma is the most typical kind of exocrine malignancy. These tumours typically begin in the pancreatic ducts and are known as ductal adenocarcinoma. If the tumour originates in the acini, it is referred to as acinar adenocarcinoma.
Intraductal papillary mucinous neoplasm (IPMN): is a more frequent tumour that forms within the pancreatic ducts and produces a viscous fluid called mucin. Pancreatic ducts transport digestive juices from the pancreas to the intestines. IPMN is not malignant at its onset but could develop into cancer if left untreated. Occasionally, by the time an IPMN is identified, it has progressed to a cancerous state. Much rarer types of exocrine pancreatic tumours include:
- Acinar cell carcinoma
- Adenosquamous carcinoma
- Colloid carcinoma
- Giant cell tumour
- Hepatoid carcinoma
- Mucinous cystic neoplasms
- Pancreatoblastoma
- Serous cystadenoma
- Signet ring cell carcinoma
- Solid and pseudopapillary tumors
- Squamous cell carcinoma
- Undifferentiated carcinoma
Endocrine tumours (also known as pancreatic neuroendocrine tumours (PNETs) and islet cell tumours): Much less prevalent than exocrine tumours, they account for approximately 7% of all pancreatic malignancies differing significantly from what the commonly occurring pancreatic cancer. A neuroendocrine tumour of the pancreas can be either functional or nonfunctional. A healthy tumour produces hormones. An inactive tumour does not produce hormones. A functioning neuroendocrine cancer is named based on the hormone the cells normally make, which includes:
- Insulinoma
- Glucagonoma
- Gastrinoma
- Somatostatinoma
- VIPomas
- PPomas
Sometimes, other types of cancer can begin in the pancreas, such as lymphoma and sarcoma.
Causes of Pancreatic cancer
Pancreatic cancer causes are unclear. Doctors have identified several risk factors for pancreatic cancer, including smoking and inheriting particular gene abnormalities. Pancreas is a pear-shaped gland about 6 inches long secreting insulin and digestive juices to process the sugar and proteins in the foods respectively.
Mutations: Pancreatic cancer occurs when the DNA of pancreatic cells is mutated (altered). The DNA of a cell includes the instructions that tell it what to do. These mutations instruct the cells to proliferate uncontrollably and survive after normal cells would have died. These cells can accumulate to develop a tumour. Pancreatic cancer cells can spread to surrounding organs and blood vessels, as well as to distant parts of the body if left untreated.
Symptoms of Pancreatic cancer
Initial pancreatic cancer symptoms are sometimes ambiguous and, as a result, frequently misinterpreted.
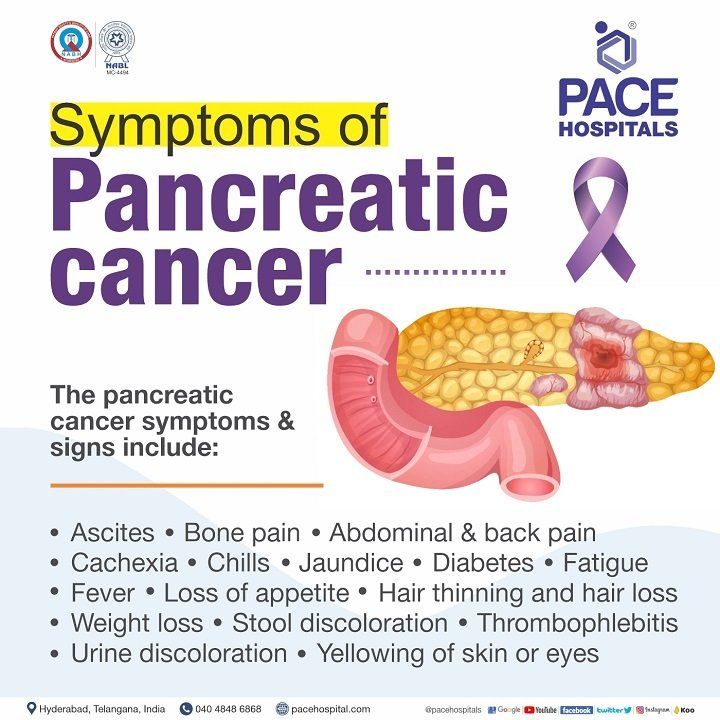
It must be understood that these pancreatic cancer symptoms are surfaced very late, so patients are usually presented to the doctor at a very advanced stage which is why the management of pancreatic cancer is difficult. The pancreatic cancer symptoms and signs include:
- Ascites (distended abdomen) - due to spread of the pancreatic cancer in abdominal cavity
- Abdominal and back pain - Tumor pushing against the surrounding organs and nerves
- Bone pain - due to pancreatic cancer spread
- Cachexia - (general weight loss and muscle wasting) usually due to metastasis (pancreatic cancer spread).
- Chills - due to infection and obstruction of the bile ducts by increased size of pancreas
- Diabetes - due to impaired insulin secretion by the pancreas
- Fatigue – Pancreatic Cancer causes malnutrition and anaemia which causes fatigues
- Fever - due to bile ducts obstruction, leading to infection of bile ducts and liver.
- Hair thinning and hair loss - due to chemotherapy
- Jaundice (yellowing of skin or eyes) - due to obstruction in bile duct due to which bile backs up into the liver and enters the bloodstream.
- Loss of appetite (anorexia) - due to the pancreatic cancer blocking gut, or by the effects of therapy.
- Stool discoloration - Bile duct and pancreatic duct are joined in the back of the head of the pancreas and opens into the duodenum. Due to blocked bile is released into bloodstream. As bile is not entering into the digestive tract, stool becomes light or clay-coloured.
- Thrombophlebitis (inflammation and clotting of veins) - body's response to pancreatic cancer or direct spread of the pancreatic cancer to blood vessels
- Urine discoloration - due to accumulation of bile in the urine makes it appear darker than usual.
- Weight loss - Almost all pancreatic cancers are associated with weight loss. Normal cells and malignant cells battle for nutrients. In addition, pancreatic cancers frequently impede digestion, which further adds to weight loss.
Risk factors of Pancreatic cancer
Tobacco use is the most prevalent among numerous established risk factors that can raise the likelihood of developing pancreatic cancer. Other pancreatic cancer risk factors include the following:
- Obesity
- Diabetes mellitus
- Chronic pancreatitis
- Genetic factors
Less than 5% of pancreatic malignancies are associated with chronic pancreatitis. Unless it is accompanied by chronic pancreatitis, alcohol use does not appear to be an independent risk factor for pancreatic cancer.
Smoking: The most prevalent environmental risk factor for pancreatic cancer is smoking. According to estimates, smoking is responsible for up to 30% of pancreatic cancer incidences.
Smokers are at least twice as likely to develop pancreatic cancer as non-smokers. Current smokers with a smoking history of over 40 pack-years may have a 5-fold increased risk for the disease. Additionally, smokeless tobacco raises the risk of pancreatic cancer.
Obesity and dietary factors: Multiple studies have linked obesity, particularly central obesity, to an increased risk of pancreatic cancer.
Overweight or obese during early adulthood was related with an increased risk of pancreatic cancer and a faster age of disease beginning, but obesity at a later age was associated with a poorer overall survival rate.
The incidence of pancreatic cancer is lower in persons with a diet rich in fresh fruits and vegetables. Red meat consumption, particularly processed red meat, is connected with an increased risk of pancreatic cancer.
Interestingly, poultry and dairy products consumption does not raise the risk.
Coffee drinking may lessen the incidence of pancreatic cancer. The roasted coffee is a complex mix of more than a thousand anticarcinogenic compounds, such as:
- Caffeine
- Cafestol
- Kahweol
- Polyphenols
- Caffeic acid
- Chlorogenic acid etc.
Diabetes mellitus: Recently diagnosed with diabetics are at 5.4 times the risk for pancreatic cancer. Diabetes has been suggested to be at least partially a consequence or pancreatic cancer early symptoms, among others.
A 30% extra risk for pancreatic cancer is observed for more than two decades after a diabetes diagnosis, supporting the bidirectional association between diabetes and pancreatic cancer.
Research concluded that people with at least five years of diabetes mellitus have a twofold greater chance of acquiring pancreatic cancer.
Chronic pancreatitis: Chronic, long-lasting pancreatitis is a significant risk factor for the development of pancreatic cancer (so much as a 26-fold increased risk of pancreatic cancer).
Chronic pancreatitis due to alcohol usage is also related with a substantially higher risk of pancreatic cancer and an earlier age of onset.
Genetic factors: Approximately 5-10% of patients with pancreatic carcinoma have some genetic predisposition to developing the disease. Approximately 5-10% of pancreatic cancer patients have a hereditary tendency to develop the disease.
About 18-36 months after a diagnosis of diabetes mellitus, patients aged 65 and older without a family history of diabetes may develop pancreatic cancer.
Patients with hereditary pancreatitis are even more likely to develop pancreatic cancer. The median age of these patients with pancreatic cancer is approximately 57 years. Hereditary pancreatitis multiplies the relative risk of pancreatic cancer by more than 50, and by age 70, the cumulative risk of pancreatic cancer is 40%. Certain precursor lesions have been linked to pancreatic cancers emerging from the pancreatic ductal epithelium.
Pancreatic intraepithelial neoplasia (PIN) is the predominant morphologic type associated with pancreatic ductal adenocarcinoma which are the result of certain genetic abnormalities contributing to the development of invasive ductal adenocarcinoma. The inherited disorders that increase the risk of pancreatic cancer include the following:
- Hereditary pancreatitis
- Multiple endocrine neoplasia
- Hereditary nonpolyposis rectal cancer
- Familial adenomatous polyposis
- Gardner syndrome
- Familial atypical multiple mole melanoma syndrome
- Von Hippel-Lindau syndrome
- Germline mutations in the BRCA1 and BRCA2 genes
Complications of Pancreatic cancer
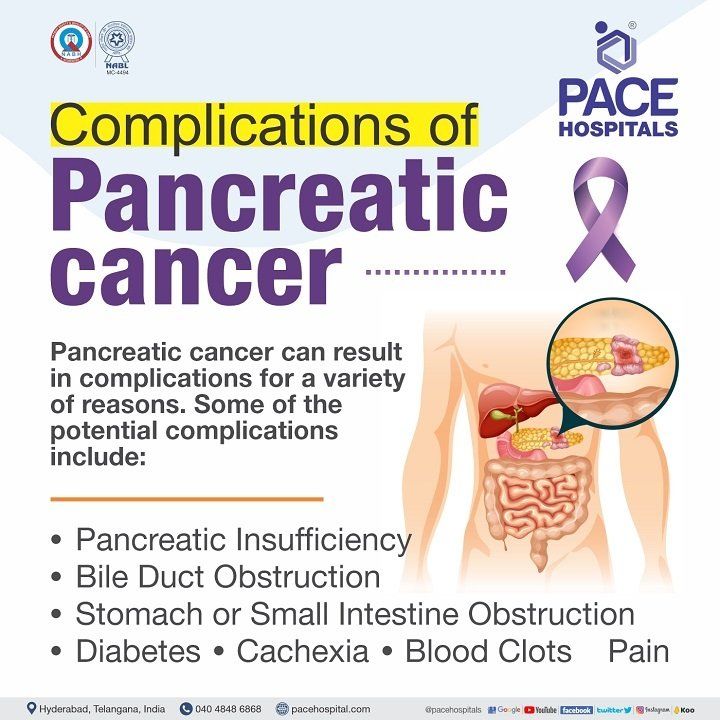
Pancreatic cancer can result in complications for a variety of reasons, including pressure on neighbouring structures, a shortage of molecules produced by normal pancreatic cells, the disease's own metabolism, or the spread of the tumour to other parts of the body (metastases). Specific potential difficulties may include:
- Pancreatic Insufficiency
- Bile Duct Obstruction
- Stomach or Small Intestine Obstruction
- Diabetes
- Cachexia
- Blood Clots
- Pain
Pancreatic Insufficiency - Most frequently, pancreatic tumours arise in the cells (exocrine cells) that make pancreatic enzymes.
- Approximately eight cups of these enzymes, which neutralise stomach acid and help in the breakdown of fats, proteins, and carbs, are produced daily by the pancreas.
- Even with a normal diet, the lack of enzymes can result in malabsorption, stomach discomfort, and malnutrition when a tumour takes over these cells.
- Pancreatic insufficiency occurs in 80-90% of people with pancreatic cancer and is treated with pancreatic enzyme replacement.
Bile Duct Obstruction - Common bile duct obstruction is a typical consequence of pancreatic cancer, which may already be present at the time of diagnosis.
Endoscopy, which includes introducing a tube into the mouth and threading it into the common bile duct, can be used to install a stent even when surgery is not possible.
Common complications of stents include:
- Stent occlusion
- Stent migration
- Cholecystitis
- Cholangitis
- Perforation
- Bleeding
Stomach or Small Intestine Obstruction - Either the gastric outlet or the initial portion of the small intestine (the duodenum) can get obstructed by a developing tumor. If this occurs, a stent can be inserted to keep these areas open, or surgery can be performed to circumvent the obstruction.
Diabetes - The abrupt onset of diabetes may signal the presence of pancreatic cancer.
- Even if insulin resistance or diabetes is not apparent at the time of diagnosis, around 85% of patients with the condition will develop it at some point.
- Moreover, hyperglycaemia (increased blood sugar) is an indicator of pancreatic cancer.
- It is believed that pancreatic cancer may cause cells to develop resistance to insulin, the important hormone produced by the pancreas that controls blood sugar.
- In other insulin-resistant states, such as obesity, insulin-producing cells in the pancreas produce more insulin to overcome insulin resistance.
- However, pancreatic cancer appears to hinder pancreatic cells that produce insulin from responding effectively to insulin resistance. This results in the development of diabetes.
Cachexia - also known as cancer-related anorexia-cachexia syndrome is a syndrome of weight loss, muscle wasting, and appetite loss.
- It is believed to be present in up to 80% of pancreatic cancer patients at the time of diagnosis.
- Cachexia may be the direct cause of death in 20% of cancer patients.
- In addition to "normal" cachexia, a shortage of pancreatic enzymes can result in malnutrition and increased weight loss, making this a crucial issue for pancreatic cancer patients to address.
Blood Clots - Deep vein thrombosis (DVT) (occurs when a blood clot (thrombus) forms in one or more of the deep veins in the body, usually in the legs) that occasionally break off and move to the lungs (pulmonary emboli) are not only a complication of pancreatic cancer; they can also be the first sign of the disease.
- They are also exceedingly prevalent at all stages of the disease.
- People with pancreatic cancer are also more prone than those with other types of cancer to bleed when taking blood thinners, thus therapy must be closely watched.
Pain - The pain associated with pancreatic cancer can be extremely intense, but there are numerous methods for managing pancreatic cancer pain.
- Frequently, many treatments, such as pain medicines, radiation therapy to the abdomen, and a "celiac block," a surgery that stops the nerves to the abdomen that convey pain signals to the brain, are combined.
- It is suggested that individuals with pancreatic cancer visit a pain or palliative care professional to ensure they receive safe, appropriate, and timely pain medication when required.
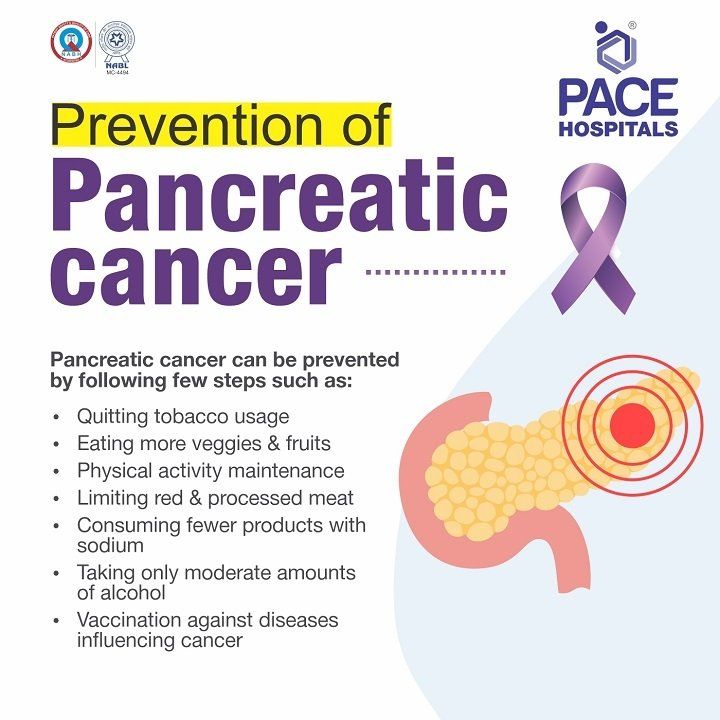
Prevention of Pancreatic cancer
Pancreatic cancer is an uncommon, deadly disease with a few identified risk factors, including smoking, genetic susceptibility, and advancing age. Recent research has revealed advancements in pancreatic cancer treatment and prevention.
- As long as pancreatic tumours are typically identified too late, the most important responsibility for every person on earth is to adopt a healthy attitude and prevent mortality in the near future.
- Vaccination against diseases influencing carcinogenesis, does not incur additional costs to the individual.
- Changes in lifestyle could play a significant impact in lowering the incidence of pancreatic cancer, with no severe side effects.
- Changes in the way of life may also allow us to remain healthier and more fulfilled. The tips include:
- Being in good shape, slim
- Physically active
- Quitting smoking
- Quitting tobacco usage
- Consuming moderate amounts of alcohol
- Consuming fewer products preserved with sodium
- Having less red meat and processed meat
- Consuming more vegetables and fruits
Frequently asked questions
Is pancreatic cancer curable?
Yes. Despite the bad prognosis (overall outlook for pancreatic cancer) and the fact that the disease is generally incurable, pancreatic cancer may be cured if detected extremely early.
- Up to 10% of patients who obtain an early diagnosis are cured following treatment.
- Patients detected with pancreatic cancer before the tumour grows significantly or spreads have an average survival period of 3 to 3.5 years.
- Surgical resection is now the only treatment option for pancreatic cancer, but only 20% of cases are surgically resectable at the time of diagnosis.
How I knew if I had pancreatic cancer?
One of the most common initial indications of a pancreatic cancer is jaundice (a yellowing of the skin and the whites of the eyes, due to excess of bilirubin in blood).
- Bilirubin is a dark, yellow-brown material created by the liver.
- The bile (which contains bilirubin) produced by the liver flows through the common bile duct into the intestines to break down lipids and is then expelled in stool.
- If the common bile duct is obstructed, bilirubin can build up and cause jaundice.
- Pancreatic cancers arising in the body or tail don't push on the duct until they've migrated through the pancreas and, in certain cases, to other organs - typically the liver, which increases jaundice.
How to diagnose pancreatic cancer early?
Early pancreatic cancer detection is difficult.
- Early malignancies in the pancreas can't be seen or felt during standard physical tests.
- The patients suffering from pancreatic cancer don't experience pancreatic cancer symptoms until the cancer is huge or has spread.
- Identification of risk population and screening them for pancreatic cancer (even though they do not show any explicit pancreatic cancer symptoms) can be of help.
Can ultrasound detect pancreatic cancer?
Yes. Ultrasound can detect pancreatic cancer. Three types of ultrasound tests can be used to detect pancreatic cancer.
- Transcutaneous ultrasonography: A practical, trustworthy method for the non-invasive diagnosis and evaluation for a variety of disorders.
- Endoscopic ultrasonography (EUS): Technique of sound energy producing images of the pancreas, bile duct, and digestive tract by sending endoscopes (thin, illuminated tubes) through patient's mouth and guided into the first portion of the small intestine via the stomach (duodenum).
- Transabdominal ultrasound (TUS): A widely utilised as a first-line diagnostic tool for patients presenting with jaundice or stomach pain. It can be conducted for annual health or screening tests for asymptomatic patients. However, the diagnostic performance of TUS is highly dependent on the patient's condition, such as obesity and the presence and quantity of bowel gas that interferes with the examination.
What is whipple procedure for pancreatic cancer?
Whipples procedure, also termed as pancreaticoduodenectomy, is a surgical procedure done to treat tumours of the pancreas, the intestine and the bile duct. It is a complicated procedure primarily used to treat pancreatic cancer confined to the head of the pancreas, part of the adjacent small intestine called the duodenum, the common bile duct, and the gallbladder.
Is pancreatic cancer hereditary?
Yes. Pancreatic cancer can be inherited.
- Genetic mutations to the DNA are the fundamental causes of pancreatic cancer.
- Most individuals with an inherited cancer syndrome inherit one mutant copy from any one of the parents.
- Nevertheless, it must be understood that not everyone with an inherited mutant cancer will be contracted with a pancreatic cancer but the risk of the same is greater.
Can you detect pancreatic cancer with a blood test?
Pancreatic cancer patients had increased carcinoembryonic antigens (CEA) and CA (carbohydrate antigen) 19-9 in their blood. False positives are possible with these tests.
- Pancreatic cancer produces CEA. Antibodies assist the body combat antigens.
- After surgery, CEA levels are often tested to understand the success of the intervention.
- CA 19-9 levels often indicate pancreatic cancer.
- It can also signal other cancers and noncancerous illnesses like cirrhosis and gallstones.
- As high CA 19-9 levels can imply multiple things, the test is not used to screen for or diagnose cancer, but to monitor pancreatic cancer and treatment effectiveness.
How long can you live with stage 4 pancreatic cancer?
Five-year survival for stage IV pancreatic cancer is 1%.
- Late-stage pancreatic cancer patients on an average typically live for 1 year post diagnosis.
- Although 5-year survival rates are known for each stage, it must be understood that all these are averages.
- As the prospects of every patient is different, it can be concluded that what works for one patient may not work for another.
How to treat pancreatic cancer pain?
Pancreatic cancer can cause severe pain in the abdomen and back. Management of cancer-related pain is one of the most important aspects of pancreatic cancer care, which combines aggressive therapy with continual assessments to ensure that patients can maintain their quality of life.
A comprehensive Pain Assessment will be conducted by the doctor to determine:
- When the pain started
- Where the pain is located
- How intense the pain is
- How various pancreatic cancer treatments have impacted the pain level
Following the assessment, the doctor will help devise a treatment plan which consists of:
- Opioids and its derivates
- Antiepileptics
- Corticosteroids
- Chemotherapy and radiation therapy
- Celiac plexus block and neurolysis
- Intrathecal therapy
Other alternative medicine include:
- Acupuncture
- Hypnosis
Can pancreatic cancer go into remission?
Yes, some patients suffering with pancreatic cancer achieve remission (showing "no signs of disease). During the course of pancreatic cancer treatment, if scans and tests no longer identify the disease in a patient's body, the patient can be considered to be in "remission".
- It must be bear in mind that despite the fact that these pancreatic cancer symptoms indicate that the cancer has been eradicated, there is always a potential that tiny cancer cells persist in the body even after successful therapy.
- These cells cannot be detected using imaging or other methods.
- If these cells are present, the patient may experience a cancer recurrence or return.
- Therefore, being in remission does not indicate that a patient is cured or free of cancer.
- Nevertheless, remission is a significant turning point in the therapeutic journey of a patient.
- It indicates that the patient has completed treatment and will begin periodic follow-up appointments, exams, and tests to monitor for signs of the pancreatic cancer returning or developing.
- If the condition returns, treatment will be resumed. It is difficult to predict when or even if a recurrence may occur.
- Every pancreatic cancer patient is unique, and a treatment that is effective for one individual may not be as effective for another.
While few pancreatic cancer patients can achieve remission, others are able to stabilise their disease or shrink their tumours through, surgery, radiation, chemotherapy, targeted therapy, or a combination of these procedures.
When to stop chemo for pancreatic cancer?
If the tumours continue to grow or spread despite maintaining perfect prescription adherence to at least the last three chemotherapy treatments for cancer, discontinuation of chemotherapy can be considered.
Other treatment choices, such as immunotherapy and other experimental treatments can be pursued.
Why is pancreatic cancer deadly?
There are three main reasons which make the pancreatic cancer a deadly disease.
Late detection: The earlier pancreatic cancer is detected, the greater a patient's chance of survival.
- However, the majority of individuals do not exhibit pancreatic cancer symptoms of pancreatic cancer in its early stages.
- Only in 10% of pancreatic cancer patients surgical intervention is possible.
- Patients exhibiting signs such as jaundice, discomfort, and weight loss are frequently diagnosed after the cancer has spread.
- There is currently no screening method for pancreatic cancer.
The anatomical positioning of pancreas: The pancreas is a vital organ positioned in the visceral cavity surrounded with several major blood arteries which can make surgery challenging.
- Additionally, the major components of the gastrointestinal tract are located in this region.
Affinity to metastasis: Pancreatic cancer is more prone to metastasis, or spread to other parts of the body.
- Around 85% of patients are presented to the doctor in the advanced stage of metastatic cancer due to which surgery is inevitable.
- The majority of people will require chemotherapy to treat their condition.
Can anyone survive pancreatic cancer?
Despite the bad disease outlook and the fact that the disease is generally incurable, pancreatic cancer may be cured if detected extremely early.
- Up to 10% of patients who obtain an early diagnosis are cured following treatment.
- Patients detected with pancreatic cancer before the tumour grows significantly or spreads have an average survival period of 3 to 3.5 years.
Does pancreatic cancer cause diabetes?
Yes. There is a high chance of the pancreatic cancer patient contracting diabetes. Diabetes is a disorder of the body in which there is always a constant rise of sugar level in blood. The sugar level in blood is regulated by insulin, which is produce by pancreas. Due to the impairment of pancreas by pancreatic cancer, the functions of pancreas may get hindered leading to poor production of insulin which in turn causes diabetes.
Does pancreatic cancer cause diarrhoea?
Pancreatic cancer can cause digestive difficulties such as weight loss, a poor appetite, and diarrhoea, due to the wrapping of a pancreatic tumour on the small intestine or stomach blocking the digestive tract.
Diarrhoea also results when the nutrients in food are not absorbed properly. Poor production of pancreatic enzymes can lead to poor absorption due to which and undigested food passes quickly through the digestive tract, causing diarrhoea.
What doctor treats pancreatic cancer?
HPB oncologists are doctors who treat pancreatic cancer. Pancreatic cancer treatment involves a multidisciplinary team of doctors to create a tailor-made pancreatic cancer treatment and overall care plan by combining various types of supportive and curative treatments. The multidisciplinary team involves various healthcare professionals such as:
- Medical Oncologists
- Surgical Oncologists
- HPB Oncologists
- Diabetologist
- Physician assistants
- Oncology Medical staff
- Clinical pharmacists
- Dietitians
How bad is itching with pancreatic cancer?
Pancreatic cancer can cause jaundice (increased bilirubin in blood). Increased bilirubin in skin not only brings discolouration but also incessant itching (pruritis). Often patients cite pruritis as one of the worse pancreatic cancer symptoms. The distressing symptom of pruritis associated with jaundice and pancreatic cancer has been exasperating and difficult to treat.
Doctors typically prescribe antihistamines for binding the bile salts in the intestine which aids in their excretion.
Share on
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868