UGI Endoscopy in Hyderabad, India
PACE Hospitals offers comprehensive UGI endoscopy services in Hyderabad, Telangana, India. Our experienced gastro specialists conduct precise endoscopy tests and endoscopy procedures to diagnose and treat a variety of digestive disorders. With state-of-the-art facilities and a patient-focused approach, we ensure safe, comfortable, and effective UGI endoscopy care.
Book an appointment for
Upper GI Endoscopy
Endoscopy Appointment Enquiry
Thank you for contacting us. We will get back to you as soon as possible. Kindly save these contact details in your contacts to receive calls and messages:-
Appointment Desk: 04048486868
WhatsApp: 8977889778
Regards,
PACE Hospitals
HITEC City and Madeenaguda
Hyderabad, Telangana, India.
Oops, there was an error sending your message. Please try again later. Kindly save these contact details in your contacts to receive calls and messages:-
Appointment Desk: 04048486868
WhatsApp: 8977889778
Regards,
PACE Hospitals
HITEC City and Madeenaguda
Hyderabad, Telangana, India.
Why Choose PACE Hospitals for Upper GI Endoscopy?

State-of-the-Art Endoscopy Suites with Advanced Video Endoscopes, High-Resolution Imaging & Safe Sedation
Expert Interventional Gastroenterologists for Comprehensive Diagnosis and Treatment of Upper GI Disorders
Upper GI Endoscopy with High Accuracy, Minimal Discomfort & Same-Day Recovery
Affordable & Transparent Upper GI Endoscopy Cost with Insurance and Cashless Options
UGI Endoscopy Test
The UGI Endoscopy Test, also known as Upper GI Endoscopy or esophagogastroduodenoscopy (EGD), is a diagnostic procedure used to examine the upper gastrointestinal tract.
UGI Endoscopy full form
It stands for Upper Gastrointestinal Endoscopy, and it includes Esophagoscopy, Gastroscopy, and Duodenoscopy to examine the esophagus, stomach, and duodenum.
What is Upper GI Endoscopy?
An Upper GI Endoscopy / esophagogastroduodenoscopy (EGD) or UGI endoscopy test is a procedure enables visualization of the upper digestive system including oropharynx, esophagus, stomach, and the proximal part of the duodenum. It allows for both diagnosis and treatment of conditions affecting the upper gastrointestinal tract. This endoscopy procedure uses a long, flexible tube known as an endoscope. One end of the tube carries a small light and a video camera. It is inserted through the mouth and throat, then carefully guided down the esophagus (food pipe) into the stomach, and finally into the duodenum.
It is a frequently performed procedure, particularly by specialists in gastroenterology. Furthermore, it serves both diagnostic and, in some cases, therapeutic purposes, allowing direct visualization and intervention within the upper digestive tract-including the oropharynx, esophagus, stomach, and the initial portion of the small intestine (duodenum). Given the complexity and scope of this examination, it is typically carried out by trained physicians known as endoscopists, with gastroenterologists being the primary providers due to their specialiced expertise in managing disorders such as inflammation (redness, irritation), bleeding, ulcers, or tumors of the gastrointestinal system.

Upper GI Endoscopy Indications
Upper GI Endoscopy or EGD is a diagnostic and therapeutic procedure that visualizes the esophagus, stomach, and duodenum. Common indications for upper gastro-intestinal tract endoscopy include the following:
- Evaluation of achalasia: EGD is recommended to rule out malignancy at the gastroesophageal junction in patients diagnosed with achalasia before initiating therapeutic procedures such as dilation or myotomy.
- Screening and surveillance for Barrett’s esophagus: EGD is indicated in patients with long-standing GERD symptoms to screen for Barrett’s esophagus. Surveillance intervals are based on the degree of dysplasia identified in biopsies.
- Assessment after caustic ingestion: When patients ingest caustic substances, EGD is necessary to assess the extent of esophageal or gastric injury and to monitor complications like strictures or malignancy.
- Diagnosis and staging of esophageal cancer: EGD enables direct visualization, biopsy, and staging of esophageal tumors. It is also used in the surveillance of treated cancer or suspected recurrence.
- Management of esophageal strictures: Patients with dysphagia from benign or malignant strictures undergo EGD for diagnosis and therapeutic dilation using balloon or bougie techniques.
- Screening for esophageal varices: In patients having cirrhosis and portal hypertension, EGD is the standard method to detect esophageal varices and to perform endoscopic band ligation if indicated.
- Removal of foreign bodies: Urgent EGD is performed to remove sharp objects, batteries, or obstructing items from the esophagus or stomach to prevent aspiration or perforation.
- Evaluation of gastric polyps: EGD helps detect and resect gastric polyps, especially adenomatous types with malignant potential, followed by surveillance to assess for recurrence.
- Diagnosis of peptic ulcer disease: Patients with symptoms of dyspepsia or suspected ulcers undergo EGD for visualization, biopsy (for H. pylori), and treatment of ulcer-related bleeding.
- Evaluation of Gastroesophageal reflux disease (GERD) with alarm symptoms: EGD is indicated in patients with GERD who have symptoms such as dysphagia, odynophagia, or weight loss to rule out complications like Barrett’s esophagus or strictures.
- Staging and biopsy of gastric cancer: EGD is used to biopsy suspicious gastric lesions and ulcers. Repeating EGD after treatment ensures healing and rules out persistent or malignant tissue.
- Detection of ampullary adenoma: EGD with a side-viewing endoscope is used to assess adenomas at the duodenal papilla and guide management, including resection or further evaluation with ERCP/EUS.
- Evaluation of nonampullary duodenal adenomas: EGD is used to identify, biopsy, and resect these adenomas, particularly in patients with familial adenomatous polyposis, followed by endoscopic surveillance.
- Surveillance in hereditary cancer syndromes: Patients with Familial Adenomatous Polyposis (FAP) or Hereditary Nonpolyposis Colorectal Cancer (HNPCC) undergo periodic EGD to detect early upper GI cancers, especially in the duodenum or stomach, due to increased malignancy risk.
- Evaluation of upper GI involvement in Inflammatory Bowel Disease (IBD): In patients with Crohn’s disease, EGD helps detect granulomas and distinguish them from ulcerative colitis in cases of indeterminate colitis.
- Placement of Percutaneous endoscopic gastrostomy (PEG) tubes: EGD is used to guide the placement of gastrostomy tubes in patients unable to maintain oral intake due to neurologic or structural impairments.
- Diagnosis and treatment of upper GI bleeding: EGD allows visualization and control of bleeding sources, such as ulcers, varices, or Mallory-Weiss tears, reducing transfusion needs and hospital stay.
- Evaluation of obscure GI bleeding: In cases where bleeding persists despite normal findings on initial endoscopy and colonoscopy, a repeat EGD may identify lesions missed during the first procedure.
- Screening for pernicious anemia: Patients with pernicious anemia undergo EGD to assess for atrophic gastritis or gastric cancer due to an elevated malignancy risk, though routine follow-up is not usually necessary.
- Preoperative and postoperative bariatric surgery evaluation: EGD is used to assess ulcers, hiatal hernias, or malignancy before surgery and to investigate symptoms like nausea or pain after surgery.
Contraindications of Upper GI Endoscopy
Upper GI endoscopy (esophagogastroduodenoscopy, or EGD) is extremely useful, but there are specific situations in which it is contraindicated due to risk or non-applicability. Contraindications for Upper GI Endoscopy include the following clinical conditions where the procedure may pose a significant risk or is not advisable:
Absolute Contraindications
- Gastrointestinal perforation or peritonitis: If there is a suspected or confirmed perforation of the digestive tract, or signs of peritonitis, EGD should be avoided, as the procedure may worsen the condition.
- Toxic megacolon with hemodynamic instability: Patients with toxic megacolon who are unstable are at high risk, performing endoscopy may precipitate perforation or clinical deterioration.
- Unstable airway or cardiovascular collapse: In settings of airway instability, respiratory compromise, or cardiovascular collapse, sedation and endoscopy carry unacceptable risk.
- Lack of informed consent or inability to cooperate: If the patient refuses consent or cannot cooperate (e.g., due to mental status, severe agitation) despite sedation options, EGD should not proceed.
Relative Contraindications
- Coagulopathy or severe thrombocytopenia: When bleeding risk is elevated (for example, markedly abnormal coagulation parameters or very low platelet counts), EGD with biopsy or therapeutic intervention should be deferred, or the coagulopathy corrected if possible.
- Severe neutropenia: Due to the increased risk of infection during mucosal instrumentation, Upper GI Endoscopy (EGD) should be deferred if possible until neutrophil counts improve.
- Recent upper GI surgery or anatomical alteration: Recent gastrointestinal surgery or structural changes may increase the risk of injury; caution is warranted.
- Bowel obstruction or severe luminal narrowing: Significant obstruction or narrowing in the upper GI tract can make scope passage difficult or dangerous.
- Recent food intake (non fasted state): If the patient has recently eaten or there is retained gastric or esophageal contents, the risk of aspiration is elevated; fasting should be ensured.
Benefits of UGI Endoscopy
Upper gastrointestinal (GI) endoscopy is a widely applied diagnostic and therapeutic tool that provides several key benefits in managing upper GI disorders. Advantages of upper GI endoscopy include the following:
- Precise and Accurate Diagnosis: Through GI Endoscopy it enables direct visualization and biopsy of lesions, providing definitive diagnosis for conditions such as ulcers, Barrett's esophagus, cancer, celiac disease, and inflammatory disorders. This accuracy surpasses non-invasive imaging techniques.
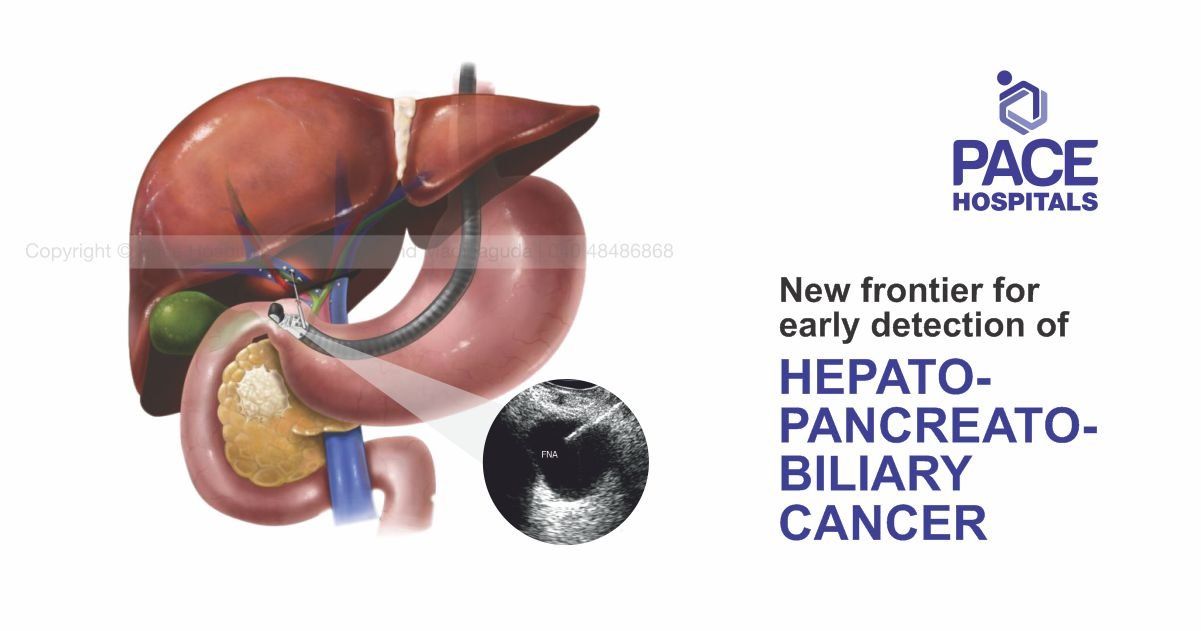
- Early Detection and Staging of GI Cancers: Timely identification of malignant and premalignant lesions improves prognosis by enabling early intervention. Endoscopic ultrasound (EUS) complements the procedure by offering detailed tumor staging and evaluation of surrounding lymph nodes.
- Therapeutic Capability: Apart from diagnosis, Upper GI endoscopy facilitates minimally invasive treatment options such as it helps in bleeding control, polyp removal, stricture dilation, and placement of feeding tubes or stents, reducing the need for surgical interventions.
- Monitoring Disease Progression: Upper GI Endoscopy assists in surveillance of chronic GI diseases, allowing assessment of treatment efficacy and early detection of complications.
- Patient Safety and Efficiency: The procedure has a favorable safety profile with low complication rates and can be performed on an outpatient basis, reducing hospital stay and promoting timely management.
By combining diagnostic precision with therapeutic flexibility, upper GI endoscopy remains a vital and effective tool for gastrointestinal healthcare.
UGI Endoscopy Preparation
Upper Endoscopy procedure preparation is essential to ensure a smooth and safe procedure. Whether you're scheduled for a diagnostic test or a therapeutic intervention, understanding how to prepare for an endoscopy can reduce risks and improve outcomes. Below is a comprehensive guide covering fasting before endoscopy, medication adjustments, and important information to share with the healthcare provider.
How to Prepare for an Upper GI Endoscopy
Upper GI endoscopy is typically performed in an outpatient setting, although it may occasionally be necessary at the bedside or in an operating room, depending on the patient's condition. Preparation includes specific dietary restrictions, medication planning, and sedation management.
Planning ahead is key. It is needed to go through below points:
- It is advised to follow specific fasting instructions.
- It is required to adjust certain medications (especially if the individuals have diabetes or take blood thinners).
- Arrange for someone to accompany the patient, as the patient won’t be able to drive after sedation.
- Discuss any health concerns or past reactions to anesthesia with the referred doctor or gastroenterologist.
Fasting Guidelines
One of the most important steps in Upper GI endoscopy preparation is fasting to ensure that the individual's stomach is empty, which reduces the risk of complications like aspiration.
According to the American Society of Anesthesiologists (ASA):
- It is advised to stop drinking clear liquids at least 2 hours before the procedure.
- It is required to avoid light meals for at least 6 hours before the scheduled date of endoscopy.
- In emergency situations or if patients have delayed gastric emptying (due to diabetes, gastroparesis, etc.), the doctor may alter the timing or type of anesthesia used-or delay the procedure for safety reasons.
Medication Adjustments
Most medications can still be taken before the procedure, usually with a small sip of water. However, some exceptions apply:
- Diabetes medications may need adjustment due to fasting requirements.
- Blood thinners and antiplatelet agents may need to be paused or managed differently. Always follow American Society for Gastrointestinal Endoscopy (ASGE) guidelines or referred doctor's instructions.
- Antibiotic prophylaxis may be necessary for patients at higher risk of infection (e.g., those with heart valve issues).
It is advised to bring a list of all medications and supplements consumed by the patients while taking the appointment.
What to Inform the referred Doctor or Gastroenterologist Before Endoscopy
Open communication with the healthcare provider is essential for a safe procedure. It is required to be sure to tell the referred doctor:
- If patient have any allergies to medications or anesthesia.
- If patients have heart, lung, or bleeding disorders.
- If individual/patient is pregnant or breastfeeding.
- About any previous reactions to sedation or anesthesia.
- If patient had recent surgeries or are currently ill.
This information helps the care team plan for the safest sedation and procedural experience.
Informed Consent
Before the procedure, it will be asked to sign an informed consent form. This document confirms that the patient understands the following:
- The purpose of the upper GI endoscopy.
- The risks and benefits of the procedure.
- The type of sedation that will be used.
- Any alternatives available.
For minors or those unable to consent, a parent or legal guardian must sign on their behalf.
Upper GI Endoscopy Procedure
Upper GI Endoscopy Procedure is done following these steps:
Before the Endoscopy Procedure
- A detailed medical history and physical examination are conducted to evaluate patient suitability for the procedure.
- Patients must disclose all medications (prescription, OTC, supplements), allergies, prior anesthesia reactions, and any bleeding disorders or anticoagulant use.
- Certain medications, particularly blood thinners, may require temporary discontinuation to minimize bleeding risk.
- Patients are instructed to fast for 6 to 8 hours beforehand to ensure the stomach and upper GI tract are empty.
- Arrangements for post-procedure transportation and care are necessary due to sedative effects on alertness and motor functions.
- Informed consent is obtained after a thorough explanation of the procedure benefits, risks, and alternatives.
During the Endoscopy Procedure
- The patient is positioned on the left lateral decubitus (side-lying) position to facilitate endoscope insertion and examination.
- Sedation or anesthesia is administered intravenously to promote relaxation; local throat anesthesia may be applied to reduce the gag reflex.
- The flexible endoscope is carefully introduced through the mouth, passing down the esophagus, into the stomach, and subsequently the duodenum.
- Air insufflation is performed via the endoscope to distend the stomach and duodenum for enhanced visualization of the mucosa.
- Real-time video imaging allows detailed examination and identification of abnormalities.
- Biopsies and therapeutic interventions such as bleeding control and stricture dilation may be performed using instruments passed through the endoscope.
- The procedure duration averages 10 to 20 minutes under sedation.
After the Endoscopy Procedure
- The patient is monitored in a recovery area until sedative effects wear off, typically within 30 to 60 minutes.
- Mild side effects, including throat soreness, bloating, or transient nausea, may occur.
- Post-procedure instructions include abstinence from driving or operating machinery for the day, adherence to specific diet or medication guidelines, and scheduling follow-up for biopsy results.
- Potential complications, though they may rarely occur, include bleeding, perforation, or reactions to sedation, warranting immediate medical attention if symptoms arise.
Complications of UGI Endoscopy
Complications following Upper GI Endoscopy or esophagogastroduodenoscopy (EGD) are very few, with a reported incidence of less than 2%. These complications may be associated with sedation, the mechanical passage of the endoscope, or specific diagnostic and therapeutic procedures. While most adverse events are mild, some may require medical or surgical intervention if not checked properly. Below are the most recognized complications of upper GI endoscopy:
- Sedation-related complications: The most common and potentially serious complications of endoscopy are related to sedation, especially cardiopulmonary complications. These include hypoxemia, hypoventilation, hypotension, arrhythmias, airway obstruction, and aspiration pneumonia. Proper patient monitoring during upper GI endoscopy is essential to reduce these risks.
- Bleeding: In certain situations, bleeding after an Upper GI endoscopy, particularly after mucosal biopsy, occurs in approximately 0.3% of cases. It may occur as hematemesis or bloody output from a gastrostomy tube. Most cases are self-limited, but some may require endoscopic hemostasis or further medical management steps.
- Perforation: Gastrointestinal perforation is a rare but serious complication, occurring in less than 0.3% of EGD procedures. Symptoms include abdominal pain, fever, tachycardia, and distension. Perforation after endoscopy is diagnosed through various abdominal imaging (e.g., X-ray or CT scan), and treatment ranges from conservative management to surgical repair.
- Infection: In certain conditions, infection after endoscopy is uncommon, especially following diagnostic EGD. However, infection risk increases during therapeutic endoscopy or in immunocompromised patients. Signs include fever, pain, or signs of systemic infection, and typically require antibiotic therapy.
- Duodenal hematoma: A duodenal hematoma is a rare complication of upper GI endoscopy, more frequently observed in the case of children. It may lead to nausea, vomiting, abdominal pain, and sometimes bowel obstruction. Management is typically non-surgical, involving bowel rest and observation.
- Aspiration: In some cases, aspiration during endoscopy can occur, especially in patients with impaired swallowing or delayed gastric emptying. It can lead to aspiration pneumonia and requires prompt treatment with supportive care and antibiotics, if necessary.
- Intraluminal hematoma: This rare complication may develop as a result of post-biopsy bleeding during EGD. Symptoms may vary based on size and location, but are usually managed with conservative measures such as observation and rest.
Most endoscopy complications become evident within the first 24 hours of the procedure. Early detection of bleeding, perforation, or infection is crucial for effective treatment and prevention of further complications.
Upper GI Endoscopy Recovery Time
Recovery time following upper gastrointestinal (GI) endoscopy is influenced by several factors, including the type and dose of sedation used, patient age, and underlying medical conditions. On average, patients require about 30 to 60 minutes in a recovery area after the procedure, during which vital signs and consciousness levels are closely monitored to ensure safe awakening from sedatives.
- Recovery can be assessed using standardized scoring systems such as the Modified Aldrete Score (MAS), which evaluates parameters like respiratory function, oxygen saturation, circulation, consciousness, and movement ability. Patients are typically discharged once they achieve full recovery criteria to ensure safety.
- Higher doses of sedatives can prolong recovery time, while factors such as a history of stroke or chronic conditions may also extend the period needed for complete awakening.
- Elderly patients and females have been found to experience longer recovery durations and may have a higher susceptibility to post-procedural nausea or adverse effects.
- Post-recovery, patients are advised to avoid activities requiring full alertness such as driving or operating machinery for at least 12 to 24 hours.
Effective management during the recovery phase is crucial to reducing complications and ensuring patient safety before discharge.
Questions to Ask Your Healthcare Team About the Upper GI Endoscopy Procedure?
- When can I go home after the procedure?
- Will I be under sedation or anesthesia, and how will it affect me afterward?
- When can I eat or drink again after the Upper GI endoscopy?
- What kind of discomfort or side effects should I expect after the procedure?
- How long is the typical recovery time?
- Are there any activities I should avoid after the procedure?
- Do I need someone to accompany me or drive me home?
- What symptoms should I watch for that might indicate a complication?
- When will I receive the results of my endoscopy or biopsy?
- Do I need a follow-up appointment, and when should that be scheduled?
- Will I need further tests or treatments based on the results?
- Are there dietary restrictions I should follow after the procedure?
- Is this procedure both diagnostic and potentially therapeutic?
- How will this endoscopy help in managing my symptoms or condition?
Difference between Upper GI Endoscopy and Colonoscopy
Upper GI Endoscopy vs Colonoscopy
Upper GI Endoscopy and Colonoscopy are two common diagnostic procedures used to examine different parts of the gastrointestinal (GI) tract. They vary in scope, technique, and clinical application. Below are the parameters that help in differentiating Upper GI Endoscopy and Colonoscopy procedure:
| Parameters | GI Endoscopy (Upper Endoscopy / EGD) | Colonoscopy |
|---|---|---|
| Definition | A procedure that uses a flexible tube with a camera to examine the esophagus, stomach, and upper small intestine through the mouth. | It is a diagnostic and therapeutic procedure used to examine the colon and rectum using a scope inserted through the rectum. |
| Common indications | GERD, ulcers, upper GI bleeding, difficulty swallowing, and upper abdominal pain. | Colon cancer screening, polyps, chronic diarrhea, lower GI bleeding, colitis. |
| Invasiveness | Minimally invasive – involves passing a scope via the mouth. | Minimally invasive – involves passing a scope via the rectum. |
| Recovery time | Quick recovery – usually same-day discharge. | Quick recovery – most patients return to normal activities within 24 hours. |
| Preparation needed | Requires fasting for 6–8 hours prior to the procedure. | Requires bowel cleansing (laxatives) the day before. |
| Complications | Rare – may include sore throat, perforation, or bleeding. | Rare – risks include bleeding, perforation, and reaction to sedation. |
Upper GI Endoscopy Cost in Hyderabad, India
The cost of UGI Endoscopy in Hyderabad generally ranges from ₹4,000 to ₹12,000 (approximately US $50 – US $145).
The exact UGI endoscopy test price varies depending on factors such as whether the procedure is diagnostic or therapeutic, whether a biopsy is required, use of sedation, gastroenterologist expertise, and the hospital facilities chosen — including cashless treatment options, TPA corporate tie-ups, and assistance with medical insurance approvals wherever applicable.
Cost Breakdown According to Type of Procedure
- Basic Diagnostic UGI Endoscopy (No Sedation / No Biopsy) – ₹4,000 – ₹6,000 (US $50 – US $72)
- UGI Endoscopy with Biopsy / Minor Therapeutic Procedure – ₹6,000 – ₹9,000 (US $72 – US $108)
- Sedated / Premium UGI Endoscopy – ₹9,000 – ₹12,000 (US $108 – US $145)
Frequently Asked Questions (FAQs) on Upper GI Endoscopy
What diseases can be detected by an Upper GI endoscopy?
An endoscopy is widely used to detect various gastrointestinal diseases including peptic ulcers, Gastroesophageal reflux disease (GERD), Crohn’s disease, infections like Helicobacter pylori, esophageal varices, and GI cancers. It allows direct visualization and biopsy of suspicious lesions, helping to diagnose inflammatory conditions, strictures, and sources of bleeding. Therapeutic interventions, such as polyp removal, can also be performed during endoscopy.
Which Is the best hospital for UGI Endoscopy in Hyderabad, India?
PACE Hospitals, Hyderabad is regarded as one of the most trusted centres for upper GI diagnostic and therapeutic endoscopy. Our expert gastroenterologists use high-definition endoscopes, safe sedation techniques, and minimally invasive protocols to ensure quick, accurate, and comfortable diagnosis.
With advanced endoscopy suites, dedicated recovery units, and seamless patient-support services, PACE Hospitals ensures safe, efficient, and high-quality care — supported by cashless facility options, TPA corporate tie-ups, and assistance with medical insurance processing for eligible patients.
Can Upper GI endoscopy cause infection?
While endoscopy is generally safe, there is a small risk of infection, primarily if proper sterilization protocols are not followed. Inadequate cleaning of endoscopic equipment can lead to transmission of infections such as hepatitis B, hepatitis C, HIV, and other bacterial infections. To resolve this risk, healthcare facilities adhere to strict infection control measures, including thorough disinfection and sterilization of instruments between procedures which is essential. Patients should ensure that their healthcare providers follow established safety protocols to minimize infection risks.
Why is Upper GI endoscopy required?
An Upper GI Endoscopy test is conducted to diagnose, monitor, and treat various conditions affecting the digestive system and gastrointestinal tract. It is particularly beneficial for investigating symptoms like persistent abdominal pain, unexplained weight loss, gastrointestinal bleeding, and difficulty swallowing. Upper GI Endoscopy helps for direct visualization of the esophagus, stomach, and intestines, enabling healthcare providers to identify abnormalities such as ulcers, tumors, inflammation, or bleeding sites. Additionally, it facilitates therapeutic interventions like polyp removal, dilation of strictures, and stent placements.
Does Upper GI endoscopy have side effects?
The side effects of endoscopy may include sore throat, bloating, mild abdominal discomfort, or nausea. Serious complications are generally rare but can include bleeding or perforation. Most side effects are resolved quickly without intervention.
What Is the UGI Endoscopy test price in Hyderabad at PACE Hospitals?
At PACE Hospitals, Hyderabad, the cost of UGI Endoscopy typically ranges from ₹3,500 to ₹10,000 and above (approximately US $45 – US $120), depending on:
- Type of procedure (diagnostic vs biopsy vs therapeutic)
- Whether sedation is required
- Gastroenterologist expertise
- Use of advanced endoscopic equipment
- Day-care or short-stay requirement
- Additional diagnostics or pathology tests
For simple diagnostic procedures, costs fall at the lower end, whereas sedated, biopsy-based, or therapeutic endoscopies fall toward the higher end.
After a gastroenterology consultation and clinical evaluation, our specialists will provide a personalised procedure plan and a transparent cost estimate based on your clinical needs.
What is RUT positive in Upper GI endoscopy?
Rapid Urease Test (RUT) positivity during endoscopy indicates the existence of Helicobacter pylori infection, a common cause of gastritis and peptic ulcers. Biopsy specimens from the stomach lining are tested for urease enzyme activity.
Is Upper GI Endoscopy painful?
Upper GI Endoscopy is generally not painful. Most patients experience mild discomfort, such as a sensation of pressure or gagging during the procedure. Sedation or topical anesthetics are often used to minimize discomfort and improve tolerance. After the procedure, some may have a mild sore throat or bloating effect, but these symptoms usually resolve quickly.
Will I be asleep during upper endoscopy?
Upper endoscopy is usually performed under sedation, which ranges from mild sedation (patient awake but relaxed) to moderate or deep sedation (patient may be asleep). Sedation ensures patient comfort and reduces anxiety during the procedure. The exact sedation level depends on patient factors and physician’s discretion.
Is Upper GI endoscopy dangerous?
Endoscopy is generally safe, with a low risk of complications such as bleeding, perforation, or adverse sedation reactions. Complication rates are around 0.1% for upper endoscopy and slightly higher for colonoscopy. Risks increase with patient comorbidities and the complexity of the procedure.
Does Upper GI endoscopy detect cancer?
Yes, Upper GI endoscopy is a valuable tool in detecting cancers of the gastrointestinal tract. It helps for direct visualization of abnormal growths, lesions, or tissue changes that may indicate possibility of cancer. During the procedure, biopsies can be taken from suspicious areas for histopathological examination, aiding in the diagnosis of conditions like esophageal, stomach, and colorectal cancers. Through early detection with endoscopy it can significantly improve treatment outcomes and survival rates.
Is Upper GI endoscopy done empty stomach?
Yes, fasting is typically required before an endoscopy to ensure clear visualization of the various parts of gastrointestinal tract and to reduce the risk of aspiration. For upper gastrointestinal endoscopy, patients are usually instructed to fast for at least 6–8 hours prior to the procedure. This fasting period makes the stomach empty, providing a clearer view and minimizing the risk of complications. Patients should follow specific fasting instructions provided by experienced GI healthcare expert to ensure the best possible results.
What to drink after Upper GI endoscopy?
After an endoscopy test, it's essential to stay hydrated. Patients are generally advised to start with small sips of water once the sedative effects have worn off and swallowing is safe. Further, they can progress to other clear liquids like broth or diluted fruit juices. It’s crucial to avoid consuming hot beverages initially, as the throat may be numbed from the procedure. Patients should follow specific post-procedure instructions provided by their healthcare provider to ensure a safe recovery.
What to eat after Upper GI endoscopy?
Post-procedure dietary recommendations vary depending on the type of endoscopy performed and the patient's individual health condition. Generally, after an upper GI endoscopy, patients are advised to resume eating soft, bland foods once they feel ready, avoiding spicy, acidic, or hard-to-digest items initially. It's crucial to follow the specific dietary guidelines provided by the gastroenterologists to ensure proper recovery.
Can Upper GI endoscopy detect pregnancy?
Upper GI Endoscopy is not a method used to detect pregnancy. Pregnancy is typically confirmed through urine or blood tests measuring hCG levels. However, if a pregnant woman requires an endoscopic procedure, special considerations are taken to minimize risks to both the mother and the fetus. Endoscopic procedures during pregnancy are generally safe when performed with appropriate precautions and under the guidance of experienced medical professionals.
Why repeat Upper GI endoscopy in 3 months?
Repeating endoscopy within a short timeframe may be recommended to monitor the progression of a known condition, assess the effectiveness of a treatment, or investigate persistent or new symptoms. It can help confirm healing or detect early recurrence.