Pancreatic Pseudocyst Treatment in Hyderabad, India
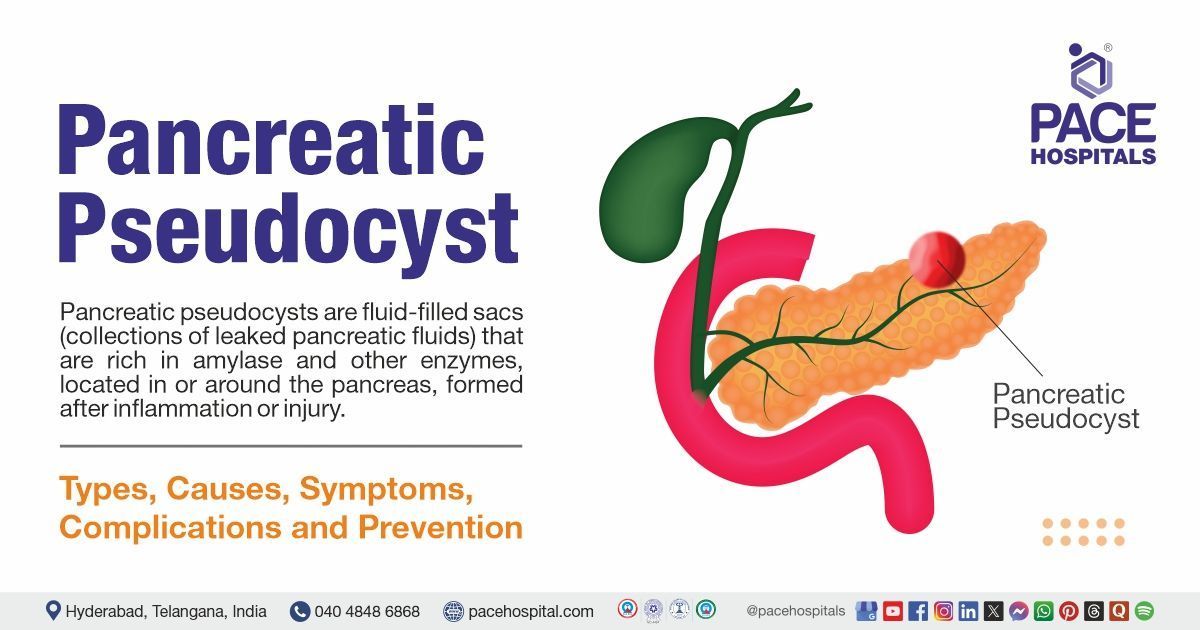
PACE Hospitals is recognized as one of the best centers for pancreatic pseudocyst treatment in Hyderabad, Telangana, India. Our expert team of gastroenterologists, surgeons, endocrinologists, and dietitians offers a multidisciplinary approach to diagnose and manage pseudocysts—fluid-filled sacs that often arise from pancreatitis. Using advanced imaging tools like MRI, CT scan, and endoscopic ultrasound (EUS), we assess cyst characteristics and determine the most suitable treatment.
Treatment options are tailored to each patient and may include medications, enzyme therapy, drainage procedures, or surgery. Our focus is on relieving symptoms, preventing complications, and improving quality of life through expert care and continuous support.
Book Appointment for Pancreatic Pseudocyst Treatment
Pancreatic Pseudocyst Treatment Online Appointment
Thank you for contacting us. We will get back to you as soon as possible. Kindly save these contact details in your contacts to receive calls and messages:-
Appointment Desk: 04048486868
WhatsApp: 8977889778
Regards,
PACE Hospitals
HITEC City and Madeenaguda
Hyderabad, Telangana, India.
Oops, there was an error sending your message. Please try again later. Kindly save these contact details in your contacts to receive calls and messages:-
Appointment Desk: 04048486868
WhatsApp: 8977889778
Regards,
PACE Hospitals
HITEC City and Madeenaguda
Hyderabad, Telangana, India.
Why Choose PACE Hospitals for Pancreatic Pseudocyst Treatment?

Advanced Diagnostic Facilities: CT scan, MRI with MRCP, EUS, Pancreatic Function Tests (PFTs)
Expert Gastroenterologists, Endocrinologists & GI Surgeons in Hyderabad
Minimally Invasive and Surgical Treatment Options
Affordable & Transparent Pancreatitis Treatment with Insurance & Cashless Options
The diagnosis of a pancreatic pseudocyst requires a combination of clinical evaluation, detailed history taking, and confirmatory imaging. Unlike true cysts, pseudocysts lack an epithelial lining and often arise as complications of acute or chronic pancreatitis.
Their presentation can vary depending on size, location, and whether complications such as infection, haemorrhage, or rupture are present. As such, careful consideration of various clinical parameters is crucial before proceeding with diagnostic tests.
Pancreatic Pseudocyst Diagnosis
Based on the above evaluation, doctors select the most appropriate diagnostic tests to confirm the presence of a pseudocyst and guide treatment:
Clinical Assessment
- Presented Signs and Symptoms
- Recent History of Pancreatitis or Pancreatic Trauma
- General Health and Risk Profile
- Medical and Medication History
- Focused Physical Examination
Imaging Studies (Confirmatory)
- Abdominal Ultrasound
- Contrast-enhanced CT scan (CECT)
- MRI/MRCP
- Endoscopic Ultrasound (EUS)
Laboratory Investigations
- Serum amylase/lipase:
- White blood cell count & CRP
- Serum bilirubin and liver enzymes
- Tumor markers (CEA, CA 19-9)
Pancreatic Fluid Analysis (if aspirated)
- Amylase-rich fluid
- Culture and Gram Stain
- Cytology
Clinical Assessment
Before ordering diagnostic investigations, the treating physician, typically a gastroenterologist or a surgical specialist, will evaluate the following factors to determine the likelihood of a pancreatic pseudocyst and to guide the appropriate workup:
Presented Signs and Symptoms
Patients with pancreatic pseudocysts may present with persistent abdominal pain, typically in the epigastric region and often radiating to the back. Other common symptoms include abdominal fullness or a palpable mass, early satiety, bloating, nausea, vomiting, low-grade fever (especially if infection is present), and unintentional weight loss. A recent history of acute or chronic pancreatitis is frequently noted, as pseudocysts generally develop as a complication of these conditions. Because these symptoms are not specific and can mimic other gastrointestinal or intra-abdominal conditions, physicians maintain a high index of suspicion for pancreatic pseudocyst in any patient with a relevant history and persistent abdominal complaints. The diagnosis is particularly considered in individuals who have recently recovered from pancreatitis but continue to exhibit gastrointestinal symptoms or systemic signs of inflammation.
Recent History of Pancreatitis or Pancreatic Trauma
A recent episode of acute pancreatitis, particularly within the previous 4 to 6 weeks, is a strong clinical clue for the development of a pancreatic pseudocyst. These fluid-filled collections most often arise as a complication of acute pancreatitis, especially the necrotizing form, but may also result from chronic pancreatitis or direct pancreatic trauma, such as blunt abdominal injury or surgical procedures involving the pancreas. Clinicians pay close attention to the timing between the initial pancreatic insult and the persistence or recurrence of symptoms, as this helps differentiate pancreatic pseudocysts from other types of fluid collections, including acute peripancreatic fluid collections (APFCs) and walled-off necrosis (WON). Accurate identification is essential because each type of collection has a different natural history, treatment approach, and risk of complications.
General Health and Risk Profile
When evaluating a patient for a possible pancreatic pseudocyst, physicians carefully assess the individual’s general health and risk profile. Factors such as age and immune status are important, as older or immunocompromised patients may have a higher risk of complications like infection or bleeding. Lifestyle habits, including a history of chronic alcohol use and smoking, are also significant, as they are major contributors to both acute and chronic pancreatitis, the underlying conditions that commonly lead to pseudocyst formation.
Medical and Medication History
A thorough medical and medication history is essential when evaluating a patient for a pancreatic pseudocyst. Physicians look for a history of recurrent episodes of pancreatitis, which may indicate chronic pancreatic injury and increase the risk of pseudocyst formation. Prior abdominal trauma or surgeries, as well as past interventions for pancreatic conditions, such as stent placements or drainage procedures, can also contribute to or complicate pseudocyst development. In addition, clinicians review the patient’s current and past medications, particularly those known to cause pancreatic inflammation or fluid retention, such as corticosteroids and immunosuppressants. This step is crucial not only for identifying potential causes, but also for ruling out other cystic pancreatic lesions. It also helps assess the likelihood of complications like haemorrhage or infection, which can significantly impact management decisions.
Focused Physical Examination
A physical exam is conducted to assess for clinical signs suggestive of a pseudocyst and related complications:
Imaging tests
Abdominal Ultrasound
It is often the initial imaging modality used to detect pancreatic pseudocysts due to its accessibility and non-invasive nature. It can identify fluid-filled cystic lesions in or near the pancreas, especially when they are large and well-defined. While it provides limited detail compared to cross-sectional imaging, it is useful for monitoring known pseudocysts and evaluating for complications such as rupture or infection.
Contrast-enhanced CT scan (CECT)
It is considered the most definitive imaging test for diagnosing pancreatic pseudocysts. It provides high-resolution images that clearly show the size, location, wall thickness, and internal contents of the cyst. CECT is especially valuable in detecting complications such as haemorrhage, infection, or compression of adjacent structures, and it helps differentiate pseudocysts from other pancreatic masses or neoplasms.
MRI/MRCP (Magnetic Resonance Imaging with Magnetic Resonance Cholangiopancreatography)
This offers excellent soft tissue contrast and detailed imaging of the pancreatic ductal system. It helps distinguish pseudocysts from cystic tumors or walled-off necrosis, and is particularly useful when CT findings are inconclusive. MRCP can non-invasively visualize any communication between the pseudocyst and the main pancreatic duct, which is critical for planning treatment.
Endoscopic Ultrasound (EUS)
It is a highly sensitive tool for evaluating small or equivocal pancreatic cystic lesions that may not be clearly visible on CT or MRI. It allows for close-up imaging of the cyst from within the gastrointestinal tract and can guide fine-needle aspiration (FNA) to obtain fluid samples for biochemical, cytological, or microbial analysis. EUS is also used to guide drainage procedures when intervention is required.
Laboratory Investigations
Serum Amylase and Lipase levels
These are typically elevated during acute episodes of pancreatitis, which often precede the formation of pancreatic pseudocysts. While these enzymes may return to normal in chronic or late stages, persistently high levels can indicate ongoing pancreatic inflammation. Their presence supports a recent or active pancreatic insult, helping clinicians link the current cystic lesion to a pancreatitis-related origin.
White Blood Cell (WBC) Count and C-Reactive Protein (CRP)
These are inflammatory markers that help detect infection or ongoing inflammation within a pseudocyst. Elevated WBC or CRP levels, particularly in a patient with fever and abdominal symptoms, raise suspicion for an infected pseudocyst or abscess formation. These markers also assist in monitoring the response to medical or interventional treatment.
Serum Bilirubin and Liver Enzymes (such as ALT, AST, ALP, and GGT)
These are assessed when there is concern for biliary obstruction caused by a large pseudocyst compressing the bile duct. Elevated levels may point to cholestasis or biliary involvement, prompting further imaging or intervention to relieve the obstruction.
Tumor Markers such as CEA and CA 19-9
These are not routinely elevated in simple pseudocysts but are measured when the cyst has atypical features on imaging, such as septations, solid components, or irregular walls. Elevated levels of these markers may suggest a neoplastic cyst or cystic pancreatic tumor rather than a benign pseudocyst, guiding further diagnostic evaluation and possibly surgical management.
Pancreatic Fluid Analysis (if aspirated)
Amylase-rich fluid
It is obtained through aspiration and is a hallmark of pancreatic pseudocysts, as these lesions often contain enzyme-rich fluid leaked from the pancreatic duct. High amylase levels in the aspirate strongly support a diagnosis of pseudocyst rather than other cystic lesions, such as mucinous neoplasms, which typically have low enzyme content.
Culture and Gram Stain
Culture and Gram Stain of the aspirated fluid are critical for identifying infection within the pseudocyst, especially if the patient presents with fever, leucocytosis, or signs of sepsis. A positive culture confirms the presence of bacteria, guiding the need for antibiotics or drainage, while Gram stain offers a rapid preliminary identification of the causative organism.
Cytology
It is performed on aspirated fluid to examine cellular characteristics and rule out malignancy. Although pseudocysts are non-neoplastic, some cystic pancreatic tumors can mimic their appearance on imaging. The presence of atypical or malignant cells in cytology prompts further investigation, possibly shifting the diagnosis away from pseudocyst toward a cystic neoplasm requiring surgical evaluation.
Treatment Considerations
Before selecting the appropriate treatment for a pancreatic pseudocyst, healthcare professionals carefully evaluate several clinical factors to determine the most effective and safe approach for each patient. Key considerations include:
- Size and Location of the Pseudocyst: Larger cysts (>5–6 cm) or those causing symptoms often require intervention; location determines the most suitable drainage route.
- Presence of Symptoms or Complications: Symptomatic pseudocysts or those causing infection, obstruction, or bleeding are more likely to need active treatment.
- Duration of the Pseudocyst: Pseudocysts persisting for more than 4–6 weeks are more likely to mature with a defined wall and may be safely drained.
- Patient’s Overall Health and Surgical Risk: Minimally invasive options are preferred in high-risk surgical patients or those with significant comorbidities.
- Suspicion of Malignancy or Atypical Features: Cysts with irregular walls, solid components, or atypical imaging findings may require resection and histopathological evaluation.
Treatment for pancreatic pseudocyst is initiated once the diagnosis is confirmed and the cyst becomes symptomatic or complicated. The management strategy depends on factors such as cyst size, location, duration, and presence of infection or obstruction. Here are some of the treatment options that may be considered for managing a pancreatic pseudocyst:
Conservative Management
Conservative management of pancreatic pseudocyst is aimed at relieving symptoms, promoting spontaneous resolution, and preventing complications in stable patients. Here are some of the non-surgical treatment approaches that may be considered for the conservative management of a pancreatic pseudocyst:
Observation and Monitoring
Small (<6 cm), asymptomatic pseudocysts are often managed conservatively with regular follow-up imaging to monitor for resolution or progression. Most resolve spontaneously if there is no ductal obstruction or infection.
Nutritional Support
Patients are advised to follow a low-fat diet and maintain adequate hydration. In cases of malnutrition, dietitian-guided nutritional support may be necessary, especially if the pseudocyst is associated with chronic pancreatitis.
Management of Underlying Pancreatitis
Addressing the underlying cause (e.g., alcohol cessation, treatment of gallstones, or discontinuation of offending medications) helps prevent recurrence and promotes resolution of the pseudocyst.
Endoscopic Interventions
Endoscopic interventions are minimally invasive procedures used to manage pancreatic pseudocysts, especially in cases with ductal obstruction or complications. They offer symptom relief and may prevent the need for surgery in appropriately selected patients. Here are some of the endoscopic treatment options that may be considered for managing a pancreatic pseudocyst in select cases with ductal involvement or complications:
Endoscopic Ultrasound-Guided Drainage (EUS-Guided Cystogastrostomy/Cystoduodenostomy)
This is the preferred minimally invasive approach for symptomatic or enlarging pseudocysts. It involves creating a connection between the pseudocyst and the stomach or duodenum under EUS guidance for internal drainage.
ERCP (Endoscopic Retrograde Cholangiopancreatography)
It is indicated if the pseudocyst communicates with the main pancreatic duct or if there is ductal obstruction. ERCP may involve the placement of pancreatic duct stents to improve drainage.
Transpapillary Drainage
It is performed when the pseudocyst is in communication with the ductal system and located near the pancreatic head. A stent is placed via
ERCP to drain the pseudocyst into the duodenum.
Surgical Management
Surgical management is considered when conservative and endoscopic treatments are unsuccessful or complications develop. It is typically reserved for patients with persistent symptoms, obstructive features, or suspicion of malignancy. Here are some of the surgical treatment options that may be considered for managing a pancreatic pseudocyst when less invasive approaches are ineffective or complications are present:
Cystogastrostomy
A surgical procedure that creates an opening between the pseudocyst and the posterior wall of the stomach to allow continuous internal drainage. This is typically chosen when the pseudocyst is adherent to the posterior wall of the stomach and easily accessible via this route. It is ideal for pseudocysts located in the head or body of the pancreas that bulge into the stomach.
Cystojejunostomy
It is preferred for pseudocysts located in the body or tail of the pancreas. A loop of the jejunum is connected to the pseudocyst to facilitate drainage. This approach is selected when the pseudocyst is not amenable to drainage into the stomach or duodenum, particularly for deep-seated or multiple cysts in the distal pancreas.
Cystoduodenostomy
This is done when the pseudocyst is adjacent to the duodenum, allowing for drainage into the intestinal tract. It is chosen for pseudocysts located near the pancreatic head that are in proximity to the duodenum, making it a direct and effective route for drainage.
Resection (e.g., Distal Pancreatectomy)
It is reserved for complicated cases or when malignancy cannot be ruled out. Surgical removal of the pseudocyst along with part of the pancreas may be necessary. This is indicated when the pseudocyst has suspicious features (e.g., thickened walls or solid components), is recurrent, or is associated with non-functioning or diseased pancreatic tissue.
Pancreatic Pseudocyst Treatment Cost in Hyderabad, India
The cost of Pancreatic Pseudocyst Treatment in Hyderabad generally ranges from ₹1,000 to ₹1,25,000 and above (approx. US $12 – US $1,500).
The exact cost varies depending on the size of the pseudocyst, presence of infection or complications, required diagnostic tests (CT, MRI, ultrasound, EUS), type of treatment (medical therapy, endoscopic drainage, or surgical drainage), hospitalization, and hospital facilities — including cashless insurance, TPA corporate tie-ups, and support for medical insurance wherever applicable.
Cost Breakdown According to Type of Pancreatic Pseudocyst Treatment
- Gastroenterologist / HPB Specialist Consultation – ₹1,000 – ₹2,000 (US $12 – US $24)
- Blood Tests (CBC, LFT, Amylase, Lipase) – ₹900 – ₹2,200 (US $11 – US $26)
- Ultrasound Abdomen – ₹1,000 – ₹2,500 (US $12 – US $30)
- Contrast CT Abdomen – ₹4,500 – ₹9,000 (US $54 – US $108)
- MRI Abdomen / MRCP – ₹4,500 – ₹10,000 (US $54 – US $120)
- Endoscopic Ultrasound (EUS) – ₹8,500 – ₹18,000 (US $100 – US $215)
- EUS-Guided Aspiration / Cyst Drainage – ₹12,000 – ₹28,000 (US $145 – US $335)
- Endoscopic Transgastric / Transduodenal Drainage – ₹30,000 – ₹55,000 (US $360 – US $660)
- Surgical Cystogastrostomy / Cystojejunostomy – ₹65,000 – ₹1,25,000 (US $780 – US $1,500)
- Hospitalization (2–5 Days) – ₹8,000 – ₹25,000 (US $95 – US $300)
- Medical Management (Antibiotics, Enzyme Therapy, Pain Relief) – ₹1,000 – ₹5,000 (US $12 – US $60)
- Follow-up Imaging (Ultrasound / CT) – ₹1,000 – ₹2,500 (US $12 – US $30)
Frequently Asked Questions (FAQs) on Pancreatic Pseudocyst
What are the pancreatic pseudocyst causes?
The most common causes are acute or chronic pancreatitis, abdominal trauma, or pancreatic ductal injury. Alcohol abuse and gallstones are common underlying triggers.
Which Is the best hospital for Pancreatic Pseudocyst Treatment in Hyderabad, India?
PACE Hospitals, Hyderabad, is one of the most trusted centres for diagnosing and treating pancreatic pseudocysts, offering advanced gastroenterology, hepatobiliary, and interventional expertise under one roof.
We provide guidance through experienced gastroenterologists, HPB surgeons, interventional radiologists, and endoscopy specialists treat:
Post-pancreatitis pseudocysts
Large symptomatic pseudocysts
Infected pseudocysts
Pseudocysts causing pain, vomiting, jaundice, or gastric obstruction
Recurrent or complex pseudocysts
Pseudocysts associated with chronic pancreatitis
With EUS-guided drainage, endoscopic cystogastrostomy, CT/MRI, minimally invasive surgical procedures, and dedicated ICU support, PACE Hospitals provides safe, accurate, and patient-focused treatment — supported by cashless insurance, TPA tie-ups, and seamless documentation services.
What are the typical symptoms of a pancreatic pseudocyst?
Many pseudocysts are asymptomatic, but when symptoms occur, they may include abdominal pain, bloating, nausea, vomiting, and a palpable abdominal mass. In severe cases, jaundice or fever may develop due to complications.
Can pancreatic pseudocysts lead to complications?
Yes. Potential complications include infection, rupture, haemorrhage, compression of nearby organs, and pancreatic duct obstruction. Rarely, they may mimic or mask pancreatic tumours.
How much does Pancreatic Pseudocyst surgery cost in Hyderabad at PACE Hospitals?
At PACE Hospitals, Hyderabad, the cost of pancreatic pseudocyst surgery typically ranges from ₹1,000 to ₹1,15,000 and above (approx. US $12 – US $1,380), making it an affordable and advanced option for pancreatic care. However, the final cost depends on:
- Size and location of the pseudocyst
- Need for CT, MRI, EUS, or aspiration
- Medical treatment vs. endoscopic drainage vs. surgery
- Presence of infection or complications
- Type of drainage (EUS-guided, endoscopic, or surgical)
- Duration of hospital stay
- Follow-up imaging and long-term monitoring
Smaller, uncomplicated pseudocysts treated with observation or medical therapy fall in the lower range, while large or complicated pseudocysts requiring endoscopic or surgical drainage fall toward the higher end.
After clinical assessment, imaging, and specialist consultation, our HPB and gastroenterology team will provide a personalised treatment plan and a transparent cost estimate based on the pseudocyst’s characteristics.
What is the haemorrhagic pancreatic pseudocyst?
A haemorrhagic pancreatic pseudocyst is a rare but serious complication in which a pseudocyst bleeds due to erosion into nearby blood vessels. It can lead to sudden abdominal pain, shock, or gastrointestinal bleeding and requires urgent medical or surgical intervention.
What is the difference between walled-off ‘pancreatic necrosis and pseudocyst?
Walled-off pancreatic necrosis (WON) and pancreatic pseudocyst are both late complications of pancreatitis but differ in content and structure. A pseudocyst contains only fluid and has a well-defined fibrous wall, typically forming after acute pancreatitis. In contrast, WON contains both fluid and necrotic (dead) tissue and develops after necrotizing pancreatitis. Imaging helps differentiate them, as WON appears more hetero geneous due to solid debris.
At what size does a pancreatic pseudocyst require treatment?
Pseudocysts larger than 5–6 cm, especially if symptomatic or persistent beyond 4–6 weeks, are typically evaluated for drainage or surgical intervention. Smaller, asymptomatic cysts may be monitored conservatively.
How is a pancreatic pseudocyst diagnosed?
Diagnosis is usually made using imaging studies such as abdominal ultrasound, CT scan or MRI. Endoscopic ultrasound (EUS) can also help assess cyst characteristics and guide drainage.
What are the risk factors for developing a pancreatic pseudocyst?
Risk factors include recurrent or severe pancreatitis, heavy alcohol use, gallstones, abdominal trauma, pancreatic surgery, and ductal disruptions.
How are pancreatic pseudocysts treated?
Treatment depends on the size, location, symptoms, and complications. Options include conservative management, endoscopic drainage, percutaneous drainage, or surgical intervention.
How has the trend in managing pancreatic pseudocysts shifted in recent years?
There has been a notable shift towards conservative management of pancreatic pseudocysts, attributed to increased success rates and safety of non-invasive procedures. Endoscopic drainage, in particular, is associated with better healthcare resource utilization during hospital stays, although mortality rates remain comparable to other interventions.
Is a pancreatic pseudocyst dangerous during pregnancy?
A pseudocyst can be risky if it becomes large, infected, or ruptures. It may pose complications for both mother and foetus, so close monitoring and a multidisciplinary approach are essential.
Can children get pancreatic pseudocysts?
Children can develop pancreatic pseudocysts, most commonly after abdominal trauma, such as a bicycle handlebar injury, or as a complication of acute pancreatitis.