Prostate Cancer Treatment in Hyderabad | Surgery and Cost
We Pace Hospitals, have team of the best prostate cancer specialist doctors, medical and surgical oncologist, laser and laparoscopic urologist and robotic urology surgeons in Hyderabad. They are expert in performing:
- Open radical prostatectomy
- Radical laparoscopic prostatectomy
- Robot-assisted laparoscopic radical prostatectomy
- Transurethral resection of the prostate (TURP)
- Pelvic lymphadenectomy
- Bilateral orchiectomy
Book Appointment for Prostate Cancer Treatment
Prostate Cancer Treatment Enquiry
We are equipped with “The World’s First Universal Surgical Robotic System”, State-of-the-art facility, world-class laser treatment equipment offering comprehensive treatment for prostate cancer and its complications.
We are one of the advanced prostate cancer treatment hospital in India backed up with team of best prostate cancer specialist doctors, medical oncologists, laser and laparoscopic urologist, radiation oncologists, paramedical staff, dietitian and physiotherapist in India. Our doctors are experts in diagnosing and treating conditions related to the male and female urinary tract and the male reproductive organs.
Diagnosis of Prostate Cancer
The prostate gland is a part of the male reproductive system, it is about the size of a walnut and surrounds part of the urethra and situated in front of the rectum, just below the bladder. The following diagnostic tests used to detect prostate cancer:
Physical Examination
– Doctor will first take the medical history, health habits, past illness and treatments then will do the physical examination of the body to check the lump or any other signs of disease
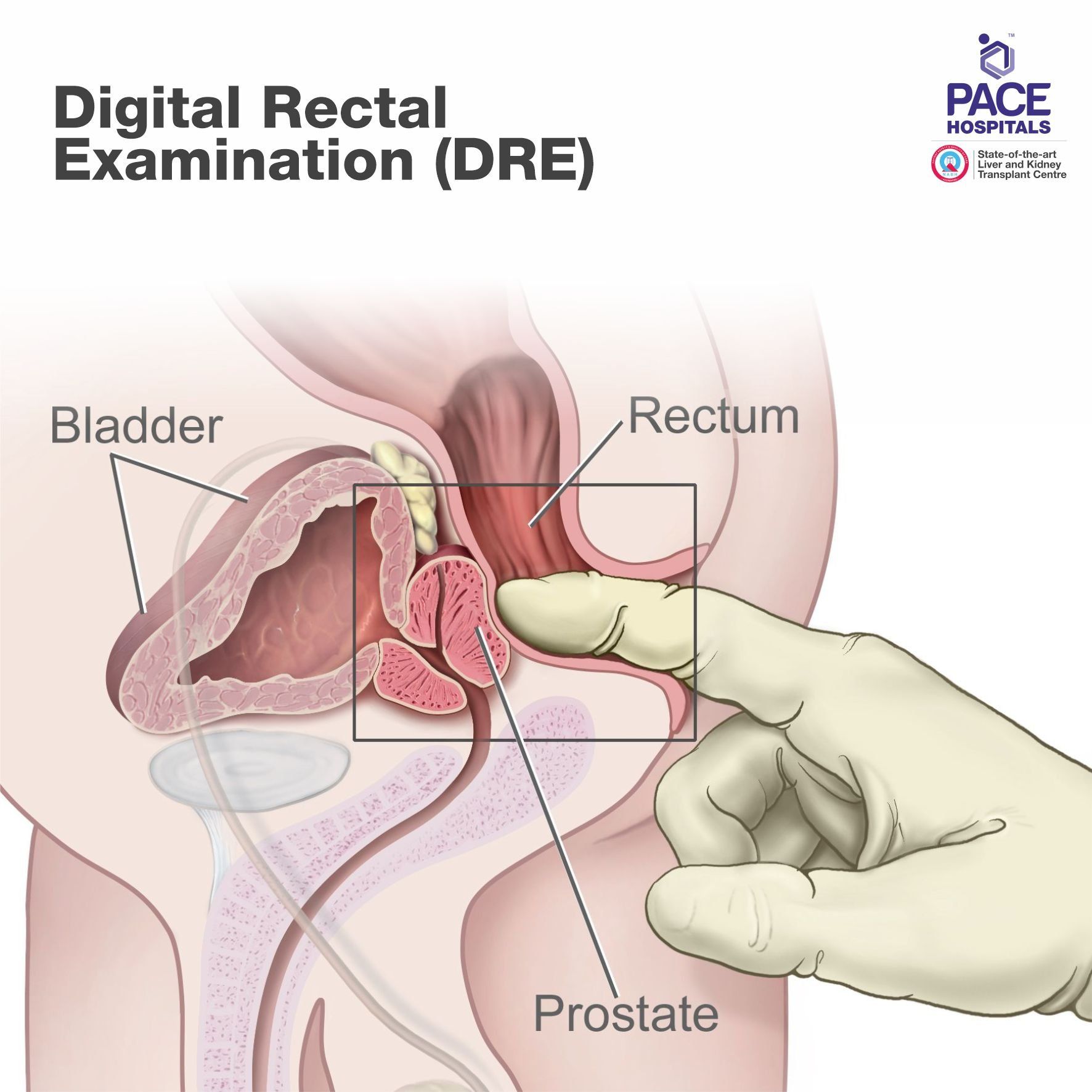
Digital rectal examination (DRE) - The doctor inserts a gloved, lubricated finger into the rectum and feels the prostate through the rectal wall to check for abnormal areas or lumps.
Prostate-specific antigen (PSA) test: Prostate-specific antigen, is a protein produced by the prostate gland. The Prostate-specific antigen test measures the level of PSA in a man’s blood. The blood level of PSA is often elevated in men with prostate cancer, apart from this other non-cancerous conditions such as prostatitis, benign prostatic hyperplasia or enlargement of the prostate can cause an elevation in PSA level.
Transrectal magnetic resonance imaging (MRI): A transrectal MRI is done to find out if the cancer has spread outside the prostate into nearby tissues. This procedure is also called nuclear magnetic resonance imaging (NMRI).
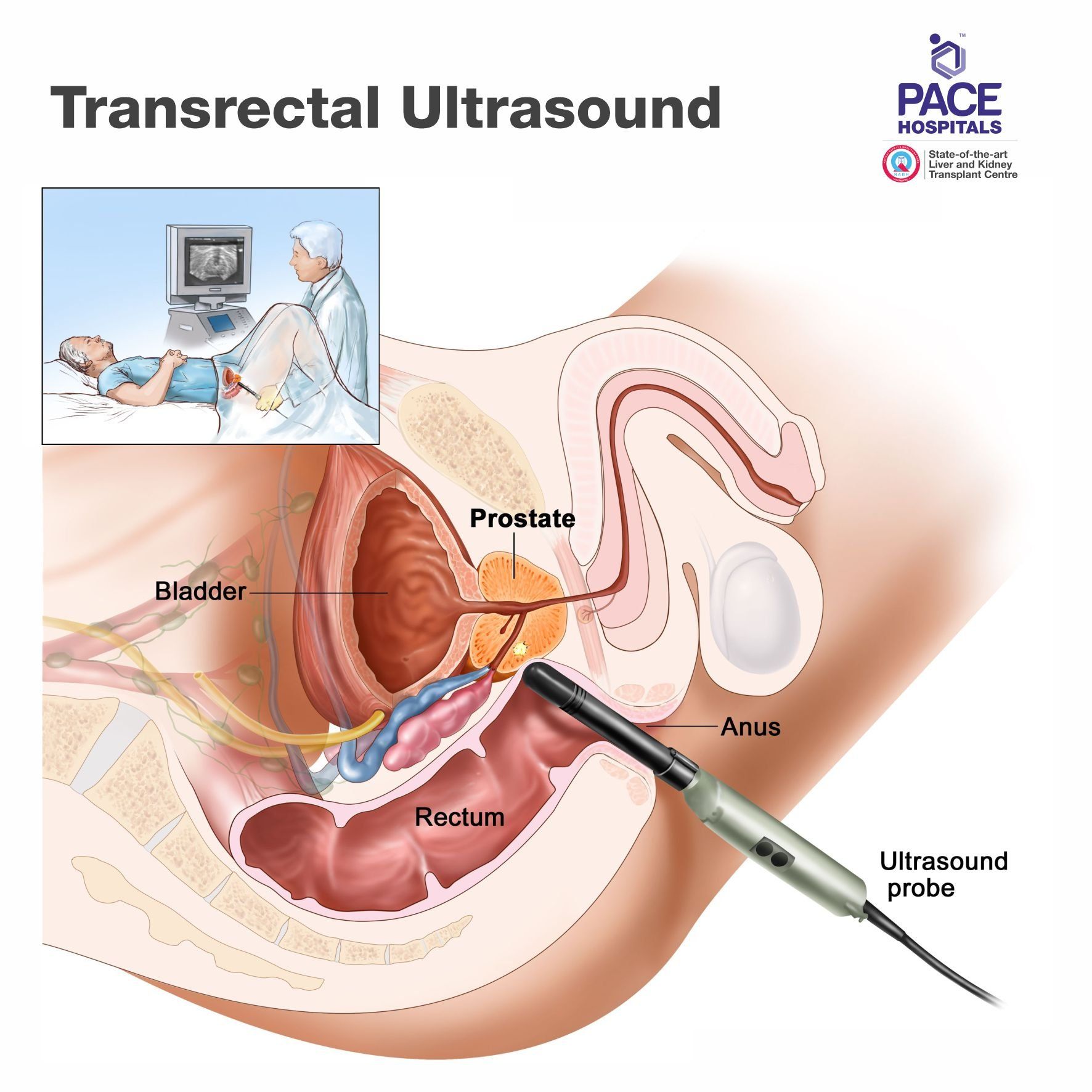
Transrectal ultrasound:
Transrectal ultrasound is used to look for abnormalities in the rectum and nearby structures. An ultrasound probe is inserted into the rectum to check the prostate. The probe bounces sound waves off body tissues to make echoes that form a sonogram of the prostate. It is also called as endorectal ultrasound.
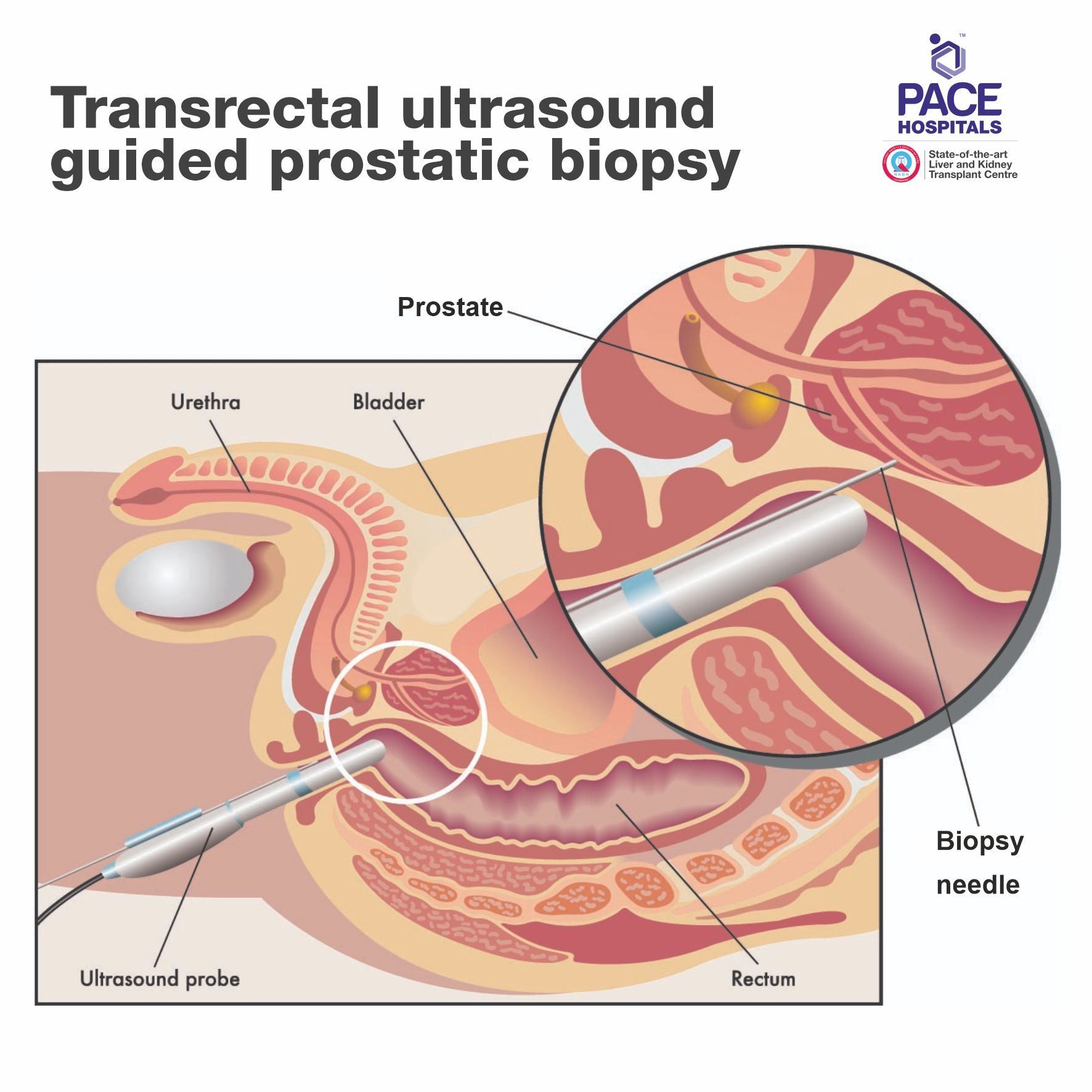
Transrectal Biopsy: A transrectal biopsy is used to diagnose prostate cancer and determine Gleason score in addition to stage to help plan treatment. This procedure performed either by using transrectal ultrasound called as transrectal ultrasound guided prostatic biopsy or by MRI called as transrectal MRI guided biopsy.
A transrectal biopsy is the collection of tissue samples from the prostate by inserting a thin needle through the rectum wall and into the prostate. Sometimes a biopsy is done using a tissue sample that was removed during a transurethral resection of the prostate (TURP) to treat enlarged prostate.
TRUS prostatic biopsy performed in men with a rapidly increasing PSA level and a palpable abnormality on a digital rectal examination (DRE). TRUS is a highly sensitive diagnostic modality for rectal wall involvement in patients with locally advanced prostate cancer.
Treatment for Prostate Cancer
Prostate cancer treatment options and recommendations depend upon level of PSA in blood, Gleason score, Grade, first time detected or recurrent, such as - medical management, radiation therapy, hormone therapy, minimally-invasive procedures, and surgical management. The choice or selection of the prostatic carcinoma treatment depends upon the other health conditions, past treatment for prostate cancer and severity of the symptoms.
Most prostate cancers are found in the early stages, when they are growing slowly. These are different types of treatment by stage of prostate cancer for patients:
Watchful waiting and active surveillance
If prostate cancer is in an early stage, is growing slowly, and treating the cancer would cause more problems than the disease itself, a doctor may recommend watchful waiting and active surveillance.
During watchful waiting, routine PSA test, digital rectal examination, and prostate biopsy are not usually done. In case of urine blockage due to prostate cancer then treatment would be initiated to relive symptoms.
Further treatment plan can be discussed based on the patient’s life expectancy and other illnesses to determine whether watchful waiting and active surveillance is appropriate.
Surgery
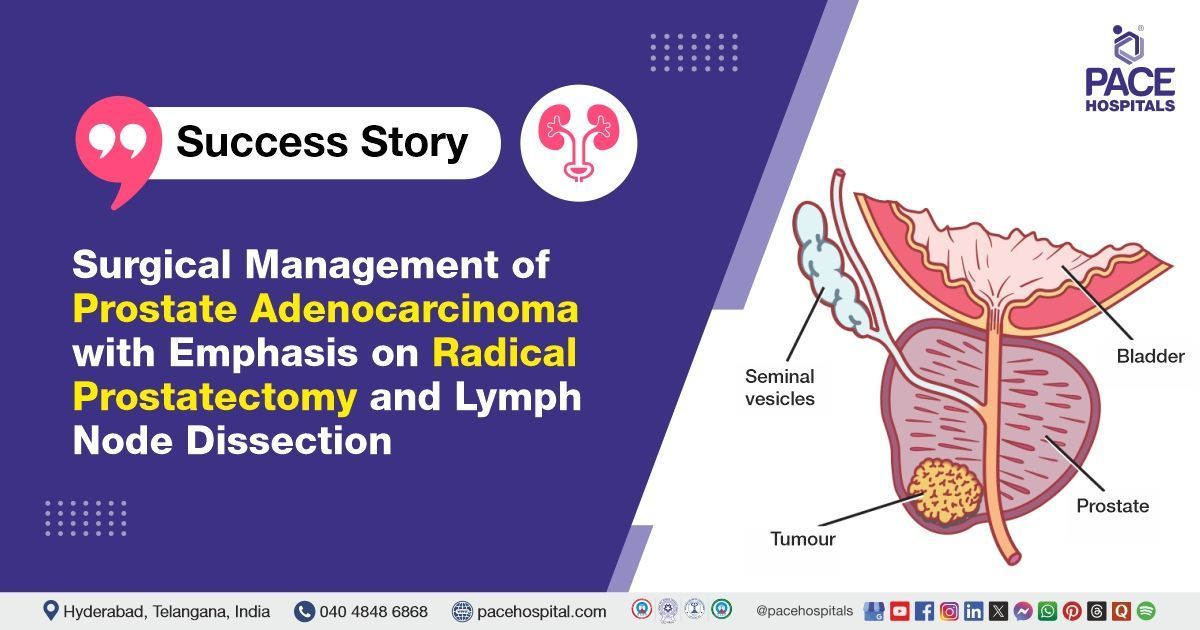
During prostatectomy surgery, the prostate gland and, or surrounding lymph nodes will be removed to treat prostate cancer. A urologist or urologic oncologist (surgical oncologist) perform surgery to remove the tumor from the prostate gland or remove complete gland. If the cancer spread outside the prostate gland, then systemic treatment required to destroy the cancer cells. The following types of surgery are used, and it depends on the stage and grade of the disease, the patient’s health condition, and other factors.
- Open radical prostatectomy: removing prostate gland through open procedure
- Radical laparoscopic prostatectomy: removing prostate gland through laparoscopic instruments
- Robot-assisted laparoscopic radical prostatectomy: removing prostate gland through robot-assisted laparoscopic instruments
- Transurethral resection of the prostate (TURP): It is most often used to relieve symptoms of a urinary blockage in patients with prostate cancer
- Pelvic lymphadenectomy
- Bilateral orchiectomy
Radiation therapy
Radiation therapy is the use of high-energy x-rays or other types of radiation to destroy the cancer cells or keep them from growing. A radiation therapy schedule, usually consists of a specific number of treatments that is given over a period of time. These are different types of radiation therapies:
- External radiation therapy
- Hypofractionated radiation therapy
- Internal radiation therapy or brachytherapy
- Intensity-modulated radiation therapy (IMRT)
- Proton therapy
- Radiopharmaceutical therapy
Robot-assisted laparoscopic radical prostatectomy
In the
Robot-assisted laparoscopic radical prostatectomy will make small incisions in your abdomen to insert the robotic-assisted laparoscopic and surgical instruments to perform the surgery. Our team of uro-oncologist, surgeons and skilled technicians are trained to use robotic assisted laparoscopic instruments.
Hormone therapy
Hormone therapy in a prostate cancer treatment helps to remove hormones or block their action and stops cancer cells from growing. Drugs, surgery, or other hormones are used to reduce the amount of male hormones or block them from working.
Chemotherapy
Chemotherapy in a prostate cancer treatment that uses drugs to stop the growth of cancer cells, either by destroying the cells or by stopping them from dividing.
Targeted therapy
Targeted therapy in a prostate cancer treatment that uses drugs or other substances to identify and attack specific cancer cells. Targeted therapies usually cause less harm to normal cells than chemotherapy or radiation therapy do.
Immunotherapy
Immunotherapy in a prostate cancer treatment that uses the patient’s immune system to fight cancer. Substances made by the body or made in a laboratory are used to boost, direct, or restore the body’s natural defenses against cancer. This cancer treatment is a type of biologic therapy.
Bisphosphonate therapy
Bisphosphonate drugs, reduce bone disease when cancer has spread to the bone. Men who are treated with antiandrogen therapy or orchiectomy are at an increased risk of bone loss. In these men, bisphosphonate drugs lessen the risk of bone fracture (breaks).
Palliative care
Palliative care or supportive care mainly focuses on providing relief from pain and other symptoms of the disease. People with cancer may feel better and live longer in palliative care with all the other appropriate treatments. Palliative care can be used while undergoing other treatments, such as surgery, chemotherapy or radiation therapy.
Palliative care team, including oncologists, nurses and other specially trained paramedical professionals, aim to improve the quality of life for people with cancer and their families.
Prostate Cancer Treatment Cost in Hyderabad, India
The cost of Prostate Cancer Treatment in Hyderabad generally ranges from ₹2,500 to ₹4,50,000 (approx. US $30 – US $5,400).
The exact cost varies depending on the stage of cancer, diagnostic tests required (PSA, biopsy, MRI, PET-CT), type of treatment (surgery, radiation therapy, hormone therapy, chemotherapy), length of hospital stay, specialist consultations (urologist, oncologist), and hospital facilities — including cashless insurance, TPA corporate tie-ups, and support with medical insurance processing wherever applicable.
Cost Breakdown According to Type of Prostate Cancer Treatment
- Urologist / Oncologist Consultation – ₹1,000 – ₹1,800 (US $12 – US $22)
- PSA Blood Test – ₹800 – ₹1,500 (US $10 – US $18)
- TRUS-Guided Prostate Biopsy – ₹6,000 – ₹15,000 (US $72 – US $180)
- MRI Prostate (Multiparametric MRI) – ₹6,500 – ₹14,000 (US $78 – US $168)
- PET-CT Scan (If Needed) – ₹18,000 – ₹32,000 (US $215 – US $385)
- Hormone Therapy (Monthly) – ₹3,500 – ₹12,000 (US $42 – US $145)
- Radical Prostatectomy (Surgery) – ₹1,40,000 – ₹2,40,000 (US $1,680 – US $2,880)
- Laser Prostate Surgery (Select Cases) – ₹90,000 – ₹1,60,000 (US $1,080 – US $1,920)
- Radiation Therapy (External Beam / IMRT) – ₹1,20,000 – ₹4,50,000 (US $1,440 – US $5,400)
- Chemotherapy (Per Cycle) – ₹12,000 – ₹35,000 (US $145 – US $420)
- Hospital Admission (1–4 Days) – ₹10,000 – ₹35,000 (US $120 – US $420)
Everything you need to know about Prostate Cancer
Prostate Cancer Related Resources, Case Studies and Podcast
Frequently Asked Questions (FAQs) Prostate Cancer
What is prostate cancer?
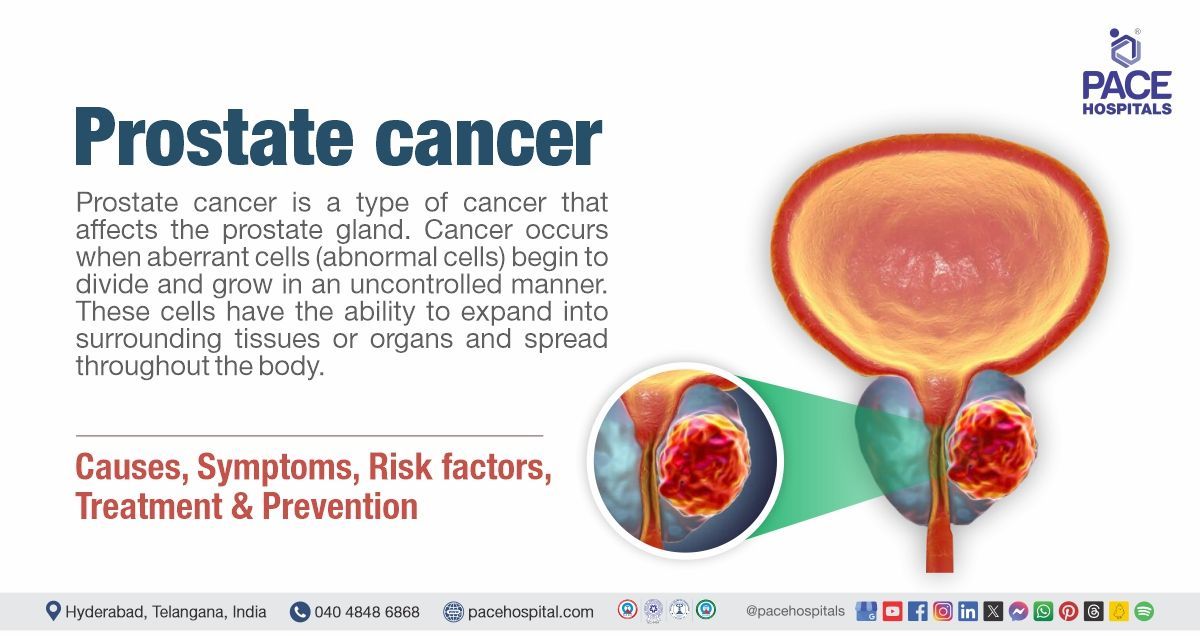
Prostate cancer is a malignancy characterised by the uncontrolled growth of abnormal cells within the prostate gland. It is one of the most common cancers affecting men worldwide. Most prostate cancers grow slowly and may remain asymptomatic for many years; however, some variants are aggressive and can metastasise to distant organs. In its early stages, the disease produces no symptoms. As it progresses, patients may experience urinary difficulties such as a weak stream or frequent nighttime urination, and blood in the urine or semen.
Which Is the best Hospital for Prostate Cancer Treatment in Hyderabad, India?
PACE Hospitals, Hyderabad, is one of the most trusted centres for the diagnosis and treatment of prostate cancer.
We resolve complicated cases guided by expert urologists, oncologists, radiologists, and rehabilitation teams deliver advanced, evidence-based care for:
- Localized and advanced prostate cancer
- Rising PSA levels / PSA-related concerns
- Prostate enlargement with suspected malignancy
- Metastatic prostate cancer
- Hormone-sensitive and hormone-resistant cancers
With state-of-the-art diagnostics, advanced surgical options, precision radiation therapy, targeted medical treatment, and comprehensive rehabilitation, PACE Hospitals ensures safe, effective, and patient-focused prostate cancer management — supported by cashless insurance, TPA tie-ups, and complete documentation assistance.
How effective is hormone treatment for prostate cancer?
Hormone therapy or androgen suppression therapy is used for reducing levels of male hormones (androgens - testosterone and dihydrotestosterone (DHT)), in the body, or to stop them from stimulating prostate cancer cells. Hormone therapy is effective in slowing down the cancer growth or shrink them.
Hormone therapy does not cure alone the prostate cancer, it can be used:
- If the prostate cancer has spread too far and surgery or radiation can’t be used
- If the prostate cancer comes back or remains after radiation therapy or surgery
- To make radiation therapy more effective
What is the prostate cancer survival rate by stage?
Prostate cancer survival rates depend strongly on the stage at diagnosis. When the cancer is confined to the prostate (localised stage), the five-year survival rate is about 99%. If it has spread to nearby tissues or lymph nodes (regional stage), the survival rate remains above 95%. When the cancer has spread to distant organs such as the bones (advanced stage), the five-year survival rate drops to around 30–37%.
What Is the cost of Prostate Cancer Treatment at PACE Hospitals, Hyderabad?
At PACE Hospitals, Hyderabad, the cost of prostate cancer treatment generally ranges from ₹2,000 to ₹4,20,000 and above (approx. US $24 – US $5,040), making it a highly competitive and specialized option for cancer care. However, the final cost depends on:
- Stage and aggressiveness of the cancer
- PSA levels and diagnostic requirements
- Choice of treatment (surgery, radiation, hormone therapy, chemotherapy)
- Number of therapy cycles or radiation sessions
- Length of hospital stay and recovery needs
- Follow-up care, medications, and long-term monitoring
- Co-existing conditions (diabetes, hypertension, prostate enlargement)
Early-stage prostate cancer managed with hormone therapy and monitoring falls at the lower range, while surgery or radiation for advanced disease falls toward the higher end.
After a complete diagnostic evaluation and consultation, our oncology and urology teams provide a personalized treatment plan and a transparent cost estimate tailored to your clinical needs.
How does immunotherapy offer a surgery-free option for prostate cancer?
Immunotherapy works by strengthening the body’s own immune system so it can recognise and attack prostate cancer cells. Instead of removing the prostate gland, this approach targets cancer cells through immune activation, which may slow disease progression or control cancer growth. In prostate cancer, immunotherapy is mainly used in some selected or advanced cases rather than as a universal cure for all patients affected. While it may not replace surgery for early-stage disease, it offers a surgery-free treatment option for patients who are not suitable candidates for surgery or radiation. Ongoing research continues to explore how immunotherapy can be used earlier and more effectively in prostate cancer care.
What dietary changes can help reduce the risk of prostate cancer?
Diet plays an important role in overall prostate health and may influence prostate cancer risk. Research suggests that diets rich in fruits, vegetables, whole grains, and healthy fats support protective metabolic and hormonal balance. Reducing intake of processed foods, excess red meat, and saturated fats may help lower inflammation linked to cancer development. Maintaining a healthy body weight through balanced nutrition is also associated with a reduced risk of aggressive prostate cancer. While diet alone cannot prevent prostate cancer, healthy dietary patterns support long-term prostate and general health.
Understanding Prostate Cancer
Where is the prostate gland located, and what does it do?
Understanding the prostate gland helps clarify why prostate-related conditions affect urinary and reproductive health. The prostate gland functions as follows:
- The prostate is a small, walnut-shaped gland located just below the bladder and in front of the rectum.
- It surrounds the upper part of the urethra, the tube that carries urine out of the body.
- The gland produces fluid that nourishes and protects sperm, forming part of semen.
- Prostate health directly affects urination and male fertility.
How common is prostate cancer in men?
Prostate cancer is one of the most frequently diagnosed cancers in men worldwide. Its occurrence is influenced by the following factors:
- Risk increases with age, especially after 50 years.
- Family history and genetic factors raise the likelihood of developing the disease.
- Many cases are detected through routine screening rather than symptoms.
- Early detection improves treatment outcomes significantly.
Is prostate cancer always life-threatening?
Not all prostate cancers behave the same way.
Important points to understand include:
- Many men live long, healthy lives after diagnosis, especially when cancer is detected early.
- Some prostate cancers grow very slowly and may not cause harm for many years.
- Aggressive forms can spread quickly and require prompt treatment.
- Treatment decisions depend on cancer type, stage, and overall health.
- A urologist helps determine whether active treatment or close monitoring is appropriate.
Can prostate cancer develop without symptoms?
Prostate cancer often develops silently in its early stages.
Key considerations include:
- Many men do not experience symptoms in the early phase of the disease.
- Symptoms, when present, may appear only as the cancer grows or spreads.
- Routine screening helps detect prostate cancer before symptoms occur.
- Early diagnosis allows for more treatment options and better outcomes.
- A urologist recommends appropriate screening based on age and risk factors.
Causes & Risk Factors
What causes prostate cancer?
Prostate cancer develops due to changes in prostate cells that lead to uncontrolled growth.
Common contributing factors include:
- Abnormal changes in cell DNA that affect normal cell growth and repair.
- Hormonal influences, especially male hormones that affect prostate cell activity.
- Increasing age, which allows more time for genetic changes to accumulate.
- Family history or inherited genetic mutations in some individuals.
Who is at higher risk of developing prostate cancer?
Certain groups of men have a higher likelihood of developing prostate cancer.
Higher-risk categories include:
- Men above the age of 50 years.
- Those with a close family member diagnosed with prostate cancer.
- Individuals with a history of genetic mutations linked to cancer risk.
- Men with long-standing hormonal or metabolic conditions.
Does age increase the risk of prostate cancer?
Age is one of the strongest risk factors for prostate cancer.
Age-related considerations include:
- Prostate cancer is uncommon in younger men but becomes more frequent with advancing age.
- Most diagnoses occur in men over 60 years.
- Age-related cellular changes increase the likelihood of abnormal prostate cell growth.
- Regular screening becomes more important as men get older.
Is prostate cancer hereditary or genetic?
Genetics can play a role in prostate cancer risk for some men.
Important points include:
- Men with a family history of prostate cancer have a higher risk compared to those not having in family history genetic predisposition.
- Certain inherited genetic mutations are linked to increased susceptibility.
- Hereditary cases tend to occur at a younger age.
- Not all prostate cancers are inherited; many occur without a family history.
Can lifestyle or diet influence prostate cancer risk?
Lifestyle choices may affect prostate cancer risk and overall prostate health.
Factors that may influence risk include:
- Diets high in processed foods and unhealthy fats.
- Low intake of fruits, vegetables, and fibre-rich foods.
- Lack of regular physical activity and obesity.
- Smoking and excessive alcohol consumption.
Diagnosis & Staging
How is prostate cancer diagnosed?
Prostate cancer diagnosis involves a step-by-step evaluation to identify abnormal changes in the prostate gland.
The diagnostic process usually includes:
- Review of symptoms, medical history, and family history.
- Blood testing, especially Prostate-Specific Antigen (PSA) levels.
- Physical examination using Digital Rectal Examination (DRE).
- Imaging and tissue testing when cancer is suspected.
What is a PSA (Prostate-Specific Antigen) blood test?
The Prostate-Specific Antigen (PSA) blood test measures a protein produced by prostate cells.
Important points include:
- PSA is normally present in small amounts in the blood.
- Elevated PSA levels may indicate prostate enlargement, inflammation, or cancer.
- PSA testing is commonly used for screening and follow-up.
- Results are interpreted along with age and prostate size.
Does a high PSA level always mean cancer?
A raised Prostate-Specific Antigen (PSA) level does not always indicate prostate cancer.
Other possible causes include:
- Benign Prostatic Hyperplasia (BPH), which is non-cancerous prostate enlargement.
- Prostatitis, which is inflammation or infection of the prostate.
- Recent urinary procedures or ejaculation.
- PSA trends over time are more meaningful than a single value.
- A urologist determines the cause through additional evaluation.
What tests are used to confirm prostate cancer?
Confirmation of prostate cancer requires specific diagnostic tests beyond screening.
Common confirmatory tests include:
- Repeat Prostate-Specific Antigen (PSA) testing to assess changes over time.
- Magnetic Resonance Imaging (MRI) of the prostate for detailed imaging.
- Transrectal Ultrasound (TRUS)–guided prostate biopsy.
- Additional scans to evaluate possible spread, if cancer is detected.
- A urologist selects appropriate tests based on clinical findings.
What is prostate biopsy, and is it painful?
A prostate biopsy involves collecting small tissue samples from the prostate gland for examination.
Key points include:
- It is commonly performed using Transrectal Ultrasound (TRUS) guidance.
- Local anaesthesia is used to minimise discomfort.
- Most patients experience mild discomfort rather than severe pain.
- Temporary side effects such as mild bleeding may occur.
What does staging mean in prostate cancer?
Staging describes how far prostate cancer has spread within or outside the prostate.
Staging helps determine:
- Whether cancer is confined to the prostate or has spread to nearby tissues or organs.
- Tumour size and involvement of lymph nodes or bones.
- Appropriate treatment options and prognosis.
- Need for additional imaging such as Computed Tomography (CT) Scan or Positron Emission Tomography (PET) Scan.
How is prostate cancer graded or classified?
Grading explains how aggressive prostate cancer cells appear under the microscope.
Classification is based on:
- The Gleason Score (GS) system.
- The Grade Group (GG) system, which classifies cancer from Group 1 to Group 5.
- Higher grades indicate faster-growing and more aggressive cancer.
- Grading helps predict disease behaviour and guide treatment decisions.
Treatment Basics
What are the treatment options for prostate cancer?
Prostate cancer treatment depends on how aggressive the disease is and the patient’s overall health.
The main treatment options include:
- Active surveillance, for slow-growing cancers that may not need immediate treatment.
- Surgery to remove the prostate gland when cancer is localised.
- Radiation therapy to destroy cancer cells without removing the prostate.
- Hormone therapy (Androgen Deprivation Therapy – ADT) to reduce male hormones that fuel cancer growth.
- A urologist discusses suitable options based on cancer stage and risk level.
How is the best treatment chosen for prostate cancer?
Selecting the most appropriate treatment requires careful evaluation of several factors.
The decision is based on:
- Cancer stage and grade, including Gleason Score (GS) and Grade Group (GG).
- Prostate-Specific Antigen (PSA) levels and tumour spread.
- Age, overall health, and life expectancy.
- Potential side effects and impact on quality of life.
- A urologist guides the decision-making process after discussing all options.
Is prostate cancer always treated with surgery?
Surgery is not required for every case of prostate cancer.
Important considerations include:
- Many early-stage or slow-growing cancers may not need surgery.
- Non-surgical options such as radiation or hormone therapy may be equally effective in selected cases.
- Treatment choice depends on cancer behaviour and patient preference.
- Avoiding unnecessary surgery can reduce side effects.
- A urologist determines whether surgery is necessary.
When is active surveillance recommended prostate cancer?
Active surveillance is advised for selected men with low-risk prostate cancer.
It is recommended when:
- Cancer is small, localised, and slow-growing.
- PSA levels are low and stable.
- There are no troubling symptoms.
- Regular monitoring with PSA tests, imaging, and biopsies is feasible.
- A urologist closely monitors the condition to intervene if needed.
When is hormone therapy used for prostate cancer?
Hormone therapy helps slow or stop cancer growth by reducing male hormones.
It is commonly used when:
- Cancer has spread beyond the prostate.
- Cancer returns after initial treatment.
- Used along with radiation therapy in certain cases.
- Surgery or radiation is not suitable.
- A urologist decides the timing and duration of hormone therapy.
Can prostate cancer be treated without removing the prostate?
In many cases, prostate cancer can be treated without surgery.
Non-surgical approaches include:
- Radiation therapy aimed at destroying cancer cells.
- Hormone therapy to control cancer growth.
- Active surveillance for low-risk cases.
- These approaches may preserve urinary and sexual function.
- A urologist explains which non-surgical option is appropriate.
Surgery-Related FAQs
What is radical prostatectomy?
Radical prostatectomy is a surgical procedure to remove the entire prostate gland.
Important aspects include:
Removal of the prostate along with nearby tissues that may contain cancer cells.
It aims to completely eliminate localised prostate cancer.
Nerve-sparing techniques may be used to reduce side effects.
Lymph nodes may also be removed in selected cases.
Is prostate cancer surgery safe?
Prostate cancer surgery is generally considered safe when performed by experienced specialists.
Safety considerations include:
- Modern surgical techniques have improved precision and successful
- outcomes.
- Complication rates are lower when surgery is done at specialised centres.
- Risks may include bleeding, infection, or temporary functional changes.
- Careful preoperative evaluation improves safety.
- A urologist discusses potential risks and benefits before surgery.
How long does recovery take after prostate cancer surgery?
Recovery time varies depending on the individual and surgical approach. However in most cases complete recovery 1 to 2.5 months (nearly 4-10 weeks)
General recovery expectations include:
- Hospital stay is usually short, depending on recovery progress.
- Most daily activities with light exercises can be resumed within a few weeks (2–3 weeks approx.).
- Temporary urinary control issues may improve over time.
- Complete recovery may take several weeks to months.
- A urologist provides guidance on activity, follow-up, and rehabilitation.
Will surgery completely cure prostate cancer?
Surgery can be highly effective, especially when cancer is detected early.
Important points to understand include:
- Surgery offers a high chance of cure for localised prostate cancer.
- Outcomes depend on cancer stage, grade, and margins.
- Some patients may need additional treatment after surgery.
- Regular follow-up is essential to monitor for recurrence.
- A urologist evaluates long-term outcomes and follow-up plans.
Side Effects & Quality of Life
What are the common side effects of prostate cancer treatment?
Prostate cancer treatments can affect different body functions, depending on the type of therapy used to combat the problem.
Common side effects may include:
- Urinary symptoms such as increased frequency or mild discomfort.
- Temporary tiredness or weakness during or after treatment.
- Changes in bowel habits, especially after radiation therapy.
- Sexual health changes, including reduced libido or erectile difficulties.
- A urologist monitors side effects faced by the patients and provides supportive care throughout treatment.
Does prostate cancer treatment affect urinary control?
Urinary control can be affected, particularly after certain treatments.
Key points include:
- Temporary urinary leakage may occur after surgery in some cases.
- Most patients see gradual improvement with time and exercises.
- Radiation therapy may cause irritation of the bladder in some cases.
- Long-term urinary problems are less common with modern techniques.
Can prostate cancer treatment affect sexual function?
Sexual function may get affected following prostate cancer treatment.
Important considerations include:
- Nerve-sparing techniques help reduce sexual side effects.
- Erectile difficulties may occur after surgery or radiation therapy.
- Recovery of sexual function varies between individuals.
- Emotional and psychological factors also play a key role.
- A urologist discusses treatment options to support sexual health.
Are treatment side effects permanent?
Not all side effects are long-lasting.
Recovery depends on several factors:
- Type of treatment and surgical technique used.
- Overall health and age of the patient.
- Early rehabilitation and follow-up care.
- Many side effects improve gradually over months.
- A urologist evaluates progress and manages long-term concerns.
How can side effects be managed?
Most treatment-related side effects can be effectively managed.
Management strategies include:
- Medications to control urinary or sexual symptoms.
- Pelvic floor exercises to improve bladder control.
- Lifestyle modifications and physical activity.
- Counselling and support services when needed.
- A urologist develops a personalised plan to minimise side effects and improve quality of life.
Outcomes & Prognosis
What is the survival rate of a person with prostate cancer?
| Cancer Stage | What This Stage Indicates | 5-Year Relative Survival Rate |
|---|---|---|
| Localized | Cancer is confined to the prostate gland | >99% |
| Regional | Cancer has spread to nearby tissues or lymph nodes | >99% |
| Distant (Metastatic) | Cancer has spread to distant organs such as bones or lungs | ~38% |
| All stages combined | Includes all stages of prostate cancer | ~98% |
Note:
- Prostate cancer generally has an excellent overall outlook, with a 5-year survival rate of approximately 97%–99%.
- When diagnosed at a localized or regional stage, survival at five years is nearly 100%.
- In advanced or metastatic disease, the five-year survival rate is lower, at around 30%–38%, but treatment can still control the disease and improve quality of life.
- Long-term outcomes remain strong, with about 98% of patients surviving at least 10 years and approximately 95% surviving 15 years after diagnosis.
- Individual survival varies and is influenced mainly by cancer stage, grade, Gleason score, and overall health.
Source: (Based on population data from men diagnosed between 2015 and 2021) from organizations like the American Cancer Society and the Centers for Disease Control and Prevention | CDC (.gov).
Can prostate cancer come back after treatment?
Prostate cancer can sometimes recur even after successful initial treatment.
Important considerations include:
- Rising PSA levels after treatment may be an early sign of recurrence.
- Recurrence risk also depends on factors such as cancer stage, grade, and treatment type performed.
- Recurrence does not always mean advanced disease and can often be treated.
- Early detection of recurrence improves treatment options
How often are follow-up tests needed after treatment?
Regular follow-up is essential to monitor recovery and detect recurrence early.
Follow-up usually with tests and physical examination that involves:
- Periodic Prostate-Specific Antigen (PSA) blood tests.
- Clinical evaluation and symptom review.
- Imaging tests if PSA levels rise or symptoms appear.
- Follow-up frequency may reduce over time if results remain stable.
- A urologist determines the follow-up schedule based on risk level.
What happens if prostate cancer spreads?
When prostate cancer spreads beyond the prostate, it is referred to as advanced or metastatic disease.
Key points include:
- Cancer may spread to nearby tissues, lymph nodes, or bones.
- Treatment focuses on controlling disease, relieving symptoms, and maintaining quality of life.
- Hormone therapy, radiation, or other systemic treatments may be used.
- Many patients continue to live active lives with ongoing treatment.
- General Patient Concerns
Is prostate cancer treatment painful?
Many patients worry about discomfort during prostate cancer treatment, but pain is usually well controlled.
Important points to be aware of include:
- Surgery-related discomfort or pain is typically temporary and managed with prescribed pain medicines.
- Most treatments are performed with pain-relief measures such as anaesthesia or supportive medications.
- Radiation therapy is usually painless, though mild irritation may occur over time.
- Hormone therapy does not cause pain but may have other side effects.
- A urologist ensures pain is minimised and addresses discomfort promptly during treatment.
How long does prostate cancer treatment last?
The duration of treatment varies depending on the type of therapy and progression of the diseases especially the cancer stage.
Treatment timelines generally include:
- Surgery is a one-time procedure followed by a recovery period.
- Radiation therapy may be given over several weeks in planned sessions.
- Hormone therapy can continue for months or longer, depending on response.
- Active surveillance involves long-term monitoring rather than active treatment.
- A urologist explains the expected treatment duration based on the chosen approach.
Can patients continue normal activities during treatment?
Activity levels depend on:
- Type of treatment and individual tolerance.
- Temporary fatigue, which may occur during radiation or hormone therapy.
- Nature of work and physical demands.
- Need for rest during recovery after surgery.
- A urologist advises on safe activity levels and work adjustments during treatment.
Can prostate cancer be prevented?
There is no such guaranteed way to prevent prostate cancer, but certain measures may reduce risk.
Risk-reduction strategies include:
- Maintaining a proper healthy weight and staying physically active.
- Eating a balanced diet rich in fruits, vegetables, and whole grains.
- Avoiding smoking and limiting alcohol intake.
- Regular health check-ups and age-appropriate screening.
- A urologist guides screening and risk-reduction based on individual factors.
How much does prostate cancer treatment cost in India?
Prostate cancer treatment recommendations depend upon level of PSA, Gleason score, Grade, co-morbid conditions of the patient. Average cost of prostate cancer treatment in India would vary from Rs. 4,50,000 to Rs. 7,50,000 (four lakh fifty thousand to seven lakh fifty thousand). Prostate cancer treatment cost in India vary in different hospitals at different cities. These are different surgical treatment options and their cost:
- Radical Laparoscopic Prostatectomy cost in India - Rs. 4,80,000 to Rs. 5,50,000 (four lakh eighty thousand to five lakh fifty thousand)
- Robot-assisted laparoscopic radical prostatectomy cost in India - Rs. 7,00,000 to Rs. 7,50,000 (seven lakh to seven lakh fifty thousand)
- Open radical prostatectomy cost in India - Rs. 3,00,000 to Rs. 4,00,000 (three lakh to four lakh)