Best Pulmonology Hospital in Hyderabad for all Respiratory Disease Treatment
PACE Hospitals is one of the Best Lungs Hospital in Hyderabad, India, providing holistic and patient centric pulmonary treatment. The team of experienced and skilled pulmonary doctors, interventional pulmonologist have vast expertise in managing all kind of infectious and critical respiratory disease and disorder, including:
- Bronchitis & Bronchial Asthma
- Chronic Obstructive Pulmonary Disease (COPD)
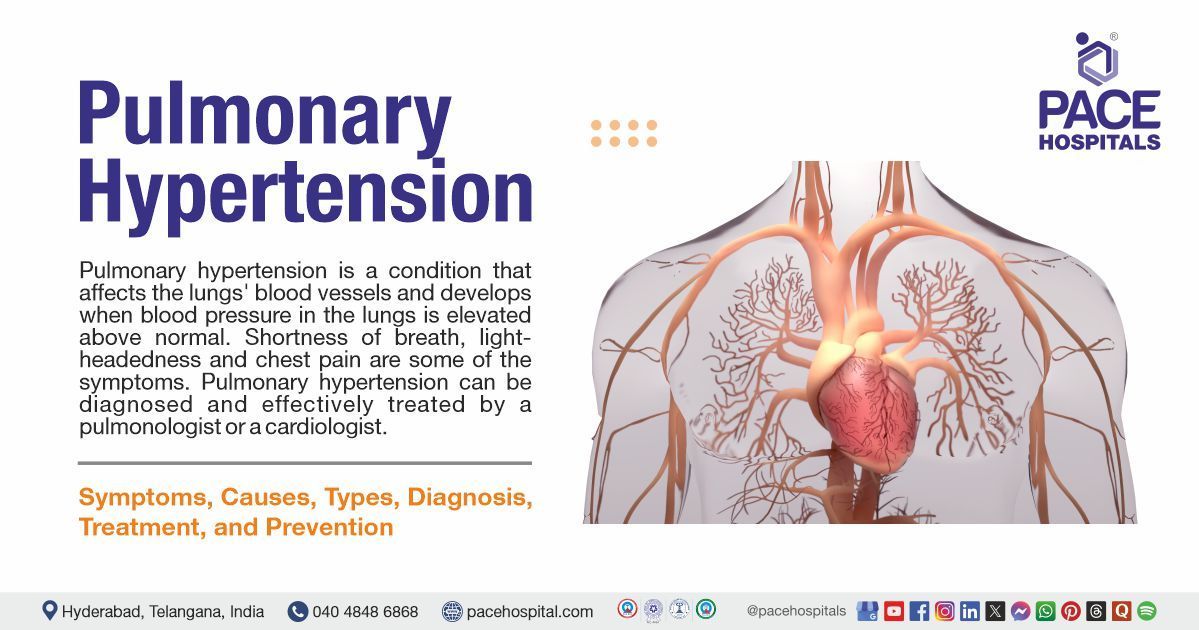
- Pneumonia, Tuberculosis (TB), Pulmonary Hypertension
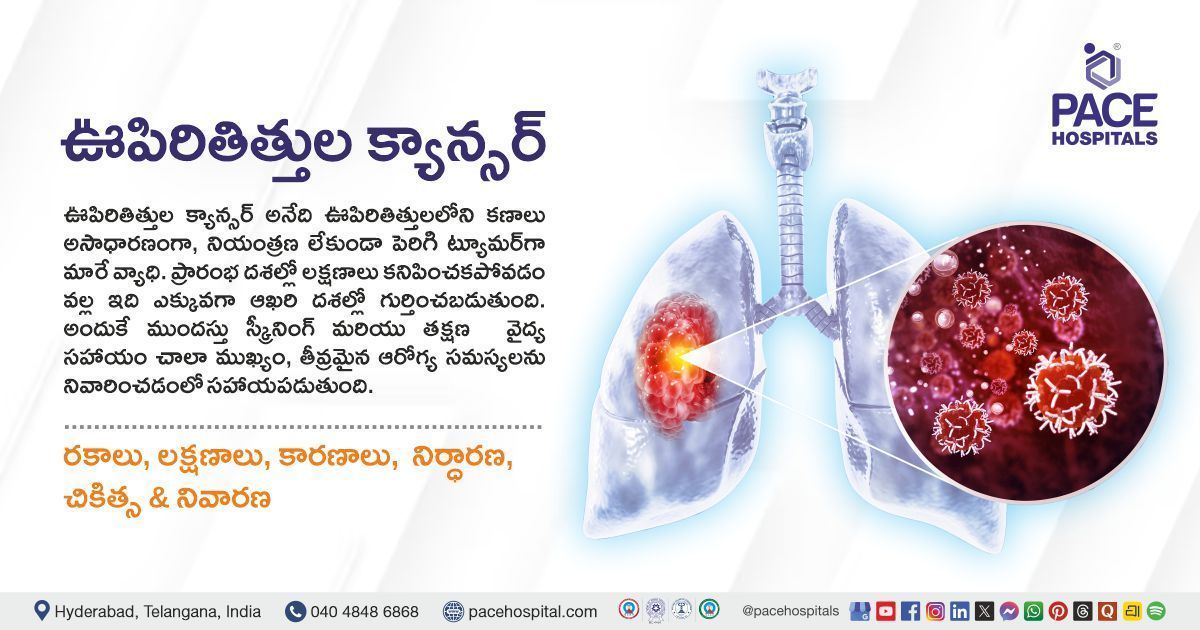
- Pulmonary Fibrosis, Cystic Fibrosis, Lung infections, Lung Cancer, Sleep Apnea, Pulmonary Embolism
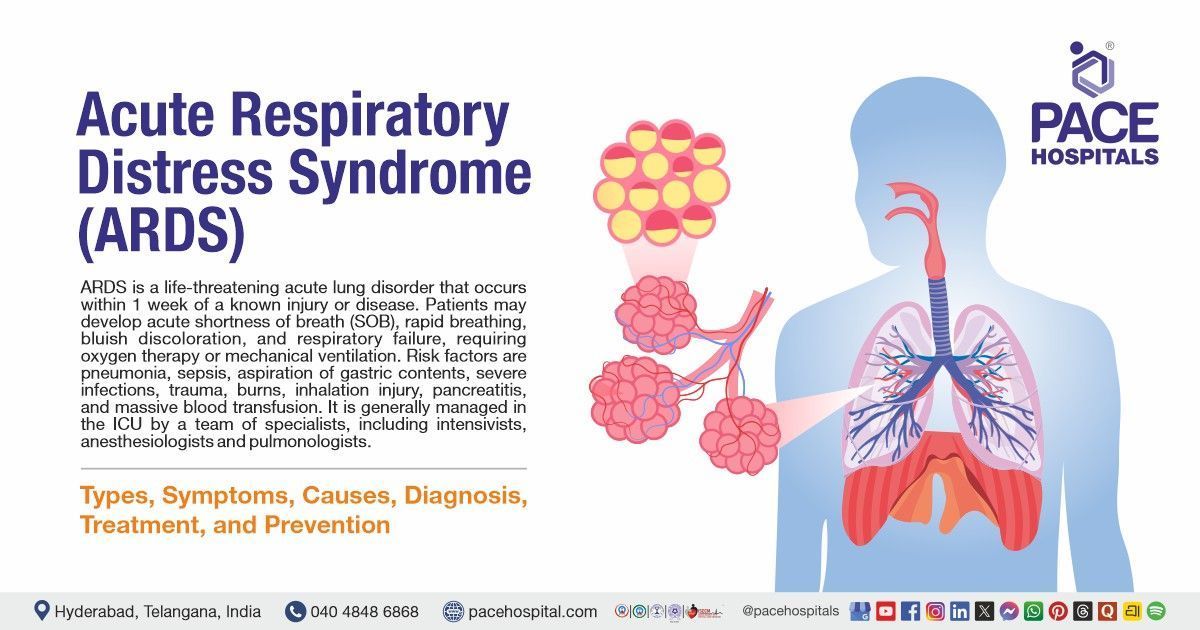
- Interstitial Lung Disease (ILD), Pleural effusions & Emphysema, Acute and chronic respiratory failure
- Sleep disorders & Pulmonary hypertension
- Pulmonary Edema
Why Choose PACE Hospitals for Lung & Respiratory Care?
Comprehensive Respiratory Care
Providing treatment to a wide range of lung and respiratory disorders, including acute & chronic respiratory diseases and Infections, sleep apnea, COPD, pulmonary fibrosis and lung cancer.
Advanced State-of-the-art Facility
Equipped with advanced and latest diagnostic equipment, robotic and minimally invasive surgical facilities for lung and respiratory disease treatment.
Skilled & Experienced Pulmonary Doctor
Team of experienced pulmonary doctor, chest specialist & interventional pulmonologist with vast experience in minimally invasive procedures.
Advanced Centre for Respiratory Disease Treatment in Hyderabad, Telangana
The pulmonology department at PACE Hospitals is one of the top lung care centre in hyderabad. The department is staffed with a team of skilled and experienced chest specialist doctors, lung doctors, interventional pulmonologists and multidisciplinary teams who work collaboratively to provide the most effective and up-to-date care possible. They have vast expertise in diagnosing and managing critical conditions related to the respiratory tract and lungs and are well-versed in the latest treatment modalities catering to compassionate, holistic, and precise respiratory disease treatment with a high success rate.
The Department of Pulmonology is equipped with state-of-the-art and cutting-edge facilities that offer a wide range of comprehensive respiratory care, including advanced imaging systems, bronchoscopy suites, High Flow Non-invasive Ventilator (HF-NIV), minimally invasive surgeries and intensive care units to manage a broad spectrum of respiratory conditions, ensuring the personalized and evidence-based treatment plans dedicated to patient's unique needs.
3,28,338
99,825
684
2011
Best Pulmonology Specialist in Hyderabad | Top Lung Doctor
Team of the best pulmonology specialist in Hyderabad, India, having extensive expertise in specialized respiratory care treatment for acute or chronic respiratory tract infections, chronic obstructive pulmonary disease (COPD), interstitial lung disease (ILD), pulmonary fibrosis, lung cancer and respiratory failure, are committed to delivering patient-centric, evidence-based and compassionate respiratory treatment care to the patients. The specialized team of chest specialist doctor, lung doctor, pulmonology Specialist and interventional pulmonologist are highly skilled and apt with the latest and advanced treatment modalities to cater for the utmost treatment care with precision, minimal complications and a high success rate.
Dr. Pradeep Kiran Panchadi
MBBS, DNB (Pulmonary Medicine), FIP (Fellowship in Interventional Pulmonology), CCEBDM
Experience : 12+ years
Consultant Interventional Pulmonologist, Specialist in Bronchoscopy and EBUS
Consultation Timing:
Mon to Sat - 9 am to 6 pm
Location:
PACE Hospitals, Hitech City
Pulmonology Diseases and Conditions Explained by Drs
Need Help?
Struggling with the typical respiratory tract, lung or chest-related issues or seeking treatment for pneumonia recovery, tuberculosis (TB), asthma, persistent cough, shortness of breath, recurrent lung infections, unexplained chest Pain, acute or chronic respiratory tract infections, interstitial lung disease or critical pulmonary conditions like respiratory failure, chronic obstructive pulmonary disease (COPD), pulmonary fibrosis or lung cancer, we offer evidence-based solutions tailored to your needs. Our team of skilled and experienced pulmonary doctors and interventional pulmonologists provides comprehensive and compassionate care for geriatric, adult and pediatric patients.
What we treat?
We specialize in treating various pulmonology diseases and conditions affecting the respiratory tract and lungs. From asthma, pneumonia, tuberculosis (TB), chronic obstructive pulmonary disease (COPD), sleep apnea, and pulmonary hypertension to all kinds of acute and chronic upper respiratory tract infections (URTIs), lower respiratory tract infections (LRTIs) and complicated respiratory disorders like pulmonary fibrosis, pulmonary embolism and lung cancer, our team of chest specialist doctor and interventional pulmonologist is committed to cater patient centric comprehensive solutions for all your respiratory health.
Patient Testimonials
Patient with COPD, pneumonia, and acute respiratory failure treated successfully with medications and supportive treatment.
Pulmonology Diagnostic Tests and Procedures Performed
We provide comprehensive pulmonology diagnostic tests to carry out evidence-based treatment. Our advanced and latest screening approach examines all kinds of abnormalities and impairments in the upper and lower respiratory tract, lungs, and chest region. This results in early detection and precise evaluation, enabling our pulmonology doctors and interventional pulmonologists to make an informed decision to proceed with the appropriate treatment modalities and surgical procedures.

1. Chest X-ray: It is a painless and fast imaging technique to find the structures in and around the patient's chest. The amount of radiation is significantly less, so one cannot worry about taking this test. This test helps find the diseases such as tuberculosis, emphysema, heart failure, pneumonia and lung cancer. Healthcare practitioners may use this imaging test to see how well the treatments are working in patients and to find the complications after some specific surgeries or procedures.
2. Chest MRI: A chest MRI scan uses magnets, radio waves, and computers to create images of the structures within a patient's chest. This procedure can be done in a hospital or imaging centre. The healthcare provider may inject a contrast dye into the patient's arm veins to highlight the blood vessels and heart. It can diagnose diseases such as blood vessel problems, cystic fibrosis, pulmonary embolism, pulmonary hypertension, tumour or pleural disorders and abnormal lymph nodes.
4. Computerized Tomography (CT) or Positron Emission Tomography (PET) Scans:
Both are advanced imaging tests and can be used to find issues such as cancers (e.g., solitary pulmonary nodule and non-small cell lung cancer). CT scan is a sequence of X-rays that have been taken from various (different) angles that give a complete picture of the lungs. In a PET scan, a special dye will use to see the body parts.
5. Pulmonary Angiogram: It is a technique that concentrates on pulmonary arteries (blood vessels that connect the heart and lungs), present with an X-ray of the blood vessels. A notable contrast dye is injected into the patient’s blood vessels and used to find dangerous blood clots within or around the lungs called pulmonary embolism.
6. Pulmonary Function Test (PFTs):
Pulmonary function tests are a type of non-invasive examination that assesses the functionality of the lungs without the need for intrusive instruments. These tests measure various lung parameters, including capacity, volume, gas exchange, and flow rates.
7. Spirometry: The test is simple and commonly used. The patient simply inhales and exhales through a tube, and the pulmonologist measures the amount of air exhaled after a deep breath. This helps determine the patient's lung capacity and the speed at which they can exhale air. This test identifies conditions such as chronic obstructive pulmonary disease (COPD), which can affect the amount of air the lungs can hold.
8. Pulse Oximetry: Measuring the oxygen levels in the blood is done through pulse oximetry. This method is usually performed by placing a clip on the fingertip, but it can also be done on the toes, feet, or ears. The procedure is painless, and the results are shown as a percentage. If a patient's pulse oximetry reading is less than 90%, they may require oxygen.
9. Lung Volume Test: Body plethysmography, also known as lung volume measurement, is a test that accurately estimates the amount of air the patient's lungs can hold. This test helps to assess the air volume in the lungs.
- Tidal Volume (VT): It determines the amount of air taken in or breathed out during a patient's regular breathing.
- Minute Volume (MV): It refers to the total amount of air that is exhaled in a single minute.
- Vital Capacity (VC): It measures the amount of air that can be exhaled after inhaling as much air as possible.
- Functional Residual Capacity (FRC): This test calculates the amount of air that left in patient lungs after normal exhalation.
- Inspiratory Reserve Volume (IRV): It refers to the amount of air a patient can inhale forcefully after taking a normal tidal volume.
- Expiratory Reserve Volume (ERV): It refers to the volume of air that a person can exhale forcefully after breathing out the regular tidal volume.
- Residual Volume (RV): It is used to determine the amount of air that remains in a patient's lungs after they have exhaled as much as possible.
- Total Lung Capacity (TLC): It refers to the maximum volume of air that the lungs can hold when they are completely filled.
- Forced Vital Capacity (FVC): It refers to the amount of air that is exhaled forcefully and rapidly following a maximal inhalation.
- Forced Expiratory Volume (FEV): It measures the amount of air that is exhaled during the first three seconds of a Forced Vital Capacity (FVC) test.
- Forced Expiratory Flow (FEF): The Forced Expiratory Flow (FEF) is the average airflow rate during the middle half of the Forced Vital Capacity (FVC).
- Peak Expiratory Flow Rate (PEFR): It refers to the maximum speed at which a person can exhale air from their lungs.
- Inspiratory Capacity (IC): It can be calculated by adding up the four primary lung volumes, which are TV, IRV, expiratory reserve volume (ERV), and residual volume (RV).
- Vital Capacity (VC): The vital capacity of a patient is the total amount of air exhaled after taking in a full breath. This can be calculated by adding together the tidal volume, inspiratory reserve volume, and expiratory reserve volume. The formula for vital capacity is VC = TV + IRV + ERV.
- Function Residual Capacity (FRC): refers to the air that remains in the lungs after a typical exhalation. The residual capacity of the lungs, also known as FRC, refers to the air that remains in the lungs after a regular exhalation.
10. Gas Diffusion Study: This test measures the amount of oxygen and other gases that are transferred from the lungs to the blood.
11. Cardiopulmonary Exercise Test (CPET): This assessment evaluates the functionality of the patient's heart, lungs, and muscles while engaging in physical activity. The patient will ride a bicycle or walk on a treadmill with attached machines, and a healthcare practitioner will monitor blood pressure, blood oxygen levels, and heartbeat.
12. Fractional Exhaled Nitric Oxide (FENO) Tests: This test determines the nitric oxide level in the patient's breath. Elevated nitric oxide levels indicate lung inflammation, which can cause breathing difficulties. The patient must exhale into a tube connected to a portable device to conduct the test.
13. Arterial Blood Gas Test: This medical examination assesses the quantity of oxygen and carbon dioxide in the bloodstream. Usually, the blood sample is collected from the patient's wrist artery, where the pulse is monitored.
14. Bronchial Provocation Test: The bronchial provocation test is a helpful tool for identifying asthma and determining its severity. In this test, the patient is asked to inhale a specific medication that causes the airways to narrow. Then, the patient must undergo a spirometry test multiple times while the pulmonologist records readings to measure the extent of the airway narrowing during an asthma attack.
15. Respiratory Muscle Function Test: This measures the pressure generated by the breathing muscles when the patient inhales or exhales.
16. Sputum Cytology: Sputum cytology is a simple, non-invasive, and safe diagnostic process that identifies and counts the cell types and its morphology to assess the normal and diseased characteristics of the mucosa. This method aids in the identification of abnormal cells, inflammatory cells (lymphocytes, neutrophils, eosinophils, mast cells), bacteria, and hyphae/spores of fungi in the sputum. It helps in diagnosing lung cancer.
Pulmonology Procedures Performed:
1. Bronchoscopy: It is a procedure that looks inside the lung airways and is also used to find the causative factor of a lung problem. It can recognize signs of infection, tumours, bleeding, excess mucus in airways and lung blockages. The pulmonologist will slide a small tube attached to a camera at the end of the airways. By looking into the camera, they can see the passages inside, such as blood, mucus or tumours. A medicine to sleep, or a drug, should be given to numb air passages before performing this procedure.
- Flexible Bronchoscopy: Bronchoscopy is one of the most common procedures in pulmonology. It entails the insertion of a flexible endoscope through the nose or mouth and into the airways of the lungs to detect any abnormalities. The bronchoscope also has a small tool passage at the end, which allows the pulmonologist to perform various procedures.
- Rigid Bronchoscopy: A lengthy, rigid bronchoscope (a metallic tube) is inserted into the patient's primary airways and trachea during this procedure. This enables the pulmonologist to employ more advanced surgical instruments and methods. The process necessitates general anaesthesia, just like a surgical operation.
- Ballon Bronchoscopy: A pulmonologist inserts a deflated balloon into a narrowed and abnormal section of the airways. They then inflate the balloon with water, which helps to enlarge the airway and reduce symptoms. This procedure can be done before placing an airway stent to help widen a bronchus.
- Electromagnetic Navigational Bronchoscopy: An electromagnetic navigational bronchoscopy uses GPS-like technology to examine a patient's lungs more precisely than a common bronchoscopy. It allows healthcare professionals to explore a larger area of the lungs. During the procedure, a long, flexible tube with a light at the end, known as a bronchoscope, is guided down the patient's throat and into their lungs to inspect them. Biopsies can also be taken inside the patient's lungs to determine if additional treatment is necessary. This procedure is often recommended when abnormal tissue, known as nodules, is detected during a CT scan or chest X-ray.
- Robotic Bronchoscopy: This specific bronchoscopy method allows pulmonologists to control the flexible bronchoscope tube using a controller accurately. The instrument is smaller than standard bronchoscopes and helps access hard-to-reach areas of the lungs that cannot be easily reached with a traditional bronchoscope. This procedure is usually carried out on patients with lung nodules or biopsies (masses in the lungs) to determine whether they are cancerous.
2. Chest Tube Procedure: Pulmonologists use the chest tube procedure to drain fluid or blood, inflate a collapsed lung, or deliver medications. The procedure involves inserting a thin plastic tube into the pleural cavity (space) to identify conditions such as emphysema, pneumothorax, pleural effusion, and hemothorax.
3. Mediastinoscopy: A mediastinoscopy is a surgical procedure involving a mediastinoscope to examine the mediastinum, the space between the lung lobes behind the breastbone. The mediastinoscope contains a small camera to provide a visual of the area. However, healthcare practitioners must create a small hole in the chest to insert the device. This procedure is typically performed to identify signs of various cancers and to diagnose conditions like inflammation, sarcoidosis, thymoma, and cancer affecting the bronchi or other structures in the mediastinum.
4. Pleural Biopsy: The lungs are surrounded by two layers of membranes, known as the pleural cavity. Sometimes, certain illnesses can lead to fluid accumulation in the area between the lungs and the pleura. If this occurs, pulmonologists may suggest a test to check for any fluid build-up. This test involves using a specialized biopsy needle to extract a small piece of pleura. Its purpose is to diagnose infections, cancers, or other diseases.
5. Oxygen Therapy: Some individuals with breathing disorders may be unable to obtain sufficient oxygen on their own. In such cases, they may need oxygen therapy or supplemental oxygen. This is usually caused by underlying lung conditions that prevent oxygen absorption, such as pneumonia, asthma, heart failure, upper airway obstruction, trauma, severe asthma, and chronic obstructive pulmonary disease (COPD).
6. Bronchoalveolar Lavage: During bronchoscopy, a process is performed where sterile water is injected into lung segments using a bronchoscope. This process is called bronchoalveolar lavage. The resulting fluid is then suctioned back and sent for testing. This procedure can aid in diagnosing bleeding, infection, cancer, and other medical conditions.
8. Airway Stent (Bronchial Stent): When cancer or certain other conditions affect a bronchus (airway tube), it can become compressed or narrow, resulting in coughing, breathing difficulties, and the pneumonia. A pulmonologist can use a bronchoscope to insert a wire mesh stent into the affected airway to alleviate these symptoms. This stent expands to open up the airway and relieve constriction.
9. Pleuroscopy: Interventional Pulmonologist creates a small opening in the chest wall and inserts a pleuroscope, a type of endoscope, into the chest cavity. The pleuroscope is navigated around one side of the lung and chest wall, enabling the diagnosis of certain lung lining conditions (pleura) and providing visibility of the outer edge of the patient's lung. However, this procedure cannot be done through bronchoscopy.
10. Lung Biopsy or Lymph Node: During a bronchoscopy procedure, a pulmonologist may collect a small piece of tissue from the lungs or a nearby lymph node to examine for infection, sarcoidosis, cancer, or other conditions. This is done using forceps or needles through the bronchoscope to obtain a specific tissue sample. The collected tissue (biopsies) can accurately identify cancer spreading in patients with lung cancer or other types of cancer.
11. Thoracoscopy: A thoracoscopy is a medical procedure that utilizes a thin, flexible tube with a light and attached camera at the end to examine the cavity within the chest and the surface of the lungs. It is performed to identify the underlying causes of lung problems, such as coughing up blood and difficulty breathing, and to obtain tissue samples (biopsy) from abnormal lung tissue, the chest wall, lymph nodes, or the pleura (lining of the lung). This procedure is commonly used for patients who have lung cancer and mesothelioma.
12. Thoracentesis: A pulmonologist conducts thoracentesis to address pleural effusion, which is the accumulation of fluid around the lungs. During this procedure, a needle is inserted into the chest wall, and a plastic catheter is attached to it. The excess fluid is then suctioned out from the pleura. After the procedure, the catheter is removed and properly disposed of.
13. Pleurodesis: For patients experiencing recurring pleural effusions, a medical procedure called pleurodesis is often recommended. During this procedure, a pulmonologist makes an incision in the chest wall and inserts a plastic tube into the chest cavity. An irritating chemical is then sprayed around the lung, causing the inflamed pleura to stick tightly to the chest wall, preventing the re-accumulation of fluid around the lung.
14. Indwelling Pleural Catheter:
A pleural catheter is used as an alternative to pleurodesis for treating recurrent pleural effusion (fluid around the lung). This procedure involves the insertion of a plastic catheter under the skin and into the chest cavity, with its tip placed inside. As fluid builds up around the lung, a healthcare professional can use sterile supplies to drain the indwelling pleural catheter at home.
15. Endobronchial Ultrasound (EBUS): This interventional procedure involves using a bronchoscope, a thin tube with a bright light inserted through the patient's mouth and down to the windpipe and bronchi. The bronchoscope has a small camera that allows a pulmonologist to visually examine the airways, blood vessels, lungs, and lymph nodes on an ultrasound monitor. Additionally, a needle is attached to the bronchoscope to extract fluid and tissue samples from the patient's lungs and surrounding lymph nodes. This procedure is referred to as transbronchial needle aspiration.
16. Percutaneous Tracheostomy: Percutaneous dilational tracheostomy is a frequently used medical procedure for critically ill patients. It is typically performed on those experiencing short-term respiratory failure and requiring prolonged mechanical ventilation. This procedure involves creating a surgically generated airway that remains open with a breathing or tracheostomy tube inserted directly into the trachea through a neck incision. A flexible bronchoscope is necessary during the procedure to ensure proper positioning of the oral endotracheal tube.
17. Bronchoscopic Cryobiopsy: A new procedure has been developed for identifying lung diseases by taking a sample of lung tissue. It involves using a bronchoscope with a flexible cryoprobe tool to reach inside the lung. The process can be done with a specialized cryoprobe or cryotherapy spray in the airway. The cryoprobe works by freezing tissue to collect a sample that can be evaluated further.
18. Bronchoscopic Cryotherapy: Cryotherapy is a medical procedure that utilizes extreme cold to freeze and eliminate abnormal cells. Pulmonologists often use this technique to treat certain types of cancers, including lung cancer, by inducing tissue necrosis or cellular death. This is accomplished using a specialized cryoprobe attached to a bronchoscope or administering a cryotherapy spray. Cryotherapy is also referred to as cryoablation.
Bronchoscopic cryotherapy can address various medical conditions, such as foreign body removal, endobronchial biopsy, transbronchial biopsy, and the treatment of benign and malignant central airway obstruction.
19. Bronchoscopic Thermoplasty: Thermoplasty is a respiratory procedure designed for individuals with severe asthma who do not respond to medication. During a bronchoscopy, a pulmonologist uses a heat probe to apply heat to the airway walls. This heat eliminates a layer of smooth muscle responsible for the constriction that leads to asthma symptoms.
20. Lobectomy: A lobectomy may be necessary when one part of a lung is damaged or diseased. This surgical procedure removes the affected lobe, leaving the remaining healthy tissue to function normally. Conditions requiring a lobectomy include tuberculosis, emphysema, lung abscess, fungal infections, and lung cancer.
21. Pneumonectomy: Pneumonectomy is a surgical procedure involving removing one of a patient's lungs due to trauma, cancer, or other diseases. The most common reason for this procedure is lung cancer, and other conditions may include congenital lung disease, traumatic lung injury, tuberculosis, and bronchiectasis. Usually, healthcare professionals aim to remove some lung tissue.
22. Bullectomy: This type of surgical procedure is performed to remove lung air pockets. The lungs contain various tiny air sacs known as alveoli that can grow into larger spaces called bullae when they are damaged. Bullae are significant lung air pockets that can develop due to certain medical conditions like emphysema and COPD. Pulmonologists may suggest removing bullae when they cause breathing difficulties or other health problems.
23. Lung Volume Reduction Surgery (LVRS): Patients suffering from severe emphysema or end-stage chronic obstructive pulmonary disease may undergo lung volume reduction surgery (LVRS) to improve their lung capacity, breathing ability, and overall quality and quantity of life. This surgery can be performed using open sternotomy, video-assisted thoracoscopic surgery, or thoracotomy.
24. Pulmonary Endarterectomy: Pulmonary thromboendarterectomy is a complicated surgical procedure that involves removing scar tissue and old blood clots from the pulmonary arteries in the lungs. The procedure helps to eliminate the blockages, which restores normal blood pressure and blood flow in the lungs while reducing the strain on the right side of the heart. By removing these clots, the heart and lungs can function better, leading to a general improvement in well-being.
25. Pulmonary Wedge Resection: It is a surgical procedure to remove a wedge-shaped small piece of tissue from the lung. It is typically done for individuals with early-stage lung cancer, metastatic tumours, bullous lung disease, tuberculosis, and lung nodules or lesions. This procedure is most effective when the cancer or disease is identified early and only affects a small area.
Health and Diseases Information
Why choose PACE Hospitals?
- A Multi-Super Speciality Hospital.
- NABH, NABL, NBE & NABH - Nursing Excellence accreditation.
- State-of-the-art Liver and Kidney transplant centre.
- Empanelled with all TPAs for smooth cashless benefits.
- Centralized HIMS (Hospital Information System).
- Computerized health records available via website.
- Minimum waiting time for Inpatient and Outpatient.
- Round-the-clock guidance from highly qualified super specialist doctors, surgeons and physicians.
- Standardization of ethical medical care.
- 24X7 Outpatient & Inpatient Pharmacy Services.
- State-of-the-art operation theaters.
- Intensive Care Units (Surgical and Medical) with ISO-9001 accreditation.