Bronchoscopy Test - Procedure Indications, Treatment, Surgery & Cost
At PACE Hospitals, the latest endoscopic suite is equipped with world-class HD Video Bronchoscope to perform minimally invasive major and supra-major bronchoscopy procedure.
Our team of the best pulmonologist in Hyderabad and lung specialist are having extensive experience in performing bronchoscopy procedure.
Request an Appointment for Bronchoscopy Procedure
Bronchoscopy Procedure - appointment
Why choose PACE Hospitals for Bronchoscopy Test?
5000+ Bronchoscopy Test Performed
Advanced 3D HD Video Bronchoscope
Team of the Best Bronchoscopy Doctors
All insurance and TPAs accepted
What is a Bronchoscopy test and its purpose?
Bronchoscopy meaning
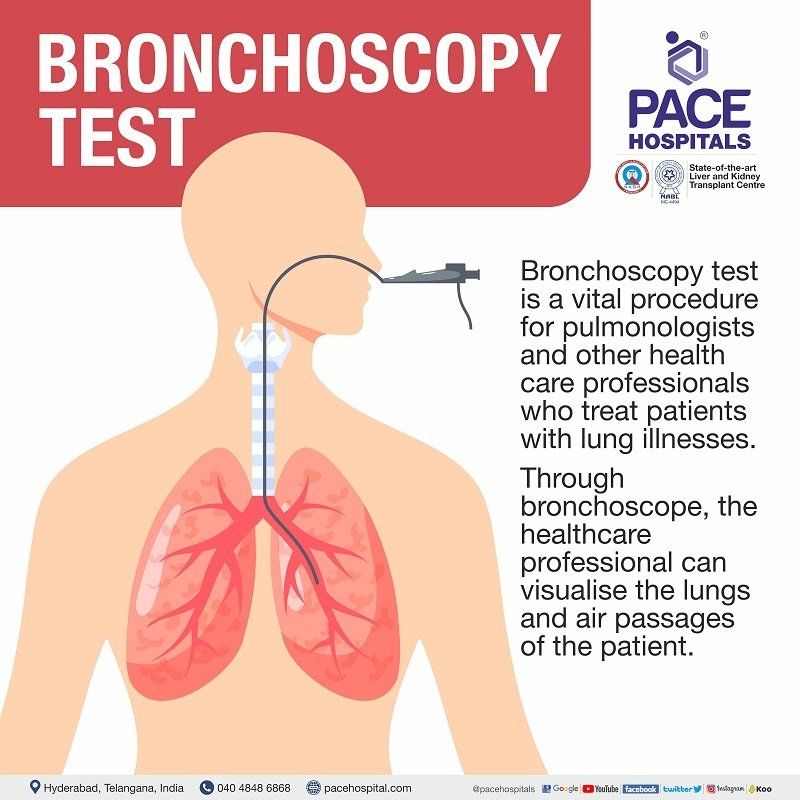
The Bronchoscopy test is a vital procedure for pulmonologists and other health care professionals who treat patients with lung illnesses. Through a bronchoscope, the healthcare professional can visualize the lungs and air passages of the patient.
Usually through the nose or mouth, and sometimes through a tracheostomy (a surgical opening from the exterior to the trachea which makes the patient capable of breathing when normal breathing is impaired), a long instrument equipped in tiny video recording apparatus capable of remote control is inserted into the airways which enabling the pulmonologist to visualise the anomalies (which could include bleeding, tumours, or inflammation) or any foreign materials.
The bronchoscope is also equipped with high precision apparatus (such as optical alligator grasping forceps) which can be utilised to extract specimens from the lungs or to remove foreign body objects or other blockages from the lungs or airways
What are the uses of Bronchoscopy procedure?
These are some situation when Bronchoscopy procedure is used by a doctor for the patients:
Diagnosis - diagnosing the problems related to lungs such as a lung disorder or a lung infection or a lung disease or a lung cancer or a collapsed lung or tumor that are causing someone a chronic coughing, coughing up blood, blood in sputum, shortness of breath, blockages in the airways. Simultaneously diagnosing some autoimmune or interstitial lung disease (ILDs) such as Sarcoidosis.
Assessing damage – checking the damage causes by inhaling chemicals or toxic gases.
Biopsy
– Various types of tissue samples are collected from airways and lungs depending on the necessity like BAL (Bronchoalveolar Lavage – fluid is injected into the airways and recollected), endobronchial biopsy and transbronchial lung biopsy, protective specimen brushing. These samples will be sent for different microbiological and pathological investigations. The treatment or mode of management of the patient depends on these tests.
Foreign objects removal and drainage - drainage of lung abscess, removal of mucus plug, foreign body objects in the airways; dilatation of a narrowed or blocked airway. It is also used in the patients who are on ventilator for clearing airway secretions and getting samples to rule out lung infection
Types of bronchoscopy test
There are 2 types of bronchoscopy test.
- Rigid bronchoscopy
- Flexible bronchoscopy
Rigid bronchoscopy: In this procedure a straight tube which can be used to observe only the larger airways. Bronchoscopy with rigid bronchoscope is an old method and is less preferable. Within the bronchi, it can be used to:
- Take out a lot of secretions or blood obstructing the lungs.
- Stop the bleeding
- Take out any foreign objects.
- Take out any diseased tissue (lesions)
- Perform procedures like stents and other treatments etc
Flexible bronchoscopy: It is relatively new and is more commonly used. It can be moved into smaller airways (bronchioles) which could not be possible with the former. The flexible bronchoscope can be used for:
- Inserting a breathing tube into the airway to assist with oxygen delivery.
- Suctioning out the secretions, if any.
- Collecting tissue samples (biopsy)
- Injecting the medication into the lungs.
From the last 10–15 years, pulmonology department have witnessed a tremendous development in the field of interventional pulmonology. A few of novel bronchoscopes are as follows:
- Convex EBUS – Endobronchial Ultrasound
- Ultrathin bronchoscope
- Radial EBUS
The considerations of a pulmonologist before performing a bronchoscopy procedure to any tentative patient
Before planning bronchoscopy test, it is crucial to conduct a thorough evaluation of the indications and contraindications. In some instances, contraindications may overcome the indications. In some instances, another invasive procedure may be preferable. If the patient presents with an abnormal mediastinum (the partition between the lungs), endoscopic ultrasound with biopsy via the oesophagus or via the trachea should be considered.
Cutting the financial burden: It is the duty of the pulmonologist to make every effort possible involving their scientific and medical acumen to maximise diagnostic yield by obtaining the diagnosis within a single (rather than repeated) procedure, thus cutting the financial burden, discomfort, pain and the time of the patient.
Justification for bronchoscopy test:
- This is the length of brainstorming and daunting work that goes before any patient who is subjected to bronchoscopy because although it is a minimally invasive procedure, it is nonetheless invasive.
- Every justification for bronchoscopy must be substantiated to the patient, with careful considerations for invasive and non-invasive options before diagnosis or therapy.
Pre-bronchoscopy plan:
- The pulmonologist will analyse to make sure that the necessity of bronchoscopy is justified for the indication by reviewing the medical history of the patient and the associated radiographic images of the disease.
- Once the necessity is justified, a pre-bronchoscopy plan will be formulated taking into consideration all the bronchoscopic and non-bronchoscopic procedures which are necessary to widen the diagnostic yield or therapeutic success.
- The patient is then informed about the bronchoscopic necessity and this discussion also concludes the safety issues, such as what the patient may be expected after the bronchoscopy and the comfort levels necessary for the procedure.
For instance, if bronchoscopy test indicates no anomalies in the airways, the bronchoscopist should be prepared to undertake transbronchoscopy sampling (biopsy – a small portion of the inner mass is cut and removed through bronchoscopy as the doctor cannot be able to analyse through bronchoscopy). In this instance, yield may be raised if radiographic guidance is utilised, and is unquestionably increased if on-site cytopathologic examination is conducted. Ethically, informed consent is acceptable because patients "have a right to know,".
The bronchoscopy test can be variedly utilised for the examination of the lung cancer or other pulmonary diseases (referring to lung and respiratory origins) especially the central airways. Diagnostic sensitivity of bronchoscopy test increases when the tumour (abnormal growth of tissue which could be either cancerous or non-cancerous in nature) is more centrally located (> 90%) and decreases when the tumour is located more peripherally in the airways (10-30%).
Indications for diagnostic bronchoscopy test include:
- Diffuse or localised lung infiltrates (any substance denser than air such as blood, protein, pus, oedema, or cells which stays within the lung),
- Recurrent and/or unresolved pneumonia (inflammation, infection and filling of air sacs in the lungs called alveoli with fluid or pus),
- Haemoptysis (blood coming from cough as small flecks in the mucus or enormous quantity due to impaired lung function),
- Persistent cough,
- Bronchiectasis (abnormal broadening of either the bronchi or the branches which could be a risk for any pulmonary infection) and
- Other symptoms of endobronchial obstruction (hinderance in the airways).
Indications for therapeutic bronchoscopy test include:
- Airway obstruction due to secretions with accompanying atelectasis (partial collapse or incomplete inflation of the lung),
- Removal of foreign objects or endobronchial tumour tissue,
- Insertion of stent (a temporarily splint placed inside the bronchi or bronchioles which helps in healing/relieving an obstruction or to help in breathing),
- Laser removal of tumour,
- Drainage of lung abscess (inflammation and pus-filled cavity in the lung), and other conditions.
Contraindications of Bronchoscopy procedure
- Severe cardiac decompensation (Inability of the heart to eject and/or receive blood within physiological pressure levels due to structural or functional change),
- Unstable angina (a type of throbbing chest pain caused by insufficient blood flow through the arteries of the heart muscle, which can result in heart attack),
- Cardiac arrhythmias (irregular heart beat),
- Recent myocardial infarction (death of heart tissue due to unavailability of oxygen from blood),
- Dysregulated diabetes,
- Unstable bronchial asthma,
- Severe impairment of lung function, hypoxemia (low volume of blood in the body), and
- Severe untreated hypertension (blood pressure) are all contraindications.
- Because of the risk of pneumothorax, (lingering of air or gas in the cavity between the lungs and the chest wall, resulting in lung collapse) transbronchial biopsy should not be performed in patients on mechanical ventilation.
As with all patients enduring invasive procedures, careful consideration must be given to antithrombotic therapy that may increase the likelihood of bleeding, such as in patients with
- Mechanical heart valves,
- Atrial fibrillation (very rapid or irregular heart rhythm), or
- Deep vein thrombosis (blood flow from other parts of body to heart is impaired. Most evident in legs).
Bronchoscopy Test Procedure
What to expect during Bronchoscopy procedure?
The bronchoscopy procedure may be performed on an outpatient basis, which implicates that the patient shall be returning to their home within the same day. Bronchoscopy test depends on the ailment and the methods used by the healthcare professional. Typically, bronchoscopy comprises the following:
- After the physician explained the method of bronchoscopy test and obtained the informed consent, the patient may be asked to remove his/her clothing in order to wear a clinical gown which the hospital/clinic provided.
- During the removal of clothing, the patient is also asked to remove jewellery and other personal items he/she may possess at the time of the examination.
- The patient will be made to sit comfortably sit on the procedure table with the head kept in an elevated position and may receive a dose of antibiotics through intravenous route (medication sent into the body directly through a vein) in your arm.
- The antibiotics may be administered both prior and after the procedure.
- In the majority of the cases, the patient will be conscious throughout the procedure but in some cases, the patient may be given general anaesthesia which renders him/her unconscious, especially if the physician uses a rigid bronchoscope.
- In case of patient being conscious, a mild sedative may be given which helps in relaxation. In addition, a liquid anaesthetic will be administered superficially on the nose and throat of the patient which helps in numbing so that the patient would be insensitive to the discomforts of the procedure.
- Monitoring of the sedation degree, respiratory rate, heart rate and oxygen saturation is done during the procedure.
- Oxygen may be administered via nasal tube or face mask. During the procedure, the regularities of the heart rate, blood pressure, and breathing will be monitored.
- A spray of anaesthetic will be administered to the back of the throat of the patient, which can help in suppressing the gag reflex that is necessary for the prevention of vomiting and nausea during the passage of the bronchoscope down the throat. Despite the availability or non-availability of mint flavoured local anaesthetic, the patient must be warned of the unpleasant aftertaste of the anaesthetic. Once the passage of the tube was completed, owing to the local anaesthetic, the gag reflex and the after-taste usually subsides.
- Neither speaking nor swallowing will be possible during the procedure. As a necessary precaution, usually the saliva will be suctioned from the buccal cavity (mouth) of the patient.
- The physician will move the bronchoscope down the patient's throat and into the airways, during which the patient may experience mild discomfort. Nevertheless, care will be taken so that the airway will not be obstructed, and it is possible for the patient to breathe around the bronchoscope. If needed, given additional oxygen will also be provided.
- As the bronchoscope is passes beyond the vocal cords, the entire airway is carefully examined. Specifically, endobronchial lesions (a region in an organ or tissue which has suffered damage through injury or disease, such as a wound etc) or mucosal abnormalities, as well as any signs of constriction or dynamic collapse, are evaluated.
- Based on the procedure's indication, the physician selects the appropriate instruments to perform specific tasks, such as tissue sampling (cutting a small sample of the tissue for tests) or tumour debulking (removing the tumour in the lungs). Images and videos can be archived for future use. Unnecessary contact with the mucosa is being avoided by the physician to avoid any trauma.
- As the bronchoscope is retracted, the patients’ lungs will be inspected. Other procedures may be performed if necessary, such as administering medication or staunching a wound (stop the blood flow from the wound). A final assessment of the airway will be performed at the conclusion of the procedure to ensure adequate haemostasis (stopping the flow of blood).
- When the examination and other procedures have been completed, the bronchoscope will be removed, which culminates the procedure.
What to expect after Bronchoscopy procedure?
Post-procedure the patient will be guided to a recovery room and will be kept under a watch until the sedation/general anaesthesia wears off. Patients who were under general anaesthesia may experience deliriums while waking up.
Until the patient is fully awake, any form of eatable or drinkables were not provided as they can cause nausea/vomiting. Recovery can range from one to three hours.
To determine the presence of a pneumothorax, a necessary post-procedural chest x-ray may be developed.
The results of tests or biopsies done during the procedure may take a few days to obtain. Nevertheless, a preliminary observation can be expected from the doctor.
After an uneventful recovery and in the absence of complications, the patient is eligible for same-day discharge. As the effects of the medications may last for several hours, the patient is advised not to drive, operate heavy machinery, or engage in any activity requiring full consciousness for the remainder of the day.
The soreness in the throat with a low-grade fever can be expected to persist for a day or two. The patient must contact the doctor in case of:
- Persistent chills or fever
- Persistent cough or throat pain
- Coughing up blood
- Shortness of breath
- Chest pain or trouble breathing.
Risks / Complications of bronchoscopy procedure
Bronchoscopy-related complications are uncommon, with a 0.01% lethality. Pneumonia (bacterial/viral lung infection, in which the air sacs fill with pus), haemorrhage (internal blood loss), cardiac arrhythmias (irregular heartbeat), and pneumothorax (presence of air/gas in the cavity between the lungs and the chest wall, causing lung collapse) are the most prevalent adverse effects. The risks or complications of bronchoscopy test are two types:
- Medication induced (pharmacological)
- Complications from the procedure (mechanical)
Medication induced (pharmacological)
- An overdose of local anaesthetics can cause neuropathy (disease/dysfunction of one or more peripheral nerves causing numbness/weakness), seizures (sudden, uncontrolled electrical disturbance in the brain causing changes in the behaviour, movements or feelings, and in levels of consciousness), and coma (prolonged unconsciousness) in the central nervous system.
- Methemoglobinemia (Methemoglobin is a form of haemoglobin that cannot carry oxygen. Increased methemoglobin in the blood is methemoglobinemia)
- Most sedatives can cause hemodynamic effects such as low blood pressure or heart rate.
- Malignant hyperthermia (abnormally high body temperature due to failure of the heat-regulating mechanisms) and prolonged neuromuscular paralysis (interruption of nervous transmission by nerve or muscle disease) can occur as a result of general anaesthetics.
Complications from the procedure (mechanical)
Bleeding: Bleeding is usually self-limiting (stopping on its own without any medical intervention) in most cases. A careful check for haemostasis (stopping the flow of blood) must be done and if severe bleeding is found, prompt management will be performed which includes:
- Intravenous administration of antifibrinolytics
- The patient is positioned laterally with the bleeding lung in a situation of dependence
- Vasoconstrictors are administered by bronchoscope at the location of bleeding
- In the event of continuing bleeding, the pulmonologist can consult the cardiac arrest healthcare professionals.
Pneumothorax: It can occur after transbronchial biopsies in 1-3% of patients.
- While small pneumothoraces can be treated conservatively, the symptomatic and large pneumothoraces necessitate the doctor to perform chest tube insertion, requiring the hospitalisation of the patient.
- The doctor looks out for the signs of tension pneumothorax (air is trapped in the pleural space, displacing mediastinal structures, and compromising cardiopulmonary function) as it causes hemodynamic instability (hypotension in the circulatory system to keep blood flowing reliably to all the various body parts) even in the absence of imaging studies.
- Immediate life-saving measures, such as chest tube insertion, should be taken.
- It must be understood that most pneumothoraces after bronchoscopy occur within the first hour of the procedure, but they can occur up to 24 hours later.
- Appropriate instructions and follow-up should be given to the patient.
Cardiac arrhythmias: can also occur, especially in patients with a history of heart disease. Other potential complications of the procedure include:
- vocal cord trauma,
- pneumomediastinum (air in mediastinum),
- hypoxia (low amount of oxygen in the tissues of the body), and,
- in rare cases, death.
Questions that the patients can ask the healthcare team about the Bronchoscopy Test?
Before the consent is provided for the test or process, the patient must be made aware of the following thoroughly:
- What is the test or procedure's name?
- Is the concerned patient eligible for the procedure (free of contraindicative features)?
- What is the absolute necessity for undergoing the test or procedure?
- Any other tests or treatments which can be considered?
- What kind of findings can be anticipated and their implications?
- What is the test's or procedure's risks and advantages?
- What are the potential adverse effects or complications?
- When and where the test or operation will be performed?
- Who will do the test or process, and what are their credentials?
- Who will do the test or process, in case of the unavailability of the concerned doctor?
- What would happen in the case of unavailability of the test or procedure?
- When and how will shall the results of the test be received?
- Whom to contact in case of concerns or issues following the test or process?
- How much will the test or operation cost, and what is the mode of payment?
- Is this test covered by the insurance?
Bronchoscopy Test Cost in Hyderabad, India
The cost of a Bronchoscopy Test in Hyderabad generally ranges from ₹ 4,500 to ₹ 28,000 (approximately US $55 – US $340). The exact Bronchoscopy cost in India varies depending on whether the bronchoscopy is diagnostic or therapeutic, the use of local or general anaesthesia, whether biopsy or lavage is performed, the type of bronchoscope used (flexible or rigid), the patient’s respiratory condition, and the hospital facilities chosen — including cashless treatment options, TPA corporate tie-ups, and assistance with medical insurance approvals wherever applicable.
Breakdown of Bronchoscopy test price in accordance with procedures
- Flexible Bronchoscopy (Diagnostic) –
₹ 4,500 – ₹ 15,000 (US $55 – US $180)
- Bronchoscopy with Biopsy / BAL (Bronchoalveolar Lavage) –
₹ 14,000 – ₹ 22,000 (US $170 – US $270)
- Rigid Bronchoscopy (Therapeutic / Foreign Body Removal) –
₹ 18,000 – ₹ 28,000 (US $220 – US $340)
- Bronchoscopy with Endobronchial-Ultrasound (EBUS) – ₹ 20,000 – ₹ 35,000 (US $245 – US $425)
Frequently asked questions (FAQs) on Bronchoscopy Test
What are the benefits of bronchoscopy test?
The main benefits of bronchoscopy includes the diagnoses and treatment of various lung problems which are undetected in other imaging test such as mediastinoscopy, X-ray etc.
- Airway obstructions due to tracheal deviation towards the side of collapse of lung lobes can be detected by chest X-ray.
- However, often it becomes difficult to distinguish the collapse of lung lobes from a large pulmonary effusion (thick mucus production in lungs).
- Through bronchoscopy procedure, not only the distinction is possible but even the thick mucus secretions can be suctioned out to clear the plugging which in turn caused the collapse of lobes in first place.
- Patients with airway bleeding can develop blood clots that result in bronchial obstruction.
- Bronchoscope can aid not only in the evacuation of blood from the airway, but also in the allowance of other adjunctive treatments to treat the bleeding lesions.
- Studies demonstrated that Endobronchial ultrasound (EBUS) was more sensitive (88% vs. 91%) and more accurate (92% vs. 89%) when compared to mediastinoscopy for evaluating lymph node in lung cancer.
What is a bronchoscopy biopsy?
The bronchoscopy apart from visualising any anomalies in the airways of the patient, can also be used for bronchoscopy biopsy (also called transbronchoscopy sampling) where a small portion of the inner mass is cut and removed through bronchoscopy as the bronchoscopist cannot be able to analyse through the mass through bronchoscopy).
Can bronchoscopy detect TB (tuberculosis)?
Yes, a bronchoscopy is a reliable and safe approach for the diagnosis of pulmonary tuberculosis in individuals with negative sputum smear (smear containing smaller bacterial load). Sputum collected after bronchoscopy improves overall diagnostic sensitivity.
Are you sedated for a bronchoscopy?
Usually, the patient will be conscious during the procedure and will be provided with a, mild sedative may be given which helps in relaxation. In addition, a liquid anaesthetic will be administered superficially on the nose and throat of the patient which helps in numbing so that the patient would be insensitive to the discomforts of the procedure.
What is a bronchoscopy wash?
During bronchoscopy, the surface of the airways is washed with mild salt solution to collect cells for microscopic evaluations to find infections or even cancer cells.
Can bronchoscopy treat atelectasis?
Yes, as per the research data, a bronchoscopy procedure is effective in the treatment of atelectasis (partial collapse or incomplete inflation of the lung) with high success rates. Atelectasis is a frequent complication seen in the ICU and prolonged atelectasis may worsen hypoxemia (low level of oxygen in blood) thus predisposing the patient to nosocomial (hospital acquired) pneumonia.
Can bronchoscopy treat pneumothorax?
No. Pneumothorax is a rare complication of bronchoscopy is rare. It can be treated with other procedures such as observation, needle aspiration, chest tube insertion, nonsurgical repair or surgery.
Can you drink water before bronchoscopy?
No. At least six to twelve hours prior to the procedure, it is better if the patient could refrain from any eatables / beverages to avoid any unnecessary complications. However, clear fluids such as black tea and coffee, water and juice can be taken up to two hours prior to appointment time.
How long does a bronchoscopy take?
The bronchoscopy procedure may take from 15 min to 45 min depending on the co-operation of the patient, the type of bronchoscope used, the indication and the type of samples that needs to be taken. Although the duration of total procedure which includes the preparation and recovery time is about 4 hours.
What is fiberoptic bronchoscopy?
Flexible fiberoptic bronchoscopy is a safe invasive diagnostic and therapeutic device which includes a light source, fibre optics, and a camera for diagnosis and treatment. Patients with haemoptysis (coughing up of blood.), chest infection, parenchymal lung illness, lung nodules or masses, persistent pulmonary infiltrates, mediastinal lymphadenopathy (swelling of lymph nodes in the chest, specifically in the region located between the lungs), and probable lung transplant rejection are frequently diagnosed. In addition, flexible fiberoptic bronchoscopy can be utilised therapeutically for foreign body aspiration, endobronchial mass ablation or debulking, airway stenosis, and lung lavage.
Does a bronchoscopy hurt?
No, it may not be painful but could be uncomfortable. The health care staff will make every effort to ensure your comfort. Using instruments passed through the bronchoscope, tissue and fluid samples can be collected and procedures can be performed. The physician may inquire about chest, back, or shoulder pain. Painkillers can be utilised in case of severe pain.
How much does a bronchoscopy cost in India?
The average cost of bronchoscopy test in India is approximately 7,800 (Rupees seven thousand eight hundred only). However, bronchoscopy cost in India ranges vary from ₹6,200 to ₹12,000 (Rupees six thousand two hundred to twelve thousands) and bronchoscopy test cost may vary depending upon the different private hospitals in different cities.