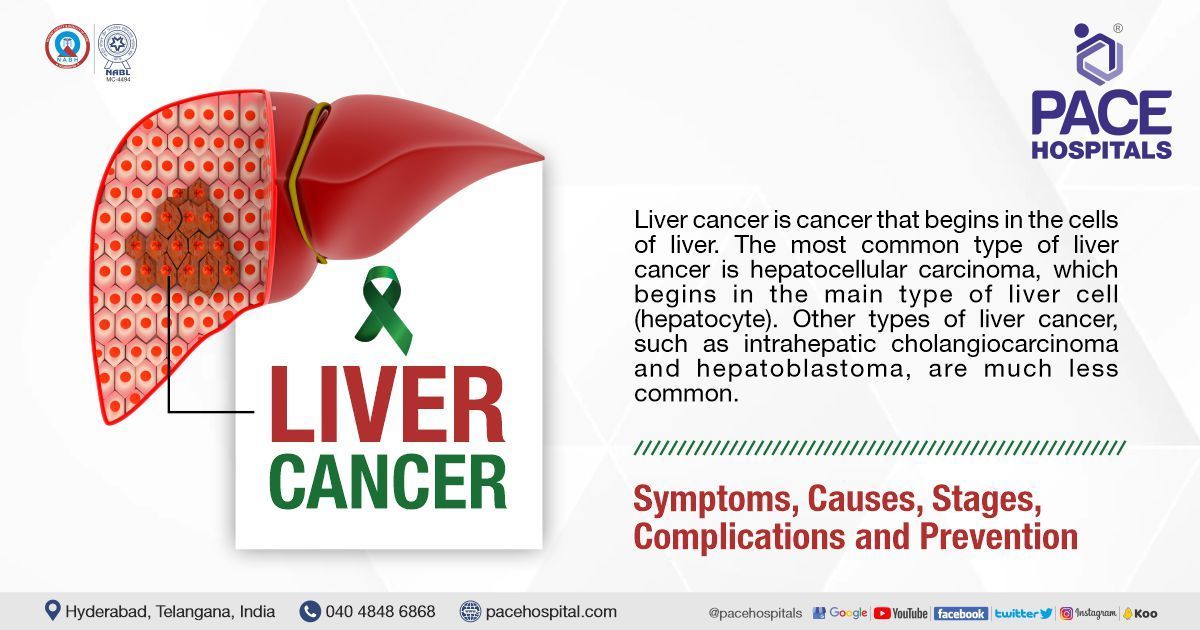
Liver Cancer Treatment in Hyderabad, India
PACE Hospitals, is one of the best hospital for liver cancer treatment in Hyderabad, India, having team of top liver cancer doctors in Hyderabad include hepatologist, liver transplant doctors. They are experienced in handling complex cases of liver related diseases and its complications such as cirrhosis of the liver, liver cancer, chronic liver disease, non-alcoholic fatty liver disease, alcoholic liver disease, liver parenchymal disease, autoimmune liver disease, cholestatic liver disease.
Request Appointment for Liver Cancer Treatment
Liver Cancer Treatment - appointment
Why Choose PACE Hospitals for Liver Cancer Treatment?

Dedicated Liver Intensive Care Unit for Acute and Chronic Liver Disease
Team of the Top Liver Cancer Doctors and Specialist with 35 + years of expertise
Equipped with latest technology for liver transplantation
CGHS, ECHS and All insurance accepted for cashless treatment
Liver Cancer Diagnosis
While there are various liver cancer diagnostic tests to identify different types of liver cancer, not every individual necessarily needs to undergo every test outlined here. When selecting a diagnostic test, the oncologist may consider the following:
- Suspected kind of cancer
- Symptoms and indicators
- Age and health condition
- The outcomes of previous medical exams
Usually, with noninvasive imaging, the diagnosis can be confirmed. Even when biopsy is needed, imaging is usually required for guidance. Before prescribing any laboratory tests or scans, the liver cancer specialist doctor looks for signs of liver cancer on the body of the patient. The doctor may perform the following tasks, such as:
- Palpation (feeling) of the abdomen to detect lumps, swelling, or other abnormalities in the liver, spleen, and other adjacent organs
- Search for peculiarities such as ascites (abnormal accumulation of fluid in the abdomen) and jaundice symptoms, such as yellowing skin and whites of the eyes.
- Search for liver decompensation with the development of encephalopathy (brain function loss due to damaged liver being incapacitated to remove toxins from blood) should raise a suspicion for hepatocellular carcinoma (liver cancer)
- Looking for engorged collateral veins (caput medusa, also known as the palm tree sign, which are dilated superficial veins over the abdominal area).
Once the physical examination and the symptoms coincide with the history of the patient, the doctor may suspect various other diagnosis along with liver cancer. To confirm the diagnosis of liver cancer, the liver cancer specialist doctor may prescribe various other laboratory tests or scans, such as:
Blood tests: In conjunction with the physical examination, the physician will usually perform a blood test to detect alpha-fetoprotein (AFP).
- Approximately 50-70% of individuals with liver cancer in have increased levels of AFP in their blood.
- The doctor will also test the individual's blood for hepatitis B or C.
- Other blood tests may indicate the health of the liver.
- Usually, an increase of AFP above 500 mcg/L could be an indication of liver cancer.
Disadvantage of AFP: Although AFP has a crucial role in initiating monitoring and terminating the treatment of liver cancer.
- AFP cannot be used to assess therapy response, however, if its levels were not high before treatment.
- Approximately one-third of liver cancer patients do not have an elevated AFP level in liver cancer.
- In these patients AFP may render futile in the therapy of liver cancer
Ultrasonography: provides image of the body's internal components through ultrasound.
- The sound waves reflect off the liver and other organs, as well as malignancies.
- Each reflected wave produces a unique image on a computer display.
Computed tomography (CT or CAT) scan: Using x-rays gathered from many angles, a CT scan generates a three-dimensional representation of the body's interior.
- A computer merges the images to create cross-sectional view for any anomalies or malignancies.
- Occasionally, contrast medium - (dye) may be administered into the patient's vein before to the scan to improve picture detail.
- This dye may be injected into a patient's vein or administered orally as a drink.
- Typically, liver cancer may be identified based on CT scan findings that are unique to the malignancy.
- This aids patients in avoiding liver biopsies. A CT scan may be performed to determine the size of the tumour.
Magnetic resonance imaging (MRI): Instead of x-rays, an MRI employs magnetic fields to provide detailed pictures of the body.
- MRI may be used to assess the size of the tumour.
- Before the scan, a contrast material is administered to provide a more distinct image.
- This dye may be injected into a patient's vein or administered orally as a drink.
Angiogram: A radiograph of blood arteries with an injected dye into the circulation to make the liver's blood vessels visible on an x-ray.
Laparoscopy: A laparoscope is a narrow, illuminated, flexible tube that enables the physician to view within the body during laparoscopy.
- The patient is anaesthetized as the tube is implanted via a minor abdominal incision.
- Laparoscopy is rarely used to diagnose liver cancer.
Liver Biopsy: the removal of a tiny sample of tissue from liver for microscopic examination and then analysed by a pathologist.
Biomarker testing of the tumour (also called as tumour molecular testing):
Laboratory tests for determining liver cancer by taking blood and analysing it. Biomarker testing also determines the treatment choices including targeted therapy.
Liver Cancer Staging System
There have been a number of staging systems developed for the purpose of determining the prognosis of liver cancer, such as:
- Tumour-node metastasis (TNM) (the most widely used of these staging systems)
- Okuda system of staging liver cancer and
- American Joint Committee on Cancer (AJCC)
- Barcelona Clinic Liver Cancer (BCLC) systems, and
- Cancer of the Liver Italian Program (CLIP) score
- Groupe d'Etude du Traitement du Carcinome H'epatocellulaire (GRETCH),
- Chinese University Prognostic System (CUPI), and
- Japan Integrated Staging (JIS) systems
The Barcelona Clinic Liver Cancer (BCLC) method is often used by medical professionals to understand the stage of liver cancer through which the treatment choices can be managed and manipulated. The BCLC method classifies liver cancer according to the features of the tumour, as well as liver function, performance status, and symptoms associated with malignancy.
The BCLC stage groupings include:
Very early stage: is defined if the size of the tumour is less than two centimetres.
- There is no indication of a rise in pressure in the portal vein, (one of the primary veins that carry blood out from the liver).
- The amounts of bilirubin, which is the component that is responsible for jaundice, are typical.
- In most cases, surgical intervention is suggested.
Early stage. The tumour is smaller than 5 cm.
- The liver function could fluctuate.
- It is possible to expect two types of conditions:
- There could be an increase or a normalised portal vein pressure accompanied by normal or
- There could be an increase in portal vein pressure and in bilirubin levels.
- Those who are diagnosed with the illness at an earlier stage may be candidates for
- liver transplantation
- surgical intervention or
- radiofrequency ablation (RFA).
Intermediate stage. There may be more than one tumour, or the tumour itself may be rather enormous. The treating oncologist often recommends:
- Regional therapy, such as trans-arterial chemoembolization,
Advanced stage: The tumour has made its way into the portal vein or has migrated to other regions of the body, such as
- the lungs,
- the lymph nodes, or
- the bones.
- Targeted treatment is often recommended by the oncological team.
While there is no general agreement over which staging method is the most accurate among renowned oncologists, various studies that have compared multiple staging systems have found that these systems have diverse prognostic values when applied to different patient groups.
- There are various evidences pointing out the chances of certain scoring system being the most optimal for a particular patient group.
- Clinical staging systems, such as the BCLC and CLIP systems, may have more prognostic value for patients with advanced liver cancer and cirrhosis who are not candidates for surgery.
- On the other hand, pathologic staging systems, such as the AJCC and TNM staging system, may be superior to clinical staging systems in prognosis classification for patients who have surgical resection.
Liver cancer differential diagnosis
There are various conditions which can mimic the symptoms of liver cancer that include:
- Dysplastic nodules in cirrhosis (nodules with a diameter of 1 mm or more, show abnormal tissue development, and lack definite histopathologic findings of malignancy).
- Fibrous nodular hyperplasia (the most frequent benign, non-neoplastic, reactive growth of the liver).
- Primary hepatic lymphoma (rare type of primary liver tumour and an unusual type of lymphoma, usually presenting with constitutional symptoms such as:
- hepatomegaly but without lymphadenopathy and
- extrahepatic lymphomas i.e., bone marrow, other lymphoid tissue, spleen).
- Cholangiocarcinoma (bile duct cancer).
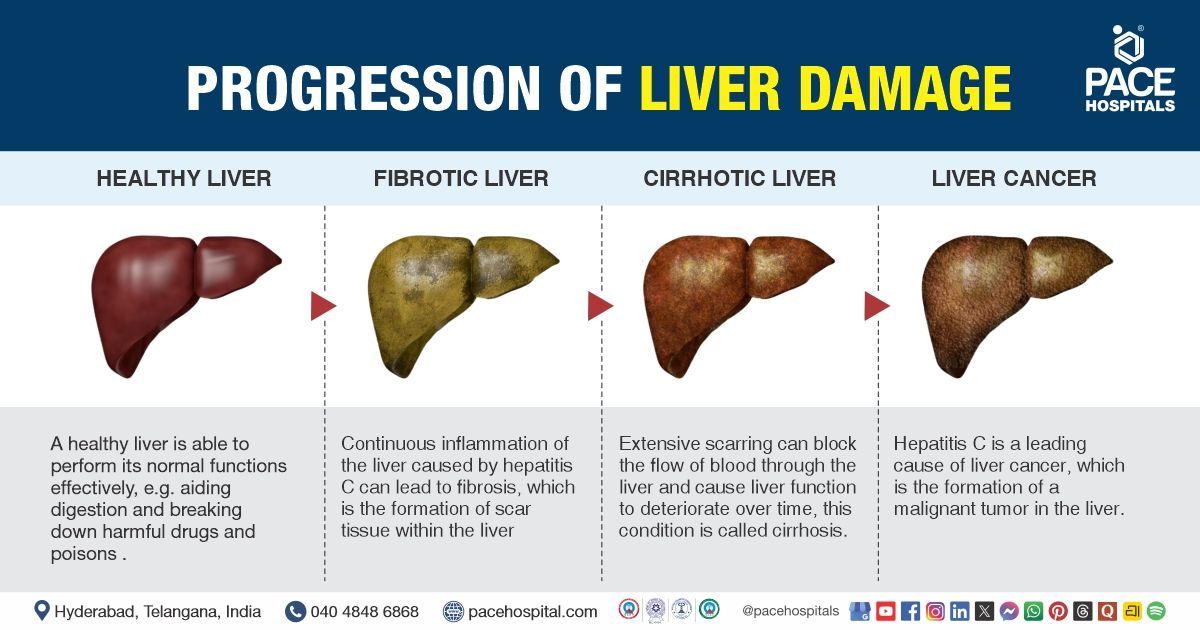
- Cirrhosis (advanced liver-stage disease where the healthy liver tissue is replaced with scar tissue, permanently damaging the liver).
- Hepatocellular Adenoma
(Hepatic Adenoma) (rare, but benign epithelial tumours of the liver frequently associated with oral contraceptive pill use).
The goals of a multidisciplinary team before treating a liver cancer
Each type of treatment has a different goal. The goal of liver cancer treatment is to do one or more of these things:
- Remove the cancer in the liver (or the entire liver) while doing as little damage as possible to nearby areas
- Kill cancer cells or keep them from growing or spreading
- Keep the cancer from coming back or delay its return
- Ease symptoms of the cancer, such as pain or blockages
The treatment of liver cancer is increasingly multidisciplinary, and the selection of multimodal therapy options are necessarily done on an individualised basis according to the complicated interplay of tumour stage and the amount of underlying liver disease, as well as the patient's overall general condition.
The treatment is basically patient centric and the oncologist takes consideration of various variables such as the
- the size of the cancer
- location and stage of the tumour, as well as
- the general health
- the fitness levels of the patient.
A thorough discussion takes place involving the Oncologist and Liver Cancer Specialist Doctors patient and the patient’s caregivers. It is in these discussions the doctor explains the condition of the patient to the patient and caregivers. The oncologist, apart from providing necessary knowledge of the treatment options also take the preferences of patient into account.
A multidisciplinary team consisting of several specialists would be contributing to the treatment plan, focussing on the tailor cut optimal care. The specialists include:
- Interventional radiologists: to provide patient care information by analysing imaging tests.
- Oncologic-oriented hepatologists: for expert opinion on the best choices (systemic therapy or chemotherapy) for therapy optimised for patient
- Hepatologists: for management of the novel systemic agents and their associated side effects.
- Radiation oncologists: are more common in those patients who require external beam irradiation as a part of therapy.
- Pathologists: to provide analysis of tissue samples by utilising biomarkers, thus steering the therapy
- Gastroenterologists: with their tacit role, their contribution lies in their extensive education to remain current in liver cancer management.
- Surgical oncologists: are useful in recognising and performing resection in patients with early liver cancer
- Oncology nursing staff: a critical component of patient care, the nursing force ensure patient compliance and treatment adherence.
- Primary care physicians: for preliminary screening and surveillance of the disease
- Oncology dietitians: for adjusting and developing a diet during radiation therapy.
- Oncology counsellors: Providing specialized counselling education, and boosting up the patients’ morale.
Frequently asked questions (FAQs) on Liver Cancer
Is fatty liver a sign of cancer?
Fatty liver could be a sign of liver cancer. Liver cancer can be linked with obesity. In the last two decades, there has been a more than doubling in the number of cases of non-alcoholic fatty liver, which currently affects almost one-fourth of the country's population.
NAFLD causes inflammation and scarring in the liver, which is comparable to the damage produced by excessive alcohol use. Additionally, the condition raises the chance of developing liver cancer.
Which Is the best hospital for Liver Cancer Treatment in Hyderabad, India?
PACE Hospitals, Hyderabad, is one of the leading centres for the diagnosis and treatment of Liver Cancer, including Hepatocellular Carcinoma (HCC) and metastatic liver tumors.
Our multidisciplinary team of hepatologists, gastroenterologists, oncologists, interventional radiologists, and liver surgeons provides comprehensive, evidence-based care for:
- Early-stage liver cancer
- Intermediate-stage liver tumors
- Advanced or metastatic liver cancer
- Liver cirrhosis with cancer
- Post-TACE/ablation follow-up
- Cancer-related pain, nutrition, and supportive care
We are equipped with advanced imaging, PET-CT, TACE, radiofrequency ablation, microwave ablation, liver cancer surgery, targeted therapy, and 24/7 emergency support, PACE Hospitals ensures accurate diagnosis, timely treatment, and improved outcomes — supported by cashless insurance, TPA tie-ups, and complete documentation assistance.
What is the biggest risk factor for liver cancer?
Chronic viral hepatitis is the biggest risk factor for liver cancer.
Chronic infection with the hepatitis B virus (HBV) or the hepatitis C virus (HCV) is the most prevalent cause of liver cancer. This is because chronic infection lasts for a long period of time. Cirrhosis of the liver is the result of these infections, which are also responsible for the fact that liver cancer is the most frequent kind of cancer in many regions of the globe.
What is the first sign of liver cancer?
Liver cancer may not show any apparent signs and symptoms during its development. Any form of noticeable symptoms can be observed over time with the development of cancer. While the early signs differ from person to person, the common early warning signs include:
- Constant and insidiously growing pain in the upper abdomen on the right side or near the right shoulder blade.
- Ascites (abdominal swelling) or bloating in the abdomen that could sometimes be felt.
- Hepatomegaly (enlarged liver) can be felt under the ribs on the right side
- Jaundice (yellowing of the skin and eyes)
How long can you live with liver cancer?
The length of time a person can live with liver cancer depends on a number of factors, including the stage of liver cancer, the type of cancer, the person's overall health, and their response to treatment.
Overall survival rates for liver cancer by stage:
- Localized liver cancer: 31%
- Regional liver cancer: 11%
- Distant liver cancer: 3%
Median survival rates for liver cancer by stage:
- Localized liver cancer: 34 months
- Regional liver cancer: 11 months
- Distant liver cancer: 4 months
Some people with liver cancer may survive for many years, while others may live for only a few months. Early diagnosis and treatment are essential for improving the chances of survival.
What Is the cost of Liver Cancer Treatment at PACE Hospitals, Hyderabad?
At PACE Hospitals, Hyderabad, the cost of liver cancer treatment typically ranges from ₹1,800 to ₹3,25,000 and above (approx. US $22 – US $3,900), offering an affordable and specialised option for advanced liver cancer care. However, the final cost depends on:
- Type and stage of liver cancer (HCC vs. metastatic)
- Need for imaging (ultrasound, CT, MRI, PET-CT)
- Requirement for TACE, ablation, or surgery
- Targeted therapy or immunotherapy cycles
- Extent of liver function impairment (cirrhosis, hepatitis history)
- Duration of hospital stay
- Nutrition and supportive care needs
- Associated complications (ascites, jaundice, bleeding)
Early-stage cancers requiring imaging and medical therapy fall at the lower range, while advanced-stage tumors requiring TACE, targeted therapy, surgery, or multiple interventions fall toward the higher range.
After full evaluation, imaging, and multidisciplinary discussion, our specialists provide a personalized treatment plan and a transparent cost estimate based on your clinical condition and treatment goals.
What causes liver cancer?
Mutations in DNA cause liver cancer. there are various risk factors which encourage the process.
- Hepatitis C infection
- Hepatitis B infection
- Hepatitis D infection
- Cirrhosis
- Non-alcoholic steatohepatitis
- Alcoholism
- Tobacco use
- Aflatoxin B1,
- Butter-yellow
- Nitrosamines
- Haemochromatosis;
- α-1-antitrypsin deficiency;
- Prolonged immunosuppressive therapy in renal transplant patients;
- Clonorchiasis
- Schistosomiasis.
What are the symptoms of liver cancer in humans?
Most people with liver cancer are asymptomatic (don't have any symptoms) in the initial stages of the development, but those who have had it for a while may start to notice them as a result of the liver illness it causes. Patients show a wide variety of symptoms of liver cancer, which could include:
- Weight loss
- Nausea and Vomiting
- Diarrhoea
- Constipation
- Bloating
- Ascites (pain and distention in the abdomen)
- Encephalopathy (impaired brain functions due to viral infection/toxins/conditions)
- Jaundice (yellowish discolouration of skin, eyes due to high level of bilirubin)
- Hematemesis (blood vomiting)
- Hypoglycaemia (low blood sugar levels)
- Erythrocytosis (high concentration of red blood cells)
- Hypercalcemia (increased calcium levels in body)
- Acute watery diarrhoea
Can smoking cause liver cancer?
Researchers have shown a link between excessive smoking and liver cell damage, which manifests as
- Necroinflammation (the inflammatory response to cell death)
- Apoptosis (programmed cell death)
- An excess accumulation of iron in the liver
These consequences may be traced back to an excessive amount of iron, which then led to iron accumulation in the hepatocytes. Oxidative stress and lipid peroxidation are both caused by an excess of iron in the liver. Oxidative stress produces free radicals abich in turn causes causes cancer.
What not to eat with liver cancer?
There are various foods which are not to be eaten when diagnosed with liver cancer. Some them are:
- Saturated or trans fats, such as red meats, full-fat milk, and pastries
- Added sugars, such as sweetened beverages, cakes, cookies, and candies
- Salts, such as sodium-rich canned soups, cured meats, and potato chips
- Alcohol consumption
Which alcohol causes liver cancer?
All alcoholic drinks, including red and white wine, beer, and liquor, are linked with cancer. The higher the amount of drink, the higher the risk of cancer.
Ethanol is the form of alcohol present in alcoholic beverages such as beers, wines, liquors (distilled spirits), and other beverages.
A regular size drink of any sort –
- 12 ounces of beer
- 5 ounces of wine, or
- 1.5 ounces of 80-proof liquor
has about the same amount of ethanol (about half an ounce). Larger or "stronger" cocktails may contain more ethanol than this.
Overall, it is the quantity of alcohol consumed over time, rather than the kind of alcoholic beverage, is the most relevant factor in increasing cancer risk.
Which fruits and vegetables give cure of liver cancer patients?
In order to maintain healthy liver function, it is essential to consume a diet that is both well-rounded and abundant in foods high in fibre. Oncologists may recommend the consumption of a broad range of foods to get the best possible health results, such as:
- Fruits and vegetables, such as apples and leafy greens
- Whole grains, such as whole-wheat bread, brown rice, quinoa, and oats
- Lean protein sources, such as skinless chicken, fish, tofu, and beans
- Low fat dairy products, such as fat-free milk, cheese, and yogurt
- Nuts and seeds
- In some cases, oncologists may encourage to increase the calorie or protein intake.
What is the survival rate for liver cancer?
- Stage 0: The median survival time for stage 0 liver cancer without therapy is more than 3 years. With therapy, 70-90% of patients will live for 5 years or longer. To treat stage 0 liver cancer, you may have a resection procedure, a liver transplant, or treatment to kill the tumour, generally using heat (ablation therapy).
- Stage A: Without treatment, the median survival for stage A liver cancer is 3 years. With treatment, 50 – 70% of the patients survive for 5 years or more. Liver resection can be done to treat the patient suffering with stage A liver cancer. Liver transplant or ablation therapy may also be used.
- Stage B: Without treatment, the median survival for stage B liver cancer is 16 months. With treatment, the median survival for stage B liver cancer is 20 months. To treat stage B liver cancer, trans arterial chemoembolization (TACE) may be administered.
- Stage C: Without treatment, the median survival for stage C liver cancer is between 4-8 months. With treatment, the median survival for stage C liver cancer is between 6-11 months. To treat stage C liver cancer, targeted therapies may be utilised.
- Stage D: Without treatment, the median survival for stage D liver cancer is less than 4 months. Although there are no treatments for stage D liver cancers, the doctors and specialist continue palliative therapy to treat any symptoms.
Can liver cancer be cured?
Yes, liver cancer can be cured, especially if it is diagnosed and treated early. The cure rate for early-stage liver cancer is around 70%. There are a number of different treatments for liver cancer, depending on the stage of the cancer and the patient's overall health. Treatment options include:
- Surgery: Surgery to remove the tumor or the entire liver may be an option for early-stage liver cancer.
- Liver transplant: A liver transplant may be an option for patients with more advanced liver cancer or those with underlying liver disease.
- Ablation: Ablation therapy uses heat or cold to destroy cancer cells.
- Embolization: Embolization therapy involves blocking the blood supply to the tumor, causing it to shrink or die.
- Targeted therapy: Targeted therapy drugs attack specific molecules that are involved in the growth and survival of cancer cells.
- Immunotherapy: Immunotherapy drugs help the body's own immune system to fight cancer cells.
Even if liver cancer cannot be cured, there are treatments that can help to control the cancer and improve the patient's quality of life.
What age is liver cancer common?
Liver cancer is most common in people over the age of 40. The average age at diagnosis is 63. Liver cancer is more common in men than in women. However, liver cancer can occur at any age, including in children. The risk of liver cancer increases with age because the liver accumulates damage over time. This damage can be caused by a number of factors, including:
- Chronic hepatitis B virus (HBV) or hepatitis C virus (HCV) infection
- Cirrhosis of the liver
- Nonalcoholic fatty liver disease (NAFLD)
- Alcohol abuse
- Obesity
- Smoking
- Diabetes
- Certain genetic conditions
Is liver cancer very painful?
Liver cancer pain can vary from mild to severe, depending on the size and location of the tumor, as well as the stage of the cancer. Some people with liver cancer do not experience any pain, while others may have excruciating pain that is difficult to manage.
The most common type of pain associated with liver cancer is a dull, aching pain in the upper right abdomen. This pain is caused by the tumor pressing on the liver or on nearby organs.
Can a blood test detect liver cancer?
Yes, a blood test can detect liver cancer, but it is not a perfect test. There are two main blood tests that are used to detect liver cancer:
- Alpha-fetoprotein (AFP) test: AFP is a protein that is produced by the liver. High levels of AFP in the blood can be a sign of liver cancer, but it can also be caused by other conditions, such as hepatitis and cirrhosis.
- Liver function tests (LFTs): LFTs measure the levels of certain enzymes and proteins in the blood that are produced by the liver. High levels of these enzymes and proteins can be a sign of liver damage, which can be caused by liver cancer or other conditions.
If a blood test shows high levels of AFP or abnormal LFT results, it does not mean that you have liver cancer. However, it does mean that you need further testing to rule out liver cancer and other conditions.
Other tests that may be used to diagnose liver cancer include imaging tests, such as ultrasound, MRI, and CT scans, and a liver biopsy.
Does liver cancer spread quickly?
Yes, liver cancer can spread quickly. It can spread to other parts of the liver, as well as to other organs in the body, such as the lungs, bones, and brain. The speed at which liver cancer spreads depends on a number of factors, including the type of liver cancer, the size and location of the tumor, and the patient's overall health.
Some types of liver cancer are more aggressive than others and are more likely to spread quickly. For example, hepatocellular carcinoma (HCC) is the most common type of liver cancer and is also the most aggressive type. HCC can spread to other organs in the body within a few months of diagnosis.
The size and location of the tumor can also affect how quickly liver cancer spreads. Larger tumors are more likely to spread to other organs than smaller tumors. Tumors that are located near the blood vessels or lymph nodes are also more likely to spread.
The patient's overall health can also affect how quickly liver cancer spreads. Patients with weakened immune systems are more likely to develop metastatic liver cancer, which is liver cancer that has spread to other organs in the body.
How painful is end stage liver cancer?
End-stage liver cancer can be very painful, but the severity of pain varies from person to person. Some people may experience mild to moderate pain, while others may have severe pain. The pain can be constant or intermittent, and it may be accompanied by other symptoms such as nausea, vomiting, fatigue, and jaundice.
The pain from end-stage liver cancer can be caused by a number of factors, including:
- The size and location of the tumor
- The tumor pressing on nearby nerves or organs
- Liver damage caused by the cancer
- Ascites (fluid buildup in the abdomen)
- Portal hypertension (high blood pressure in the portal vein)
- Metastasis (spread of the cancer to other organs)
Is jaundice last stage of liver cancer?
Jaundice is not necessarily the last stage of liver cancer, but it is a common symptom of advanced liver cancer. Jaundice is a yellowing of the skin and eyes caused by a build-up of bilirubin in the blood. Bilirubin is a waste product that is produced when red blood cells break down. The liver normally filters bilirubin from the blood and excretes it through the bile duct. However, when the liver is damaged, it cannot filter bilirubin as effectively, which leads to a build-up of bilirubin in the blood.
Jaundice can be caused by a number of different conditions, including liver cancer, hepatitis, cirrhosis, and gallstones. In people with liver cancer, jaundice is often caused by a tumor blocking the bile duct. Jaundice can be a sign that liver cancer has spread to other organs in the body, such as the lungs or bones. However, it is important to note that not everyone with jaundice has liver cancer.
Who is the best liver cancer specialist in Hyderabad for liver cancer treatment?
Liver cancer doctors at PACE Hospitals, who are among the top 10 liver cancer specialist in Hyderabad, with vast expertise in handling severe and critical cases of liver diseases with the help of the latest treatment modalities, are among the best liver cancer doctors in Hyderabad, India for liver cancer treatment.
What is liver cancer treatment cost in India?
Liver cancer treatment cost in India depends upon the multiple factors such as the patient's age, stage of liver damage and scarring, complications associated. It must be understood that the damage to the liver is permanent. Nevertheless, right time and early diagnosis can help in treating the causes and further any additional liver impairment must be avoided to slow the prognosis.