Fatty Liver - Symptoms, Grade, Causes, Complications, Prevention
PACE Hospitals
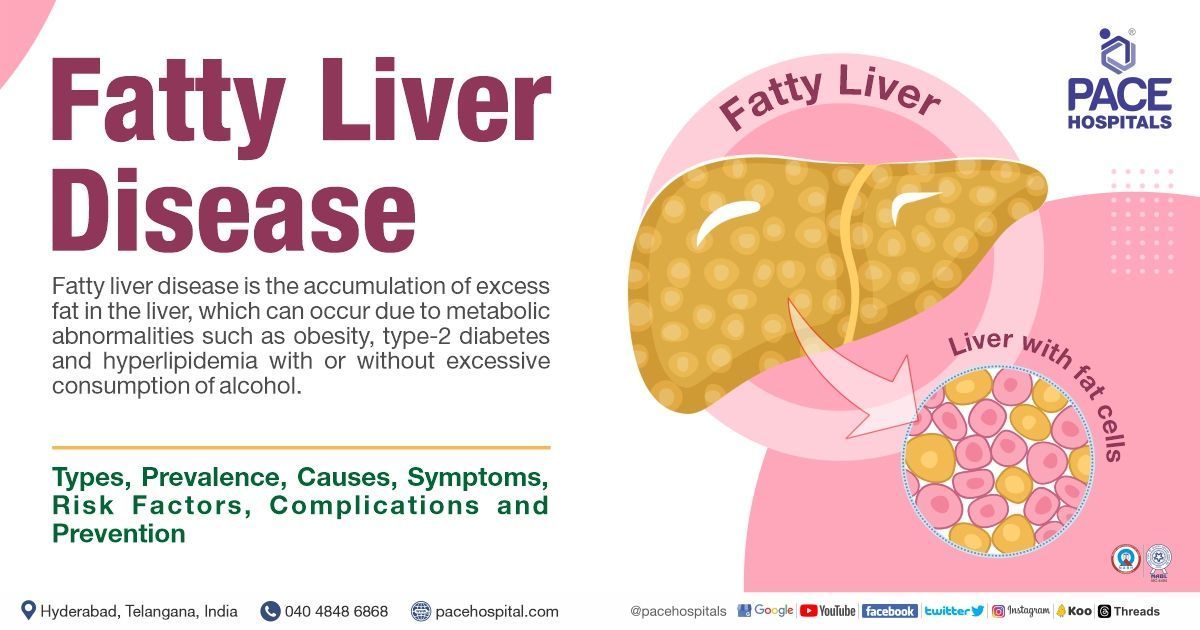
Fatty liver meaning
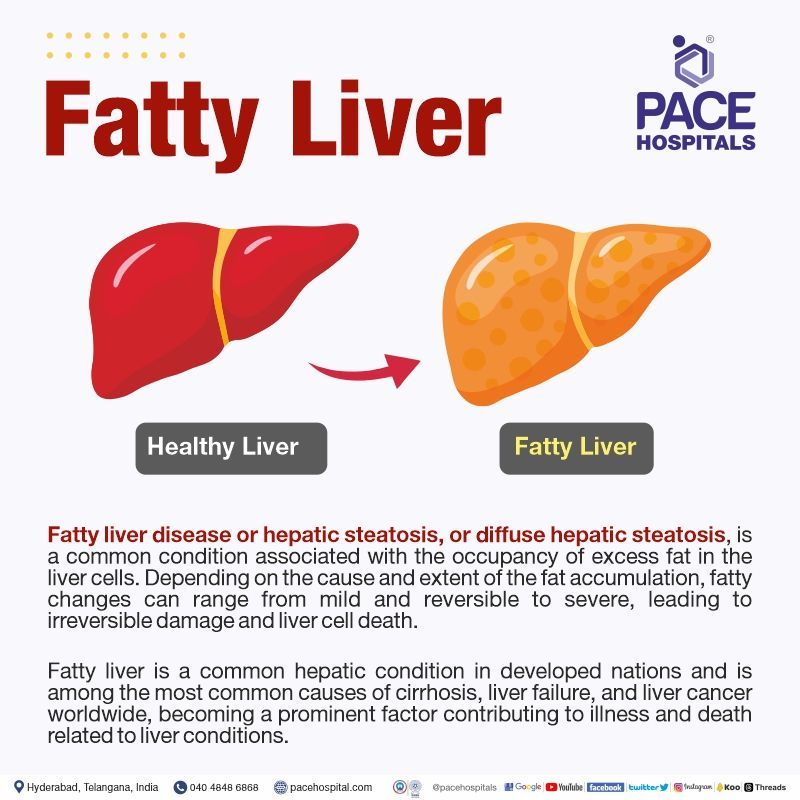
Fatty liver disease or hepatic steatosis, or diffuse hepatic steatosis, is a common condition associated with the occupancy of excess fat in the liver cells. The liver is the most frequent location for fat build-up since it plays a crucial role in the metabolism of fats. Usually, the liver contains some amount of fat, but when the deposition reaches or exceeds 5% of the liver cells (hepatocytes), it is treated as unhealthy.
Researchers predict that in the next one to two decades (10–20 years), fatty liver disease leading to cirrhosis will outnumber liver transplants caused by hepatitis C and excessive alcohol consumption. Depending on the cause and extent of the accumulation, fatty changes can range from mild and reversible to severe, leading to irreversible damage and liver cell death.
One can frequently avoid or even reverse fatty liver disease through modifications in their lifestyle if the patient is at the early stages of fatty liver.
Types of Fatty Liver Disease
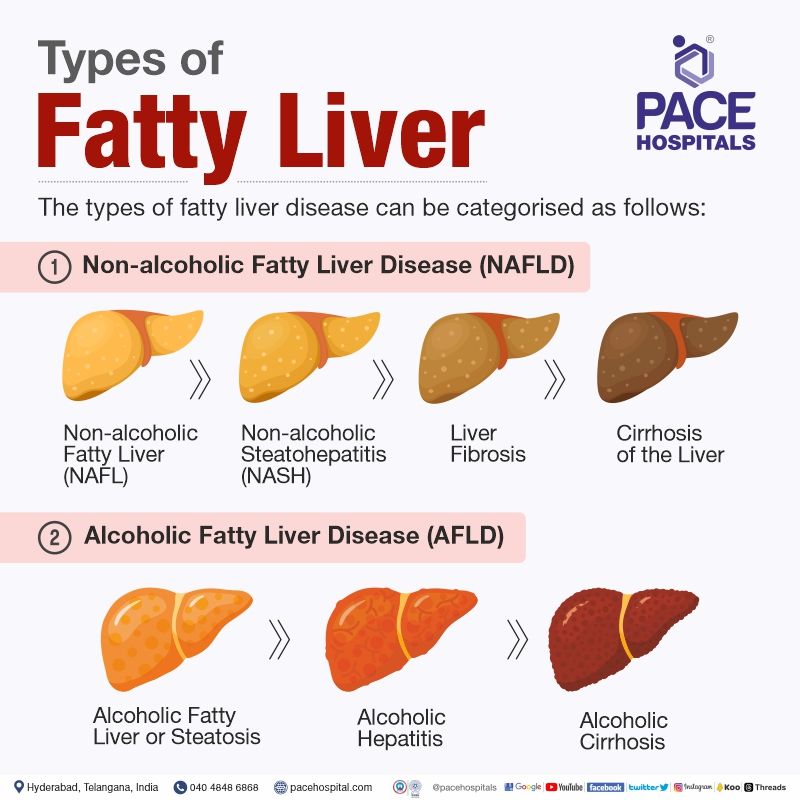
The types of fatty liver disease can be categorised as follows:
- Non-alcoholic Fatty Liver Disease (NAFLD)
- Alcoholic Fatty Liver Disease (AFLD)
Non-alcoholic Fatty Liver Disease (NAFLD)
It is an increasingly recognised fatty liver disease where fat builds up in the liver without excessive alcohol intake. It can lead to significant damage over the years. This condition is further divided into four stages.
The non-alcoholic fatty liver disease stages are as follows:
- Non-alcoholic Fatty Liver (NAFL)
- Non-alcoholic Steatohepatitis (NASH)
- Fibrosis
- Cirrhosis
Non-alcoholic Fatty Liver (NAFL): It is also known as a simple fatty liver condition characterised by fat deposition in the liver without significant inflammation or harm to the liver cells. This may result in abdominal discomfort or pain due to hepatomegaly (enlarged liver).
Non-alcoholic Steatohepatitis (NASH): This is a severe form of NAFLD condition characterised by fat accumulation, inflammation, and damage in the liver. NASH has the potential to advance to liver fibrosis, cirrhosis and liver cancer; it is important to note that NASH can be a coexisting condition with other liver diseases such as chronic hepatitis C.
NASH is categorised into two types:
- Primary, which is linked to obesity and diabetes without excessive alcohol consumption.
- Secondary, which is induced by drugs or toxins.
Fibrosis: Fatty liver fibrosis is a condition characterised by the formation of scar tissue (fibrosis) in the liver and adjacent hepatic blood vessels due to prolonged inflammation in the liver.
Cirrhosis: Fatty liver cirrhosis is the most advanced stage and emerges after prolonged inflammation, causing the liver to contract, develop permanent scarring, and become nodular in appearance. This damage is irreversible and can result in liver failure and risk of liver cancer.
Most individuals with non-alcoholic fatty liver disease typically exhibit the initial phase of the condition, known as simple fatty liver or steatosis, while only little progress to the more severe stages. The development of fibrosis or cirrhosis may take several years to occur.
Non-alcoholic fatty liver disease (NAFLD) is associated frequently with metabolic syndrome, characterised by obesity, diabetes, and hyperlipidaemia. As per a research study report, around 80% of individuals diagnosed with metabolic syndrome also present with NAFLD.
Alcoholic Fatty Liver Disease (AFLD)
Alcoholic fatty liver disease, also called alcoholic steatohepatitis, is one of the Alcoholic Liver Disease (Alcoholic Related Liver Disease - ARLD) conditions caused by excessive consumption of alcohol (≥ 40g in males, ≥ 20g in females) and is often a result of the metabolic effects caused by consuming moderate to high quantities of ethanol (alcohol). Ingesting such amounts of alcohol can lead to the development of fatty liver due to its impact on the body's metabolism.
In the consumption of alcohol, the liver metabolises most of it to eliminate it from the system. However, this breakdown process generates toxic compounds that can harm liver cells, trigger inflammation, and compromise the body's inherent defences.
Alcoholic fatty Liver Disease typically improves upon cessation (stoppage) of alcohol intake. However, if alcohol consumption continues, it can lead to severe liver problems.
The alcoholic fatty liver disease stages are as follows:
- Alcoholic Fatty Liver or Steatosis
- Alcoholic hepatitis
- Alcoholic cirrhosis
Alcoholic Fatty Liver or Steatosis: It is a common condition caused by alcohol-induced fatty liver. In this condition, the liver enlarges, which may or may not cause noticeable symptoms. Discomfort or pain can arise in the upper right area of the abdomen.
Alcoholic hepatitis: It is a condition characterised by inflammation of the liver, resulting in symptoms such as fever, nausea, vomiting, abdominal pain, and jaundice.
Alcoholic cirrhosis: This is the advanced stage where the liver cells develop fibrous scar tissue.
The extent of liver damage increases proportionally with the amount of alcohol consumed. Alcoholic fatty liver disease represents the initial phase of liver damage resulting from alcohol consumption, followed by alcoholic hepatitis and cirrhosis as progressive stages of alcohol-related liver disease.
Prevalence of Fatty Liver Disease
Fatty liver (hepatic steatosis) is a common hepatic condition in developed nations and is among the most common causes of cirrhosis, liver failure, and liver cancer worldwide, becoming a prominent factor contributing to illness and death related to liver conditions.
- As per a study reported in 2021, It was estimated that around 25% of the global population has Non-alcoholic fatty liver disease.
- As per a research report, the prevalence of fatty liver disease (NAFLD) ranges from 80% -90% in adults with obesity, 30%-50% in individuals diagnosed with diabetes mellitus, 90% or higher in patients with hyperlipidaemia, 3% to 10% in paediatric populations, and can reach as high as 40% to 70% among children who are obese.
- The incidence of NASH is expected to increase by up to 56% in the next decade, as per a 2020 research report, indicating a rise in the number of cases where individuals develop inflammation and damage in the liver due to fatty deposits.
- The occurrence of liver cancer, specifically hepatocellular carcinoma, caused by NAFLD will likely rise alongside the increasing rates of obesity on a global scale.
- An observational study found that the prevalence rates of steatosis (fatty liver) were 46.4% among heavy drinkers consuming more than 60 grams of alcohol daily. Additionally, among heavy drinkers who were also obese, the prevalence of steatosis was even higher, reaching 94.5%.
- Females experience a more rapid and severe progression of alcoholic liver disease (ALD) at lower alcohol consumption levels than males. This might be due to variations in alcohol processes in the liver, the production of cytokines, and the breakdown of alcohol in the stomach across men and women.
Fatty Liver causes
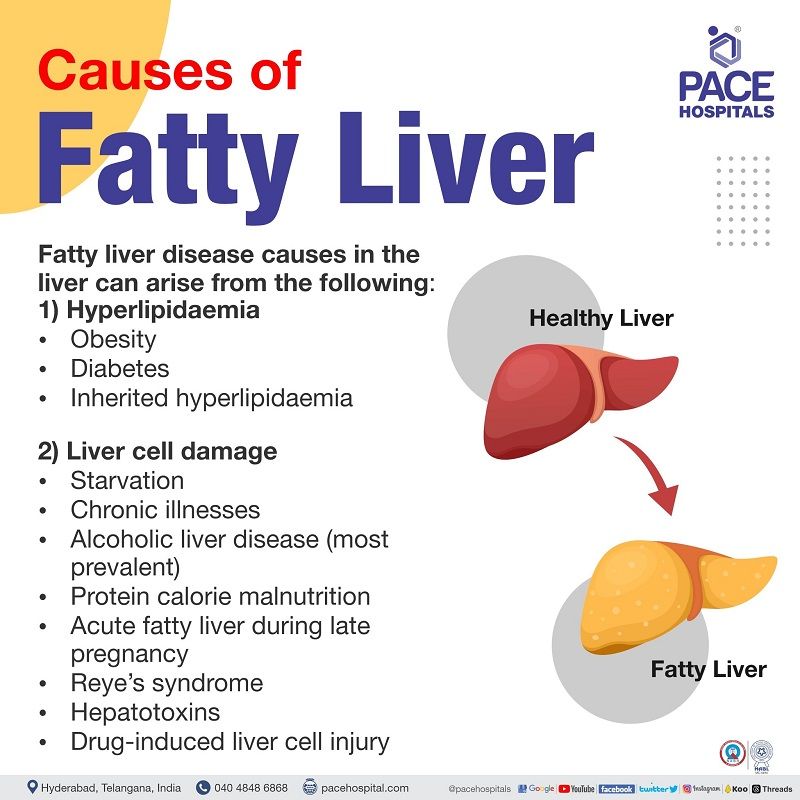
Fatty liver disease causes in the liver can arise from the following:
- Hyperlipidaemia
- Liver cell damage
Hyperlipidaemia: Excessive fat surpassing the liver's capacity to metabolise it. The following are the conditions that cause hyperlipidaemia:
- Obesity
- Diabetes
- Inherited hyperlipidaemia
Liver cell damage: Due to liver cell impairment, the liver fails to break down or process the accumulated fat. The following are the causes of liver abnormality:
- Starvation
- Chronic illnesses
- Alcoholic liver disease (most prevalent)
- Protein calorie malnutrition
- Acute fatty liver during late pregnancy
- Reye’s syndrome
- Hepatotoxins
- Drug-induced liver cell injury
Fatty Liver symptoms
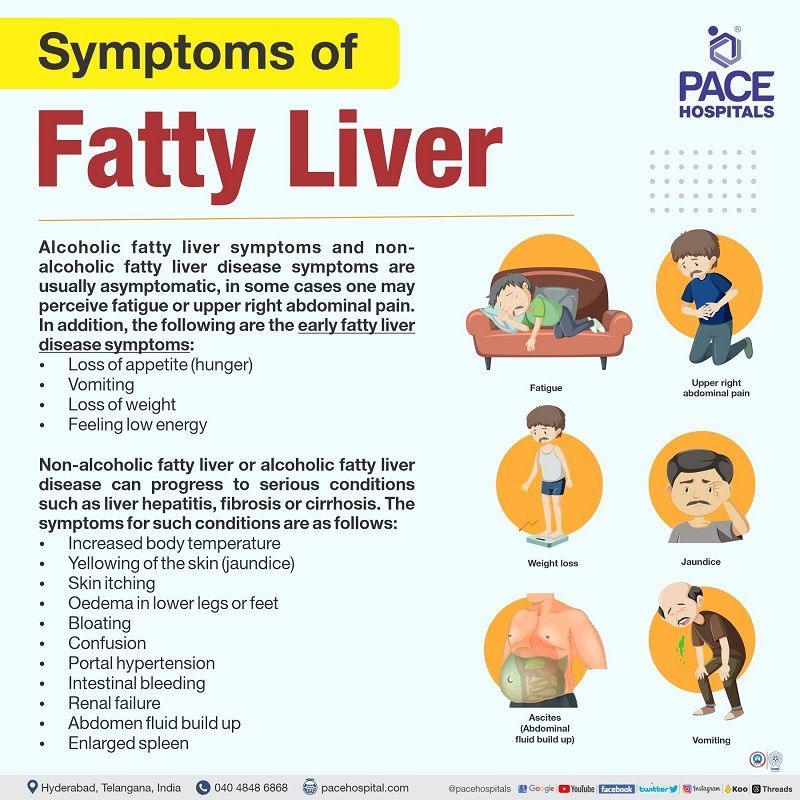
The fatty liver disease symptoms typically present as asymptomatic or with minimal symptoms, and the condition is typically detected incidentally during routine blood tests. In the instance of experiencing alcoholic fatty liver symptoms and non-alcoholic fatty liver disease symptoms, one may perceive fatigue or experience uneasiness in the upper right region of the abdomen, potentially caused by liver inflammation.
The early symptoms of fatty liver disease might include:
- Loss of appetite (hunger)
- Vomiting
- Loss of weight
- Feeling low energy
Non-alcoholic Fatty liver or alcoholic fatty liver disease can progress to serious conditions such as liver hepatitis or liver cirrhosis. The symptoms for such conditions are as follows, but not limited to:
- Increased body temperature
- Yellowing of the skin (Jaundice)
- Skin itching
- Oedema in lower legs or feet
- Bloating
- Confusion
- Portal hypertension
- Intestinal bleeding
- Renal failure
- Abdomen fluid build up
- Enlarged spleen
Fatty Liver symptoms in females
Fatty liver disease is more prevalent in women due to hormonal changes during pregnancy and the transition into menopause. The progression of this condition is gradual, and the initial stages may not exhibit noticeable symptoms. As it advances, the following are the fatty liver disease symptoms in females:
- Fatigue
- Abdominal uneasiness
- Oedema in the legs or abdomen
Women at risk of fatty liver disease must undergo routine medical examinations with their healthcare professionals to facilitate early identification and intervention.
Acute Fatty Liver of pregnancy
Acute fatty liver of pregnancy (AFLP) is a rare and critical condition occurring in about 5 out of 100,000 pregnancies that poses a significant risk to the health and lives of both the mother and foetus. It is primarily characterised by liver dysfunction (acute), and it usually occurs during the later stages of pregnancy. This condition requires immediate medical attention and intervention due to its potentially serious complications.
Acute fatty liver of pregnancy criteria includes the presence of liver dysfunction (acute) after 20 weeks of gestation period with supportive laboratory and clinical findings.
Acute Fatty Liver of pregnancy symptoms
Pregnant women with acute fatty liver of pregnancy (AFLP) typically exhibit the following symptoms during their third trimester of pregnancy:
- Nausea
- Vomiting
- Loss of appetite
- Abdominal pain
- Headache
- Confusion
- Anorexia
Some patients may also have high blood pressure and protein in their urine, which can be linked to conditions such as Hemolysis, Elevated Liver enzymes and Low Platelets (HELLP) syndrome or pre-eclampsia.
Fatty Liver of pregnancy complications
Acute fatty liver in pregnancy (AFLP) can cause liver failure associated with encephalopathy, coagulopathy, and hypoglycemia.
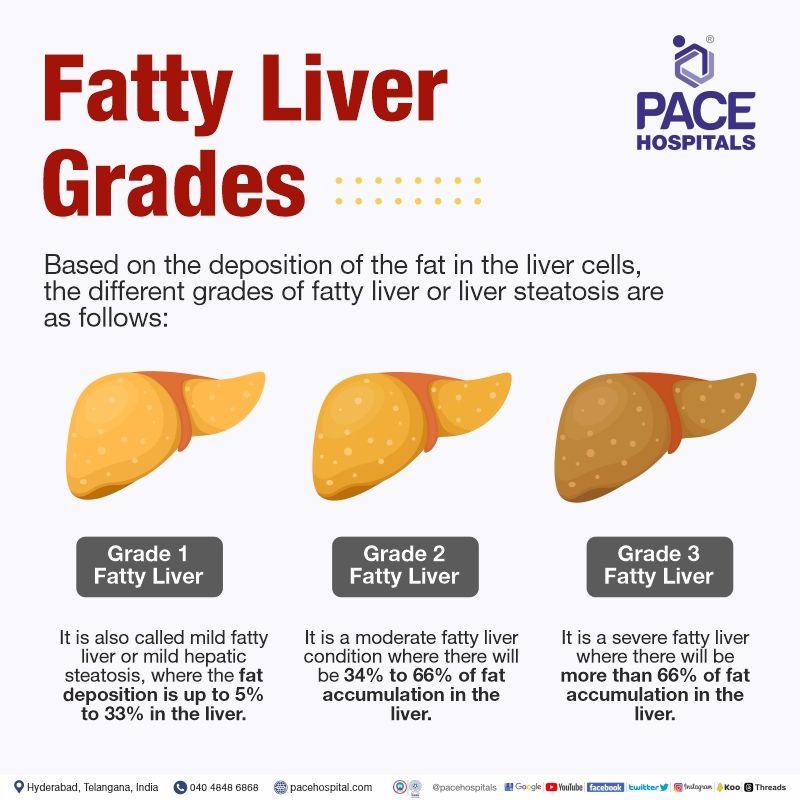
Fatty Liver grades
Based on the deposition of the fat in the liver cells, the different grades of fatty liver or liver steatosis are as follows:
- Grade 1 Fatty Liver or Grade 1 hepatic steatosis
- Grade 2 Fatty Liver or Grade 2 hepatic steatosis
- Grade 3 Fatty Liver or Grade 3 hepatic steatosis
Grade 1 Fatty Liver: It is also called mild fatty liver or mild hepatic steatosis, where the fat deposition is up to 5%-33%.
Grade 2 Fatty Liver: It is a moderate fatty liver condition where there will be 34% to 66% of fat accumulation.
Grade 3 Fatty Liver: It is a severe fatty liver where there will be more than 66% of fat accumulation in the liver.
Fatty Liver risk factors
One of the most common risk factors for fatty liver disease is obesity and consumption of alcohol (ranging from 40-80g daily from 10–12 years). With the increasing obesity in the population, there is a rise in the prevalence of fatty liver. In addition to the above, the following are the risk factors for non-alcoholic and alcoholic fatty liver disease, such as:
Non-alcoholic fatty liver disease
- Diabetes mellitus or Insulin resistance
- Older age
- Poor dietary habits
- Hyperlipidemia (high cholesterol levels)
- Hypertension (high blood pressure)
- Metabolic Syndrome (hypertension, hyperglycaemia, excess body fat around the waist and abnormal cholesterol levels)
- Infections such as Hepatitis C
- Hypothyroidism (underactive thyroid)
- Hypopituitarism (deficiency of the pituitary hormones)
- Exposure to toxins
- Genetic factors affecting alcohol metabolism
- Presence of Polycystic Ovarian Syndrome
Alcoholic fatty liver disease
- Women gender
- Pre-existing conditions like hepatitis C.
When compared to men, women have a higher risk of developing alcoholic hepatitis and cirrhosis from drinking the same amount of alcohol.
Fatty Liver complications
Complications of Non-alcoholic Fatty Liver Disease (NAFLD)
The severity of the following non-alcoholic fatty liver disease complications is proportional to the severity of the histology stage and grade of liver disease.
- Hepatocellular carcinoma
- Cardiovascular disease
- End-stage liver disease
Alcoholic Fatty Liver Complications
Alcoholic fatty liver disease (AFLD) complications are both common and rare. Common complications of alcoholic fatty liver disease:
- Spontaneous Bacterial Peritonitis
- Variceal Hemorrhage
- Hepatopulmonary syndrome
- Ascites
- Hepatic hydrothorax
- Hepatorenal syndrome
- Hepatic encephalopathy
Rare complications of alcoholic fatty liver disease:
- Portal vein thrombosis
- Portal gastropathy
- Liver cancer
- Cirrhotic Cardiomyopathy
- Portopulmonary hypertension
Fatty Liver diagnosis
The fatty liver disease diagnosis is often made incidentally when routine lab testing reveals abnormal liver function tests or imaging tests that reveal the presence of hepatic steatosis or inflammation of liver cells. The fatty liver diagnostic tests lack specificity and cannot differentiate NASH from NAFLD.
However, the following are the fatty liver test prescribed by the gastroenterologist or hepatologist to assess the fatty liver condition.
- Blood tests
- Imaging tests
- Liver biopsy tests
Blood tests for fatty liver disease
- Complete liver profile (LFT) that includes ALT, AST, alkaline phosphatase, bilirubin, albumin, International Normalized Ratio, etc
- Fibrosis-4 (Fib-4)
- NAFLD fibrosis score (NFS)
- Commercial fibrosis marker panels such as the Enhanced liver fibrosis (ELF) test, Fibro Test
- Lipid profile
- Iron levels
- Insulin resistance test
- Quantitative Insulin Sensitivity Check Index
- Homeostasis Model Assessment
In patients with persistently abnormal liver enzymes or a strong family history of cirrhosis, the following are the additional lab tests:
- Alpha 1-antitrypsin
- Anti-nuclear antibody
- Smooth muscle antibody
- Thyroid-stimulating hormone (TSH) levels
- Ceruloplasmin
Imaging tests for fatty liver disease
- Ultrasonography
- Computed tomography
- Magnetic resonance imaging (MRI)
- Radiologic techniques such as Fibro scan associated with ultrasound transient elastography, Acoustic radiation force impulse imaging, Magnetic resonance elastography (MRE)
Liver biopsy tests for fatty liver disease
- It is a gold standard for diagnosis of chronic hepatitis and fibrosis; however, depending on disease severity, laboratory values and risk factors of the patient, the gastroenterologist would prescribe liver biopsy, as this test is not indicated in patients with normal serum aminotransferases levels.
Fatty Liver treatment
Fatty liver disease treatment, also known as hepatic steatosis treatment, usually involves lifestyle modifications and management of fatty liver disease's underlying causes and associated risk factors such as excess body weight, elevated blood lipid levels, reduced insulin sensitivity, and type 2 diabetes.
Pharmacological interventions (medical and surgical management) for hepatic steatosis treatment should be restricted to individuals who have undergone a liver biopsy confirming the presence of non-alcoholic steatohepatitis (NASH) and fibrosis. They are as follows:
- Antioxidants (vitamin E therapy)
- Omega-3 fatty acids
- Glucagon-like-peptides (GLP1) agonists
- Statins (to treat dyslipidemia in fatty liver patients)
- Bariatric surgery (for morbidly obese patients)
- Liver transplantation (if the liver is damaged fully)
Fatty Liver Disease prevention
Fatty liver prevention can be done by practising healthy lifestyle habits such as:
- Losing 5% to 10% of healthy body weight
- Exercising regularly
- Consuming a balanced diet that includes limited intake of salt, sugar, and oils and increased intake of proteins, whole grains, fruits and vegetables
- Controlling the existence of conditions such as hypertension, diabetes and hyperlipidaemia by taking the prescribed medications
- Avoiding alcohol consumption
Fatty Liver vs Normal Liver
The normal healthy liver contains traces of fat; however, if it accounts for more than 5 % of the liver, it is known as fatty liver. The differences between normal liver and fatty liver are as follows.
| Elements | Normal Liver | Fatty Liver |
|---|---|---|
| Physical finding (By percussion) | The mean size of regular healthy liver is 7cm in women and 10.5 cm in men (normal values) | Fatty liver is 2 to 3 cm larger than normal size |
| Liver shape | Cone and dark reddish brown | Enlarged and discoloured |
| Lab values | Normal levels of liver function tests | Abnormal liver function tests such as ALT, AST, Albumin, Alkaline phosphatase etc. |
| Symptoms | No symptoms | Loss of appetite, vomiting, weight loss, fatigue, abdominal pain, itchy skin etc |
Non-alcoholic Fatty Liver vs Alcoholic Fatty Liver
Both Non-alcoholic fatty liver and Alcoholic fatty liver disease are liver problems which are treatable at the initial stage with the help of lifestyle modifications such as abstinence from alcohol, daily exercise and diet changes. However, the following are the differences between them.
| Elements | Non-alcoholic Fatty Liver | Alcoholic Fatty Liver |
|---|---|---|
| Steatosis | Accumulation of excess fat in the liver due to metabolic abnormalities | Accumulation of excess fat in the liver due to the excessive consumption of alcohol (40g in males, 20-30g in females) |
| Signs and symptoms | Fatigue, obesity, abdominal pain, enlarged liver, darkened pigmentation around the neck and joints | Jaundice, weight loss, diarrhoea, and portal hypertension |
| Risk factors | Obesity, Type2 diabetes, and hyperlipidaemia | Alcohol intake, women gender, preexisting conditions like hepatitis C |
| Treatment | Lifestyle modifications: weight reduction, manage the diseases like type 2 diabetes, hypertension, and hyperlipidaemia | Alcohol abstinence, Nutritional support, and Glucocorticosteroids for inflammation |
FAQs (frequently asked questions on Fatty Liver Disease)
Share on
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868