Liver Cancer - Symptoms, Causes, Types, Complications and Prevention
PACE Hospitals
Overview | Types | Symptoms | Causes | Risk Factors | Stages | Complications | Diagnosis | Treatment | Prevention | FAQs | When to consult a Doctor
Liver cancer definition
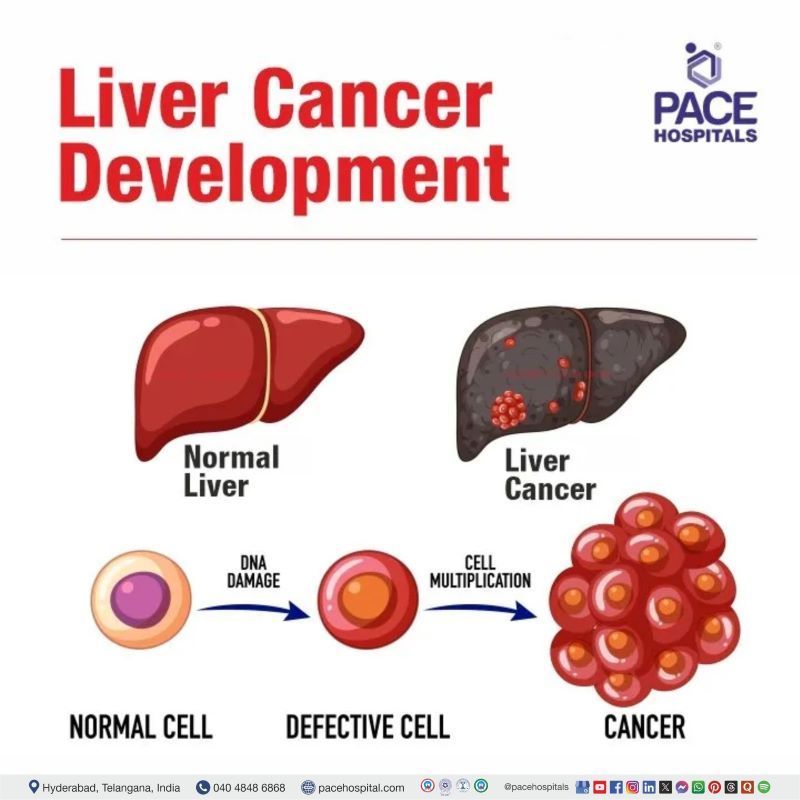
Cancer develops when normally functioning cells undergo mutation and multiply out of control, forming a tumour mass and it can happen in any tissue. When hepatic cells (liver cells) proliferate (increase rapidly in number or multiply) out of control, it is called liver cancer.
Both benign (non-cancerous) and malignant (cancerous) forms of tumours exist. If left untreated, a malignant tumour may quickly develop and metastasize (spread) to other organs. When a tumour is considered benign, it might still grow but will not metastasize.
Hepatocellular carcinoma (HCC) is the most common type of liver cancer and accounts for about 80% of all cases of liver cancer whereas Intrahepatic cholangiocarcinoma (bile duct cancer), Angiosarcoma, Hemangiosarcoma, Hepatoblastoma, Biliary cystadenocarcinoma and Undifferentiated embryonal sarcoma of the liver (UESL) are much less common or rare kind of liver cancer.
What is Liver and its Functions?
The liver is one of the important and largest parts of the body. It located towards the upper right-hand portion of the abdominal cavity.
At any one time, nearly 1 pint of blood (13% of total volume) is stored in the liver at any time. There are many functions of liver are found, few of them include:
- Bile production – necessary for food digestion, especially fats
- Red blood cells apoptosis – The controlled cell death of red blood cells occurs in liver from which bilirubin is emerged. It forms the major part of bile juice.
- Metabolism – of various products such as food, medicines blood etc
- Production of plasma proteins in blood
- Cholesterol production
- Glycogenesis (excess glucose into glycogen for storage)
- Processing of hemoglobin for use of its iron content (the liver stores iron)
- Ornithine cycle (conversion of poisonous ammonia to urea)
- Regulation of blood clotting etc.
Types of Liver Cancer
There are broadly two types of liver cancers - primary and secondary liver cancers.
- Most of the primary liver cancers originate from epithelial tissue of the liver and rarely from the non-epithelial tissue of the liver.
- The secondary cancers include various cancers which originated from other organs such as pancreas, colon, stomach, breast, or lung and metastasized (spread) to liver.
The subtypes of primary and secondary liver cancers include:
Primary liver cancers
| Epithelial cancers | Non-epithelial cancers |
|---|---|
| Hepatocellular carcinoma | Epithelioid haemangioendothelioma |
| Intrahepatic cholangiocarcinoma (peripheral bile duct carcinoma) | Angiosarcoma |
| Adenocarcinoma | Embryonal sarcoma |
| Adenosquamous | Rhabdomyosarcoma |
| Cholangiolocellular carcinoma | |
| Mucinous carcinoma | |
| Signet-ring cell carcinoma | |
| Sarcomatous intrahepatic cholangiocarcinoma | |
| Lymphoepithelioma-like carcinoma | |
| Clear cell variant intrahepatic cholangiocarcinoma | |
| Mucoepidemoid carcinoma | |
| Bile duct cystadenocarcinoma | |
| Combined hepatocellular & cholangiocarcinoma | |
| Hepatoblastoma | |
| Undifferentiated carcinoma |
Secondary liver cancers
Metastasized cancers from other organs, such as:
- Pancreas
- Colon
- Stomach
- Breast
- Lung
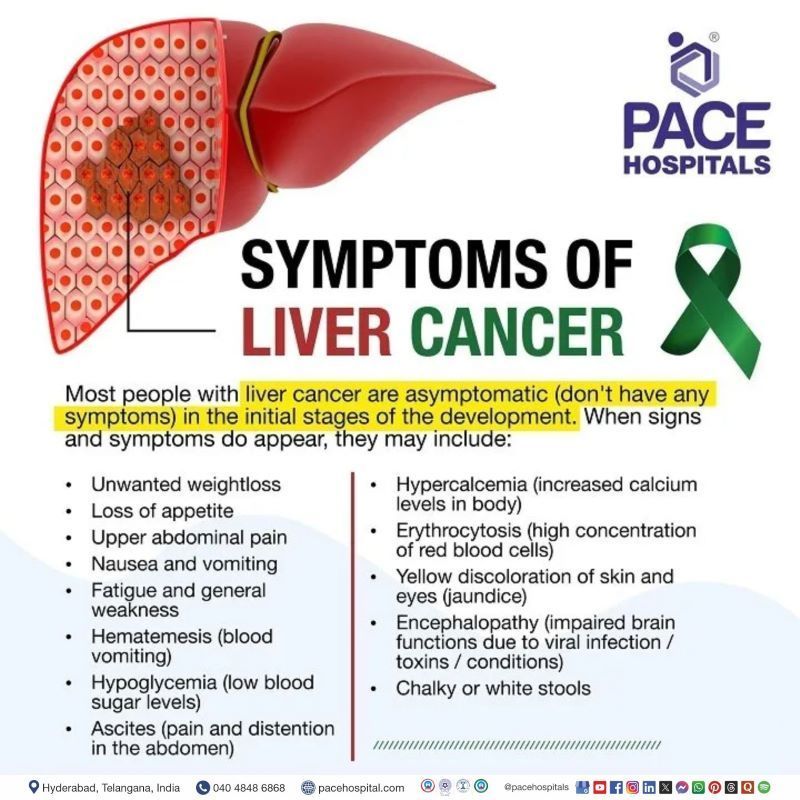
Liver Cancer Symptoms
Most people with liver cancer are asymptomatic (don't have any symptoms) in the initial stages of the development, but those who have had it for a while may start to notice them as a result of the liver illness it causes. Patients show early signs and symptoms, which could include:
- Unwanted weight loss
- Loss of appetite
- Upper abdominal pain
- Nausea and vomiting
- Fatigue and general weakness
- Hematemesis (blood vomiting)
- Hypoglycemia (low blood sugar levels)
- Ascites (pain and distention in the abdomen)
- Hypercalcemia (increased calcium levels in body)
- Erythrocytosis (high concentration of red blood cells)
- Yellow discoloration of skin and eyes (jaundice)
- Encephalopathy (impaired brain functions due to viral infection / toxins / conditions)
- Chalky or white stools
Liver Cancer Causes
Although the risk factors have been clearly elucidated, there isn’t much luck about the causes of liver cancer, but the multifactorial pathways have been established.
Liver cirrhosis can contribute to the progression of liver cancer. Liver cirrhosis is can be caused by various components such as:
- Necrosis (hepatic cell death)
- Fibrosis (accumulation of proteins due to repetitive/long-lasting injury or inflammation)
- Ongoing regeneration (continuous regeneration of liver cells, even when unnecessary)
In some cases, especially in Hepatitis B patients, liver fibrosis can trigger superfluous regeneration in the liver which can incite the development of liver cancer, even without the development of cirrhosis. This is called non-cirrhotic pathway of liver cancer.
Although Hepatitis C causes liver cancer through the context of cirrhosis, Hepatitis B on the other hand, can incite cancer as the viral DNA is integrated into the host creating the HBV X protein, which promotes cell proliferation (eventually causing cancer).
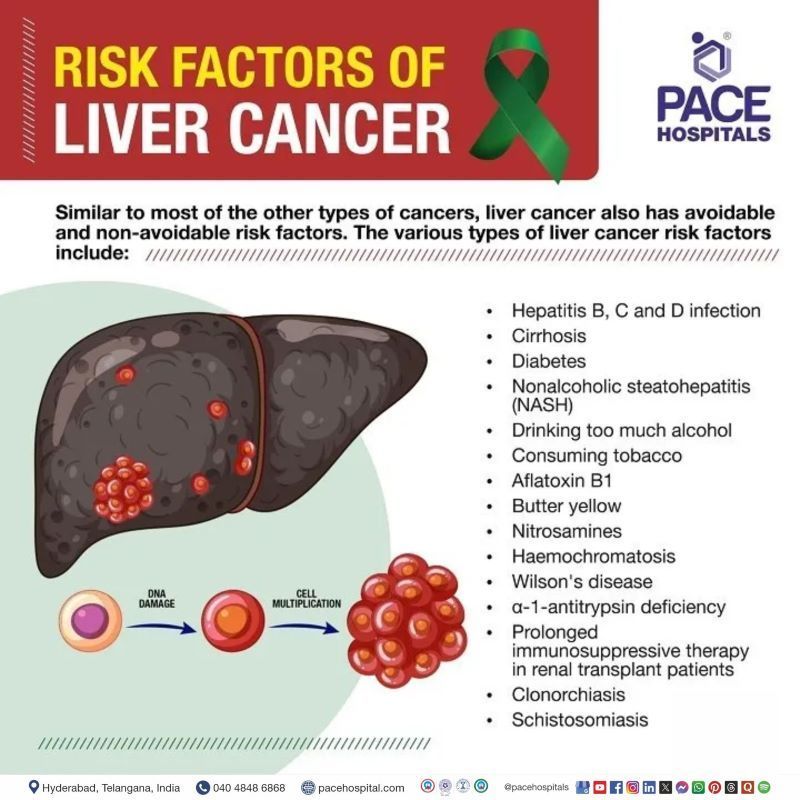
Liver Cancer Risk Factors
Similar to most of the other types of cancers, liver cancer also has avoidable and non-avoidable risk factors. The various types of liver cancer risk factors include:
- Hepatitis B, C and D infection
- Cirrhosis
- Diabetes
- Nonalcoholic steatohepatitis (NASH)
- Drinking too much alcohol
- Consuming tobacco
- Aflatoxin B1
- Butter yellow
- Nitrosamines
- Haemochromatosis
- Wilson's disease
- α-1-antitrypsin deficiency
- Prolonged immunosuppressive therapy in renal transplant patients
- Clonorchiasis
- Schistosomiasis
Viral hepatitis infections
Hepatitis B virus (HBV): One of the most common chronic infections worldwide, with high mortality. The geographical incidence patterns of liver cancer mostly follow that of HBV. The highest rates of HBV are seen in sub-Saharan Africa and East Asia. Around 2% of the Middle Eastern and the Indian subcontinent are infected with HBV.
Through contact with blood or body fluids during sexual intercourse the viral spread is done which induces mutation in the hepatocytes of the host thus paving the path for liver cancer.
Hepatitis C virus (HCV): With 14 crores of infections worldwide, around 3,50,000–5,00,000 patients die of HCV or HVC induced liver cancer. Transmission can be limited with improved hygiene standards as it spreads from parenteral routes, invasive sexual practices. It is rarely transmitted from mother to child. The mechanisms underlying HCV-associated carcinogenesis include:
- increased hepatocyte proliferation and steatosis (fat accumulation in liver)
- virus-induced inflammation and oxidative stress inducing mutations
- effects of virus-induced host immune responses.
Hepatitis Delta virus (HDV): A satellite virus which depends on HBV for generation and propagation. HDV demonstrated pronounced inflammation and severe liver disease than HBV, accelerating the prognosis of fibrosis and cirrhosis and finally to liver cancer.
Chronic liver disease
Cirrhosis: Although there are cirrhotic and non-cirrhotic pathways of liver cancer, cirrhosis; especially macronodular post-necrotic cirrhosis, is the most prevalent cause of the cancer. About 60% of cirrhotic patients develop liver cell dysplasia (precancerous stage) characterised by:
- cellular expansion (increased cell number due to cell growth and cell division.)
- nuclear hyperchromatism (excess chromatin/nuclear material)
- multinucleate cells (cells with many nuclei)
Nonalcoholic steatohepatitis (NASH): The liver scarring and eventual cancer that may result from NASH which is the most severe form of nonalcoholic fatty liver disease (excess fat build-up in the liver). An inflammatory response and damage to liver cells may result in certain persons.
Diabetes mellitus
People specially with type-2 diabetes are at greater risk of developing nonalcoholic fatty liver disease (NAFLD) and chronic liver disease (CLD) further that can lead to liver cancer.
Habits
Alcoholism: About four-fold increased risk of liver cancer could be seen with in alcoholics when compared with teetotallers. It could act as a co-carcinogen in patients suffering with HBV or HCV.
Tobacco use: A higher risk of liver cancer can be linked to cigarette smoking. The number of pack years is directly proportional to the risk.
Mycotoxins
Mycotoxins are naturally occurring poisons generated by a wide variety of moulds (fungi). Many foods, especially cereals, dried fruits, nuts, and spices, are susceptible for mycotoxins growth. Mycotoxins are chemically stable and may thus remain in foods even after preparation.
Aflatoxins: the most poisonous mycotoxins - produced by Aspergillus flavus and Aspergillus parasiticus. Apart from the milk of animals that are fed contaminated feed, aflatoxin can also be seen in:
- cereals (corn, sorghum, wheat and rice)
- oil seeds (soybean, peanut, sunflower and cotton seeds)
- spices (chili peppers, black pepper, coriander, turmeric and ginger)
- tree nuts (pistachio, almond, walnut, coconut and Brazil nut)
- Acute poisoning (aflatoxicosis) caused by high levels exposure to aflatoxins can cause liver. Its carcinogenic effect, can induce DNA damage inciting liver cancer.
Fumonisins: Produced by Fusarium fungus, fumonisins it can grow in oats and maize. Studies have linked fumonisins to oesophageal cancer and suspicions for liver cancer
Chemical carcinogens
A number of chemical carcinogens can induce liver cancer in experimental animals. These include butter-yellow and nitrosamines used as common food additives.
Butter yellow: Butter yellow is a food dye when used in long term causes bile duct dilatation and hyperplasia (increased cell number) in adjacent hepatocytes.
Nitrosamines: chemicals produced by the reaction of nitrites and secondary amines used as food preservatives can cause liver cancers among various others.
Arsenic: In few geographical places, drinking water can contain arsenic naturally. Arsenic is also a part of vinyl chloride, used for certain plastics that can increase risk for liver cancer.
Inherited liver diseases
Haemochromatosis: a hereditary disorder of iron salts being deposited in the tissues, leading to liver damage, diabetes mellitus, bronze discoloration of the skin and finally liver cancer.
Wilson's disease (hepatolenticular degeneration): a hereditary (ATP7B gene) disorder of copper being deposited in the tissues of liver, brain and other vital organs, leading to liver and organ damage finally liver cancer.
Various other medical conditions
α-1-antitrypsin deficiency: an inherited condition in which α-1-antitrypsin that protects the lungs produced by the liver is not produced. This leads to lung and liver cancer.
Clonorchiasis: infection with the liver fluke Clonorchis sinensis usually due to undercooked freshwater fish.
Schistosomiasis (also called bilharzia): a disease caused by parasitic worms.
Prolonged immunosuppressive therapy in renal transplant patients: can also increase liver cancer risk
Excessive intake of male hormones or anabolic steroids: These hormones, for building muscle, are a risk factor.
Liver Cancer Degeneration Stages
Before the development of liver cancer can be understood, the usual degeneration stages of liver must be understood.
Stage 1: Liver Inflammation: Swollen or inflamed liver as a natural response to injury. Nevertheless, the liver is able to repair itself.
Stage 2: Liver Fibrosis: Liver scarring due to untreated inflammation, disrupting its functions. Once hepatocytes (liver cells) are replaced by scar tissue, the liver can’t be able to repair itself. External supplantation / medicines are necessary.
Stage 3: Cirrhosis: Severe, irreversible scarring of the liver which can take several years to decades. Liver cirrhotic people are also more susceptible to developing liver cancer.
Stage 4: Liver Failure: Cease of hepatic function. Liver can’t be repaired by itself or even with medicines. Liver transplant is the only option for recovery.
Complications of Liver cancer
Liver cancer results in several complications as liver is the source of metabolism, enzyme activation, the storage of minerals and glucose, etc. Any abnormality in the liver leads to altered functions. Liver cancer may be caused by tumour pressure on the bile duct or other organs, hormones released by cancer cells, and liver malfunction resulting in a build-up of toxins in the body. Common complications of liver cancer, include: ·
- Anaemia (lack of healthy red blood cells)
- Obstruction of bile duct
- Increase in portal blood pressure (portal hypertension)
- Hypercalcemia (high blood calcium)
- Hepatorenal Syndrome (occurrence of kidney disease due to the presence of liver disease)
- Hepatic Encephalopathy
Liver Cancer Diagnosis
Based on the symptoms, liver specialist doctor might suggest the series of blood test and imaging tests to identify the stage of liver cancer, that include:
- Physical examination
- Blood tests
- Ultrasonography
- Computed tomography (CT or CAT) scan
- Magnetic resonance imaging (MRI)
- Angiogram
- Liver Biopsy
- Biomarker testing of the tumour (also called as tumour molecular testing)
Liver Cancer Treatment
The various liver cancer treatment options include according to stage:
- Surgery
- Radiofrequency ablation (RFA)
- Percutaneous ethanol injection
- Radiation therapy
- Chemoembolization
- Radioembolization
- Targeted therapy
- Immunotherapy
- Palliative care
Treatment according to liver cancer stage
Early liver cancer
- Surgical Resection (Partial Hepatectomy)
- Adjuvant Therapy after Surgical Resection
- Liver Transplantation
- Locoregional Therapy
Intermediate stage
- Transarterial embolization
- Radioembolization
Advanced stage
- Systemic Therapy
Why Choose PACE Hospitals?
Expert Super Specialist Doctors
Advanced Diagnostics & Treatment
Affordable & Transparent Care
24x7 Emergency & ICU Support
Liver Cancer Prevention
There are few established steps to know about how to prevent liver cancer? Various variables contribute to the development of cancer. Despite the fact that there is currently no perfect and proven method of preventing liver cancer, various steps have been elucidated by the researchers which can reduce the chances of its development, these include:
- Viral hepatitis prevention and vaccination: liver cancer can be prevented if viral hepatitis C can be prevented. A vaccine can protect healthy people from contracting hepatitis B. Blood must be tested before transfusion to avoid any contamination.
- Cirrhosis treatment: it can be avoided by prompt treatment of the liver injury.
- Avoiding alcohol and tobacco consumption: Even liver injury can be avoided by abstinence from alcoholism and tobacco.
- Maintain a healthy weight: Obesity prevention could be an additional line of defense against liver cancer. Fatty liver disease and diabetes are both risk factors for liver cancer, and both are more common in obese people.
- Limit exposure to cancer-causing chemicals: Changing the way certain grains are stored in tropical and subtropical countries could reduce exposure to cancer-causing substances such as aflatoxins. Many developed countries already have regulations to prevent and monitor grain contamination.
Frequently Asked Questions (FAQs) on Liver cancer
Is liver cancer curable?
Liver cancer is often treatable, but sometimes it can be difficult to treat. The treatment depends on:
- The origin of cancer (primary or secondary)
- The size of liver cancer
- The type of liver cancer you have
- The location of liver cancer
- The metastasis (spread) of liver cancer
- The general health of patient
- The multimodal treatment could include surgery, chemotherapy, thermal ablation, using targeted therapy, and radiotherapy.
What is the best treatment for liver cancer?
Liver transplantation has been shown to be the most effective treatment option for patients diagnosed with hepatocellular carcinoma, the most common form of liver cancer. If a patient has a condition of the liver, such as cirrhosis, liver transplantation may reduce the risk of the illness coming back after treatment has been administered.
What are the symptoms of liver cancer?
Liver cancer could be asymptomatic particularly if the tumour is detected early. In patients where the symptoms are seen, the commonly expressed symptoms are right upper abdominal pain, weight loss, fatigue, weakness, and jaundice.
How to detect liver cancer early?
It is often hard to find liver cancer early because signs and symptoms often do not appear until it is in its later stages.
As the right rib cage covers the majority of the liver, it might be difficult to identify even relatively small tumours in the liver during a physical examination. When a tumour finally becomes noticeable, it may have already reached a considerable size.
Constant vigilance over the risk factors of liver cancer is the recommended solution. Cancer screening for people susceptible to liver cancer also helps.
Can you survive cancer that has spread to the liver?
If the cancer has metastasised (spread) to the liver, it is almost never possible to treat it successfully. When cancer has progressed to the point that it has spread to the liver, the patient almost always succumbs to the illness. On the other hand, medicines have the potential to reduce the size of tumours, increase life expectancy, and alleviate symptoms.
Is liver cancer curable if caught early?
If detected at an early stage of liver cancer, cancer may sometimes be surgically removed in its whole. The treatment options for liver cancer are dependent on the stage of the ailment. Options for treating liver cancer in its earlier stages include:
- Hepatic resection - procedure in which a piece of the liver is surgically removed.
- Liver transplant - the damaged liver is replaced with a donor's healthy liver.
- Microwave or radiofrequency ablation – micro or radio waves to destroy the cancer.
Can liver cancer be cured with chemotherapy?
Yes, Chemotherapy combined with surgery can be administered in the early stages of liver cancer to cure it. Chemotherapy can also be prescribed in few patients in whom surgery or other loco regional therapies are impossible, citing various reasons. Local therapies include ablation, embolization etc. The various drug classes which can be included for chemotherapeutic administration include:
- Antimetabolites
- Alkylating agents
- Platinum-containing compounds.
- Anthracyclines
- Anthracenediones
Can ultrasound detect liver cancer?
Yes. Ultrasound is often the first test to be prescribed when the suspicion of liver cancer arises. The scanning of ultrasound results in the production of a picture on a computer screen via the of sound waves. This test may reveal the presence of tumours forming in the liver, which can subsequently be examined for signs of cancer if that becomes necessary.
Ultrasound is one of many other imaging tests. The other imaging tests include:
- Computed tomography (CT) scan
- Magnetic resonance imaging (MRI) scan
- Angiography
- Bone scan
How accurate is ultrasound for liver cancer?
Ultrasonography is one of the most accurate imaging tests for hepatocellular carcinoma (liver cancer) as it provides inexpensive, real-time, and non-invasive detection. Recent developments in ultrasonography technology provide additional information about liver cancer and the localisation of diagnosis. Research demonstrated the accuracy of ultrasound to be at:
- 84.4% for benign liver cancer
- 87.7% for malignant liver cancer
- 85.7% for metastatic liver cancer
How effective is immunotherapy for liver cancer?
Immunotherapy is very effective for the management of liver cancer, which boosts immune cells for the elimination of liver cancer. There are several forms of immunotherapy, which include:
- Cancer vaccines
- Checkpoint inhibitors
- Oncolytic or tumour-infecting viruses
- Targeted antibodies
- Adjuvants
- Cytokines
Three main reasons for choosing immunotherapy for the treatment of liver cancer are:
- Immunotherapy has been effective for several cancer types. Immunotherapy works when radiation or chemotherapy aren't enough for certain tumours.
- Chemotherapy or radiation combined with immunotherapy effectively treats cancer.
- Immunotherapy addresses the immune system, not cells. Immunotherapy is less toxic than other cancer therapies.
What is the survival rate after immunotherapy?
The percentage of cancer patients who see a response to immunotherapy medication typically falls around between 20-50%. The response rate is reliant on the particular kind of cancer that is being treated. Oncologists, however, are of the opinion that long responses may become more common as with the constant improvement of immunotherapy research as researchers acquire new insights into the ways in which the immune system and cancer cells interact with one another.
When to consult a doctor for liver cancer?
Consult a doctor for liver cancer when abdominal pain, unexplained weight loss, or yellowing of the skin and eyes (jaundice) persist. Early diagnosis is essential as liver cancer often shows late symptoms.
Warning signs include:
- Upper abdominal pain or swelling
- Loss of appetite or sudden weight loss
- Nausea or vomiting
- Yellowing of skin and eyes
- Ongoing fatigue
A liver cancer specialist, hepatologist or oncologist can diagnose the condition and recommend suitable liver cancer treatment, including surgery or other medical options.
Share on
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868