Best Hospital for Pancreatitis Treatment in Hyderabad, Acute & Chronic
Our team of the best pancreas specialist doctors in India are expert in treating acute pancreatitis, chronic pancreatitis, hereditary pancreatitis and its complications such as-
- Malnutrition, due to lack of digestive enzymes
- Pancreas infection
- Kidney problem / failure
- Pancreatic cancer
- Necrotizing pancreatitis
- Pancreatic pseudocyst
- Lungs problem such as difficult in breathing
Book an Appointment for Pancreatitis Treatment
Pancreatitis Appointment Enquiry
We are one of the advanced pancreatitis and pancreatic cancer treatment hospital in Hyderabad backed up with team of best pancreatologist, pancreas specialist doctors, internationally renowned team of medical and surgical gastroenterologists, transplant surgeons, and paramedical staff, psychologist and physiotherapist in India.
We are equipped with “The World’s First Universal Surgical Robotic System”, State-of-the-art facility and latest technology offering comprehensive treatment for acute pancreatitis, chronic pancreatitis, hereditary pancreatitis, Pancreatic cancer and its complications.

Our Pancreatology department is equipped with high end diagnostic endoscopy and colonoscopy equipment, Endoscopic ultrasound, Endoscopic retrograde cholangiopancreatography (ERCP), Capsule endoscopy, Balloon-assisted enteroscopy, 24 hour esophageal pH metry, Latest imaging and radiology services offering diagnosis of pancreatitis and its severe malignancy like Pancreas infection, Pancreatic cancer, Necrotizing pancreatitis and Pancreatic pseudocyst.
Our team of pancreas specialist doctors are experts in doing interventional medical and surgical procedures like EUS-guided gallbladder drainage, Endoscopic Retrograde Cholangiopancreatography (ERCP), Sphincterotomy for pseudocyst drainage, Balloon dilatation, Pancreatic or bile duct stent placement, Laparoscopic cholecystectomy, Distal pancreatectomy, Pancreaticoduodenectomy (whipple procedure), and Total pancreatectomy.
What are the types of pancreatitis?
Pancreatitis may be a mild, short-term condition and self-limiting, or can cause severe, life-threatening complications that can remain for many years. There are a different type of conditions related to the pancreas including acute pancreatitis, chronic pancreatitis, hereditary pancreatitis and Pancreatic cancer.
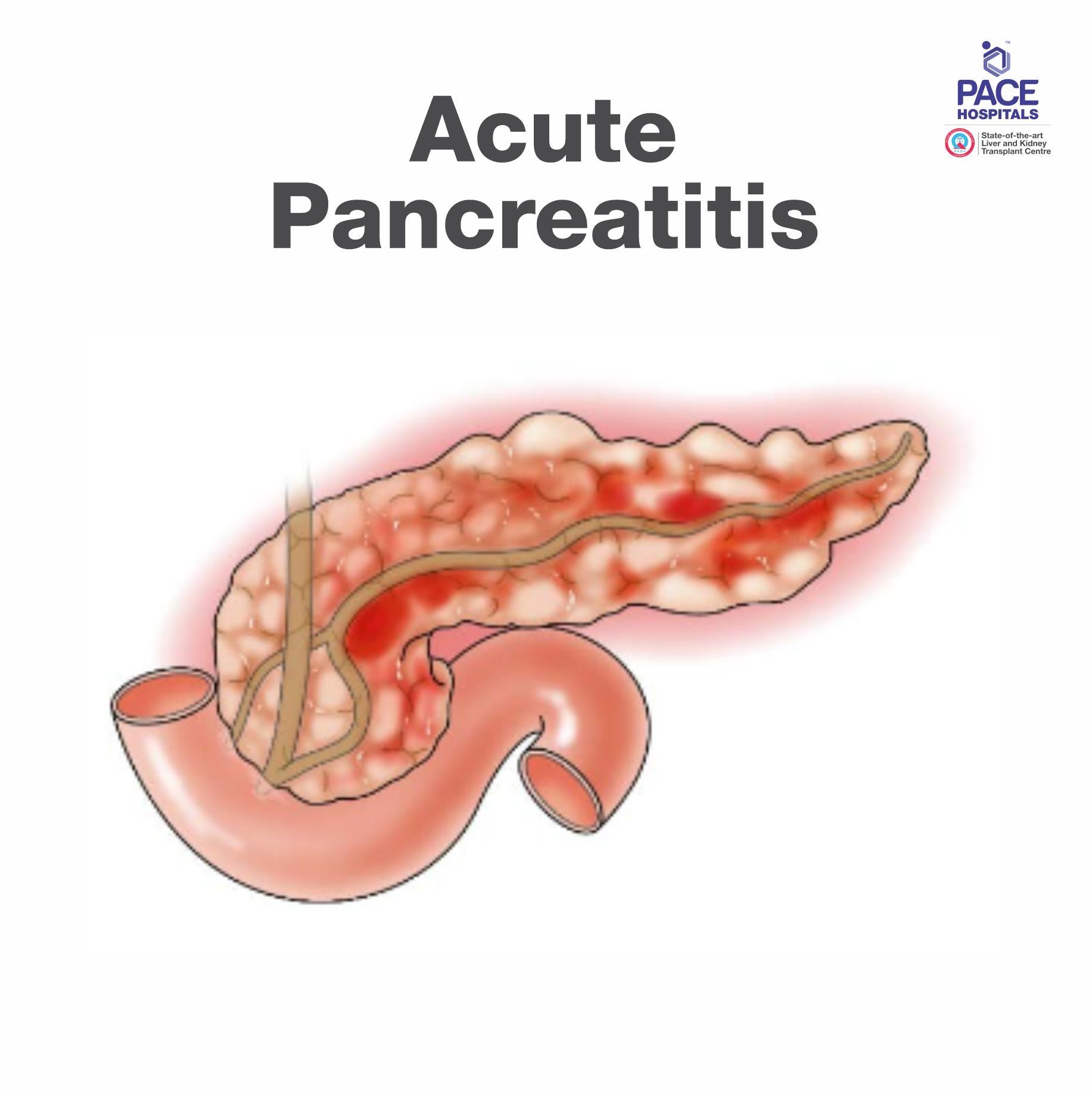
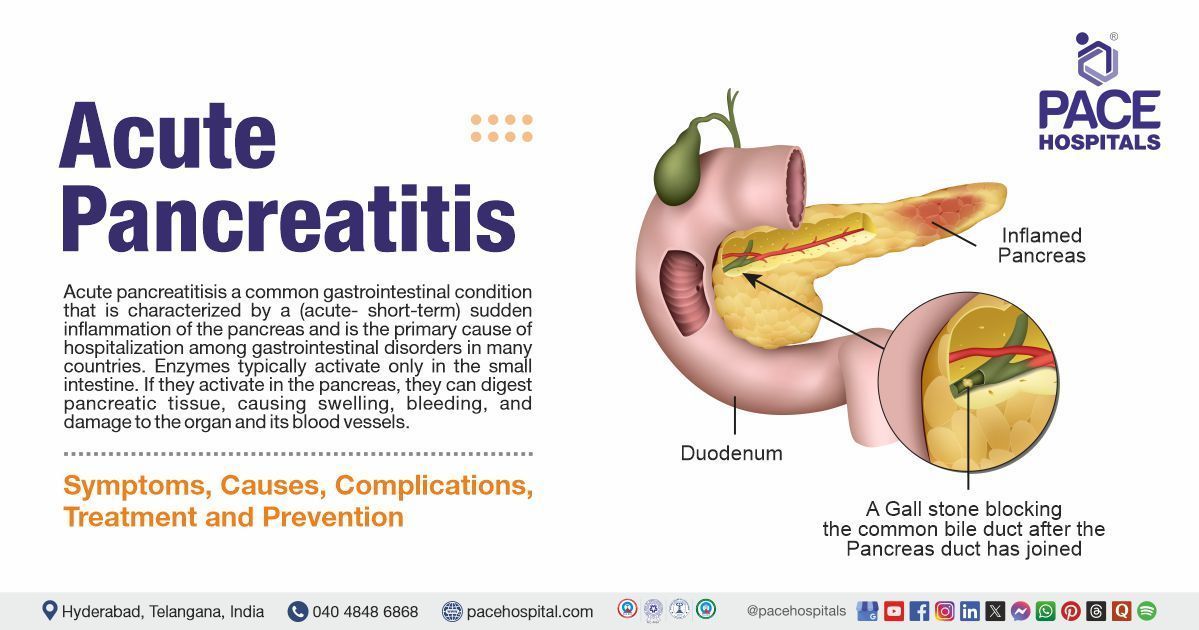
What is Acute Pancreatitis?
Acute pancreatitis is a short term condition and occurs suddenly; causing inflammation of the pancreas. Acute pancreatitis may be mild and can develop further complications if not treated and monitored properly, such as necrotizing pancreatitis, pancreas infection, pancreatic pseudocyst, or organ failure.
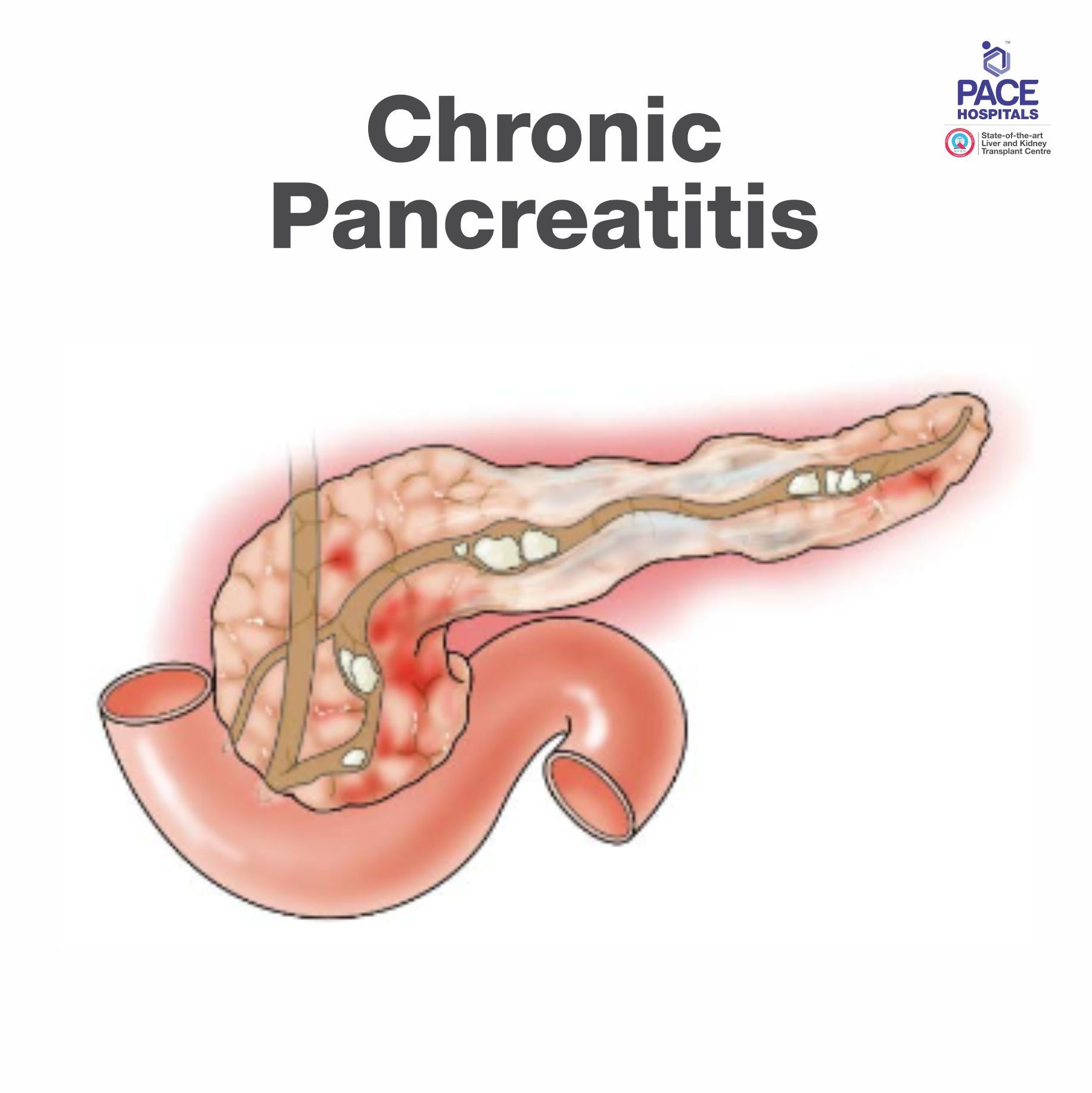
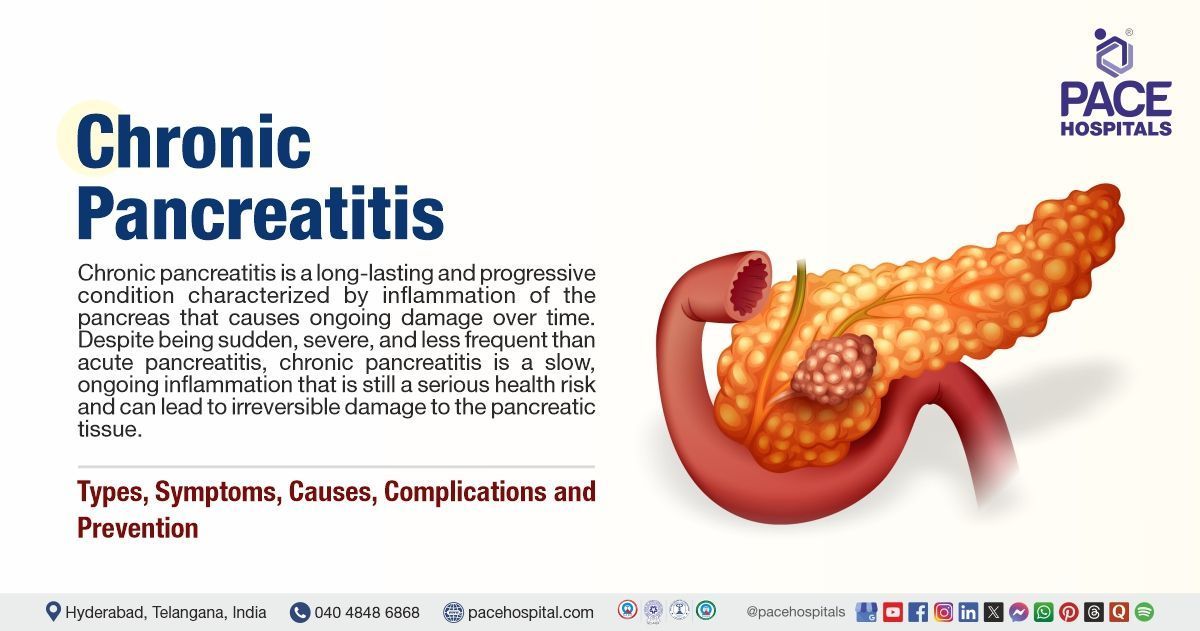
What is Chronic Pancreatitis?
Chronic pancreatitis is long-term progressive disease, causing inflammation and permanent damage of the pancreas. It is a progressive disorder associated with the damaging the tissues of the pancreas that can't be reversed. It is more common in male aged between 32 to 45 years.
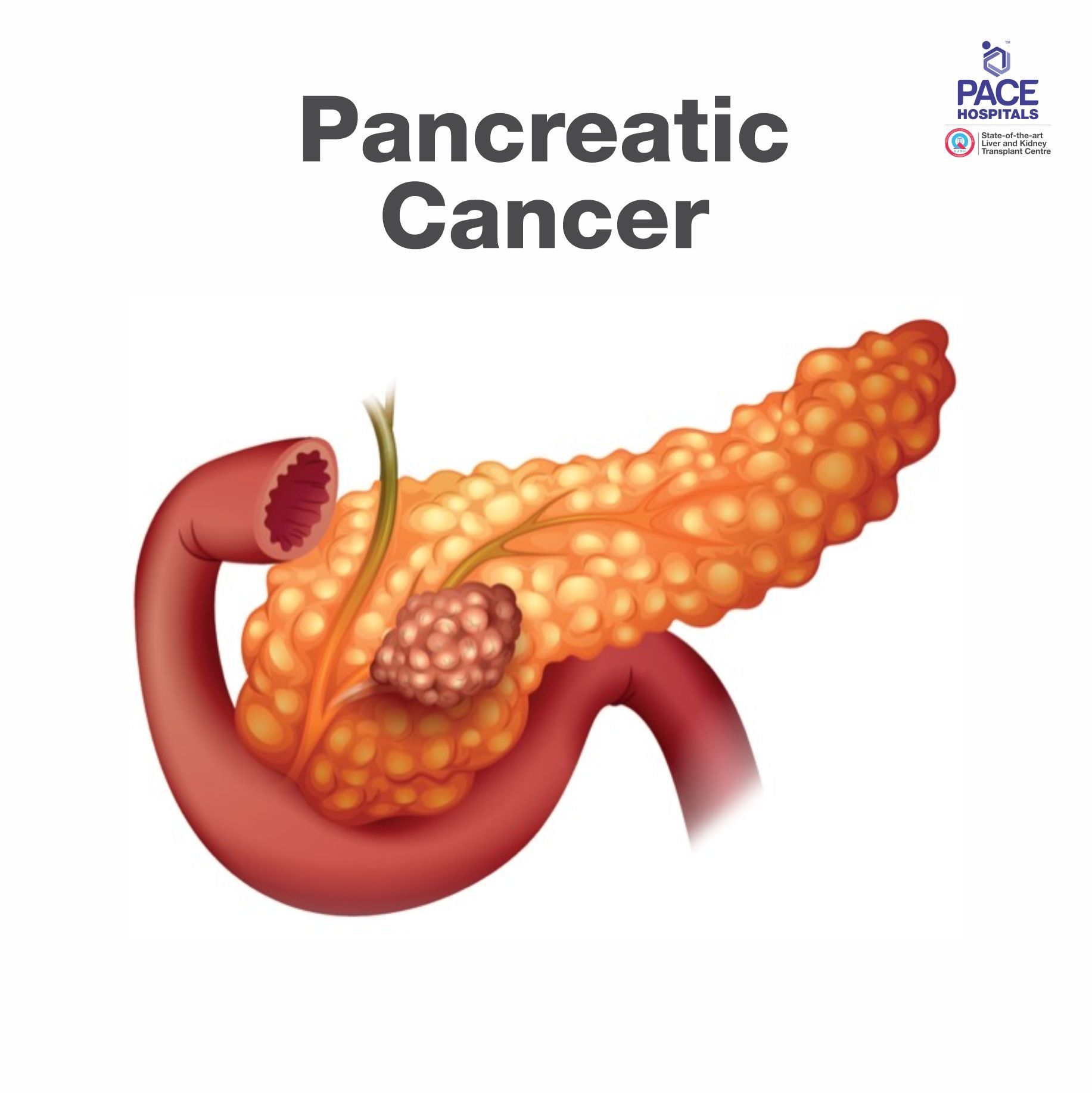
What is Pancreatic Cancer?
Pancreatic cancer occur when uncontrolled cell growth begins in the tissues of the pancreas. Cancerous and noncancerous tumors growths can occur in the pancreas. Pancreatic cancer can be cured if detected early but in most of the cases due to no symptoms is early stages it’s difficult to find it.
Patient Testimonial: Young lady presented with history of recurrent abdominal pain. On evaluation, she was found to have changes of chronic pancreatitis with dilated pancreatic duct and multiple pancreatic ductal stones along with parenchymal calcification.
Frequently Asked Questions on Acute Pancreatitis and Chronic Pancreatitis
Can pancreatitis be cured?
Of course, pancreatitis can be cured. The first approach would be to take out the inciting cause like if patient is consuming alcohol or patient has gallstones or has high calcium or high triglycerides leading to pancreatitis. The inciting factor should be cleared and that cures the pancreas like gallstones are there, they should be removed by surgery. Alcohol intake should be stopped and increase calcium if it's due to parathyroid hormone. That can also be cured by surgery, low cholesterol and triglyceride levels should be corrected by stopping alcohol, adjusting the diet and some medication. Likewise, there's in patients with recurrent acute pancreatitis we do use some medicines which have a role like pancreatic enzyme supplements and large doses of antioxidants supposed to reduce the attacks of pancreatitis.
Of course, in patients who are having continued attacks of pancreatitis despite medical therapy, we have the options of endoscope endo therapy like endoscopic sphincterotomy, endoscopic stenting, endoscopic stone removal, and endoscopic stricture dilation. In patients who don't respond even to these, surgery is frequently done option with very high success rates, around 90 to 95%. In patients with acute pancreatitis when the pancreas becomes necrosed and becomes infected, we perform minimally invasive necrosectomy, laparoscopic necrosectomy to clear the infection and cure the patient. While in chronic pancreatitis when the pancreas becomes much scarred with multiple obstructions and lot of stones, we can do surgery like pancreaticojejunostomy in which the all the blocks in the pancreas, all the block ducts are cleared and all the stones are cleared. By this we can permanently cure the pain that is caused by pancreatitis.
What Is the cost of Pancreatitis Treatment at PACE Hospitals, Hyderabad?
At PACE Hospitals, Hyderabad, the cost of pancreatitis treatment typically ranges from ₹1,000 to ₹1,25,000 and above (approx. US $12 – US $1,500), making it an affordable and advanced option for complete pancreatic care. However, the final cost depends on:
- Type of pancreatitis (acute vs. chronic)
- Severity of inflammation and complications
- Need for CT, MRI, EUS, or MRCP
- Requirement for ICU care
- Need for ERCP or interventional drainage
- Duration of hospitalization
- Pancreatic enzyme therapy & long-term medications
- Nutritional support and follow-up monitoring
Mild acute pancreatitis managed with IV fluids and observation falls in the lower range, while severe pancreatitis requiring ICU care, ERCP, or drainage procedures falls toward the higher range.
After consultation, imaging, and specialist evaluation, our pancreatology team provides a personalised treatment plan and a transparent cost estimate based on your condition.
What is the best treatment for acute pancreatitis?
The best treatment for acute pancreatitis depends on the phase of illness, and so in the inflammatory phase, which is in the first two weeks of illness, the best treatment is the best supportive care. Especially patients with severe pancreatitis should get yourself admitted in a gastroenterology specialty hospital where the ICU and the doctors are equipped with routinely taking after pancreatitis patients. It mainly involves nutritional support, maintaining hydration, giving good supportive care, maintaining blood pressure, the renal function, the lung function and also very importantly maintaining the nutrition. After the second week when you have the infective phase when the pancreatic neck gets necrosed and then you have the infective complications, the best state-of-the-art treatment is of course minimally invasive procedures. It could be endoscopic necrosectomy, or minimally invasive laparoscopic, or retroperitoneal necrosectomy, which is the best possible way to deal with this infective phase.
How to prevent pancreatitis?
Pancreatitis can be prevented mostly by lifestyle choices. Not all the causes of pancreatitis, but some cause of pancreatitis can be prevented by lifestyle choices. Obviously, alcohol intake is the commonest cause of both acute and chronic pancreatitis, so we should completely stop consuming alcohol. Obesity is another risk factor for pancreatitis, once you have pancreatitis if you're obese, your pancreas tends to be much more severe and more life-threatening, that's why obesity should be controlled.
Sedentary lifestyle increase the risk of formation of gallstones and increase obesity. So an active lifestyle helps you prevent pancreatitis. Unnecessary uses of the certain drugs like, steroids, azathioprine etc. should be avoided, and you should always take it under physician supervision. Patients with gallstones if they have symptomatic gallstones they should get them treated laparoscopically because that's the simplest way, you just remove the gallstones you'll never have an attack of gallstones pancreatitis. However, if you have gallstones, if you're symptomatic, don't waste your time using some alternate medicines in the hope that gallstones will be dissolved, because if in the meanwhile you get a gallstone pancreas pancreatitis, it could be pretty life-threatening.
What is the best treatment for chronic pancreatitis?
The best treatment for chronic pancreatitis obviously depends on the type of disease you have, and a patient has a single structure in the pancreas or a single stone in the head and that kind of pretty simple disease. Endo therapy is a good option, so endo therapy ERCP combined with stenting and sometimes extracorporeal shockwave lithotripsy (ESWL) to break the stone. These are ideal for patients with simple disease like a single dominant stricture in the head of the pancreas with a single large stone.
However, for patients with multiple structures of the pancreas, most of the time they have multiple structures with multiple stones and extensive scarring. These kinds of patients, they are dealt better by surgery. The surgery, depending on the kind of disease they have, if they have focal pancreatitis, we do pancreatic resections such as a pancreatic head resection or a distal pancreatectomy, depending on the focus of the disease or patients who have diffused disease throughout the pancreas - the tail, head and body. Those kinds of patients we do drainage procedures like phrase pancreaticojejunostomy. Both surgery and resection surgery and phrase pancreaticojejunostomy. If we choose the patients well and if they're done by an expert, the treatment success rate is as high as 85 to 90%.
Why is PACE Hospitals is known as the best hospital for pancreatitis treatment in Hyderabad, India?
PACE Hospitals is regarded as the best hospital for pancreatitis treatment in Hyderabad, offering advanced care for patients with acute pancreatitis and chronic pancreatitis. Our experienced gastroenterologists and pancreatic specialists provide accurate diagnosis, timely intervention, and personalized pancreatitis treatment plans to reduce inflammation and prevent complications. As the best pancreatic hospital in Hyderabad, we use cutting-edge imaging, minimally invasive procedures, and evidence-based therapies to ensure effective recovery and long-term digestive health. With a patient-focused approach and round-the-clock medical support, PACE Hospitals delivers comprehensive care for all forms of pancreatitis.
How long does pancreatitis take to heal?
The patient with pancreas. How long does it take to recover, it depends basically on whether it's acute pancreatitis or chronic pancreatitis. In acute pancreatitis, how long the patient recovers depends on the severity of pancreatitis. In a mild and moderate pancreatitis usually in the absence of any pancreatic necrosis within a couple of weeks (7 days to 14 days) pancreatitis resolves and the patient settles down.
On the other hand, severe pancreatitis is a very serious illness with the mortality of about 20 to 30% in this case 1 out of 3 (one out of three) patients may die, and the patients who survive has a very prolonged course. There's an early inflammatory phase in which the patient has several issues related to pancreatic inflammation like breathing difficulties, kidney failure, or BP going down, ICU requirement and after four weeks or so then the necrotic pancreas gets infected and they developed all sorts of infectious complications such as walled off pancreatic necrosis, infected necrosis, pseudo aneurysm and all that. In prolonged phase even if surgery is done, many times patients undergo necrosectomy, and then after that they develop a fistula, and the fistula takes a lot of time to heal. During the entire process they become malnourished that takes a lot of time to recover, so basically. Mild pancreatitis would recover in about 2 weeks or so while severe pancreatitis recovery can take anywhere between one and a half, two months to six months depending on how bad the course was.
On the other hand, chronic pancreatitis, it does not heal. By definition, acute pancreatitis, once the at least especially for mild pancreatitis once the pancreatitis is over, the pancreas comes back to its normal anatomy, while chronic pancreatitis it never heals, because with every attack it progressively keeps on getting scarred and scared when the pancreas does not have the ability to repair itself so the pancreas becomes permanently scarred and there's no healing in the pancreas. In chronic pancreatitis as the attacks progress the pancreas also becomes progressively more and more shrunken, hard, fibrotic, and the pancreatic function also keeps progressively deteriorating.
What is pancreatitis?
The pancreas is a fatty structure located in the posterior aspect of the body, just in front of the spine. Its main functions are production of insulin and digestion of fatty food, inflammation of the pancreas that is swelling of the pancreas is called pancreatitis. There are two forms of pancreatitis - acute pancreatitis and chronic pancreatitis. Acute pancreatitis, a sudden onset inflammation, secondary to usually alcohol gallbladder stones, viral fevers and drugs, and all that. In which a previously normal pancreas, suddenly becomes severely inflamed and the patient comes to the hospital in an emergency with severe abdominal pain with breathing difficulty, the blood pressure going down leading onto organ dysfunction.
There's another entity called chronic pancreatitis, in which over a period of time the pancreas becomes very scarred and hard, and the patient presents, usually with repeated episodes of pain for several years. Obviously that is worsening along with diabetes and fatty indigestion with greasy stools.
What is the role of pancreatic enzymes?
The pancreas has mainly two functions, exocrine and endocrine. Endocrine means it produces insulin and glucagon, which are mainly related in the sugar control. In terms of digestion, the pancreas produces several enzymes like trypsin, chymotrypsin, lipase and amylase. For the protein digestion and the carbohydrate digestion we have the intestinal secretions, duodenal secretions and saliva; they all help in protein and carbohydrate digestion.
But for fat digestion especially, the pancreas is the only organ that produces lipase. So pancreas is very critical for fatty food digestion. The patients with pancreatic insufficiency develop fat malabsorption, this leads to a lot of nutritional issues, a lot of deficiencies of fat soluble vitamins such as ADEK, and also causes calcium malabsorption leading to osteoporosis and later on it can lead to liver problems and heart problems.
What causes pancreatitis?
The cause of pancreatitis depends on the type of pancreatitis we look at. So you have acute and chronic pancreatitis. Acute pancreatitis mostly caused by gallstones, and alcohol intake. Together, gallstones and alcohol intake account for 90% of the acute pancreatitis. Other causes are certain drugs like steroids, azathioprine and a lot of other drugs can cause pancreatitis. Calcium abnormalities hypercalcemia, especially secondary to hyperparathyroidism, hypertriglyceridemia increased cholesterol and triglycerides, some congenital anomalies of the pancreas like pancreas divisum, abnormal pancreaticobiliary union, viral fevers like dengue and chikungunya and other viral fevers, even COVID can cause pancreatitis. In addition, there are some genetic mutations which make you more prone to pancreatitis like Spink-1, PRSS-1 CFTR gene mutations.
On the other hand, chronic pancreatitis is mostly one of the common cause’s alcohol intake, and the other causes we have in India is called tropical chronic pancreatitis. Now it's called idiopathic chronic pancreatitis. Basically, in this, more involvement of women than men, unlike normal pancreatitis, which is more in men, and it is actually a very young age by 20 years of age, large stones form in the pancreas becomes very atrophic with the risk of diabetes and cancer. And this we don't know the exact cause for this, but certain genetic mutations and childhood malnutrition are supposed to be involved. Other cause of chronic pancreatitis can be hereditary chronic pancreatitis and sometimes recurrent acute pancreatitis. Multiple attacks of acute pancreatitis of the previously etiologies can lead to chronic pancreatitis.
Is GERD associated with pancreatitis?
No GERD is not associated with pancreatitis. They have some common associations like patients with obesity, patients with alcohol intake, patient with a lot of smoking they can tend to have more incidents of GERD and they tend to have a higher incidence of pancreatitis. So that way the risk factor are associated. But directly GERD does not cause pancreatitis.
Can gallbladder removal cause pancreatitis?
Actually gallstones cause pancreatitis. So removal of the gallbladder is a very good way to prevent recurrent pancreatitis in patients with gallstones. So gallbladder removal does not cause pancreatitis. But if you have had pancreatitis after your gallbladder stone removal, you should get an MRCP done and this will show you if there's any stone from the gallbladder that has slipped into the bile duct which is causing pancreatitis despite your gas stone removal. It will also rule out other causes such as chronic pancreatitis or pancreas divisum and abnormal pancreaticobiliary union which can be associated with pancreatitis.
Does prolonged antacid treatment cause pancreatic adenocarcinoma?
Prolonged antacid treatment has not found to increase the incidence of pancreatic adenocarcinoma. There is no association but prolonged abuse of antacids for unnecessary indications has other deleterious effects on the body. Such as it interacts with cardiac medications and increases the incidence of heart disease. It can affect your kidneys, can increase the incidence of Alzheimer's and those kind of deleterious effects.
Can I smoke after acute pancreatitis treatment?
Smoking is not recommended after acute pancreatitis treatment because patients who had severe acute pancreatitis, they would have chronic pancreatitis. And if you smoke further after that in the setting of chronic pancreatitis, it can have further worsening of the pancreas insufficiency and also lead to pancreatic cancer.
Is ESWL treatment is good for chronic pancreatitis?
ESWL (extracorporeal shockwave lithotripsy) that is used mainly in kidney stones for breaking the stones. ESWL is widely used in chronic pancreatitis but it has very limited load for highly selected patients with a single large stone or a single dominant structure in the head of the pancreas. In these kind of patients usually ESWL cannot be used alone, it has to be combined with ERCP and pancreatic stricture, dilation and pancreatic stenting. So in highly selected patients with a single dominant structure and single large. You can do pancreatic stenting and then break the stones by ESWL for the patients who are fit for ESWL. These kind of patients with large stones in the pancreas, they're better served by surgery for chronic pancreatitis because phrase longitudinal pancreaticojejunostomy and pancreatic drainage procedures tackle the stones permanently and tackle the structures also more thoroughly.
What is a whipple procedure?
The
Whipple procedure or
whipple surgery is the primary treatment for pancreatic cancer, it’s also called as a pancreaticoduodenectomy. In this operation, the surgeon may remove the body of the pancreas, the entire duodenum and a portion of the stomach to treat the pancreatic cancer.
What is the cost of pancreatitis treatment in India?
Pancreatitis treatment depends upon its and stages such as acute pancreatitis and chronic pancreatitis. The cost of pancreatitis treatment in India vary from Rs. 5,25,000 to Rs. 12,00,000 (five lakh twenty-five thousand to twelve lakhs) or more, it depends upon the type, stage, medical conditions of the patients and surgical treatment. However, pancreatitis treatment cost in India may vary depending upon the different hospitals in different cities.
What is the cost of pancreatitis treatment in Hyderabad?
The average cost of pancreatitis treatment in Hyderabad is approximately Rs. 4,50,000 to Rs. 9,50,000 (four lakh fifty thousand to nine lakh fifty thousand) in the case of acute pancreatitis since chronic pancreatitis is irreversible cost may vary depending upon the stage, surgery, medication, hospital stay, follow up and many other factors.
In sort, cost of pancreatitis treatment and its complications can’t be defined due to its stages and severity.
Related Resources
Why choose PACE Hospitals?
- A Multi-Super Speciality Hospital.
- NABH, NABL, NBE & NABH - Nursing Excellence accreditation.
- State-of-the-art Liver and Kidney transplant centre.
- Empanelled with all TPA’s for smooth cashless benefits.
- Centralized HIMS (Hospital Information System).
- Computerized health records available via website.
- Minimum waiting time for Inpatient and Outpatient.
- Round-the-clock guidance from highly qualified medical and surgical gastroenterologists.
- Standardization of ethical medical care.
- 24X7 Outpatient & Inpatient Pharmacy Services.
- State-of-the-art operation theaters.
- Intensive Care Units (Surgical and Medical) with ISO-9001 accreditation.