Pancreatic stones - Causes, Symptoms, Incidence, Complications, Treatment & Prevention
Pace Hospitals
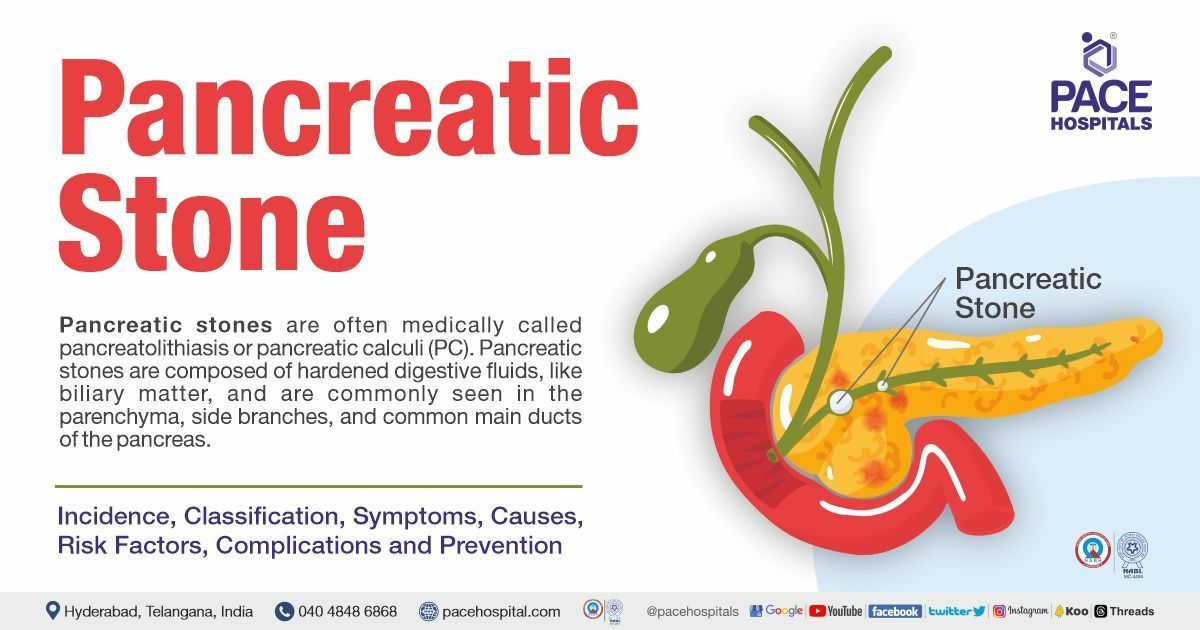
What are pancreatic stones?
Pancreatic stones are often medically called pancreatolithiasis or pancreatic calculi (PC). Pancreatolithiasis is the consequence of chronic pancreatitis and is commonly seen in parenchyma, side branches, and the common main ducts of the pancreas. Calculi are the product, regardless of how chronic pancreatitis originated. Pancreatic calculi have an inner nidus that is encircled by consecutive calcium carbonate layers.
Pancreatic stones are composed of hardened digestive fluids, like biliary matter. Pancreatic calculi, however, are often formed of fragments of calcium carbonate that have solidified out of pancreatic enzymes and become lodged in the duct connecting the pancreas to the small intestine.
Composition of pancreatic stones
Pancreatic stones are composed of a calcium carbonate crystalline lattice embedded within a gel-like matrix comprising multiple fibrillar proteins and polysaccharides.
Incidence of pancreatic stones
Pancreatolithiasis is seen in less than 1% of the general population and is primarily diagnosed in those with chronic pancreatitis. The consequence or complication of chronic pancreatitis, known as pancreatic calculi (PC), can develop in roughly 50% of chronic pancreatitis patients.
Classification of pancreatic calculi
Pancreatic calculi or pancreatic stones are classified based on the type, number of stones and location.
Based on the type, the pancreatic calculi are:
- Radio opaque
- Radiolucent
- Mixed
Based on the number, the pancreatic calculi are:
- Single or
- Multiple
Based on the location, the pancreatic calculi may occur at:
- Main pancreatic duct (MPD)
- Side branches or in the pancreatic parenchyma
- Head, body or tail regions of the pancreas
Symptoms of pancreatic stones
Pancreas stones can cause a variety of symptoms, based on the type, number and location, including:
- Severe abdominal pain in the upper left or middle abdomen, radiates to the back or chest
- Sudden and intense pain may last for several hours or days
- Jaundice (yellowing of the skin and eyes)
- Nausea & vomiting
- Fever & Chills
- Difficulty digesting food
- Unwanted weight loss
- Irregular heartbeat (arrhythmia)
- Dehydration
- Low blood pressure
Stone blockage in the pancreatic duct leads to severe abdominal pain; the pain might be seen in the upper part of the stomach or radiate to the chest or back region. In addition, pancreatic stone results in pancreatitis (inflammation of the pancreas), which induces fever, nausea, chills, vomiting and more.
These symptoms might be constant or intermittent. However, the onset of the occurrence is sudden. Some uncommon symptoms, such as jaundice, light-coloured stools, dark urine, fast breathing (tachypnoea), and rapid heart rate (tachycardia), are seen in occasional cases.
NOTE: If any of the above signs are seen, it's crucial to consult the gastroenterologist as soon as possible. If pancreatic stones are not treated immediately, they can result in serious complications.
It's crucial to remember that not all people with pancreatic stones will exhibit the above symptoms. In certain circumstances, imaging examinations for other medical issues may unintentionally discover pancreatic stones.
Pancreatic stones causes
The exact cause of pancreas stones is not clearly understood, but they are contemplated to form when substances in pancreatic juice such as calcium carbonate, protein, bilirubin solidify.
Pancreas stones are more commonly found in people who have:
- A history of gallstones (cholelithiasis)
- Chronic pancreatitis
- High levels of triglycerides or calcium in the blood
- Certain genetic disorders or inherited diseases
Most pancreatic stones are due to gallstones; the gallstones travel from the gall bladder to the common biliary duct and cause obstruction in the biliary duct, thus resulting in gall stone pancreatitis and stone formation. The blockage of the common bile duct results in the backup of bile into the pancreatic duct, resulting in stone formation.
The causes of pancreatic stones are as follows:
- The high levels of calcium deposition in the pancreatic duct as a result of calcium carbonate fragments that have solidified from pancreatic enzymes result in the formation of pancreatic stones. Also, high calcium levels due to hyperparathyroidism might be prone to pancreatic stones.
- Sliding or travelling of gall or biliary stones to the pancreatic duct (blockage of the biliary duct by gall stones).
Risk factors for pancreatic stones
Pancreatic stones are the consequence of chronic pancreatitis. However, not all pancreatic stones are of pancreatic origin; the following factors might have developed some of them:
- Alcohol abuse: Studies have shown that increased alcohol consumption (5 drinks per day) increases the risk of chronic pancreatitis. Chronic pancreatitis patients associated with alcohol show decreased pancreatic stone protein secretion, resulting in calcium carbonate crystallisation and deposition, leading to stone formation.
- Smoking: Nicotine induces structural and functional changes in the exocrine pancreas.
- Gene mutations: SPINK1 gene (pancreatic secretory trypsin inhibitor gene) mutations can increase the risk of chronic pancreatitis, which plays a major role in pancreatic stones.
- Autoimmune diseases: In diseases like autoimmune pancreatitis (AIP), the levels of immunoglobulin G4 (IgG4) are elevated; this phenomenon has a high risk of stone formation.
- Metabolic disturbances: Hypertriglyceridemia, hypercalcemia (due to hyperparathyroidism), diabetes mellitus, porphyria, and Wilson's disease tend to increase the risk of pancreatitis and stone formation.
- Environmental conditions: Other factors such as obesity and a sedentary lifestyle increase individuals' risk of stone formation.
- Anatomical abnormalities: Chronic obstructive pancreatitis and stone evolution might result from ductal blockage caused by inflammatory strictures or malignancies.
- Cystic fibrosis: In cystic fibrosis conditions, the role of cystic fibrosis transmembrane conductance regulator (CFTR) Cl- channel is impaired. CTFR plays a significant role in pancreatic ductal secretory functions.
Complications of pancreatic stones
The pancreatic stones might cause some complications, such as:
- Recurrent pancreatitis: As the stone gets obstructed or dislodged, it might develop inflammation of the pancreas.
- Peritonitis: long-lasting inflammation leads to fluid accumulation in the tissues between the organs.
- Hypovolemic shock: In some cases, with chronic inflammation, fluid accumulation depletes the blood volume and leads to dehydration. This causes the kidneys to retain the fluid, resulting in hypovolemic shock.
- Cholecystitis and cholangitis: The pancreatic stones might lead to gall bladder and common bile duct inflammation.
- Infection and septic shock: The stone blockage might cause the bacteria from the small intestine to backwash into the ducts, resulting in an infection. Sometimes, this infection might travel to the bloodstream and cause sepsis, which is life-threatening.
- Malnutrition: Nutrient absorption and digestion might be impaired by pancreatic stones. Weight loss and malnutrition might result from this condition.
- Diabetes: Obstructive pancreatitis rarely causes type-2 diabetes. Low rates of ketosis and high rates of insulin-induced hypoglycaemia are characteristics of diabetes caused by chronic pancreatitis or pancreatic stones. Pancreatic stones interfere with the pancreas and reduce its ability to produce insulin.
- Pancreatic cancer: It is a rare complication of pancreatic stones. Pancreatic cancer is more likely to develop in patients suffering from long-lasting pancreatitis.
- Pancreatic pseudocysts: These are often seen as a complication of chronic pancreatitis. Primarily, it occurs when there is an obstruction in the pancreatic duct due to biliary or pancreatic stones.
- Pancreatic necrosis (necrotizing pancreatitis): It is caused due to chronic inflammation or injury to the pancreas. It is a serious life-threatening condition that can lead to multiple organ failure and sepsis.
Pathogenesis of pancreatic stones
A crucial component in the development of pancreatic calculi is pancreatic stone protein (PSP). Gene expression is among the many elements contributing to a decrease in PSP. Calcium carbonate becomes oversaturated in the pancreatic juice when PSP is reduced. Then, this calcium carbonate gets distributed over the interior nidus.
Diagnosis for pancreatic stones
The diagnostic approaches for pancreatic stones include:
- Blood tests: Blood tests such as white blood cell count, serum amylase, and serum lipase levels help to evaluate the signs of inflammation and pancreatitis.
- Imaging tests:
- Abdominal ultrasound
- Computed tomography (CT scan)
- Magnetic resonance imaging (MRI scan)
- Endoscopic ultrasound
- Endoscopic retrograde cholangiopancreatography (ERCP)
Treatment for pancreatic stones
Pancreas stone treatment includes the following approaches:
Medical management:
- Pain relievers and opioid medications
- Stone dissolving medications
- Anti-biotics and more
Endoscopic management:
- Endoscopic retrograde cholangiopancreatography (ERCP)
- Stone extraction with balloon baskets and trawls
- Pancreatic sphincterotomy
- Extracorporeal shock wave lithotripsy (ESWL)
- Electrohydraulic lithotripsy (EHL) or Laser lithotripsy (LL) for stone crushing
- Dilation and stenting of pancreatic duct strictures
Surgical management (drainage and resection procedures)
Prevention of pancreatic stones
The following steps can help to avoid developing pancreatic stones:
- Maintaining a healthy weight.
- Eating a healthy diet.
- Maintaining the cholesterol levels within the normal range.
- Managing diabetes and other metabolic diseases.
- Limiting alcohol consumption.
- Avoiding smoking.
- Managing other co-morbidities or medical conditions.
- Avoid foods that have high quantities of sugars and fats.
- Drink plenty of water and fluids.
Pancreatic stones vs gallstones / Difference between pancreatic stones and gallstones
| Parameters | Pancreatic stones | Gallstones |
|---|---|---|
| Origin | Pancreas | Gall bladder |
| Symptoms | Severe abdominal pain (sometimes that might radiate to the back or chest region). It might cause additional symptoms such as nausea, vomiting, fever, etc. | Biliary colic (pain in the upper abdomen), nausea, vomiting, fever, etc. |
| Risk factors | Chronic pancreatitis, metabolic disturbances, obesity, autoimmune diseases, smoking, alcohol, etc. | Hypercholesterolemia, obesity, family history, metabolic and congenital abnormalities, etc. |
| Treatment | Medical management, endoscopic approaches and surgeries. | Treatment for gallstones also includes medical management, endoscopic approaches and surgeries. |
In some cases, gallstones can relocate from the gallbladder into the bile ducts and then into the pancreatic duct. This can cause a condition called gallstone pancreatitis. Gallstone pancreatitis is the most common cause of pancreatitis.
FAQs - Frequently asked questions on pancreatic stones
Share on
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868
Appointment request - health articles
Recent Articles