Choledocholithiasis, CBD Stone - Symptoms, Types, Causes, Complications, Treatment & Prevention
Pace Hospitals
What is common bile duct?
CBD full form in medical - Common Bile Duct
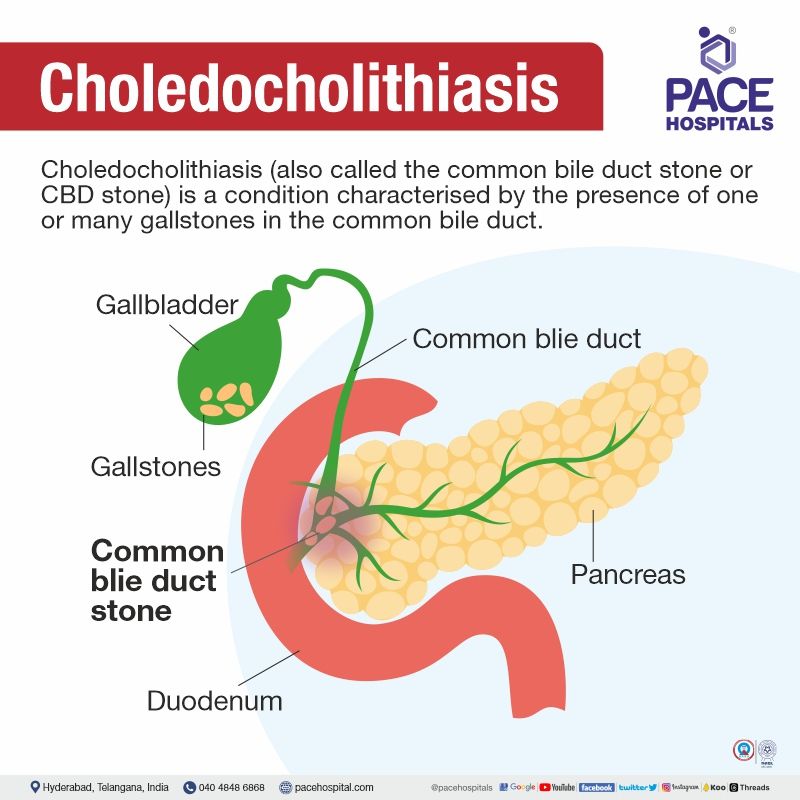
The common bile duct is a tube found in the biliary system and is responsible, for transporting bile from the liver and gallbladder to the intestine. Bile, a fluid crucial for fat digestion is produced by the liver and stored in the gallbladder until it's needed. Once food enters the intestine bile is released from the gallbladder. Travels through the common bile duct to reach the duodenum, which is the initial section of the small intestine.
The common bile duct (CBD) is located in the abdomen measuring around 8 centimetres in length the common bile duct forms when the common hepatic duct and cystic duct merge. The liver sends bile through the duct while bile from the gallbladder flows through the cystic duct. As it passes through the pancreas this important pathway joins with a duct at a pocket called ampulla of Vater. Within this pocket lies a muscle known as sphincter of Oddi for regulating both bile and pancreatic juice flow into duodenum.
An integral component of our system specifically involved in digestion is none other than common bile duct. Its main role is breaking down fats into molecules that can be easily absorbed into our bloodstream. Bile plays a role, in the absorption of vitamins like A, D, E and K which are vital, for maintaining good health.
What is Choledocholithiasis - CBD Stone?
Choledocholithiasis definition
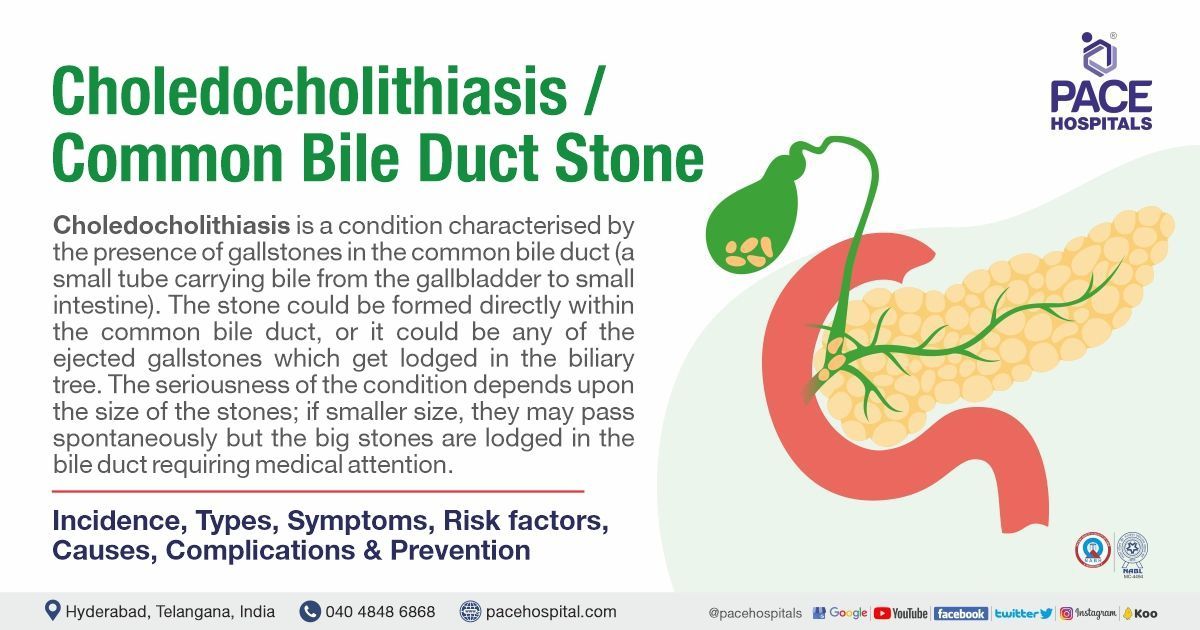
Choledocholithiasis (also called the common bile duct stone or CBD stone) is a condition characterised by the presence of one or many gallstones in the common bile duct. Painful right upper abdomen is the primary characteristic symptom. Endoscopic retrograde cholangiopancreatography (ERCP) or, in a few cases, laparoscopic cholecystectomy are the possible treatments.
- Primary choledocholithiasis: Stones which are formed directly within the biliary tree.
- Secondary choledocholithiasis: Gallstones which get ejected from the gallbladder and lodged in the biliary tree.
Choledocholithiasis meaning
Similar to many medical words, the word choledocholithiasis has Latin origins. “Choledocho” meant the common bile duct. “Lithos" is a Greek word which means stone. “Sis” is another Greek-origin word which acts as a suffix appearing in various technical words. “Sis” is used to denote any process, or presence or condition.
Choledocholithiasis incidence worldwide
About 4.6-18.8% of patients who are under cholecystectomy (surgery for gallbladder removal, usually for gallstones) are seen with choledocholithiasis (CBD stone). The incidence of choledocholithiasis increases as people age.
The preponderance of female patients among choledocholithiasis (CBD stone) patients could be due to high serum lipid levels. Similarly, choledocholithiasis (CBD stone) is more commonly seen in the elderly and in pregnant patients. choledocholithiasis (CBD stone) occurs in up to approximately 20% of patients with cholelithiasis (Gallstones).
Choledocholithiasis incidence in India
A 2016 study from Hyderabad demonstrated that the prevalence of choledocholithiasis (common bile duct stone) was 9.63%.
The prevalence of cholelithiasis (gallstones) could vary from 2-29% in India, with an increase in recent years. An Indian study published in 2014 demonstrated that the prevalence of cholelithiasis (gallstones) was way higher in Northern Indians when compared to Southern Indians, followed by Maharashtra, particularly from the coastal region.
While rampant accessibility to ultrasonographic exams could attribute to the rising incidence of cholelithiasis (gallstones) in India, the changing socio-economic structure and diet could also be responsible.
Types of choledocholithiasis (CBD Stone)
As already mentioned earlier, there are two types choledocholithiasis (CBD Stone)
- Primary choledocholithiasis (CBD Stone) (stones formed directly within the duct)
- Secondary choledocholithiasis (CBD Stone) (ejected gallstones from gallbladder lodged in the biliary tree).
Separated only by location (site), both these stones have similar composition. A 1986 study demonstrated that suture material could also be found in the centre of the stones extracted in primary choledocholithiasis patients who underwent previous cholecystectomy.
Overall, research indicates that the common bile duct stones (primary) are more likely to be pigment type than gallbladder stones. Based on the percentage of cholesterol, there are at least three different types of stones. They are:
- Cholesterol gallstones
- Mixed gallstones and
- Pigment gallstones
Cholesterol stones: The stones are made up of more than 80% of cholesterol (the most common type)
Mixed stones: At least 30–80% cholesterol, along with biliary acids and calcium salts.
Pigment stones: Less than 30% cholesterol, with the major component being bilirubin salts.
Choledocholithiasis - CBD stone symptoms
There are both symptomatic and asymptomatic choledocholithiasis (common bile duct stone). While in cases of asymptomatic choledocholithiasis, symptoms may be seen at the advanced stage, with symptomatic choledocholithiasis, the symptoms can be seen right away. Common bile duct stone (CBD stone) symptoms are similar to those of gallbladder stones.
The most common symptom includes the pain in the right upper abdomen. It is a sudden onset of pain in the right upper abdomen and is termed as biliary colic. Other choledocholithiasis (CBD stone) signs and symptoms may include:
- Jaundice (yellow discolouration of skin)
- Nausea and vomiting
- Inability to eat fatty food
- Pruritus (itchy skin)
- Chronic diarrhoea.
- Haematuria (urine turning tea-coloured)
- Steatorrhea (stools that are greasy and foul-smelling)
Choledocholithiasis risk factors
Cholelithiasis (Gallstones) and choledocholithiasis (CBD stone) are both abnormal conditions of the biliary tree and most likely share similar risk factors. Nevertheless, the common risk factors for primary choledocholithiasis as mentioned in a systematic review published in 2020 are:
- Peripapillary diverticulum: A condition of pouch type formation outside duodenum. It was confirmed that patients with peripapillary diverticulum are 2.6 times more likely to have primary choledocholithiasis (CBD stone).
- Abnormal biliary structure: It was shown that common bile duct with larger diameter had more frequent stone recurrences.
- Residual stone fragments: In patients who underwent previous cholecystectomy, patients might have tiny residual stone fragments which may be missed during stone extraction. These could act as cores for primary choledocholithiasis (CBD stone).
- Hypothyroidism: Thyroxine deficiency might increase primary choledocholithiasis (CBD stone).
- Biliary infection (Enterobacter and Helicobacter pylori): These bacteria can decompose conjugated bilirubin into unconjugated bilirubin, which combines with calcium to calcium stone primary choledocholithiasis (CBD stone).
Factors that affect hepatic production of cholesterol, gallbladder function, bile acid production, or intestinal absorption of cholesterol and bile acids are all possible contributors to the formation of gallstones. Risk factors of secondary choledocholithiasis (CBD stone) include both modifiable and nonmodifiable variables.
Nonmodifiable Risk Factors include:
- Female gender
- Family history
- Pregnancy
- Age older than 40 years
Modifiable Risk Factors include:
- Obesity - Nearly 25% of morbidly obese persons have gallbladder disease.
- Rapid weight loss – It causes an increased ratio of cholesterol to bile salts or the occurrence of bile stasis because of decreased gallbladder motility.
- Rapid weight loss cycling - The fluctuations between rapid weight loss and periods of weight gain that often equal or exceed preceding weight loss.
- High-calorie diet - A high-calorie diet can result in obesity and, thus, choledocholithiasis (CBD stone).
- Medications – Thiazide diuretics could cause gallstones upon frequent use.
- Type 2 diabetes – Metabolic syndrome causes gallstones.
- Also, medications, smoking and a sedentary lifestyle are a few of the common factors that increase gallstone formation.
Choledocholithiasis causes
The eventual slide of gallstones into the common bile duct is the cause of choledocholithiasis (CBD stone). Cholelithiasis is the formation of gallstones and may present with or without symptoms. In choledocholithiasis (CBD stone), the gallstones lodge within the common bile duct, blocking the flow of bile flow from the gallbladder to the duodenum.
While most gallstones are formed in the gallbladder, which get migrated and lodged in the common bile duct, there are cases of gallstone formation in the common bile duct itself. This is the most common reason why choledocholithiasis (CBD stone) still occurs in people who underwent cholecystectomy (gallbladder removal surgery) but are exposed to the above-said risk factors.
Choledocholithiasis complications
Not only long-standing choledocholithiasis (CBD stone) but its treatment could also lead to several complications of choledocholithiasis, such as:
- Post-ERCP Pancreatitis – At least 1-10% of the patients may experience pancreatitis post-ERCP. In high-risk patients, it can reach as much as 30%.
- Sepsis – An intense condition of extreme immune system response to an infection
- Wound infection – usually bacterial infection.
- Cholangitis - bile duct inflammation.
- Retained and impacted stones - Incomplete gallbladder removal could lead to residual stones, which could cause abdominal pain and jaundice.
- Gallstone pancreatitis - inflamed pancreas due to pancreatic duct blockage by gallstones.
- Respiratory failure - a severe condition of breathlessness, and the lungs can't get enough oxygen into the blood.
- Biliary duct injury – these injuries could be usually seen after surgery.
- Hepatic vascular injury - right hepatic artery injury may occur during cholecystectomy.
- Patients with asymptomatic choledocholithiasis (CBD stone) face a much higher risk of severe complications.
Choledocholithiasis diagnosis
Confirmation of the correct diagnosis of choledocholithiasis (CBD stone) is necessary for proper management, and similarly, there could be various other tests that the gastroenterologist may suggest ruling out choledocholithiasis differential diagnosis. The common choledocholithiasis (CBD stone) diagnosis could include:
- Understanding past medical history
- Physical examination of vital signs
- Complete blood picture
- Liver function tests
- Amylase test
- Lipase test
- Urinalysis
- Ultrasonography (transabdominal ultrasound)
- Magnetic resonance cholangiopancreatography (MRCP)
- Hepatobiliary iminodiacetic acid (HIDA) scan
There are cases in which the patient who is currently undergoing laparoscopic or open cholecystectomy, the surgeons accidentally discover unknown choledocholithiasis (CBD stone). During this time, the gastroenterologist may perform an intraoperative cholangiogram to assess choledocholithiasis.
Choledocholithiasis treatment
Since there are no medications which treat the condition, surgeries are the only way forward. The common surgical treatment of choledocholithiasis includes:
- Endoscopic retrograde cholangiopancreatography (ERCP)
- Cholecystectomy
- Open choledochotomy
- Transcystic exploration
- Percutaneous extraction
- Extracorporeal shock wave lithotripsy
Cholelithiasis (Gallstones) with choledocholithiasis (CBD stone) is not uncommon. In these cases, endoscopic and surgical procedures are the only treatment to help patients. Endoscopic Retrograde Cholangiopancreatography (ERCP) for choledocholithiasis is the most common treatment.
Choledocholithiasis presentation (symptoms appearance) is an influencing factor for the surgeons to decide if they intend to wait and observe before resorting to ERCP-guided treatment, especially in the case of asymptomatic choledocholithiasis (CBD stone).
Choledocholithiasis diet
Eating foods rich in fibre, such as fruits, peas, and whole grains are necessary in patients with choledocholithiasis (CBD stone). Similarly, foods containing refined carbohydrates (such as white flour, white rice, etc.) must be reduced.
Choledocholithiasis prevention
The prevention of choledocholithiasis (CBD stone) is invariably connected with the prevention of gallstones. Gallstones can be prevented with a few dietary tips (dietary management of gallstones), such as:
- Intake of high fibre, low saturated fatty acid and nut consumption are associated with a reduced risk of gallstones in the general population.
- At least mild-moderate physical activity can prevent gallstones and, thus, choledocholithiasis (CBD stone).
- Limiting weight loss to a moderate rate (maximum 1.5 kg/week) with measures such as
- adding 10 g of fat to low-calorie diets.
- Taking the hydrophilic bile salt ursodeoxycholic acid (UDCA).
- Treatment of biliary colic by NSAIDs reduces the risk of acute cholecystitis and choledocholithiasis (CBD stone).
Choledocholithiasis vs cholelithiasis | Difference between choledocholithiasis and cholelithiasis
Both choledocholithiasis (CBD stone) and cholelithiasis (Gallstones) represent conditions affecting the biliary tree. Choledocholithiasis is a more serious condition than cholelithiasis because it can block the flow of bile, leading to jaundice, liver damage, and other complications. Cholelithiasis can also be serious, but it is less likely to cause complications.
| Parameters | Choledocholithiasis (CBD Stone) | Cholelithiasis (Gallstones) |
|---|---|---|
| Definition | presence of gallstones in the common bile duct | presence of gallstones in the gallbladder |
| Treatment | Usually ERCP choledocholithiasis | Usually cholecystectomy (gallbladder removal surgery) |
| Recurrence | Reoccurrence seen even if gallbladder is removed | No reoccurrence with gallbladder removal |
Choledocholithiasis vs choledochal cyst | Choledocholithiasis and choledochal cyst differences
Both choledocholithiasis and choledochal cyst can cause abdominal pain, jaundice, and cholangitis (inflammation of the bile ducts).
| Parameters | Choledocholithiasis | Choledochal cyst |
|---|---|---|
| Definition | Gallstones in common bile duct | Rare congenital or acquired dilations (enlargements) of the bile ducts |
| Prevalence | It is more common in adults. | It is more common in children. |
| Complications | Mainly gallstone pancreatitis | Cholangitis with a 2% malignancy risk |
| Treatment | Usually ERCP choledocholithiasis | Complete excision and biliary tree reconstruction with hepaticojejunostomy |
Cholecystitis vs choledocholithiasis | Difference between cholecystitis and choledocholithiasis
Both cholecystitis and choledocholithiasis can cause abdominal pain, especially in the upper right abdomen. Other symptoms that can be common to both conditions include nausea, vomiting, fever, jaundice, dark urine, and pale stools.
| Parameters | Cholecystitis | Choledocholithiasis |
|---|---|---|
| Definition | Gallbladder inflammation, commonly due to cystic duct blockage by gallstones. | Gallstones in common bile duct |
| Complications | Gallbladder infection, peritonitis etc | Commonly acute biliary pancreatitis |
| Treatment | Usually cholecystectomy | Usually ERCP choledocholithiasis |
Biliary colic vs Choledocholithiasis | Difference between biliary colic vs Choledocholithiasis
Both biliary colic and choledocholithiasis can cause severe abdominal pain, especially in the upper right abdomen. Other symptoms that can be common to both conditions include nausea, vomiting, fever, and sweating.
| Parameters | Biliary colic | Choledocholithiasis |
|---|---|---|
| Definition | Steady or episodic pain in the upper right abdomen, under the rib cage, usually associated with the diseases of the biliary tree (especially with gallstones). | Gallstones in common bile duct |
| Appearance | Could be seen in cholangitis, cholecystitis or cholelithiasis or in choledocholithiasis. | Biliary colic is one of the most common features of symptomatic choledocholithiasis. |
| Treatment | Biliary colic is usually treated with over-the-counter pain relievers and fluids. | Choledocholithiasis typically requires treatment to remove the gallstones from the common bile duct through ERCP or surgery. |
Mirizzi syndrome vs choledocholithiasis | Difference between mirizzi syndrome and choledocholithiasis
Both Mirizzi syndrome and choledocholithiasis can cause obstruction of the bile flow and lead to similar symptoms, such as jaundice, abdominal pain, and fever. Mirizzi syndrome is a rare condition, while choledocholithiasis is a more common condition. Mirizzi syndrome is more likely to cause complications, such as liver damage, cholangitis (inflammation of the bile ducts), and biliary cirrhosis.
| Parameters | Mirizzi syndrome | Choledocholithiasis |
|---|---|---|
| Definition | Blockage of common hepatic duct due to compression from stone stuck in the cystic duct or infundibulum (opening) of the gallbladder | Gallstones in common bile duct |
| Complications | Cholecystobiliary or cholecysto-enteric fistula formation | Acute biliary pancreatitis |
| Treatment | Cholecystectomy | Usually ERCP choledocholithiasis |
Cholangitis vs choledocholithiasis | Difference between cholangitis and choledocholithiasis
Both cholangitis and choledocholithiasis can cause abdominal pain, jaundice, and fever. Cholangitis is a more serious condition than choledocholithiasis because it can lead to complications such as sepsis and liver abscess.
| Parameters | Cholangitis | Choledocholithiasis |
|---|---|---|
| Definition | Inflammation of the bile duct system. | Gallstones in common bile duct |
| Complications | Bacteremia/septicemia could occur. | Usually, acute biliary pancreatitis |
| Treatment | Antibiotic therapy and biliary drainage surgery. | Usually ERCP choledocholithiasis |
Share on
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868