Constipation: Symptoms, Causes, Risk Factors, Diagnosis, Treatment & Prevention
PACE Hospitals
Constipation definition
Constipation is defined as a condition characterized by infrequent or difficulty in evacuation of stools. Constipation can be accompanied by various symptoms, which include hard stools, straining while passing stools, a sensation of anorectal blockage, incomplete evacuation, and abdominal discomfort.
The main cause of constipation involves a combination of lifestyle habits, medical conditions, and medication use. Constipation can be managed by lifestyle changes and treating the underlying medical conditions. If left untreated, constipation can lead to major complications such as piles/haemorrhoids, anal fissures, faecal impaction, and rectal prolapse. These complications can cause discomfort, bleeding, infection, and, in severe situations, surgery or even death.
A general physician and gastroenterologist can successfully diagnose, treat, and manage the problem, ensuring proper healing and avoiding complications
Constipation meaning
The word constipation comes from the Latin word "constipatio", which means "a crowding together" or "a pressing together." It is derived from the verb constipare, where con-means "together" and stipare means "to press" or "to pack.
The term entered English around the early 15th century through Middle English and Medieval Latin.
Constipation Statistics
Constipation statistics worldwide
The global prevalence of constipation, particularly functional constipation, varies widely, ranging from less than 1% to more than 30% across different countries and populations. Studies using self-defined criteria indicate that approximately 12% of people worldwide report constipation. A pooled prevalence of 14. % has been reported using the Rome criteria, suggesting that functional constipation affects one in six to one in ten people globally.
Constipation statistics in India
Recent large surveys have shown that constipation affects between 11% and 24.8% of adults in India, with most studies finding it to be around 22%. This shows that constipation is a common and important health problem in both cities and villages, affecting about one in five adults across the country.
Types of Constipation
Predominantly, there are two types of constipation based on the factors that cause it, which are:
- Primary or functional constipation
- Secondary constipation
Primary or Functional Constipation
Primary constipation originates from problems directly affecting the colon or has no clear external cause. It is further divided into different types, which include:
- Normal Transit Constipation (NTC)
- Slow Transit Constipation (STC)
- Outlet Constipation (Pelvic Floor Dysfunction)
- Idiopathic Constipation
Normal Transit Constipation (NTC)
Normal transit constipation is the most common type. In this type, the colon moves stool at a normal speed, and physical check-ups usually don't show any problems. However, people still feel constipated. They may have trouble having bowel movements, go less often, have hard stools, feel bloated, or have stomach pain. Even though they feel this way, their stool usually comes out at a normal rate and is not delayed. This type can be similar to another condition called irritable bowel syndrome (IBS) with constipation (IBS-C), but without the strong stomach pain that comes with IBS-C.
Slow Transit Constipation (STC)
Slow transit constipation is less common. It happens when stool moves more slowly through the colon. This causes fewer trips to the bathroom, less frequent urges, more straining, and sometimes a swollen belly or stool that can be felt in the abdomen. The main problem is that the colon muscles are not working well. It’s more common in women. Nerve problems in the colon can also slow things down. Usual treatments like eating more fibre or using laxatives often don’t work as well for these people.
Outlet Constipation (Pelvic Floor Dysfunction)
Outlet constipation, also called pelvic floor dysfunction or defecatory disorders, happens because the muscles in the lower part of the body (pelvic floor or anus) don’t work properly. People with this problem often say they have to strain a lot, feel like they can’t fully empty their bowels, or need to use their hands (like pressing near the anus or vagina) to help pass stool.
The problem is that the muscles don’t relax or work together the right way when trying to poop, making it hard to go even if the stool is ready to come out.
Idiopathic Constipation
Idiopathic constipation means that the cause of the constipation is not known. It usually lasts a long time and can happen along with the other types of constipation. People with this kind often have a hard time going to the bathroom, don’t go often, or don’t feel fully empty after a bowel movement. The problem keeps happening over time without a clear reason.
Secondary Constipation
Secondary constipation happens when constipation is caused by something outside the digestive system, like a medical condition, medication, or certain lifestyle habits. This is different from primary constipation, which is due to problems inside the colon or rectum. Secondary constipation usually happens because of other health issues or external factors.
One of the most common causes of secondary constipation is medication. Many types of medicine, like strong painkillers (opioids), some antidepressants, certain blood pressure drugs, iron tablets, antacids, and cancer treatments (chemotherapy), can slow down the movement of the bowels or change how the gut works, leading to constipation. People may notice they get constipated after starting a new medicine or changing the dose.
Medical problems are also a big reason for secondary constipation. Hormone and metabolism issues, like low thyroid (hypothyroidism) and diabetes, can affect how the stomach and intestines work, making bowel movements less frequent. Brain and nerve diseases such as Parkinson’s disease, multiple sclerosis, dementia, and the effects of a stroke can damage the nerves and muscles needed to pass stool, making it harder. Muscle-related diseases like scleroderma and amyloidosis can also play a role by affecting the muscles in the digestive system.
Physical problems in the gut can also cause secondary constipation. These include things that block the colon or rectum, like colon cancer, narrowing of the bowel (strictures), twisted intestine (volvulus), or serious hemorrhoids and tears near the anus (anal fissures). These blockages can make it hard for stool to pass, causing constipation.
Lifestyle habits are often part of the problem too. Not drinking enough water, eating too little fibre, not moving around enough, or ignoring the need to go to the bathroom can all lead to constipation. Sudden changes in routine—like traveling, being pregnant, or staying in bed for long periods—can also cause constipation in people who are sensitive to these changes.
Constipation Symptoms
Constipation is a common digestive problem that can cause disturbance in daily routines and overall comfort. The quality and ease of bowel movements, as well as several associated symptoms, are important considerations when defining it. It is very important to recognize these symptoms for timely diagnosis and effective management.
Constipation is often recognized through a combination of noticeable bowel movements and physical discomfort.
Signs and symptoms of constipation include the following:
- Infrequent bowel movements
- Hard or lumpy stools
- Straining during defecation
- Sensation of incomplete evacuation
- Sensation of anorectal blockage or obstruction
- Need for manual maneuvers to facilitate defecation
- Abdominal discomfort or bloating
Infrequent Bowel Movements
Fewer than three bowel movements per week is a common sign of constipation. This reduction in frequency can lead to stool accumulation in the intestines, resulting in discomfort and additional digestive issues.
Hard or Lumpy Stools
When stool remains in the colon for an extended period, excessive water absorption occurs, making the stool hard, dry, or lumpy. This type of stool is more difficult to pass and is commonly associated with constipation.
Straining During Defecation
Constipation often involves significant effort to pass stool. Straining can lead to complications, such as swollen rectal veins (hemorrhoids) or minor tears in the anal lining.
Sense of Incomplete Evacuation
A feeling that the bowel has not fully emptied after defecation. This sensation can lead to repeated, often unsuccessful, attempts at bowel movements, causing frustration and discomfort.
Sensation of Anorectal Blockage or Obstruction
A sensation of blockage in the rectum that hinders stool passage is commonly noted. This may be related to functional or structural abnormalities in the rectal or pelvic floor region.
Need for Manual Maneuvers to Facilitate Defecation
In serious cases, manual assistance such as digital evacuation or pressure is applied near the anus is required to expel stool. This is typically needed in complex constipation.
Abdominal Discomfort or Bloating
Frequent constipation may result in pressure, abdominal pain, and bloating. These symptoms may occur due to the buildup of stool and gas within the intestines, which can also affect appetite and general well-being.
Pathophysiology of Constipation
Constipation results from disturbances in the normal function of the colon, rectum, or the neuromuscular coordination involved in defecation. The key mechanisms include:
Delayed Colonic Transit
In some individuals, the movement of stool through the colon is slower than normal. This prolonged transit time allows more water to be absorbed from the stool, making it dry, hard, and more difficult to pass.
Impaired Rectal Evacuation (Outlet Dysfunction)
In cases of pelvic floor dysfunction or defecatory disorders, the muscles of the pelvic floor and anal sphincter fail to relax or coordinate properly during defecation. This leads to incomplete or obstructed stool passage, despite normal or slow transit through the colon.
Abnormal Neuromuscular Activity
Nerve dysfunction affecting the enteric nervous system or central nervous system can impair the coordination of muscular contractions in the colon and rectum. This disrupts peristalsis and weakens the defecation reflex.
Altered Rectal Sensation and Compliance
Some individuals may have decreased sensation in the rectum or reduced ability of the rectal walls to stretch and accommodate stool. This leads to reduced urge to defecate and retention of stool.
Colonic Dysmotility
In slow-transit constipation, the colonic motor activity—especially high-amplitude propagated contractions (HAPCs), which help move stool—is reduced or absent. This results in infrequent bowel movements.
Causes of Constipation
Constipation occurs when the normal movement of stool through the digestive system slows down or becomes difficult. This can happen for various physical or functional reasons inside the body. Knowing the actual causes of constipation is important to help find the right treatment and prevent future problems.
Constipation can arise from several direct disruptions in the body’s digestive process. Main causes of constipation are:
- Pelvic Floor Dysfunction
- Colonic or Rectal Obstruction
- Neurological Dysfunction
- Hormonal Imbalance
- Medical Conditions That Affect Bowel Function
- Use of Certain Medications
Pelvic Floor Dysfunction
The muscles in the pelvic floor need to relax and tighten in the right way for stool to pass. If these muscles don’t work properly or don’t coordinate well during a bowel movement, stool can’t be pushed out, even when the person feels the urge to go. This makes it hard to have a complete or comfortable bowel movement.
Colonic or Rectal Obstruction
Physical blockages in the colon or rectum can prevent stool from passing. Problems like colon cancer, narrowing of the intestine (strictures), twisted bowel (volvulus), severe hemorrhoids, or anal fissures can block or narrow the path of stool. This causes stool to build up and makes bowel movements painful or difficult.
Neurological Dysfunction
Nerves control how the muscles in the intestines and rectum work. When there’s damage to these nerves—such as from a spinal cord injury or a nerve-related illness—it can interfere with the normal signals between the brain and the gut. This disrupts bowel movements and causes constipation.
Hormonal Imbalance
Certain hormones help regulate how fast the intestines move. In conditions like low thyroid (hypothyroidism) or high calcium levels in the blood (hypercalcemia), these hormonal changes slow down the activity of the digestive system. As a result, stool moves more slowly and becomes harder, leading to constipation.
Medical Conditions That Affect Bowel Function
Diseases that affect the nerves or muscles in the digestive system can make it harder for the body to move stool. Conditions like diabetes, Parkinson’s disease, multiple sclerosis, and stroke can weaken the muscles or damage the nerves that control the intestines. This leads to reduced bowel movement and constipation.
Use of Certain Medications
Some medicines can slow down how the intestines work or make the stool drier. Medications like opioid painkillers, antidepressants, iron supplements, calcium channel blockers, and certain antacids reduce the movement of the intestines or increase how much water is absorbed from the stool. This results in slower and harder bowel movements.

Constipation Risk Factors
Constipation is a condition that can affect anyone and depends on a variety of underlying risk factors.
Identifying the risk factors that lead to constipation is important, as it helps doctors to analyze people more prone to develop the condition. Early finding and management of the factors can help to prevent constipation and effectively improve the treatment.
Constipation tends to arise more frequently in the presence of risk factors like:
- Female gender
- Older age
- Low physical activity
- Low fibre diet
- Inadequate fluid intake
- Poor bowel habits
- Certain medications
- Medical conditions
- Psychological factors
- Low socioeconomic status
- Positive family history
- High work-related stress
- Irregular bowel habits
Female Gender
Women are more likely to get constipated, possibly because of hormones like progesterone, which can slow down how the gut moves. Also, differences in the shape of the pelvic area and a higher chance of certain bowel problems in women add to this risk.
Older Age
As people get older, their digestive system can slow down, and the muscles that help with bowel movements may get weaker. Older adults also often have other health problems and take medicines that can slow the bowels, making constipation more common as people age.
Low Physical Activity
Not moving around much is linked to slower movement of food through the intestines, which can cause fewer and harder bowel movements. Being active helps the gut work better and keeps bowel habits regular. People who don’t move much tend to have more constipation.
Low Fiber Diet
Fiber adds bulk to stool and helps move it through the colon more easily. Eating too little fiber leads to smaller, harder stools that move more slowly, which increases the chance of constipation, as shown in both medical studies and population surveys.
Inadequate Fluid Intake
Not drinking enough water makes the colon absorb more water from the stool, making it dry and hard to pass. While some studies give mixed results, many still agree that not drinking enough fluids can cause constipation, especially if a person also eats little fiber.
Poor Bowel Habits
Ignoring the urge to go to the bathroom can confuse the body’s natural signals. Over time, the rectum becomes less sensitive to the presence of stool. This allows stool to stay longer in the colon, where it loses more water and becomes harder, leading to constipation.
Certain Medications
Some medicines, like strong painkillers (opioids), drug that dry up secretions (anticholinergics), calming medicines (benzodiazepines), and drugs for Parkinson’s disease, can slow the gut or pull more water out of the stool. These effects are well known, and constipation caused by medication is common, especially in older people and those who are often sick.
Medical Conditions
Long-term illnesses like diabetes, Parkinson’s disease, stroke, kidney failure, and heart disease can affect the nerves or muscles that help move the bowels. This can slow things down and cause constipation. These links are supported by large studies and doctor observations.
Psychological Factors
Mental health issues like depression, anxiety, and poor sleep are closely linked with constipation. They affect how the brain and gut work together and may reduce a person’s drive to follow healthy habits, which can lead to bowel problems.
Low Socioeconomic Status
People with lower income or education may have less access to healthy foods, medical care, or information about bowel health. This can lead to poor eating habits and more exposure to things that cause constipation, though this can vary by region.
Positive Family History
If other family members have constipation, it may be due to inherited traits or shared habits and lifestyles that raise the risk. Studies show that people with constipated relatives are more likely to have it themselves.
High Work-Related Stress
Ongoing stress from work can affect how the gut works and lead to unhealthy habits, like poor eating or irregular bathroom routines, which can cause constipation.
Irregular Bowel Habits
Often, ignoring the urge to go to the bathroom or not having a regular time to go can mess up the natural signals that help to poop regularly. Over time, this can turn into long-term constipation, as shown in studies of large groups of people.
Complications of Constipation
Constipation is not only uncomfortable but can also lead to a range of complications if left unaddressed. Recognizing these complications is important for timely intervention and prevention of further morbidity.
If left unmanaged, constipation may give rise to the following complications:
- Hemorrhoids
- Anal fissures
- Fecal impaction
- Rectal prolapse
- Bowel incontinence
- Abdominal discomfort and cramps
- Rectal bleeding
- Poor quality of life
Hemorrhoids
Pushing too hard during bowel movements puts extra pressure on the veins in the rectum, which can cause hemorrhoids—swollen and sore blood vessels near the anus. These can lead to pain, itching, and bleeding, and are common in people with ongoing constipation.
Anal fissures
Passing very hard and dry stool can cause small cuts or tears in the skin around the anus. These cuts, called anal fissures, are painful, can bleed, and make it even harder and more painful to go to the bathroom, creating a cycle of pain and constipation.
Fecal impaction
If constipation is very bad or lasts too long, stool can get stuck and harden in the rectum or colon. This is called fecal impaction. It can block the bowel, cause stomach pain, and may need a doctor to remove the stool by hand or with surgery.
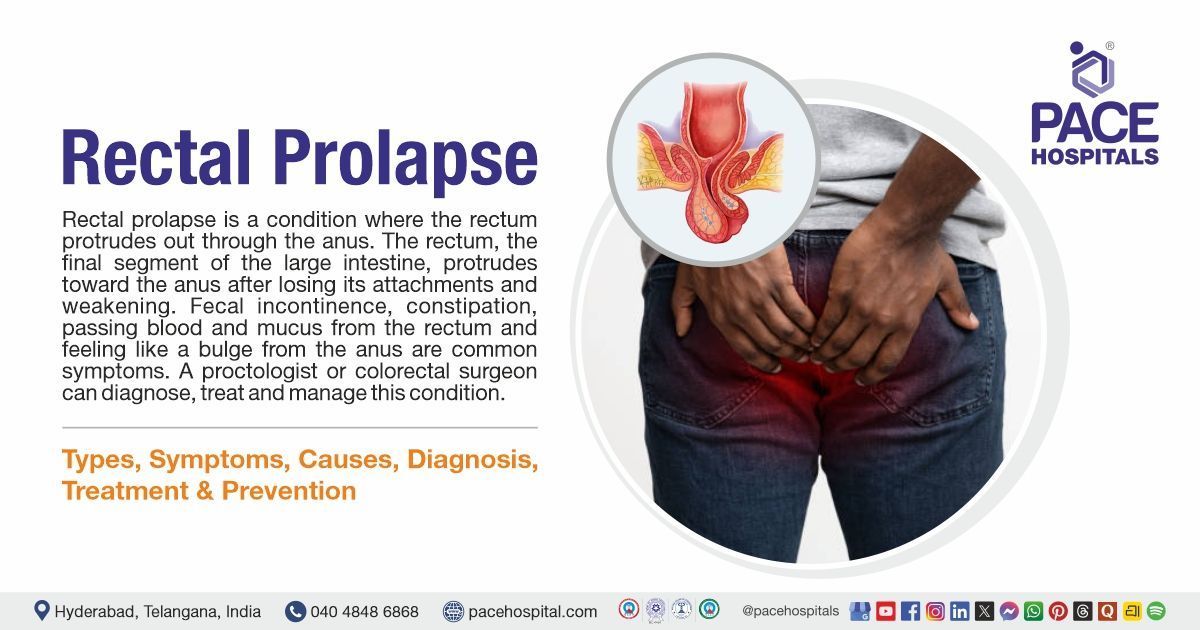
Rectal prolapse
Straining too much can weaken the muscles and tissues that hold the rectum in place. This may cause part of the rectum to slide out through the anus, a condition called rectal prolapse. It can be uncomfortable, may lead to leaking stool, and sometimes needs surgery to fix.
Bowel incontinence
Long-term constipation, especially with stool buildup, can cause watery stool to leak around the blockage. This is called overflow incontinence and leads to accidental soiling, which can be very upsetting.
Abdominal discomfort and cramps
Constipation often causes belly pain, bloating, and cramps because of built-up stool and pressure in the intestines. These symptoms can make it hard to go about daily life and feel comfortable.
Rectal bleeding
Straining and pushing out hard stools can cause small injuries in the anus or rectum, leading to bleeding. It’s usually light, but if it often happens, it can cause low iron or anemia.
Poor quality of life
Constipation and its problems can greatly affect both body and mind. It can make people feel worse overall, limit their social life, increase doctor visits, and lower their general happiness and health.
Constipation Diagnosis
In most cases, individuals with ongoing constipation first consult a general physician, who performs an initial evaluation. If the symptoms continue, are severe, or more serious underlying condition. The patient may be sent to a gastroenterologist to evaluate the condition. Then the specialist may follow a systematic process to determine the cause of the symptoms and detect any underlying problems or complication.
This process involves:
Clinical History and Physical Examination
- Detailed history: Assessment includes duration and frequency of symptoms, stool characteristics, associated symptoms (such as blood in stool, weight loss), medication use, diet, and lifestyle habits.
- Physical exam: Includes abdominal examination and a digital rectal exam to check for masses, stool in the rectum, and anorectal abnormalities.
Laboratory Tests
- Blood tests: To evaluate for anemia, hypothyroidism, diabetes, electrolyte disturbances, and other metabolic disorders.
- Stool tests: Check for occult blood, infection, or inflammation.
- Urine tests: May be used to screen for metabolic diseases such as diabetes.
Imaging and Endoscopic Evaluation
- Abdominal X-ray: Used to assess stool burden and detect bowel obstruction.
- Barium enema or lower GI series: Visualizes structural abnormalities of the colon and rectum.
- Colonoscopy or sigmoidoscopy: Direct visualization of the colon to rule out malignancy, polyps, or inflammation, especially in cases with alarm features or older age.
Colorectal Transit and Functional Tests
- Colorectal transit studies: Radiopaque marker study or scintigraphy to assess how quickly stool moves through the colon.
- Anorectal manometry: Measures pressures and muscle coordination in the rectum and anus to diagnose defecatory disorders.
- Balloon expulsion test: Evaluates the ability to expel a simulated stool, helping diagnose pelvic floor dysfunction.
- Defecography: Imaging test (X-ray or MRI) to assess the mechanics of defecation and pelvic floor function.
Other Considerations
Diagnosis is often clinical for mild or uncomplicated cases, with further testing reserved for refractory, severe, or complicated presentations, or when secondary causes are suspected.
Constipation Treatment
Management of constipation involves a certain approach that starts with lifestyle and dietary changes, which is followed by medication if required. Treatment is tailored based on the patient's symptom severity, underlying cause, and response of the treatment. In some cases, advanced therapies may be required to achieve long-term relief and improve the condition.
Treatment of constipation involves a range of supportive and therapeutic strategies, including the following approaches:
Lifestyle and Dietary Modifications
- Ensure dietary fibre intake to approximately 35 grams per day. Sources are fruits, vegetables, and grains.
- Intake of plenty of water to help soften stools.
- Encourage regular physical activity to stimulate bowel motility.
- Proper bathroom routines, especially after meals.
First-Line Pharmacological Therapy
- Bulk-forming agents: Increase stool bulk and promote movement through the colon.
- Osmotic laxatives: Draw water into the colon to soften stools and improve frequency.
- Stimulant laxatives: Stimulate intestinal contractions and are recommended if bulk-forming or osmotic agents are ineffective or for as-needed use.
Second-Line and Adjunctive Therapies
- Secretagogues and prokinetic agents: Used for chronic or refractory constipation, especially in cases of functional constipation or irritable bowel syndrome with constipation (IBS-C).
- Suppositories and enemas: Used for fecal impaction or when oral medications are ineffective.
Special Considerations
- Opioid-induced constipation: May require combination therapy with osmotic and stimulant laxatives or peripherally acting opioid receptor antagonists.
- Pregnancy: Prefer fiber, bulk-forming agents, osmotic laxatives, or stool softeners; stimulant laxatives only occasionally and under medical supervision.
Non-Pharmacological and Advanced Interventions
- Biofeedback therapy: For pelvic floor dysfunction or dyssynergia.
- Surgical intervention: Rarely needed, reserved for refractory cases with structural abnormalities or severe slow-transit constipation unresponsive to medical therapy.
Regular follow-up is essential to assess response and adjust treatment as needed. Identifying and managing any underlying or secondary causes should always be part of the therapeutic plan.
Why Choose PACE Hospitals?
Expert Super Specialist Doctors
Advanced Diagnostics & Treatment
Affordable & Transparent Care
24x7 Emergency & ICU Support
Prevention of Constipation
Preventing constipation is often easier and more effective than treating it after it develops. By making simple and consistent changes to daily habits, most people can support healthy digestion and avoid chronic issues with bowel movements. Prevention focuses on keeping the digestive system active, hydrated, and regular through natural means like diet, exercise, and mindful routines.
Constipation can be prevented by managing healthy daily habits and routines, including the following measures:
- Eating a high-fibre diet
- Drinking enough water
- Staying physically active
- Not ignoring the urge to have a bowel movement
- Establishing a regular bathroom routine
- Managing stress effectively
- Avoiding unnecessary use of constipating medications
- Ensuring adequate sleep and rest
Eating a high-fibre diet
Fiber adds bulk and softness to stool, which helps it move smoothly through the intestines. Eating fibre-rich foods like fruits, vegetables, legumes, and whole grains encourages regular bowel movements and prevents hard, dry stools that are difficult to pass.
Drinking enough water
Adequate water intake helps keep stool soft and facilitates its movement through the intestines. Proper hydration reduces water absorption by the colon from the stool, preventing it from becoming dry and hard. Sufficient fluid consumption, particularly water, is especially important when dietary fibre intake is increased.
Staying physically active
Regular exercise stimulates the natural movement of the intestines, known as peristalsis. Activities like walking, yoga, or swimming can help promote regular bowel movements and prevent sluggish digestion.
Not ignoring the urge to have a bowel movement
Responding promptly to the body’s natural urge to have a bowel movement helps maintain regularity. Ignoring the urge can cause stool to remain in the colon longer, making it harder and more difficult to pass later.
Establishing a regular bathroom routine
Setting a consistent time each day to try having a bowel movement—especially after meals—can train the body to be more regular. This improves body's natural rhythm and supports predictable bowel habits.
Managing stress effectively
Stress can affect the digestive system and brain connection, and slow down digestion. Practicing relaxation techniques like deep breathing, meditation, or regular hobbies can reduce stress and support regular bowel function.
Avoiding unnecessary use of constipating medications
Certain medications, such as painkillers and antacids, can cause constipation when used frequently or without a medical indication. These medications should be used under professional supervision, and alternative options should be considered if constipation occurs.
Ensuring adequate sleep and rest
Lack of sleep can disrupt the body’s normal processes/functions, including digestion. Getting enough rest helps the body maintain hormonal balance and regular bowel movements.
Differences Between Constipation and Diarrhoea
Constipation vs Diarrhoea
Constipation and diarrhoea are two common yet opposite digestive issues that affect bowel habits and overall health. While constipation involves difficulty passing stool, diarrhoea is marked by frequent and loose bowel movements. Understanding their differences is essential for proper management and treatment. The table below highlights key distinctions between these two conditions.
| Feature | Constipation | Diarrhoea |
|---|---|---|
| Stool Frequency | Fewer than 3 bowel movements per week | More than 3 loose or watery stools per day |
| Stool Consistency | Hard, dry, and difficult to pass | Loose, watery, or unformed stools |
| Stool Passage | Difficult, often requires straining | Urgent, often uncontrollable |
| Abdominal Symptoms | Bloating, cramping, feeling of fullness | Cramps, urgency, sometimes pain with bowel movements |
| Causes | Slow colon movement, dehydration, low fiber, medications | Infections, food intolerance, inflammation, medication side effects |
| Complications | Hemorrhoids, anal fissures, fecal impaction | Dehydration, electrolyte imbalance, nutrient loss |
Frequently Asked Questions (FAQs) on Constipation
How long does constipation last?
Constipation can last from a few days to many weeks, depending on the underlying cause and how well it is managed. It is commonly defined as having fewer than three bowel movements each week. While occasional constipation is normal and can be self-managed, persistent constipation (lasting more than three weeks) or severe symptoms require medical care.
What foods cause constipation?
Foods which are low in fibre content, high in fats, sodium, sugar, fried foods, carbonated drinks, caffeine, dairy products, and processed foods cause constipation. Avoiding these foods can improve constipation.
What is the difference between bowel obstruction and constipation?
Bowel obstruction: A bowel or intestinal obstruction happens when something blocks the normal movement of contents through the digestive tract.
Constipation: Constipation is a medical condition characterized by infrequent bowel movements, which could be fewer than three per week.
How to reduce constipation?
Constipation can be reduced by increasing dietary fibre and fluid intake, indulging in regular physical activity, and establishing consistent bowel habits. If these measures are insufficient, bulk-forming agents, osmotic or stimulant laxatives, and stool softeners may be used. Addressing underlying medical conditions and reviewing medications that may contribute to constipation are also important steps.
Is constipation dangerous?
Constipation is usually not dangerous but can lead to complications like hemorrhoids, anal fissures, fecal impaction, or rectal prolapse if severe or prolonged. Rarely, it may signal an underlying serious condition requiring medical attention.
Why does hypothyroidism cause constipation?
Hypothyroidism has a direct connection with constipation. In hypothyroidism, thyroid hormones (T3 and T4) are not produced in sufficient amounts. These hormones play a crucial role in accelerating the digestive process, particularly when the digestive tract is slowed down.
Why does constipation cause bloating?
Constipation may cause bloating because backed-up stool in the colon causes an accumulation of digestive contents, including gas. The increased volume and pressure within the gut can cause the abdomen to enlarge and feel inflated, resulting in bloating.
What is slow transit constipation, and its treatment?
Slow transit constipation is a rare type of constipation. In slow transit constipation, people do not experience normal stimulation of the bowel, which is called peristalsis. Therefore, food moves through the gastrointestinal tract more slowly than usual, and bowel movement takes more time to pass out of the colon. And this can lead to infrequent bowel movements. Treatment generally involves laxatives and dietary and lifestyle changes.
What are the complications of chronic constipation?
If constipation is not treated promptly, it can lead to several complications, like haemorrhoids, anal fissures, faecal impaction, rectal prolapse, faecal incontinence, and rectal ulcer syndrome.
What are the differences between IBS and functional constipation?
Irritable bowel syndrome with constipation is defined by recurring stomach pain triggered by bowel movements or changes in stool frequency or form, which is often accompanied by bloating and abdominal discomfort. Functional constipation, on the other hand, is characterised by consistently difficult, infrequent, or incomplete bowel movements that are not accompanied by considerable stomach pain.
While both conditions share symptoms like straining and hard stools, the presence of abdominal pain is the major characteristic that distinguishes between irritable bowel syndrome with constipation and functional constipation.
What are the causes of constipation in children?
Constipation in children can be caused by a variety of factors, including dietary changes, a lack of fibre and water, ignoring bowel urges, and specific medical conditions or drugs.
What are the causes of constipation in women?
Constipation in women can result from various factors, including dietary habits, lifestyles factors, and underlying health conditions. Inadequate fibre intake, insufficient hydration, lack of physical activity, changes in daily routine, and stress can all contribute to constipation. Additionally, medical issues such as depression, the use of certain medications, and hormonal changes during pregnancy or menopause may also play a role.
What are the complications of constipation during pregnancy?
Constipation is a common symptom during pregnancy, which is due to the combination of hormonal and mechanical factors affecting the normal gastrointestinal function. Many women suffer from constipation prior to conception, and the symptoms often worsen during pregnancy.
Does constipation cause blood in stool?
Constipation can cause blood in the stool, most commonly due to straining, which may result in hemorrhoids or anal fissures. Hard stools can damage the lining of the anus, resulting in bright red rectal bleeding. While this bleeding is often minor and self-limited, persistent or significant bleeding should be evaluated to rule out more serious conditions.
Do bananas cause constipation?
Bananas are not generally considered a cause of constipation. Ripe bananas contain soluble fibre, which can aid bowel movements, while unripe bananas have more resistant starch, which may be constipating for some individuals. The overall effect depends on the ripeness and individual digestive response.
Does coffee cause constipation?
Coffee is more commonly associated with stimulating bowel movements due to its caffeine content and effects on colonic motility. However, in rare cases, excessive coffee intake or sensitivity may contribute to dehydration, which could theoretically worsen constipation, especially if fluid intake is otherwise low.
How to relieve constipation during pregnancy immediately?
Immediate relief of constipation during pregnancy can be sought by increasing fibre and fluid intake, gentle physical activity, and using bulk-forming or osmotic laxatives if recommended by a healthcare professional. Suppositories or enemas may be considered for acute relief, but any intervention should be discussed with a healthcare professional to ensure safety.
Is constipation a sign of pregnancy?
Constipation can occur in pregnant women due to hormonal changes that slow intestinal motility, but it is not a definitive sign of pregnancy. It is one of several nonspecific symptoms that may be experienced in early pregnancy, alongside others like nausea and breast tenderness.
Is papaya good for constipation?
Papaya is considered beneficial for constipation because of its high fibre content and the presence of digestive enzymes, which may help soften stools and promote regular bowel movements. Including papaya as part of a balanced, high-fibre diet can support digestive health.
Can antibiotics cause constipation?
Antibiotics are more commonly associated with diarrhoea, but in some cases, they may disrupt gut flora and slow bowel movements, leading to constipation. The effect varies depending on the specific antibiotic and individual response.
How to relieve constipation in babies quickly?
Constipation in babies can often be relieved by gentle abdominal massage, leg exercises, ensuring adequate hydration, and in some cases, using glycerin suppositories as advised by a healthcare expert. Dietary adjustments, such as offering pureed fruits or increasing fluid intake, may also help, depending on the baby's age.
Can constipation cause cancer?
Constipation itself does not cause cancer. However, chronic constipation may be associated with an increased risk of developing certain colorectal conditions, and persistent changes in bowel habits should be evaluated, as they can sometimes indicate underlying colorectal cancer.
Does protein powder cause constipation?
Protein powders, especially those low in fibre and high in dairy content, can contribute to constipation in some individuals. Ensuring adequate fluid and fibre intake when using protein supplements can help prevent this issue.
Can constipation cause fever?
Constipation alone does not cause fever. However, complications such as fecal impaction or associated infections may lead to fever. The presence of fever with constipation warrants medical evaluation to rule out serious underlying conditions.
Can constipation cause headaches?
Constipation has been associated with headaches in some individuals, possibly due to the buildup of toxins or general discomfort. While not a direct cause, the two symptoms can occur together, particularly in functional gastrointestinal disorders.
Can constipation cause stomach pain?
Stomach pain is a common symptom of constipation, often resulting from the buildup of stool and increased gas in the intestines. The pain typically resolves once normal bowel movements resume.
Can constipation cause weight gain?
Constipation may cause a temporary increase in weight due to retained stool and fluid, but it does not cause true fat gain. The weight typically normalizes after bowel evacuation.
Can stress cause constipation?
Stress can contribute to constipation by affecting gut motility and altering digestive hormones. Psychological factors are recognized contributors to functional gastrointestinal disorders, including constipation.
Can smoking cause constipation?
Smoking is not a direct cause of constipation, but nicotine can affect gut motility. In some individuals, smoking cessation may temporarily lead to constipation as the bowel adjusts to the absence of nicotine.
Does constipation cause high blood pressure?
Constipation does not directly cause high blood pressure, but straining during bowel movements can lead to temporary spikes in blood pressure. Chronic straining may have cardiovascular implications in susceptible individuals.
When to consult a doctor for constipation?
Consult a doctor for constipation when bowel movements are infrequent, complex, or painful for several weeks, or when symptoms start interfering with daily comfort.
Key signs that need medical care include:
- Constipation lasting longer than three weeks
- Severe abdominal pain or bloating
- Blood in the stool or rectal bleeding
- Unexplained weight loss
- Persistent fatigue or weakness
A constipation doctor or gastroenterologist can recommend suitable constipation treatment, including diet changes, medications, or tests for underlying causes. Urgent care is needed if constipation comes with severe pain, vomiting, or inability to pass stool or gas.
Share on
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868