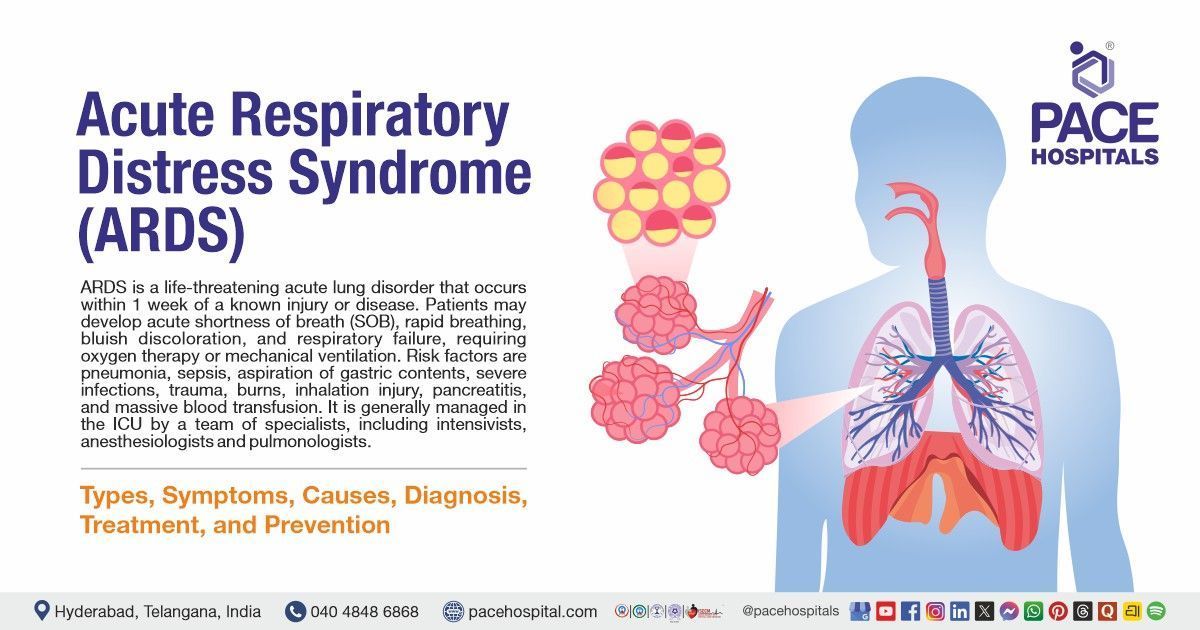
Piles (Hemorrhoids): Symptoms, Causes, Types, Prevention, Treatment
Pace Hospitals
Piles Meaning
Piles (Haemorrhoids), are lumps or common swellings containing enlarged blood vessels that develop inside and around the passage of the anal canal (back passage from where the stool passes).
The surface of the anal canal is lined with a complex network of tiny veins (blood vessels). They're more like cushiony areas above the anus that help with passing gas without the poop coming out and help control stool defecation by maintaining the blood flow and pressure in the area. These veins occasionally swell and become overloaded with blood. The enlarged veins and the tissue above them may subsequently group to form one or more swellings called piles.
They become problematic when they start causing pain, itching, bleeding, or leaking during defecation. Treatment is required only when they cause symptoms and should be treated if symptoms are persistent.
Hemorrhoids definition
Hemorrhoid word derived from Old French “emeroudis” and evolved into “haemorrhoidae” and “haimorrhoides” in Latin and Greek, where the “haima” means “Blood” and “rhoos” means “a stream, a flowing” and “rhein” means “to flow”
Piles prevalence
Piles (haemorrhoids) are a common anorectal condition, and every perianal disease is termed haemorrhoids by most patients.
According to 2016 research by the Association of Colon & Rectal Surgeons of India (ACRSI), roughly 5% of the population experiences haemorrhoids at any time, and about 50% will experience them by age 50.
A demographic study of haemorrhoids stated that the most common age group affected by haemorrhoids was the middle age group (41-60 years).
They are very common in both men and women, However, this study stated that the sex-wise distribution of haemorrhoids for male-to-female ratio was 2.2:1, which might be due to the greater likelihood of men seeking treatment for their haemorrhoids and the embarrassment felt by women to consult for anorectal problems. As per the other studies, males are more predominant than females.
This association of haemorrhoids to higher socioeconomic status may be due to the more prevalent constipation due to poor dietary habits and lack of physical activity in this group.
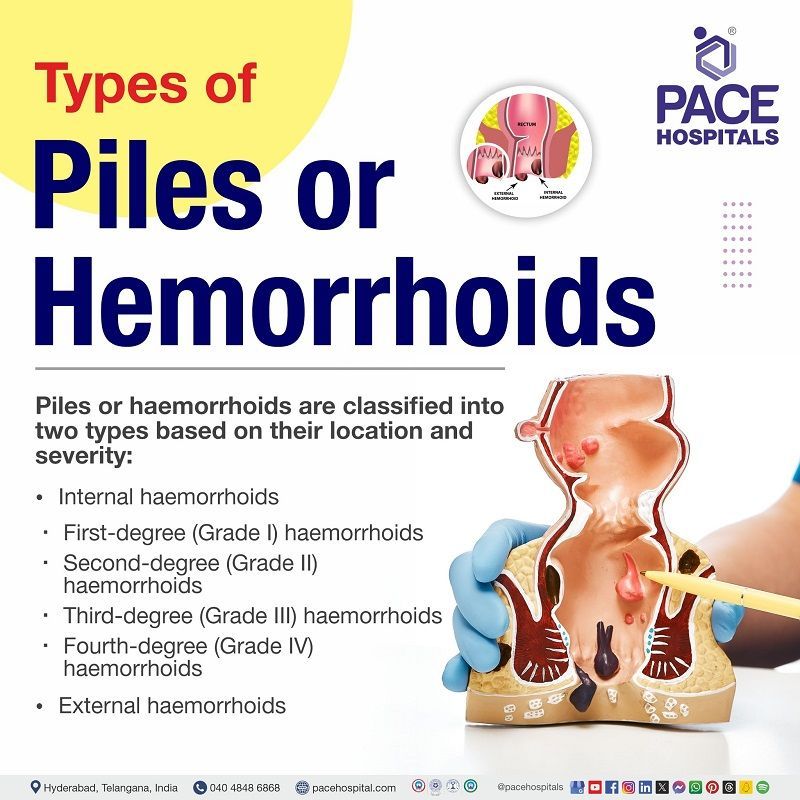
Types of piles (haemorrhoids)
Piles (haemorrhoids) are classified into two types based on their location and severity:
- Internal haemorrhoids
- First-degree (Grade I) haemorrhoids
- Second-degree (Grade II) haemorrhoids
- Third-degree (Grade III) haemorrhoids
- Fourth degree (Grade IV) haemorrhoids
- External haemorrhoids
Internal haemorrhoids
Internal haemorrhoids are deeper in origin and range above 2cm and form in the lining of the anus and lower rectum. They are typically painless but causes rectal bleeding.
- Patients may see bright red blood on the toilet paper or dripping into the toilet bowl. In some cases, they enlarge and protrude (prolapse) outside of the anus.
- Prolapsed haemorrhoids are more severe and painful. Usually, they come outside from the anus during wiping or whenever having a bowel movement.
- When a haemorrhoid protrudes, it can collect small amounts of mucus and tiny stool particles that may irritate, called pruritus ani.
- The symptoms increase slowly and are intermittent in nature. In some cases, haemorrhoids hang out permanently due to constriction of the anal sphincter (muscle).
Internal haemorrhoids are classified into four different types based on the degree of prolapse (how much they protrude outside of your anus).
- First-degree (Grade I) haemorrhoids: They bleed but do not prolapse (do not protrude from the anus).
- Second-degree (Grade II) haemorrhoids: They have the ability to prolapse and retract on their own, with or without bleeding.
- Third-degree (Grade III) haemorrhoids: These haemorrhoids can become prolapsed but can be pushed back using a finger.
- Fourth-degree (Grade IV) haemorrhoids: They can prolapse and cannot be pushed back in.
External haemorrhoids
External haemorrhoids originate under the skin around the anus, covered by sensitive skin, and range 2cm in size. These blood vessels (haemorrhoids) are usually painless unless a thrombosis (blood clot) forms, or they become very swollen due to blood and often appear as bluish-coloured lumps.
The development of blood clots or thrombosis in the haemorrhoids causes severe and constant pain (because somatic nerves supply the area). This tends to increase the pressure in the tightly held area, resulting in the breakage of the blood clot, which in turn causes leakage. If the haemorrhoids are not thrombosed, patients may complain of swelling, discomfort, and pressure.
The clot usually dissolves, leaving excess skin (a skin tag) that may itch or irritate. Skin tags are painless, small, and almost “pinched-up” pieces of skin. These are the most uncomfortable because the overlying skin becomes irritated and erodes. Thrombosis of an external haemorrhoid that may require incision and drainage.
Piles causes
Piles causes are a bit unclear. However, Piles (haemorrhoids) are thought to be caused by repeated increased pressure in the rectal and anal veins. Several factors may cause this condition, including:
- Constipation, passing large stools (faeces), and straining at the toilet: These situations can increase the pressure in and around the veins in the anus and appear to be a common reason for haemorrhoids to develop.
- Pregnancy: This condition is common in pregnant women due to the raised pressure due to the growing baby above the rectum and anus and the potential effects of hormonal changes during pregnancy on the veins.Aging. As we age, the tissues present on the lining of the anus may not support or become less supportive
- Hereditary factors: Some people may get this disease due to inheriting a weakness of the wall of the veins in the anal region.
- Straining to lift heavy objects:
This activity, especially with improper form, puts pressure on veins in the rectum or anus, causing haemorrhoids.
Piles symptoms
Piles symptoms usually go away within a few days, and some people with haemorrhoids never have symptoms. However, if it occurs, symptoms may vary from person to person. Some of the most common symptoms include:
Internal haemorrhoids
- Bright red blood: Bright red coloured blood may appear as streaks on stool or toilet paper and blood that drips into the toilet following bowel movements.
- Prolapse: Internal haemorrhoids may protrude outside the anus during bowel movements and then retract back inside.
- Pain and discomfort: Usually, Internal haemorrhoids that are not prolapsed are not painful. However, prolapsed haemorrhoids often cause pain, discomfort, and anal itching.
- Mucus discharge: Some individuals with third and fourth-degree haemorrhoids have accidental leakage in the form of mucus discharge due to an impairment of the fine regulation of continence.
External haemorrhoids
- Swelling or a hard lump around the anus: A lump that can be seen and felt around the anus with or without associated pain, and the patient may experience swelling, itching, or mucus discharge after bowel movements.
- Bleeding: Thrombosed external haemorrhoids cause bleeding, painful swelling, or a hard lump around the anus.
- Irritation and itching:
When the blood clot dissolves in thrombosed haemorrhoids, extra skin is left behind. This skin can become irritated or itchy. Excessive straining, cleaning or rubbing, around the anus area may make symptoms including itching and irritation worse.
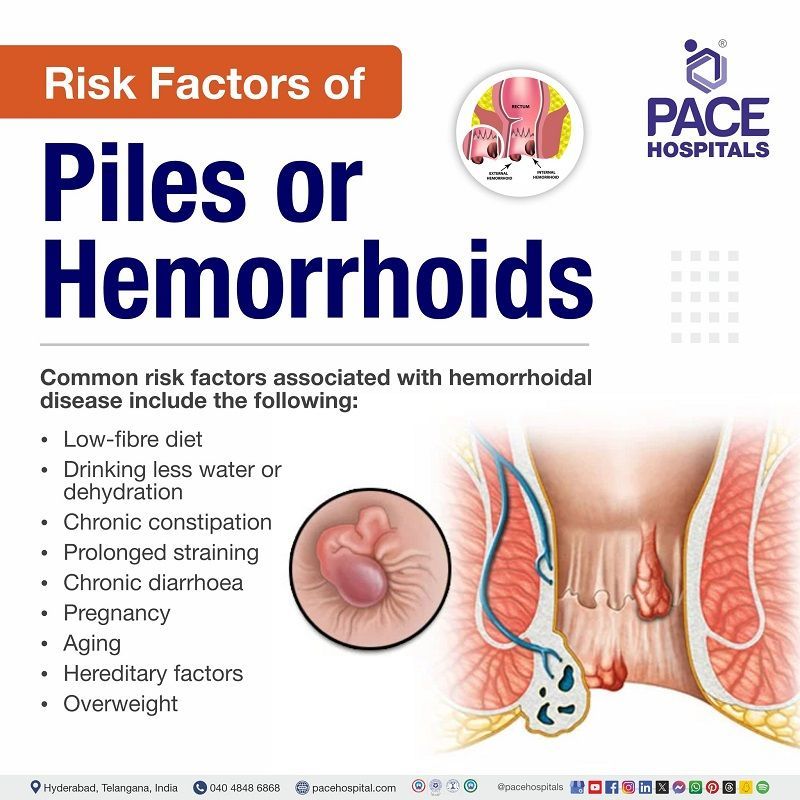
Piles risk factors
Piles risk factors are easily manageable and the following are some of the common risk factors associated with it:
- Low-fibre diet: Hemorrhoids are rare in cultures with high-fibre, unrefined diets.
- People consuming a low-fibre diet tend to strain more during bowel movements because smaller and harder stools are more difficult to pass.
- Straining increases the pressure in the abdomen, obstructing the blood flow upward through the legs.
- Over time, this increased pressure may significantly weaken the walls of veins, leading to the development of varicose veins or haemorrhoids.
- Drinking less water or dehydration: Lack of water in the body makes the stools pass harder, which in turn causes piles.
- Chronic constipation: Constipation is believed to increase the risk of haemorrhoids due to the excessive force on the anal cushions caused by passing hard stools.
- Prolonged straining: Prolonged straining increases intraabdominal pressure and may obstruct venous return, raising the risk of haemorrhoidal swelling.
- Chronic diarrhoea: Diarrhoea often contains bile or gastric acid, so passing the watery stool can irritate the rectum, which may increase the risk of haemorrhoids. The long periods of straining and sitting down associated with diarrhoea may also contribute to the formation of haemorrhoids.
- Pregnancy: Pregnancy (growing baby) increases the size of the uterus, leading to increased pressure on rectal veins, resulting in a raised risk of haemorrhoids.
- Aging: The risk of developing haemorrhoids increases as person ages because of weakening of the tissues that are supporting the veins in the rectum and anus over time.
- Hereditary factors: Inheritance of weakness in the anal wall increases the risk of haemorrhoids.
- Overweight: This puts pressure on the lower abdomen and increases the risk of haemorrhoids.
Other risk factors, such as leading a sedentary lifestyle, delaying bowel movements, lack of physical activity, high intake of a spicy and non-vegetarian mixed diet, may contribute to constipation, increase the risk of haemorrhoids, and trigger a recurrence.
Piles complications
Piles (haemorrhoids) are not life-threatening or dangerous. However, if left untreated, they may cause possible complications that should be addressed immediately:
- Perianal thrombosis: A blood clot has formed in the veins around the anus due to the external haemorrhoids causing pain and might bleed.
- Incarcerated prolapsed internal haemorrhoids with subsequent thrombosis: This complication refers to internal haemorrhoids that have slipped out of place (prolapsed) and become trapped outside the anus, causing pain and bleeding.
- Anaemia: If a patient loses more blood, anaemia condition may occur.
- Infection: Rarely, due to the bacteria from faecal matter or Irritation and breakage in the anal area may lead to severe infection.
- Stenosis: Closure of the anal passage may occur due to chronic swelling and scarring.
- Strangulation of piles: Reduced blood flow to piles occurs due to trapped prolapsed haemorrhoids outside the anus.
- Skin tags around the anus: Skin tags around the anus may result from extra skin left behind when a blood clot in an external haemorrhoid dissolve.
Piles diagnosis
Generally, haemorrhoid condition is not serious, and symptoms may disappear in a few days, but sometimes this may signal a serious problem. It is recommended to consult a healthcare professional if persistent pain and rectal bleeding occurs. A healthcare professional may perform one or more diagnostic tests to examine the anus and rectum to confirm the piles and to identify the differential diagnoses, including:
- Physical examination
- Physical exam
- Digital rectal exam
- Imaging methods
- Barium enema X ray
- Minimally invasive diagnostic techniques
- Anoscopy
- Proctoscopy
- Colonoscopy
- Sigmoidoscopy
Physical examination
- Physical exam: It is performed to check the rectum and anus to find any swollen blood vessels that could sign of external haemorrhoids.
- Digital rectal exam: The healthcare professional inserts a gloved, greased (lubricated) finger into the patient's rectum to palpate (feel) the internal haemorrhoids or any other abnormalities.
Imaging methods
- Barium enema x-ray: A barium (contrast material) is inserted into the large intestine to make the large intestine more visible in X-ray pictures to examine clearly.
Minimally invasive diagnostic techniques
- Anoscopy: Healthcare professionals use a hollow, lighted tube and insert it into the patient's anus to see the internal haemorrhoids or any abnormalities in the rectum and anus.
- Proctoscopy: During this process, a lighted tube will be inserted into the anus to get a view of the entire rectum.
- Colonoscopy: A long, flexible tube with a light and a camera called a colonoscope will be inserted into the colon (large intestine) through the rectum to examine the entire large intestine to find any ulcers (sores), swelling, redness, abnormal growths, and bleeding.
- Sigmoidoscopy: A short, flexible tube with a tiny camera and light called a sigmoidoscope is inserted into the intestine through the rectum to see inside the large intestine and determine the underlying cause of belly pain, constipation, bleeding, diarrhoea, and abnormal growth.
Both sigmoidoscopy and colonoscopy will be used to take the tissue sample (biopsy) to identify any abnormalities or cancer cells.
Piles treatment
Piles (haemorrhoid) treatment depends on the patient age, symptoms severity and state of the haemorrhoid. The following are the some of the treatments, that includes:
Conservative treatments
- Home treatments
- Sitz baths
- Ice packs
- Timed toilet training
- Lifestyle changes
- Lifestyle modifications
- Medical therapies
- Oral medications
- Creams, ointments and suppositories
Surgical procedures
- Haemorrhoidectomy
- Rubber band litigation
- Sclerotherapy
- Infrared photocoagulation
- Radiofrequency coagulation and excision
Conservative treatments
Conservative treatments should be advised as a first line of management, regardless of the severity because symptoms are expected to improve moderately with conservative treatment for all types of haemorrhoids, whether they are in an early stage or an advanced stage.
The conservative treatments may include as follows:
Home treatments
- Sitz baths: Warm bath with Epson salts will reduce irritation, itchiness and pain by lowering anal pressure, assisting in keeping the anus clean and enhancing anal blood circulation, which reduces congestion and oedema.
- Ice packs: Ice packs will be recommended to reduce swelling.
- Timed Toilet Training: It involves establishing a regular schedule for bowel movements to encourage efficient and less straining defecation.
Lifestyle changes:
Every patient may receive lifestyle recommendations from healthcare professionals for initial therapy and to reduce the likelihood of recurrence in those requiring further intervention.
- Lifestyle modifications: Following lifestyle changes such as eating high fibre food with plenty of water, exercising regularly, avoiding alcohol etc can help to reduce the constipation.
Medical therapy:
Primarily, medical therapy includes recommending fibre-based laxatives to maintain soft stools and prevent straining. Other options may include as follows:
- Oral medications: Oral medications play a role in treating haemorrhoids, either as a preventive measure in the early stages or to control severe bleeding until hospital procedures or surgery can be performed.
- Creams, ointments, suppositories: Healthcare professionals recommend oral medicines and a bland soothing cream, ointments, or suppositories to ease discomfort. These include various combinations of corticosteroids, vasoconstrictors, local anaesthetics, antiseptics, and astringents.
Surgical techniques
Surgical techniques may be needed to shrink or remove haemorrhoids. Below mentioned are some of the surgical procedures that may be performed to treat the haemorrhoids:
- Haemorrhoidectomy: If the patient is experiencing large internal haemorrhoids or external haemorrhoids that do not respond to other treatment options, a healthcare professional may recommend removing them permanently. However, removal options depend on the haemorrhoid’s location, size, and severity. Less than 10% of symptomatic haemorrhoids are treated with surgical removal.
- Rubber band litigation: In this technique, a band is placed around the haemorrhoid to cut off its blood flow, eventually causing it to fall off. This takes 5-7 days, and the patient may feel slight discomfort or pressure.
- Sclerotherapy: Chemicals are injected into the patient's haemorrhoid to shrink it. This process is typically painless but may require multiple sessions to be effective.
- Infrared photocoagulation: This method uses infrared radiation (a hot light) to eliminate excess haemorrhoid tissue. It is relatively painless but may require multiple procedures to reduce your symptoms.
- Radiofrequency coagulation and excision: In this technique, a healthcare professional delivers radio waves between 5.0 and 6.0 MHz through a radiofrequency electrode to remove the haemorrhoid while keeping the temperature low.
- Embolization: Embolization involves pushing 2-3mm fibre coils into blood vessels supplying haemorrhoids to shrink them by cutting off their blood supply under local anaesthesia, reducing symptoms.
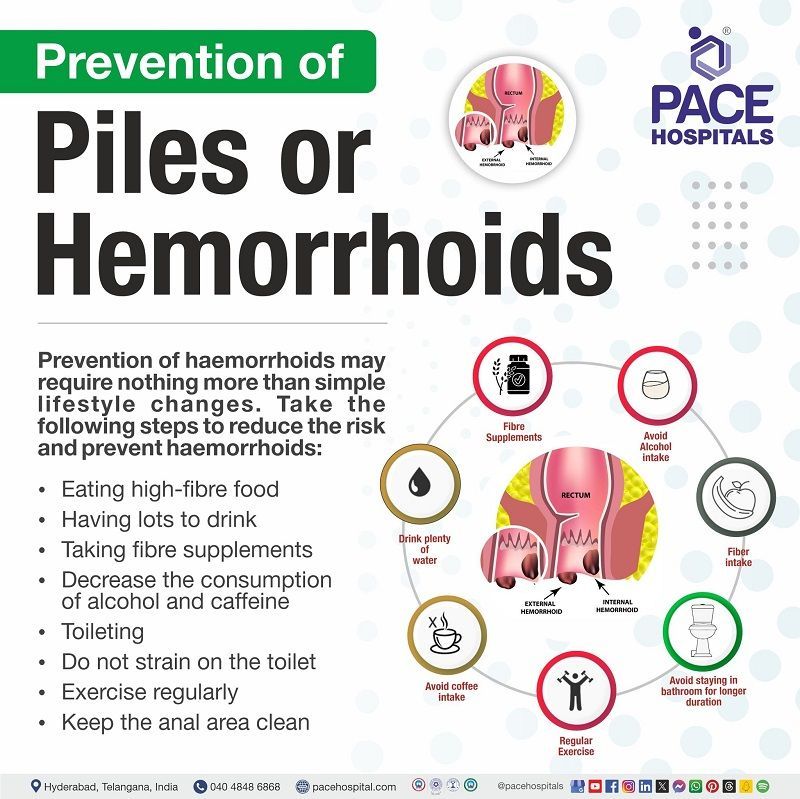
Piles prevention
Piles (haemorrhoids) prevention may require nothing more than simple lifestyle changes. Take the following steps to reduce the risk and prevent haemorrhoids:
Diet
- Eating high-fibre food: Plenty of fibre, such as fruit, vegetables, cereals, nuts, seeds, wholemeal bread, etc., will help make stools soft, bulky, and formed. High-fibre food can also help prevent constipation, resulting in a decreased risk of haemorrhoids in the future.
- Having lots to drink: Drinking lots of water, at least two litres (10-12 cups) per day, can help to soften the faeces.
- Taking fibre supplements: If a high-fibre food is not helping, fibre supplements (bulking agents) may help; hence, consult a healthcare professional before taking the supplements.
- Decrease the consumption of alcohol and caffeine: Avoiding caffeine and alcohol helps prevent haemorrhoids by reducing dehydration and irritation of the gastrointestinal tract, which can exacerbate hemorrhoidal symptoms.
Medications
- Avoiding painkillers: Some painkillers will be recommended to prevent, as they are a common cause of constipation.
Habits
- Toileting: Go to the restroom immediately after feeling the need. Some individuals suppress this feeling and plan to go to the bathroom later. This may result in bigger and harder faeces forming, which are more difficult to pass.
- Do not strain on the toilet: Avoiding excessive straining reduces pressure on haemorrhoids and helps prevent protrusion because the feeling of fullness due to haemorrhoids in the rectum may tempt one to strain at the end to try to empty the rectum further.
- Exercise regularly: Exercise regularly: Exercising helps digestion, improves circulation, and helps maintain a healthy weight.
- Keep the anal area clean: Wipe gently with soft, unperfumed tissue to keep the area clean to avoid any irritation.
Difference between piles and fissure
Piles induce swelling of veins and tissues in the anal region, especially around the anal opening, whereas in anal fissures, tearing is seen in the anal layer. Although people might confuse both conditions as similar, they have the following differences:
| Elements | Piles/haemorrhoids | Fissure |
|---|---|---|
| Causes | Constipation, pregnancy, prolonged sitting, overweight, straining to pass stool, dehydration, eating low fibre diet. | Constipation, sitting on a toilet seat for a long time, straining to pass the stool, Crohn’s disease. |
| Symptoms | Rectal bleeding, pain, bright red stools with blood, anal itching, one or more lumps with tenderness, anal pain on sitting. | Blood in stool, itching or burning sensation near the anal area, tear around the anal area, small bump near the tear, painful bowel movements. |
| Prevention | Taking fibre-rich diet, drinking a lot of water and liquids, avoid sitting continuously on toilets and hard surfaces, taking fibre supplements, maintaining healthy weight, doing exercises. | Taking fibre-rich diet, drinking a lot of water and liquids, avoid sitting continuously on hard surfaces, taking fibre supplements. |
| Treatment | Lifestyle modifications, ointments, creams, and suppositories containing corticosteroids, soothing agents, anti-biotics, and astringents. Various treatment procedures like rubber band ligation, injection sclerotherapy, infrared coagulation/photocoagulation, haemorrhoidectomy. | Lifestyle modifications, lateral sphincterotomy, open surgery, laser treatment. |
Frequently Asked Questions (FAQs) on Piles (Hemorrhoids)
How to diagnose haemorrhoids?
The healthcare provider makes a diagnosis based on criteria such as inquiring about the patient's medical background and performing a physical examination. During a digital rectal exam, a doctor can find external and internal haemorrhoids by examining the anus area and feeling for abnormalities.
Other diagnostic tests include anoscope, sigmoidoscope, and colonoscope to find any irregularities and to identify haemorrhoids.
How to cure piles/haemorrhoids?
Piles disease can be cured by taking preventive measures and following some simple lifestyle changes, such as drinking plenty of water, eating high-fibre food, exercising regularly, avoiding straining, etc. In severe cases, the surgeon prefers haemorrhoid surgery. However, piles recur if the patient doesn't follow the preventive measures.
How to control piles?
Piles can be controlled by taking fibre-rich diet, drinking a lot of water and liquids, avoiding sitting continuously on toilets hard surfaces, taking fibre supplements, maintaining healthy weight and exercising.
Is piles dangerous?
Piles are not dangerous or life-threatening. However, if left untreated in severe cases, they may cause complications such as thrombosis (formation of a clot) in piles, cut off the blood supply to the piles, and lead to severe pain. Whereas in rare cases, the piles may cause anal stenosis (closure of the anal passage).
Which foods cause piles?
Food that is with low fibre content causes piles/haemorrhoids. Food to avoid in piles are meat, frozen foods, chips, fast food, ice cream, snack foods, processed foods and microwavable food content etc.
What is piles?
Piles are often called haemorrhoids; they usually occur inside, and around the anal canal. The surface of the anal canal is lined with a complex network of tiny veins (blood vessels). These veins occasionally swell and become overloaded with blood. The enlarged veins and the tissue above them may subsequently group to form one or more swellings known as piles.
How to remove external haemorrhoids at home?
A patient can't remove haemorrhoids at home. However, they can treat the haemorrhoids at home by eating dietary fibre-rich foods, taking a fibre supplement or a stool softener, consuming enough liquids daily, not straining over when using the loo, avoiding spending excessive time on the toilet, taking warm showers to help with pain relief.
Which doctor to consult for piles?
The patient may consult the general practitioner, surgical gastroenterologist and colorectal surgeon regarding the treatment.
How to shrink haemorrhoid skin tag?
The patient cannot treat the anal skin tag beyond reassurance, but they can control it by modifying excessive wiping, maintaining a healthy weight and avoiding prolonged stays in toilets. However, surgical removal is recommended occasionally.
What is the best prescription medicine for haemorrhoids?
The piles doctor may prescribe the best medicine for piles based on the patient's condition and severity. Usually, most patients are recommended to use ointments and creams containing corticosteroids, soothing agents, and astringents for topical-local use.
What to eat in piles?
Consuming foods high in fibre, such as wholegrain bread, cereals, fruits, and vegetables, helps the stool move more easily. Drinking water keeps the patient hydrated and helps the faeces pass quickly without strain. Prevent constipation by taking fibre supplements and limiting the intake of alcohol and caffeine.
Is surgery the last option for piles?
Usually, piles can be managed in the initial stages with some medicines, ointments, food and lifestyle diet etc. But in advanced stages like grade 3 or 4, it may require a surgery to treat piles.
Is piles a lifetime disease?
No, in most of the cases piles go away on their own with lifestyle modifications, medicines, surgery etc.
Share on
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868