Pelvic Inflammatory Disease (PID) Treatment in Hyderabad, India
PACE Hospitals stands out as a leading center for pelvic inflammatory disease (PID) treatment in Hyderabad, Telangana, India. Our multidisciplinary team—comprising experienced gynecologists, infectious disease experts, radiologists, and nursing staff—works together to offer comprehensive care tailored to each patient’s needs.
We emphasize early detection and prompt treatment to prevent complications such as chronic pelvic pain and infertility. Using advanced technology and modern therapeutic approaches, we ensure effective management of PID in a caring and comfortable setting.
Book an Appointment for
PID Treatment
PID treatment appointment
Why Choose PACE Hospitals for Pelvic Inflammatory Disease Treatment?

Advanced Diagnostic & Minimally Invasive Laparoscopic Surgery
Best Gynecologists & Pelvic inflammatory disease specialists in Hyderabad, India
24/7 Emergency Care for Pelvic Inflammatory Disease Complications
Affordable & Transparent PID Treatment with Insurance & Cashless Options
The diagnosis of Pelvic inflammatory disease (PID) is based on the history and physical examination, which help the gynaecologist to conclude the diagnosis. The pelvic inflammatory disease treatment is subject to the treatment of the bacterial infections. As earlier the patient improves from the infection, the faster recovers from PID.
The gynaecologist considers the following before selecting the appropriate tests to diagnose pelvic inflammatory disease.
- The presented signs and symptoms
- Age, family history and general health of the suspected patient
- Medical history and medication history.
- The results of previous medical tests
Pelvic Inflammatory Disease (PID) Diagnosis
Usually, a gynaecologist can diagnose PID through the following:
Physical examination
- Pelvic examination
Laboratory tests
- Blood tests
- Urine examinations
- Erythrocyte sedimentation rate
- C-reactive protein
Imaging tests
- Ultrasound
- Trans-vaginal ultrasound
- CT-scan
- MRI scan
Minimally invasive procedures
- Pelvis laparoscopy
Others
- Swab test
- Nucleic Acid Amplification Tests (NAATs)
- Endometrial biopsy
- Culdocentesis
Physical examination
Pelvic Examination
Pelvic examination is the process performed to collect information about the pelvic area, which includes the vulva, vagina, cervix, uterus, ovaries, and fallopian tubes, includes visual external examination, manual examination, speculum exam, pap test and rectal exam.
Gynaecologists commonly perform pelvic examinations to feel for any swelling, assess the cervical discharge, and identify the tenderness. This test detects sexually transmitted infections (STIs), which are the primary cause for causing pelvic inflammatory disease. Samples can be taken from the cervix to find infections. It should be done to look for signs of diseases or infections.
Laboratory tests
Blood tests
A complete blood picture measures the number of white blood cells (WBC), red blood cells (RBC) and platelets in the blood. An elevated (increased) count of white blood cells indicates signs of inflammation and infection, which can be seen in pelvic inflammatory disease.
Blood tests measure hormone levels (FSH, LH, estrogen, progesterone, TSH, prolactin) and can help identify the pregnancy, providing valuable information about ectopic pregnancy that can cause similar symptoms to pelvic inflammatory disease. These tests can also diagnose specific types of sexually transmitted diseases (chlamydia, HIV, herpes, gonorrhoea, syphilis), often combined with urine tests to confirm. Blood tests alone are not enough to confirm this condition.
Urine examinations
A urinalysis is the most common diagnostic test conducted to examine the urine to detect and measure various compounds through physical, chemical, and microscopic tests and to assess many different aspects of health with a urine sample. It is performed to check RBC, proteins, WBC, and sugars.
Urinalysis is conducted to detect urinary tract infections (UTI) that can show (cause) symptoms, such as pelvic pain. It is also used to determine the presence of bacteria such as Neisseria gonorrhoeae and Chlamydia trachomatis, common causes of sexually transmitted infections (STIs). However, it is essential to note that a positive urinalysis does not necessarily indicate (signify) the presence of PID.
Erythrocyte sedimentation rate
ESR (marker of inflammation) can be increased in patients with pelvic inflammatory disease (PID). However, it is not a definitive indication(sign) of PID, as it is only observed in around 75% of women with mild cases. Moreover, ESR levels may also be increased in other medical conditions.
C-reactive protein
CRP is one of the group of proteins, called acute phase reactants, that increase in response to inflammation. CRP is another inflammatory marker in the body that has been studied in mild PID. It is often done with an erythrocyte sedimentation rate to check for inflammation. C-reactive protein will be elevated when there is inflammation in the body, such as rheumatoid arthritis, infections, and some cardiovascular diseases.
CRP levels are reduced sooner than ESR after effective antibiotic therapy, which helps find how treatment works in pelvic inflammatory disease.
Imaging tests
Pelvic ultrasound
A pelvic ultrasound is a diagnostic test that utilizes sound waves to make images of the organs inside the pelvis that are used to examine the organs and structures within the pelvis, such as the uterus, cervix, fallopian tubes, vagina and ovaries of the female. It allows the visuals of the pelvic organs. Ultrasound uses a transducer which places on the pelvic skin using the conductive gel.
In most cases, pelvic ultrasonography (ultrasound) is the first-line imaging method. Ultrasound findings suggest PID include abscess (fluid collections), thickened fallopian tubes, or increased ovarian volumes in the pelvic area. Ultrasound helps identify causative factors or rule out similar conditions, such as endometriosis.
Transvaginal Ultrasound
An ultrasound test identifies abnormalities using high-frequency sound waves to create (provide) pictures of internal organs. A transvaginal ultrasound, or endovaginal ultrasound, is used to examine the pelvis organs such as the uterus, ovaries, fallopian tubes, cervix and vagina. It differs from a regular pelvic ultrasound in that it involves the insertion of an ultrasound probe that measures approximately 2–3 inches into the vaginal canal. With this probe, the internal organs can be examined in detail, allowing gynaecologist to diagnose and treat various medical conditions.
Transvaginal sonography (transvaginal ultrasound) is very useful in identifying the suspected PID (pelvic inflammatory disease). It is usually helpful in identifying tubo-ovarian abscesses and ectopic pregnancy.
It is suggested at least three months after symptoms have subsided for patients with an adnexal mass (abnormal lump or swollen area due to infection) at the time of PID episode and for infertile patients.
CT scan
A CT scan utilizes an X-ray machine linked to a computer system to take a series of images of organs from different angles, which helps create detailed 3D pictures of the inside of the body. Before the scan, dye or contrast material can be used, or gives a needle into a vein, gives dye to swallow, which helps produce the images by highlighting specific areas in the body. The CT machine moves around the patient during the CT scan by creating the images.
On CT scan, PID can show fallopian tube and ligament thickenings, swollen lymph nodes due to infection, and fluid buildup in the pelvic area. Identifying the fallopian thickenings over 5mm strongly indicates PID (95%-chance of PID).
MRI scan
An MRI is an imaging instrument that uses powerful radio waves and magnets to take images of the body in slices. These slices are merged to create detailed cross-sectional pictures of the inside of the body to distinguish between normal and diseased tissue. During the process, the patient has to lie on a table and is pushed into a long chamber, where the MRI makes loud thumping noises and rhythmic beats. A special dye (contrast agent) was injected into a vein, which shows the pictures more brightly.
On MRI, PID shows a tubo-ovarian abscess, infected fallopian tube (pyosalpinx), fluid in a fallopian tube, or the appearance of ovaries similar to polycystic ovaries with free pelvic fluid. These findings are the signs of the PID condition, which helps diagnose it.
Minimally invasive procedures
Pelvic laparoscopy
Pelvic laparoscopy a minor invasive procedure is performed to examine and treat the abnormalities of the uterus, ovaries, cervix, and fallopian tubes in the pelvic area. It includes inserting the instrument into the abdomen by making small incisions. That instrument is called a laparoscope, which contains a thin device with an attached camera and light to visualize the organs.
Laparoscope can identify salpingitis (fallopian tube inflammation due to infection) and certain bacteria (that cause the infection). However, it can't justify the mild or unclear symptoms and cannot identify endometritis (inflammation of the uterus's inner lining).
Others
Swab test
Gynaecologist will take fluid samples from the vagina and cervix with a swab (the same as a cotton swab). Usually, it will take some days to give the result. A positive result of a swab test can confirm the diagnosis of pelvic inflammatory disease. A negative swab test result does not mean the patient is clear of pelvic inflammatory disease.
Sometimes, swabs can give false results (negative results) because swabs do not identify the exact infection causing the PID. Sometimes, an extra swab can be taken from the urethra, which increases the rate of detection of gonorrhoea, chlamydia or other infections.
Nucleic Acid Amplification Tests (NAATs)
Nucleic Acid Amplification Tests (NAATs) is the suggested test type for diagnosing chlamydia trochomatis (chlamydia) and N. gonorrhoeae. If the test is negative for sexually transmitted infections, it doesn't mean they can't cause PID. Therefore, gynaecology should consider the possibility of other organisms when diagnosing PID.
Endometrial biopsy
Gynaecologists performs a procedure called endometrial biopsy to examine the abnormalities of the uterus and to diagnose the diseases such as endometrial cancer, fertility and abnormal uterine bleeding. During the process, a thin, flexible tube called a pipeline (consisting of a small tube inside) is inserted through the cervix and into the uterus. The gynaecologist moves the pipeline back and forth to get a biopsy (tissue) sample from the uterus for laboratory evaluation.
It is an excellent alternative to laparoscopy, and helpful in examining the PID. It may show the presence of neutrophils and plasma cells in endometrial tissue, suggesting endometritis, a sign of PID. Likewise, it is suggested to diagnose the early cases that are not yet visible at laparoscopy.
Culdocentesis
Culdocentesis is a medical technique that examines the abnormal fluid behind the vagina and uterus. It is performed to remove fluid from behind the vagina (This area is called the cul-de-sac) and to test it for infection. It is performed by inserting a surgical instrument to lift the cervix and inserting a thin needle through the wall of the vagina below the cervix. The needle consists of a syringe to collect a fluid sample from the posterior cul-de-sac through the needle. It is used to diagnose ectopic pregnancy, ruptured
ovarian cysts, tubal infection.
Pelvic Inflammatory Disease (PID) Treatment
Treatment of Pelvic inflammatory disease includes antibiotics to fight against a broad spectrum of possible infectious organisms.
Antibiotics are the primary treatment for pelvic inflammatory disease, completing the antibiotics course is extremely important to reduce PID. Antibiotic treatment depends on the causative organism. For instance, patients receive a different treatment for gonorrhoea or chlamydia. The antibiotic therapy must have a wide scope, be efficient against N. gonorrhoea, C. trachomatis, and anaerobic organisms (Bacteroides fragilis).
If the patient has mild pelvic inflammatory disease (Acute PID treatment)
The gynaecologist will give an antibiotic shot
- The patient will send home with a prescription for antibiotic drugs to take for two weeks
- The patient must follow up closely with a gynaecologist to prevent the re-occurrence.
If the patient has more severe Pelvic inflammatory disease (Chronic PID treatment)
- Patients may need a hospital stay, and intravenous antibiotics are injected through a vein (intravenously).
In addition to antibiotics, anti-inflammatory and analgesic drugs can be recommended to decrease the symptoms. Improvement will occur within up to three days from the beginning of the antibiotic treatment.
Usually, gynaecologists recommend avoidance of sexual intercourse for 30 days and usage of condoms during intercourse after this time period. It is necessary and vital to practice safe sex to prevent the risk of getting infections, which may lead to Pelvic inflammatory disease. If the patient got PID by sexually transmitted infections (STIs) such as gonorrhoea or chlamydia, the patient's partner must also be treated.
Any injury or harm to the female reproductive tract that is induced due to pelvic inflammatory disease is often irreversible (not reversible). The most serious condition of pelvic inflammatory disease (PID) is the formation (collection) of a tubo-ovarian abscess, which can progress into sepsis and death if not diagnosed and treated early. So, early diagnosis and treatment are crucial in preventing scar tissue formation.
The cure involves eradicating signs and symptoms and regularising inflammation markers in lab tests. The goal of treatment is to manage the infection, lessen the tubal damage, and prevent adhesions and reoccurrence of PID.
Hospitalisation may be required in the following cases:
Surgical emergencies (appendicitis), pregnancy, tubo-ovarian abscess, severe nausea/vomiting or increased body temperature > 38°C, inability to take antibiotics, no response to oral or intramuscular medication after 72 hours of therapy, and the diagnosis is uncertain.
Surgical management of pelvic inflammatory disease
The choice of pelvic inflammatory disease surgery is based on the size of the abscess and effectiveness of antibiotics therapy, as antibiotics are the first-line treatment for pelvic inflammatory disease. Surgery might be required for severe complications like spreading infection or a burst (ruptured) abscess in the fallopian tube or ovary.
Surgical treatment involves:
A salpingo-oophorectomy is called the surgical removal of fallopian tubes and ovaries, and it involves two techniques.
Salpingectomy: Surgical removal of fallopian tube or tubes (used to treat ectopic pregnancy)
Oophorectomy: A surgical procedure that consists of the removal of the ovary or ovaries.
- Unilateral salpingo-oophorectomy: Surgical removal of one fallopian tube and ovary on the same side and sharing a blood supply. It is done for the patients who are planning to conceive in the future.
- Bilateral salpingo-oophorectomy: This is an option to remove both the ovaries and fallopian tubes.
- Hysterectomy: Based on the reasons for the surgery, salpingo-oophorectomy is periodically combined with hysterectomy (Surgical removal of uterus). A hysterectomy to remove the uterus and fallopian tubes will be suggested if the infection is severe and a woman no longer wants to conceive.
Surgical removal of ovaries is a rarely recommended process for pelvic inflammatory disease. Sometimes, specifically when there is a reoccurrence, removal of the fallopian tube (salpingectomy) or even an ovary (oophorectomy) may be required to prevent the flaring up of the disease.
This surgical treatment can be performed by using the following procedures:
- Open abdominal surgery: One technique of performing a salpingo-oophorectomy is via open abdominal surgery. During the process, one or both ovaries and fallopian tubes are removed through a large incision in the abdomen.
- Laparoscopic surgery: It is a minimally(small) invasive method to do salpingo-oophorectomy. This method uses small abdominal incisions and inserts the laparoscope (thin tube with light and camera) into the abdomen, helping the gynaecologist guide the targeted area with the pictures projected on the monitor. The gynaec surgeon detaches the ovary and fallopian tube through the small incisions.
Pelvic Inflammatory Disease (PID) Treatment Cost in Hyderabad, India
The cost of Pelvic Inflammatory Disease (PID) treatment in Hyderabad typically ranges between ₹25,000 to ₹2,80,000 (~US$300 to US$3,360). The total treatment expense depends on multiple factors such as:
- The patient’s overall health condition
- Severity and extent of infection
- Need for hospitalization or emergency care
- Diagnostic investigations (e.g., ultrasound, cultures, blood work)
- Choice between medical or surgical treatment
- The surgeon’s experience and specialization
- Insurance or corporate health plan coverage
- Hospital infrastructure and room category
Estimated Cost Breakdown by Pelvic Inflammatory Disease (PID) Treatment Type
Non-Surgical Treatment (Antibiotic Therapy): ₹25,000 to ₹60,000 (~US$300 to US$720)
Includes:
- Specialist consultation
- Pelvic ultrasound and blood tests
- Outpatient antibiotic treatment
- Follow-up care and infection monitoring
Surgical Treatment Options
In severe or recurrent cases of PID where medical therapy fails, minimally invasive surgical intervention may be recommended:
- Laparoscopic Salpingectomy or Abscess Drainage: ₹1,45,000 to ₹2,00,000 (~US$1,740 to US$2,400)
- Laparoscopic or Abdominal Hysterectomy: ₹2,00,000 to ₹2,80,000 (~US$2,400 to US$3,360)
At PACE Hospitals, we offer a comprehensive approach to PID treatment—from advanced diagnostics and outpatient management to laparoscopic surgical interventions when necessary—ensuring affordable, precise, and patient-centric care.
Frequently Asked Questions (FAQs) on PID Treatment
What causes PID?
Pelvic inflammatory disease is commonly caused by sexually transmitted infections such as chlamydia and gonorrhoea. Chlamydia trachomatis (chlamydia) is the most typical STI (sexually transmitted infection) in many developed countries and has been found in almost 30% of all pelvic inflammatory disease cases. Other vaginal bacteria also can cause this condition. These bacteria can spread through unprotected sex.
Which Is the best hospital for PID Treatment in Hyderabad, India?
PACE Hospitals, Hyderabad, is one of the most trusted centres for diagnosing and treating Pelvic Inflammatory Disease, offering comprehensive gynecological care supported by advanced diagnostic facilities.
We are having expert gynecologists, infectious disease specialists, radiologists, and women’s health teams to provide advanced treatment for:
Acute Pelvic Inflammatory Disease
Chronic PID
PID-related pelvic pain
Recurrent vaginal or cervical infections
Fallopian tube inflammation
PID linked to sexually transmitted infections
Complications such as tubo-ovarian abscess
With high-resolution pelvic ultrasound, advanced laboratory testing, targeted antibiotic therapy, fertility-preserving treatment, pain management, and 24/7 emergency care, PACE Hospitals ensures accurate diagnosis, effective treatment, and long-term recovery — supported by cashless insurance, TPA tie-ups, and complete documentation support.
Does PID affect menstrual cycle?
Yes, PID can affect the menstrual cycle. This infection can cause heavy bleeding, irregular periods, cramps and bleeding between menstrual periods. If untreated, it can lead to long-term complications such as scarring and blockages in the fallopian tubes or ovaries, which can lead to ectopic pregnancy (one of the causes of missed periods).
Can a virgin get PID?
Yes, a virgin can also develops PID condition, as PID is not always due to sexually transmitted infections. It can develop from normal bacteria that are found in the vagina due to douching.
However, it is rare in virgins (sexually inactive females). While it is common in sexually active women. Sexual activity is the primary way to transmit sexually transmitted diseases, which can lead to this condition.
Is PID contagious?
Yes, it is contagious because it can spread through sexual contact. It first enters through the lower genital tract (vulva and vagina) and moves upward to the upper genital tract such as the uterus, fallopian tubes or ovaries. Sexual activity is the primary way to transmit sexually transmitted diseases, which can lead to this condition. Some STIs can spread from mother to baby before and during childbirth.
What Is the cost of PID Treatment at PACE Hospitals, Hyderabad?
At PACE Hospitals, Hyderabad, the cost of pelvic inflammatory disease treatment typically ranges from ₹900 to ₹28,000 and above (approx. US $11 – US $340), making it an affordable and specialised option for women’s reproductive health. However, the final cost depends on:
- Severity of pelvic infection (mild, moderate, severe)
- Required investigations (blood tests, STI screening, ultrasound)
- Type of antibiotics (oral vs. IV)
- Need for hospitalization
- Presence of complications (abscess, severe pelvic pain)
- Associated conditions (PCOS, endometriosis, infertility concerns)
- Follow-up evaluation and imaging
Mild to moderate PID treated with oral antibiotics falls in the lower range, while severe PID requiring IV antibiotics or laparoscopic evaluation falls toward the higher range.
After consultation, imaging, and laboratory evaluation, our gynecology team provides a personalised treatment plan and a transparent cost estimate based on your condition.
Can PID cause infertility?
Yes, it can cause Infertility. According to research, 1 in 10 females with PID become infertile. Pelvic inflammatory conditions can cause scarring of the fallopian tubes that block the tubes and prevent egg fertilization, which leads to difficulty conceiving.
What is the best treatment for pelvic inflammatory disease (PID)?
The best treatment for pelvic inflammatory disease (PID) involves early and appropriate antibiotic therapy, selected based on the severity of the infection and clinical presentation. Treatment typically includes a combination of broad-spectrum antimicrobial categories that target the most common organisms associated with PID, including sexually transmitted and anaerobic bacteria.
Most mild to moderate cases can be managed with outpatient antibiotic therapy, while severe cases, pregnancy, lack of response to oral treatment, or complications such as abscess formation may require hospital-based (inpatient) treatment with intravenous antibiotics. In addition to antimicrobial management, patients are advised to avoid sexual activity until treatment is completed, ensure that sexual partners are evaluated and treated, and attend follow-up assessments to confirm clinical improvement and reduce the risk of long-term complications such as infertility or chronic pelvic pain.
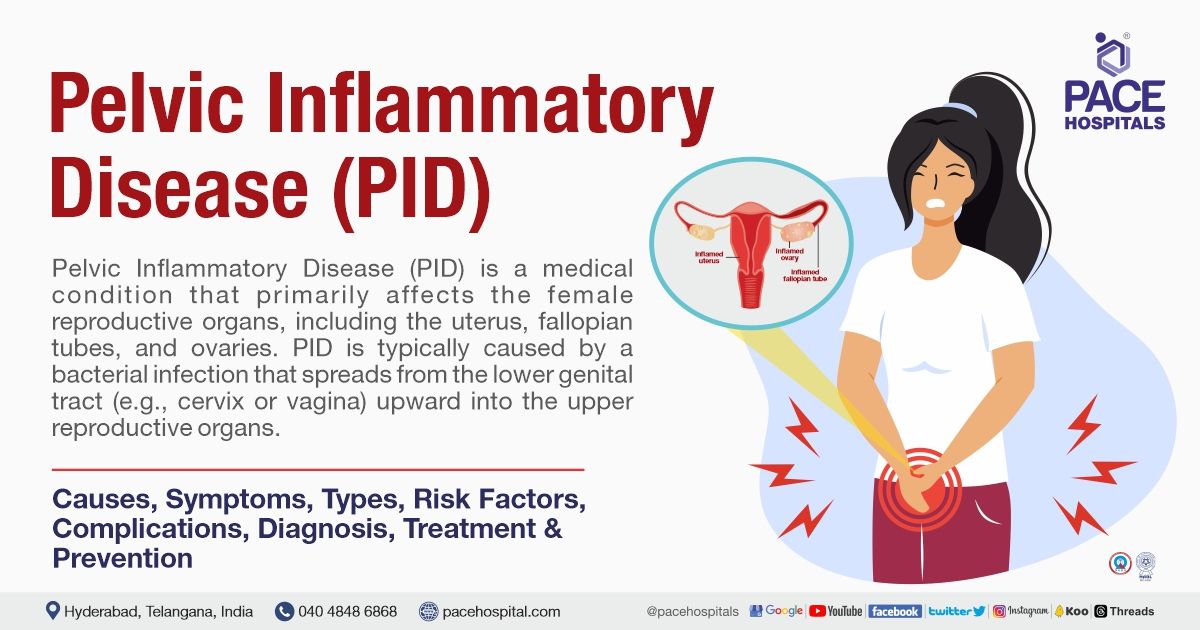
What is PID?
Pelvic inflammatory disease (PID) is an infection that occurs in the female reproductive organs such as the uterus, ovaries or fallopian tubes. Untreated sexually transmitted diseases (STDs) can cause PID. It can also be caused by infections that are not sexually transmitted in nature.
This condition is commonly seen in women aged 15 to 25 years. Over the past decade, the incidence of PID has decreased due to more women getting tested regularly for bacteria infections. However, it is still often seen in both outpatient clinics and emergency departments.
What is PID in medical terms?
PID stands for Pelvic inflammatory disease, a common condition affecting the female reproductive organs such as the fallopian tubes, ovaries and womb (uterus). If untreated, it leads to complications such as ectopic pregnancy (fertilized egg grows outside of the uterus), infertility (difficulty in conceiving) and chronic pelvic pain.
How long does it take for PID to develop?
PID caused by chlamydia or gonorrhoea can develop within a few days to a few weeks if untreated. If some other organisms cause PID, then it may take several months to develop this condition.
What are the symptoms of PID in a female?
Most infected women may show mild symptoms or not experience any symptoms (asymptomatic). However, the possible symptoms include:
- Pain in the lower abdomen (most common symptom)
- Increased temperature
- Painful sex
- Painful urination
- Unusual vaginal discharge with a foul odor
- Bleeding between menstrual periods
- Heavy and painful periods
- Nausea and vomiting
Can PID cause missed period?
No, Pelvic inflammatory disease (PID) cannot cause missed periods directly. However, PID can affect the menstrual cycle. This infection can cause bleeding between menstrual periods and sometimes causes heavy bleeding, irregular periods, and cramps. If untreated, it can lead to long-term complications such as scarring and blockages in fallopian tubes or ovaries, which can leads to ectopic pregnancy (one of the causes of missed periods).
Can PID cause HIV?
No, Pelvic inflammatory disease does not cause HIV infection. Women with PID have a higher risk of developing human immunodeficiency virus (HIV) than women without a history of PID.
PID can cause damage to a woman's reproductive organs, making it easier for HIV to enter the body during sex. PID patients are advised to test for other sexually transmitted diseases and be educated on the practice of safe sex to avoid transferring germs.
Does PID occur in males?
No, it is not possible to get pelvic inflammatory disease in men because it is an infection that affects the woman's reproductive organs, such as the uterus, fallopian tubes or ovaries. It affects only females and develops when bacteria from the vagina move from lower to upper reproductive organs during sexual contact.
However, men cannot have pelvic inflammatory disease, and they are the silent carriers of bacteria and transmit them to females during unprotected sexual intercourse. Men can still contract sexually transmitted infections, including urethritis, prostatitis or orchitis.
What is a pelvic infection?
Pelvic infection is a medical condition that usually affects females and is often clinically presented with pelvic pain, fever and foul vaginal discharge.
Pelvic infections are categorised into two types.
- Pelvic inflammatory disease: Includes upper infectious diseases such as endometritis, tubo-ovarian abscess, salpingitis, and hydrosalpinx.
- Infections occurring in specific, particular contexts: During the post-abortion period or postpartum.
Woman can get pregnant with PID?
Yes, a woman can become pregnant with PID. However, the chances of getting pregnant are lower in women who have had PID (especially more than once) than in women without PID.
This is due to the entrance of bacteria into the fallopian tubes and causing damage, leading to the formation of scar tissue. Scar tissue can obstruct the egg from travelling down the fallopian tube to the uterus, thereby preventing fertilization. Over time, this scar tissue can cause ectopic pregnancy (pregnancy occurs outside the uterus) instead of inside the uterus. Ectopic pregnancies can end in miscarriage.
Does PID cause joint pain?
No, Pelvic inflammatory disease cannot cause joint pain. However, it can cause lower abdominal pain or lower back pain that may radiate to the legs, which can be challenging to manage. If not treated early, PID can lead to severe long-term complications. So, it is essential to seek medical help if one can experience any symptoms.
What STD can cause pelvic inflammatory disease?
Chlamydia and gonorrhoeae are the bacteria that primarily cause PID. Other Sexually transmitted infections include Mycoplasma genitalium, Trichomoniasis and herpes simplex virus (HSV). Practice safe sex to avoid developing this condition and get regular STI screenings.