Arthritis - Symptoms, Types, Causes, Risk Factors, Complications
PACE Hospitals
Overview | Prevalence | Types | Symptoms | Causes | Risk Factors | Complications | Diagnosis | Treatment | Prevention | FAQs | When to consult a Doctor
Arthritis meaning
Arthritis is a Greek word that means "disease of the joints". Traditionally, arthritis is a condition characterised by joint inflammation. Inflammation implies redness and swelling in the joints. Moreover, this inflammation will also affect the tendons and ligaments surrounding the joints. Arthritis is usually associated with pain, inflammation, limited motion and joint stiffness. There are more than 100 types of arthritis conditions, and knee arthritis is commonly seen in more cases.
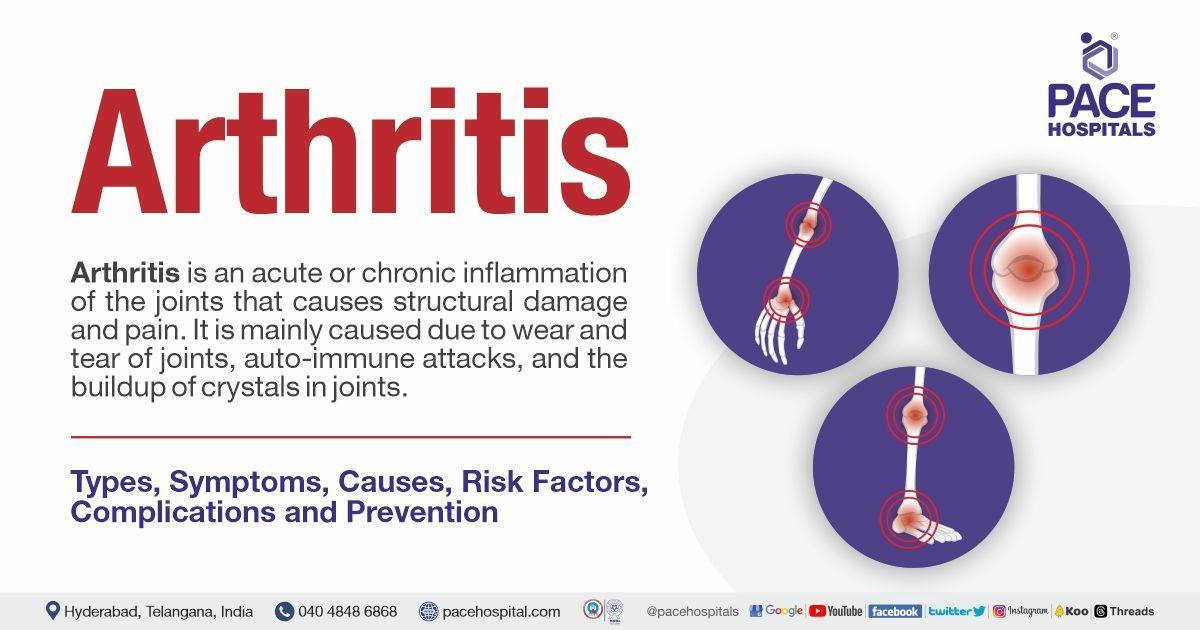
Arthritis definition
The term arthritis is defined as an acute or chronic inflammation of the joints that often accompanies structural damage and pain. The term "arthritis" actually refers to joint inflammation. Joints are the sites where the two bones adjoin, namely the elbow or knee.
What is Arthritis Disease?
The term "arthritis" is often called inflammation of the joints. The joint is the part of the body where two or more bones meet together to allow movement, such as elbows and knees. There are different types of arthritis conditions with different causes and specific treatments. The symptoms of arthritis include redness, pain, swelling, and joint heat. In some arthritis cases, it also affects the heart, eyes, and skin.
Arthritis conditions are mainly caused due to wear and tear of joints, auto-immune attacks, and the buildup of crystals in joints. In addition, gender, age, weight, hereditary factors, injuries, and infections also lead to arthritis. The most commonly affected areas by arthritis are the knees, hips, feet, hands, and lower back.
Prevalence of Arthritis Disease
Women are more likely than males to experience it. Women experience arthritis and other rheumatic disorders more frequently than males do. Arthritis conditions are frequently connected to ageing; as people grow older, they occur more frequently. However, people of all ages may be impacted by arthritis.
Types of Arthritis Disease
There are more than 100 types of arthritis conditions with specific causes and different treatments. Out of those, some of the common arthritis types include:
- Osteoarthritis: Osteoarthritis is the most common form of arthritis that develops slowly and most frequently during the middle and older ages. In this condition, the cartilage that cushions and shields the ends of the bones gradually wears away, causing osteoarthritis. Osteoarthritis (OA) is also called as wear and tear arthritis. This condition results in discomfort and stiffness that gets worse over time, making it challenging to do daily tasks.
- Rheumatoid arthritis: Rheumatoid arthritis (RA) is a long-lasting autoimmune disease that initially affects the joints in the body. It is the second-most common form of the arthritis condition. Rheumatoid arthritis arises if the person's immune system cannot protect the body from diseases and infections. In this condition, the immune system attacks its tissues, finally resulting in symptoms such as swelling, pain, loss of joint function, and stiffness.
- Gouty arthritis: Gout is an inflammatory arthritis characterised by swelling and joint pain that lasts one to two weeks and then resolves. Gout flares commonly occur in the big toe or lower limb. Gouty arthritis is caused by high levels of serum uric acid deposits in the body (hyperuricemia). This serum uric acid deposits as needle-shaped crystals around the joint, resulting in inflammation and arthritis. Usually, this happens when the body produces too much uric acid.
- Juvenile arthritis (JA), or Juvenile idiopathic arthritis (JIA), or Juvenile rheumatoid arthritis (JRA): Juvenile arthritis is a chronic type of arthritis that is commonly developed in children. Juvenile arthritis is associated with inflammation, resulting in joint pain, warmth, swelling, stiffness, and loss of motion. There are various forms of juvenile arthritis involving different patterns or features with inflammation of other parts besides the joints. It lasts for a limited time, usually a few months or years. However, in some cases, it may require lifelong treatment.
- Ankylosing spondylitis: Ankylosing spondylitis is an arthritis condition accompanied by inflammation of the joints and ligaments in the spine. Ankylosing spondylitis may also affect the peripheral joints, such as the knees, hips, and ankles. Usually, the joints and ligaments of the spine play a key role in moving and bending. Individuals affected by ankylosing spondylitis might develop stiffness in joints and tissues. This condition might lead to vertebrae fusing in some complicated cases, resulting in a rigid and inflexible spine.
- Lupus (systemic lupus erythematosus): Lupus is a long-lasting disease affecting numerous body parts. This condition arises if the person's immune system cannot protect the body from diseases and infections. In these circumstances, the immune system attacks its own tissues, resulting in inflammation and permanent tissue damage (in rare cases). This condition can also be widespread in the skin, joints, lungs, kidneys, heart, circulation, and brain.
- Psoriatic arthritis (PsA): It is an inflammatory condition that affects the joints, especially at the sites where the tendons and ligaments adhere to the bones. It is caused by an overactive immune system, which leads to pain and swelling. Psoriatic arthritis is usually developed in patients who already have psoriasis.
- Fibromyalgia: Fibromyalgia is a long-lasting disorder that primarily causes pain and tenderness all over the body. In addition to this, it also causes fatigue and trouble sleeping. There needs to be a clear understanding regarding this condition among researchers and scientists. There is no cure for fibromyalgia, but arthritis doctors might suggest a combination of exercises, movement therapies, psychological therapies, behavioural therapies, and arthritis medicines to treat this condition's symptoms.
- Reactive arthritis (ReA): As mentioned, the name reactive arthritis indicates that an infectious reaction usually causes the condition. This condition progresses due to a bacterial infection in the urinary, genital, or digestive tract. The symptoms of this condition include inflammation in the eyes, urinary tract, or genitals. Every individual might not get these three symptoms simultaneously or combined.
- Septic arthritis (SA): Septic arthritis is a serious bacterial joint inflammation caused primarily by bacterial pathogens but occasionally by fungal, mycobacterial, viral, or other uncommon pathogens. This condition is usually monoarticular, involving one large joint, such as the hip or knee. However, this might be polyarticular, involving multiple joints in some cases. Septic arthritis is an orthopaedic emergency requiring immediate treatment to reduce morbidity and mortality.
- Arthritis in knee: Knee arthritis is a condition characterised by swelling, pain, and joint stiffness. It is commonly seen in the knees; knee arthritis affects the largest joints. Knee arthritis can be serious and debilitating. The knee joint is where the thigh-bone, shin-bone, and patella meet.
- Seronegative arthritis: It is especially indicated for rheumatoid arthritis. A serology test usually gives results regarding the rheumatoid factor (RF) and citrullinated peptides (CCP). The significance of seronegative arthritis means that people with symptoms of rheumatoid arthritis test negative for RF and CCP in their blood.
Most arthritis conditions occur through these principle mechanisms:
- Inflammation: Inflammation is the body's normal healing mechanism that occurs to fight against bacterial, viral, or other reactions. There is no specific reason for inflammation; it responds to injuries. The inflammation results in swelling, pain, and stiffness in the joints. Some of the inflammatory arthritis conditions are rheumatoid arthritis, reactive arthritis, ankylosing spondylitis and psoriatic arthritis.
- Degeneration: Degeneration of cartilage leads to degenerative arthritis. The main role of cartilage is to cover the ends of the bones and to glide or move the joints. Degeneration of the cartilage leads to osteoarthritis.
- Connective tissue diseases: Connective tissues include ligaments, tendons, and cartilage. These tissues give support to the body's tissues and organs. Connective tissue diseases cause inflammation in the tissues of muscles, skin, lungs, and kidneys, resulting in joint pain and swelling. Some of the connective tissue diseases are lupus, scleroderma, etc.
- Infections: Infections such as bacterial, viral, or fungal may lead to joint inflammation. Infections may be acute or chronic (long-lasting), i.e., irreversible joint inflammation. In rare conditions, it may lead to septic arthritis, which requires immediate medical attention.
- Metabolism: Metabolic imbalances in uric acid lead to gout. In this situation, high levels of uric acid (hyperuricemia) get deposited around the joints, which leads to inflammation. e.g., gouty arthritis.
Arthritis Symptoms
The signs and symptoms of arthritis include:
- Pain: Arthritis pain may be intermittent (come and go) or persistent (constant)
- Swelling: Usually, in arthritis conditions, joints become swollen and feel warm or tender to the touch
- Tenderness (pain upon touch)
- Loss of function (decreased range of motion)
- Stiffness: Stiffness is seen in the morning or else upon sitting or performing exercises
- Deformity (joints become deformed)
- Weakness
- Instability
- Erythema (redness)
- Warmth
- Sleep disturbances, fatigue, emotional liability, and systemic illnesses may accompany the above symptoms. These symptoms are usually seen in one or more joints
- Morning stiffness, swelling, tenderness, warmth, effusion, and erythema are seen in inflammatory and osteoarthritic conditions
- Morning stiffness and overall body pain are seen in patients with fibromyalgia
- In addition to the common symptoms, fever and a low red blood cell count are seen in rheumatoid arthritis
Arthritis Disease Causes
The cause depends on the type of arthritis condition. Some of the common causes of arthritis include:
- Wear and tear of joints due to erosion or overuse
- Autoimmune attack (rheumatoid arthritis, lupus, and scleroderma)
- Abnormal metabolism - Hyperuricemia (gouty arthritis)
- Injuries due to accidents or sporting activities
- Infections
- Degeneration of joints
- Jobs with repeated stress on the joints
- Muscle weakness
- Being overweight
Arthritis Risk Factors
The risk factors might differ based on the type of arthritis condition. The common risk factors for arthritis include:
- Age: Most people gain fat and lose muscle mass as they get older, which could modify the amount of pressure placed on joints and increase the progression of arthritis.
- Obesity: Studies have shown that excess weight overloads the joints and destroys the articular cartilage.
- Gender: Women get changes in oestrogen levels after menopause; these hormones affect cushioning cartilage, which allows joint movements. In addition to this, hormonal changes lead to low mineral density and cause arthritis conditions.
- Heredity or genes: Studies have shown that HLA-B27 causes ankylosing spondylitis (spondylitis arthritis), whereas HLA-DRB1 causes rheumatoid arthritis. Thus, human leukocyte antigen (HLA) plays a significant role in developing arthritis conditions.
- Environmental factors: Factors such as sporting activities, job roles, and exercises that require frequent use of joints play a significant role in developing arthritis conditions. These activities are associated with the overuse or repetitive use of joints.
- Autoimmune disorders: In some cases, the person's immune system attacks their own cells or tissues because it mistakenly assumes they are foreign cells. This condition leads to autoimmune arthritis conditions such as rheumatoid arthritis, lupus, etc.
- Injuries: Injuries due to accidents, sporting activities, etc., may lead to the damage to joints, which in turn develops inflammation and causes arthritis conditions.
- Infections: When an infection spreads to one or more of the joints and causes inflammation, infectious arthritis results. The synovial fluid that lubricate the joints and the surface of the cartilage is inflamed. The infection, which typically originates from another area of the body and spreads to the joint through the bloodstream, may be caused by bacteria, a virus, or a fungus.
Complications of Arthritis Disease
If the arthritis is left untreated, it may lead to the following complications, such as:
- Metabolic disorders: Arthritis conditions associated with overweight might increase the chance of developing conditions such as hypertension, high cholesterol, type-2 diabetes, and heart diseases.
- Loss of mobility: Progression in arthritis might lead to decreased mobility for an individual, especially in daily activities.
- Weight gain: The individuals may gain weight due to a lack of exercise for arthritis and decreased movements.
- Spreading of inflammation: In autoimmune arthritis conditions, the inflammation may spread to the eyes, skin, lungs, and blood vessels.
- Psychological health: Arthritis may increase the risk of depression and anxiety due to inflammation, chronic pain and loneliness.
- Increased risk of falls: People with arthritis may experience fractures due to muscle weakness.
- Quality of life: Due to inflammation and pain in arthritis patients, they may develop problems such as insomnia (issues with sleep), depression, fatigue, and anxiety.
Arthritis Diagnosis
Usually, a diagnosis is required to confirm the condition. Doctors might suggest various diagnostic approaches to the patient based on the medical history and symptoms. The diagnostic approaches for arthritis are as follows:
- Physical examination
- Blood tests - Blood test for arthritis include:
- Complete blood count
- Serum creatinine
- Haematocrit
- Anti-nuclear antibody (ANA) test
- Uric acid
- Rheumatoid factor (RF) and CCP (cyclic citrullinated peptide) antibody test
- White blood cell (WBC) count etc.
- Joint aspiration (arthrocentesis)
- HLA tissue typing
- Urine test
- Muscle and skin biopsies
- Bone X-ray (radiography)
- Synovial fluid analysis
- C- reactive protein (CRP) test
- Musculoskeletal MRI (magnetic resonance imaging scan)
- Direct arthrography
- Ultrasound
- CT (computed tomography) scan
Note: The above diagnostic approaches are for different types of arthritis; based on the patient's condition and symptoms, the doctor might suggest a specific diagnostic approach related to the patient's arthritis condition.
Arthritis Treatment
Treatment for arthritis includes:
- Conservative or non-surgical treatment
- Surgical treatment
1. Conservative or non-surgical treatment
- Lifestyle modifications
- Home remedies for arthritis
- Physical therapy
- Occupational therapy
- Heat and cold therapy using the ideal pads
- Massage therapies
- Assistive devices such as Transcutaneous electrical nerve stimulation (TENS), braces and splints
- Medications such as Analgesics, Corticosteroids’, Disease-modifying antirheumatic drugs (DMARDs), Biologics, Counterirritants, Non-steroidal anti-inflammatory drugs (NSAIDs), Immunosuppressants, Visco supplements, etc.
2. Surgical treatment
- Arthroscopy
- Joint replacement
- Cartilage grafting
- Joint fusion
- Synovectomy
- Osteotomy
- Total joint replacement (TJR) that includes knee replacement, shoulder replacement, ankle, and hip replacement
Note: The above treatment approaches are for different types of arthritis; based on the patient's condition and symptoms, the
orthopedic doctor
might suggest a specific treatment approach related to the patient's arthritis condition.
Why Choose PACE Hospitals?
Expert Super Specialist Doctors
Advanced Diagnostics & Treatment
Affordable & Transparent Care
24x7 Emergency & ICU Support
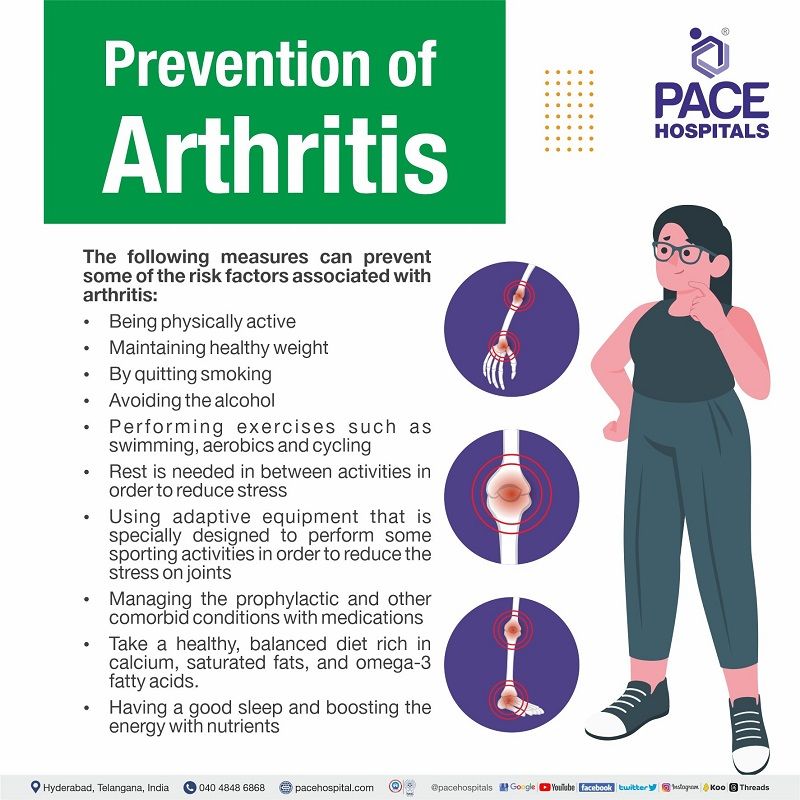
Arthritis Prevention
Usually, there is no arthritis cure; doctors give treatment to help the patient get relief from the condition (arthritis pain relief). Surgeries might be suggested in some cases, but some risk factors, such as age and heredity, can't be prevented. The following measures can prevent some of the risk factors associated with arthritis:
- Being physically active
- Maintaining healthy weight
- By quitting smoking
- Avoiding the alcohol
- Performing exercises such as swimming, aerobics and cycling
- Rest is needed in between activities in order to reduce stress
- Using adaptive equipment that is specially designed to perform some sporting activities in order to reduce the stress on joints
- Managing the prophylactic and other comorbid conditions with medications
- Take a healthy, balanced diet rich in calcium, saturated fats, and omega-3 fatty acids
- Having a good sleep and boosting the energy with nutrients
Frequently Asked Questions (FAQs) on Arthritis Disease
When to See a Doctor for Arthritis?
Arthritis affects how joints function, making them painful, stiff, or swollen and more challenging to move. It doesn’t affect only older adults—there are many types, ranging from age-related joint wear to immune system–related joint conditions.
Key warning signs:
- Ongoing joint pain that continues for several weeks
- Morning stiffness or stiffness after periods of relaxation
- Swelling or redness around joints
- Joint mobility issues or decreased range of motion
- Pain that worsens with activity or affects daily tasks
- Fatigue, weakness, or low-grade fever
If joint symptoms interfere with daily life, worsen gradually, or are accompanied by swelling and stiffness, it is essential to consult a rheumatologist or an arthritis doctor promptly.
Share on
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868