Ectopic Pregnancy: Causes, Symptoms, Types and Treatment
Pace Hospitals
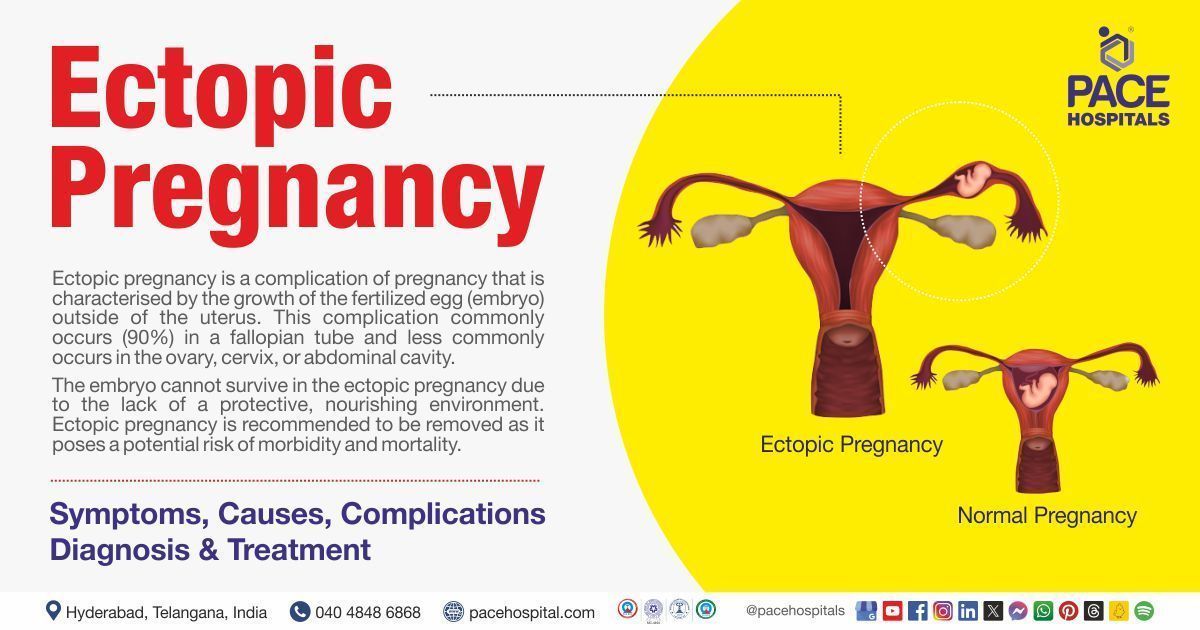
Ectopic pregnancy definition
Ectopic pregnancy is a complication of the pregnancy that is characterised by the growth of the fertilized egg (embryo) outside of the uterus. This complication commonly occurs (90%) in a fallopian tube and less commonly occurs in the ovary, cervix, or abdominal cavity.
In a healthy pregnancy, the embryo implants itself in the uterus, but in ectopic pregnancy, the embryo implants outside of the uterus. This fertilized egg (embryo) cannot survive due to the lack of a protective, nourishing environment like the uterus. However, it may continue to develop for several months, causing the tube to rupture (burst) and lead to haemorrhage (internal bleeding), which can be a life-threatening emergency that requires immediate surgery.
Ectopic pregnancy meaning
Ectopic pregnancy explains the meaning of pregnancy away from the original place, where the word "ectopic" comes from the modern Latin from the Greek "ektopos," which means "away from a place, distant, or morbid displacement of parts." The word "pregnancy" comes from the French "pregnacion" and Latin "praegnationem" which means "state of a female who has conceived or is with child".
Types of Ectopic Pregnancy
Ectopic pregnancies are categorized based on their location. The following are the different types of ectopic pregnancies:
- Tubal ectopic pregnancy: Fertilized egg implants in the fallopian tube, 75% occur at ampullary segment.
- Interstitial ectopic pregnancy: A fertilized egg attaches to the fallopian tube's interstitial portion (narrow portion).
- Caesarean scar ectopic pregnancy (CSP): A gestational sac implants into the front wall of the lower part of the uterus (anterior uterine wall of the lower uterine segment), where a caesarean scar from a prior surgery resides.
- Heterotopic ectopic pregnancy: It is a condition of pregnancy in which both intrauterine (inside the uterus) and extrauterine (outside the uterus) occur simultaneously.
- Cervical ectopic pregnancy: In this ectopic pregnancy, gestational sac implants in the mucosa of the endocervical canal (mucous lining of the cervix canal). It has a high complication rate; however, it also has a high success rate in treatment.
- Ovarian ectopic pregnancy: Gestational sac implants in the ovaries, 81% of these ectopic pregnancies are associated with concomitant intrauterine devices.
- Abdominal ectopic pregnancy: It occurs when the gestational sac implants in the peritoneal cavity of the abdomen (space within the abdomen that contains most of the abdominal organs). There are few reported cases of term deliveries of healthy babies.
- Cornual ectopic pregnancy: It is also a rare form of ectopic pregnancy, where a fertilized egg implants in the rudimentary horn (horn-like part) of the uterus. It may or may not communicate with the uterine cavity.
Prevalence of Ectopic Pregnancy
Ectopic pregnancy is the primary cause of pregnancy-related fatalities during the first trimester and is accountable for high rates of morbidity and mortality; if not recognized and treated promptly, it occurs in 1.9% of reported pregnancies.
The estimated rate of ectopic pregnancy in the general woman is around 1 to 2 out of every 100 ectopic pregnancies. The risk is higher by 2 to 5% among patients who undergo fertility treatments.
Ectopic pregnancies occurring outside of the fallopian tube account for less than 10% of all ectopic pregnancies. Around 4% of all ectopic pregnancies make up the scar tissue from the cesarean section and occur 1 in 500 pregnancies in women who underwent at least one prior cesarean section.
Another rare type of ectopic pregnancy called interstitial ectopic pregnancy, where the embryo of the woman implants deep within the uterine wall, is accountable for 4% of all ectopic implantation sites and has high risks and complications with mortality rates up to 7 times higher than compared to other ectopic pregnancies due to the high rate of bleeding.
Ectopic pregnancies in the abdominal cavity account for 1.3% of all cases. In some cases, they also exist in the spleen, liver, and retroperitoneum.
As per the Indian studies, it was found that prevalence of ectopic pregnancies range from 1-2%. It is commonly seen in the age group between 18 to 38.
Ectopic Pregnancy Causes
Reasons for ectopic pregnancy may depend on several factors. The fallopian tubes are the muscular ducts that connect the ovaries to the uterus. Every month, a woman's ovary releases a mature egg. Fimbriae are finger-like projections at the end of the fallopian tube that sweeps the matured egg into the tube. The egg then waits in the tube to be fertilized.
After intercourse, fertilization occurs with the meeting of egg and sperm in one of the two tubes. A fertilized egg (embryo) travels through the fallopian tubes and reaches the uterus, where it grows and develops into a foetus.
This embryo usually spends 4-5 days in the fallopian tube before traveling to the uterus cavity, where it implants (attaches) 6-7 days after fertilization. This is the healthy normal physiology. In case of ectopic pregnancy, the embryo development is not seen in the uterus cavity.
The following are the possible causes for ectopic pregnancy:
- Damage to the fallopian tube: Any injury or damage to the fallopian tube may cause a narrowing or blockage, leading to the inability to deliver the embryo to the uterus, resulting in the embryo implanting in the tube lining.
- Hormonal imbalance: High estrogen and/or low progesterone levels may make the muscles tight in the fallopian tube, leading to the entrapment of the fertilized egg causing ectopic pregnancy.
- Malfunction of the uterus: In case of uterine malfunctions (abnormality in its shape and structure), such as the unicornuate uterus (congenital abnormality where a patient has an abnormally shaped uterine cavity and only one fallopian tube), can sometimes cause misplaced pregnancies, even in rare areas like the ovaries.
- Infection: Pelvic infections, such as sexually transmitted infections (STDs), may cause inflammation in the fallopian tubes and nearby organs, leading to ectopic pregnancy.
All these may impair the normal function of the tubes and result in a chronic ectopic pregnancy.
Ectopic Pregnancy Symptoms
Initially, a woman may feel the ectopic pregnancy as a normal pregnancy with similar signs and symptoms such as amenorrhea (absence of menstrual period), tender breasts, or an upset stomach.
The most common signs & symptoms of ectopic pregnancy include:
- Abdominal pain: The most common symptom of ectopic pregnancy is abdominal pain due to stretching. If the embryo implants in the fallopian tube, the thin wall of the fallopian tube will stretch, leading to pain in the lower abdomen and often vaginal bleeding. It may occur on one side. It may develop slowly, sharply, or worsen over several days and become severe.
- Vaginal bleeding: The woman may have some bleeding or spotting that is different from the normal menstrual period. This ectopic bleeding may be dark and watery, heavier or lighter than usual, and prolonged, which is different from a normal menstrual period.
- Mild cramping on one side of the pelvis.
- Low back pain
- Vague complaints such as nausea and vomiting
At this stage, it may be hard to find if the patient is experiencing a typical pregnancy or an ectopic pregnancy. The fertilized egg degenerates quickly in many cases of ectopic pregnancy. It breaks down in a woman's system either before the missed period or after experiencing some slight pain and bleeding.
Ectopic pregnancy may be diagnosed rarely in these cases, and it is assumed to be a miscarriage. There is no action required in these circumstances.
When unruptured, the signs and symptoms of an ectopic pregnancy are as same as that of a normal pregnancy. Nevertheless, the classic triad of symptoms of an ectopic pregnancy are abdominal pain, bleeding from vagina and amenorrhea (the absence of menstruation).
Signs and symptoms of ruptured ectopic pregnancy:
Rupture of the ectopic pregnancy may result in severe internal bleeding, shock, and, rarely, death of the woman. Symptoms of ruptured ectopic pregnancy may include as follows:
- Internal bleeding: As an ectopic pregnancy grows, it may become more severe because it can cause the tube to rupture. A rupture can cause major internal bleeding.
- Shoulder pain: Ruptured ectopic pregnancy may cause shoulder tip pain due to blood leaking into the diaphragm and is a sign that the condition is getting worse. This pain is always there and may worsen when the patient lies down.
- Weakness, dizziness, or fainting: Some women may feel weakness or dizziness due to internal bleeding.
- Collapse:
Some women may faint suddenly due to the loss of blood caused by a ruptured tube.
- Sudden, severe pain in the abdomen or pelvis: The patient may develop intense pain in the lower abdomen or pelvis area or may collapse if the rupturing of the fertilized egg happens in the fallopian tube and internal bleeding. However, in rare cases, collapse may be the very first indication of ectopic pregnancy.
- Upset tummy: The woman may experience diarrhoea or feel pain when opening their bowels.
Other signs of ectopic pregnancy include:
- Paleness of the skin
- Increased pulse rate
- Sickness
- Diarrhoea
- Falling blood pressure
Ectopic Pregnancy Risk Factors
Any woman of childbearing age could have an ectopic pregnancy. The following medical conditions may increase ectopic pregnancy in the woman.
- Advanced maternal age: In older women, fallopian tubes likely have relatively decreased function, which may delay the oocyte (embryo) transport.
- Prior ectopic pregnancies: Women with prior ectopic pregnancies have up to ten times the risk compared to the general woman (who doesn’t have any prior ectopic pregnancies).
- Smoking: Epidemiological studies revealed that cigarette smoking is a significant risk factor for tubal ectopic pregnancy, but the reason yet remains unclear.
- Tubal damage or tubal surgery: Surgery may lead to scarring or narrowing of the fallopian tubes, and a damaged fallopian tube may cause narrowing or blockage, making it difficult for the fertilized egg to pass through properly and increasing the risk of ectopic pregnancy.
- Prior pelvic infections: An increase in the number of pelvic infections is linked with an increase in the number of ectopic pregnancies. If the pelvic infections are undetected and untreated, the infection may increase the risk of pelvic inflammatory disease and ectopic pregnancy.
- Diethylstilbesterol (DES) exposure: Diethylstilbesterol exposure (endocrine-disrupting chemical) can increase the risk for many pregnancy-related issues, such as premature birth, miscarriage, and ectopic pregnancy.
- Intrauterine devices (IUD) use: Intrauterine devices (IUD) may irritate the fallopian tubes due to the insertion of the IUD in the uterine cavity, which may prevent the egg from going into the uterus. Sometimes, bacteria brought in through IUD insertion may cause fallopian tube infection, which raises the risk of ectopic pregnancy.
- Assisted reproductive technologies: Assisted reproductive technologies, such as in vitro fertilization (IVF) and embryo transfer (ET), are a well-known risk of ectopic pregnancy. Transfer of non-top-quality embryos is linked with a higher rate of ectopic pregnancy.
Complications of Ectopic Pregnancy
When the embryo implants in the fallopian tube, it cannot find enough space or room to grow or sufficient blood flow to keep it healthy. Afterward, ectopic pregnancy may cause the following complications:
- Rupturing of the ectopic pregnancy
- Haemorrhage (Severe bleeding)
- Shock (the body's compensatory responses to a sudden drop in blood pressure)
Ectopic Pregnancy Diagnosis
Diagnosis of ectopic pregnancy may be challenging to diagnose because the symptoms may often be mistaken for gastroenteritis, normal pregnancy, irritable bowel syndrome, miscarriage, or even appendicitis.
In cases of ectopic pregnancy, the pregnancy hormone is produced, resulting in a positive pregnancy test. Suppose a woman of reproductive age presents with symptoms such as missed periods, nausea or vomiting, vaginal bleeding, abdominal pain, syncope, or hypotension. Then, the gynecologist performs a pregnancy test.
- Medical history:
If a pregnancy test is positive, the gynecologist first identifies any risk factors for ectopic pregnancy in the patient's medical history, such as if a patient has had a prior confirmed ectopic pregnancy, known fallopian tube damage (due to the history of pelvic inflammatory disease, tubal surgery, obstruction), or achieved pregnancy through the use of infertility treatment. Gynaecologists conduct tests to detect ectopic or ruptured ectopic pregnancy.
- Examination: Then gynecologist do the vaginal examination.
- Blood tests: Blood tests will be performed to check the pregnancy hormone levels – beta human chorionic gonadotrophin (βhCG) because the levels usually lower and rise more slowly or stay the same in ectopic pregnancy.
- Urine pregnancy test: If the patient did not have a positive pregnancy test, then gynaecologist may take a urine sample to do the pregnancy test. If the test is negative, then the patient is very unlikely to have symptoms due to an ectopic pregnancy.
- Ultrasound scan: Transvaginal ultrasound is more accurate than a transabdominal scan in diagnosing ectopic pregnancies.
- Diagnostic laparoscopy: If the diagnosis is not precise by other tests, the gynae specialist prefers laparoscopy to look at the patient's pelvis.
Ectopic Pregnancy Treatment
Treatment options for ectopic pregnancy may include the following:
• Expectant management:
• Medical treatment
• Surgical treatment
Expectant management (wait and see):
Expectant management refers to close monitoring or watchful waiting by medical professionals rather than immediate treatment because, sometimes, ectopic pregnancies may end on their own, like a miscarriage.
Medical treatment (medical management of ectopic pregnancy):
In some cases, gynaecologists provide medical treatment for ectopic pregnancy. The fallopian tube will not be removed. A folic acid antagonist will be provided as an injection to prevent the ectopic pregnancy from growing, and it gradually treats the ectopic pregnancy.
Surgical treatment (ectopic pregnancy surgery):
Seven in every 100 women with ectopic pregnancy may need surgery even after medical treatment.
- Salpingectomy: Segmental or complete removal of the fallopian tube. It is preferred when the tube is ruptured and damaged.
- Salpingotomy: It is a surgical creation of an opening into the fallopian tube without removing the tube itself in this procedure. It is often preferred in unruptured ectopic.
Surgeons may perform salpingectomy or salpingotomy either by using two approaches, such as:
- Laparoscopy: It is a keyhole surgery that involves the removal of the affected fallopian tube with the ectopic pregnancy.
- Laparotomy: When laparoscopy may not be suitable, and laparotomy (open surgery) is appropriate to deal with some cases, such as when the tubal rupture has happened or there are adhesions in the pelvis region.
The treatment of non-tubal ectopic pregnancy will depend on the location as the pregnancy is growing (sites of ectopic pregnancy). The gynaecologist will discuss the available treatment options with the patient based on the several factors such as levels of pregnancy hormone in blood, location of the ectopic pregnancy and the ultrasound scan report.
Ruptured Ectopic Pregnancy Treatment
If the tubal or non-tubal pregnancy has ruptured, to manage this emergency situation, emergency surgery might be needed to stop the bleeding. It is performed by removing the ruptured fallopian tube and pregnancy.
The chances of having a successful normal pregnancy (pregnancy in the uterus) in the future are good. Even if the patient has only one fallopian tube, the chances of conceiving are only slightly reduced.
Prevention of Ectopic Pregnancy
Ectopic pregnancy cannot be prevented, but one can reduce the risk of ectopic pregnancies by addressing some underlying risk factors and taking the following precautions:
- Taking regular pelvic examinations and screenings
- Early detection and treatment of sexually transmitted infections (STIs)
- Use of barrier methods during sexual intercourse
- Closely monitoring while using assisted reproductive technologies (ART)
- Avoiding smoking
- Patient counselling
Future Pregnancy Risks
If a patient has had an ectopic pregnancy, they may have a higher risk of experiencing another ectopic pregnancy in the future. The risk of ectopic pregnancy in the general woman is 1 in 50 to 80 women. The risk of another ectopic pregnancy is 1 in 10.
Difference between ectopic pregnancy and normal pregnancy symptoms
Ectopic pregnancy vs normal pregnancy symptoms
The following table shows the differences between the normal pregnancy and ectopic pregnancy symptoms:
| Elements | Normal pregnancy | Ectopic pregnancy |
|---|---|---|
| Vaginal bleeding | Light spotting in early days (first 6 to 12 days) | Often starts and stops, watery and dark brown in colour. |
| Nausea and vomiting | Most common symptoms in early pregnancy | May or may not present |
| Abdominal pain | Cramps or pain are common in pregnancy (mild to moderate) | Mild and dull to severe and sharp pain at one side or lower abdomen or in the pelvic area. |
| Constipation | Common | Not common |
| Signs of shock | Not present | May present if ectopic pregnancy ruptures |
FAQs - Frequently asked questions on Ectopic pregnancy
When does ectopic pregnancy pain start?
Symptoms of ectopic pregnancy often start between the 4th and 12th weeks of pregnancy or 6 to 8 weeks after the last normal menstrual period. However, if the ectopic pregnancy is not in the fallopian tube, the patient may experience symptoms later.
Some women don’t not experience any symptoms at first. They may not find out they have this condition until an early scan shows the issue, or they may develop more severe symptoms later on.
Will pregnancy test show positive if ectopic?
Yes, a pregnancy test can show a positive report if the woman has an ectopic pregnancy because the test detects the pregnancy hormone - human chorionic gonadotropin (hCG). However, β-HCG levels usually increase less in ectopic pregnancies than in healthy pregnancies.
Can I get pregnant after ectopic pregnancy?
Yes, a woman can get pregnant after ectopic pregnancy. As per the studies, it has been reported that many women have healthy pregnancies after an ectopic pregnancy.
However, previous ectopic pregnancy may increase the risk of future ectopic pregnancy. Hence it is recommended to get done timely consultation with gynecologist or obstetrician to find any risks.
How common is ectopic pregnancy?
The occurrence of ectopic pregnancy among all pregnancies is about 0.25-2.0%, which is rare but potentially life-threatening. As per the Indian studies, it was found that a prevalence of ectopic pregnancies could range from 1-2%. It is commonly seen in the age group between 18 to 38.
Can an ectopic pregnancy continue until delivery?
No, ectopic pregnancy cannot continue until delivery. However, with a cesarean scar ectopic pregnancy and an abdominal pregnancy, the pregnancy may theoretically continue to the point in which the pregnancy can reach a point of viability (capacity of a foetus to survive outside the uterus). Always the ectopic pregnancy is recommended to be removed.
Does hCG increase in ectopic pregnancy?
No, human chorionic gonadotropin (hCG) levels don't increase in ectopic pregnancy. In a normal pregnancy, the first-trimester β-hCG concentration rapidly increases, doubling about every 48-72 days. β-hCG levels usually increase less in ectopic pregnancies than in healthy pregnancies. A rapidly falling hCG level could indicate an extrauterine pregnancy.
Can you have an ectopic pregnancy after a hysterectomy?
No, usually, a woman cannot have an ectopic pregnancy after a hysterectomy, but in a very rare cases, a woman has a chance of having ectopic pregnancy after a hysterectomy, if the woman ovaries and fallopian tubes weren't removed during hysterectomy. Ectopic pregnancy after hysterectomy is a very uncommon event. However, its frequency is increasing due to certain types of hysterectomies (supracervical hysterectomy).
Is constipation a sign of ectopic pregnancy?
No, commonly constipation does not indicate ectopic pregnancy. The common signs and symptoms of ectopic pregnancy include missed period, abdominal pain, irregular vaginal bleeding. If the ectopic pregnancy ruptures, internal bleeding happens from the fallopian tube, then a patient feel shoulder pain.
How does an ectopic pregnancy resolve itself?
Sometimes, ectopic pregnancy does not rupture and they resolve itself without treatment. The embryo often degenerates, similar to miscarriage, and the woman may feel minimal pain or bleeding. However, some ectopic pregnancies do not resolve on their own and require medical help.
How to prevent recurrent ectopic pregnancy?
A woman can't prevent an ectopic pregnancy. Still, one can reduce the risk of ectopic pregnancies by addressing some underlying risk factors, including pelvic infections, tubal damage, or malfunction of the uterus.
Can an ectopic pregnancy be moved to the uterus?
No, an ectopic pregnancy cannot be moved, as it is not possible to re-implant and it is fatal. Hence, it always requires treatment. Commonly, a surgeon can treat the ectopic pregnancies by giving medications and performing surgery, followed by several weeks of follow-up with each treatment.
How long after ectopic pregnancy can I get pregnant?
It is recommended to wait a few months for the damaged area to heal. A surgeon probably encourages the patient to try again for 12 months if the patient age is less than 35 or 6 months if the patient age is more than 35. However, for women receiving surgery for ectopic pregnancy, the chance for intrauterine pregnancy may be the greatest within 6 months after operation.
Can ectopic pregnancy be aborted?
No, ectopic pregnancy cannot be aborted. As per the studies, there is no evidence to suggest that medical abortion treatment leads to unusual complications for women with ectopic pregnancies. However, it is possible for an early ectopic pregnancy to end in miscarriage on its own, but in most cases it does not and medical intervention will be required.
Can ectopic pregnancy be confused with appendicitis?
Yes, ectopic pregnancy may be confused with acute appendicitis because it causes similar symptoms such as abdominal pain, nausea and vomiting. These similarities make the diagnosis tricky, especially in areas with limited medical resources.
Share on
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868