Colonoscopy | Test Cost & Procedure
PACE Hospitals provides advanced colonoscopy testing in Hyderabad, India, to diagnose and manage a wide range of digestive health conditions. Whether you’re experiencing abdominal pain, rectal bleeding, or changes in bowel habits, our experienced gastroenterologists use state-of-the-art technology to offer accurate evaluation and care at an affordable cost.
Book an Appointment for Colonoscopy Procedure
Colonoscopy Appointment Enquiry
Thank you for contacting us. We will get back to you as soon as possible. Kindly save these contact details in your contacts to receive calls and messages:-
Appointment Desk: 04048486868
WhatsApp: 8977889778
Regards,
PACE Hospitals
HITEC City and Madeenaguda
Hyderabad, Telangana, India.
Oops, there was an error sending your message. Please try again later. Kindly save these contact details in your contacts to receive calls and messages:-
Appointment Desk: 04048486868
WhatsApp: 8977889778
Regards,
PACE Hospitals
HITEC City and Madeenaguda
Hyderabad, Telangana, India.
Why Choose PACE Hospitals for Colonoscopy Test?

State-of-the-Art Colonoscopy Suites with Advanced Video Colonoscopes, High-Resolution Imaging & Safe Sedation
Expert Interventional Gastroenterologists for Comprehensive Diagnosis and Treatment of Colon
Colonoscopy with High Accuracy, Minimal Discomfort & Same-Day Recovery
Affordable & Transparent Colonoscopy Test Cost with Insurance & Cashless Options
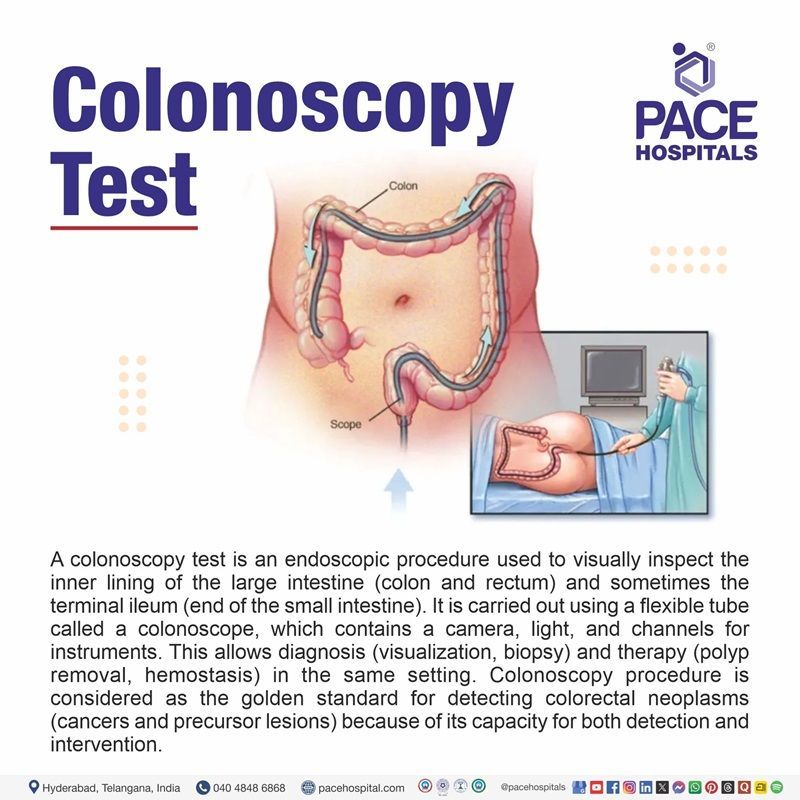
Colonoscopy Test
A colonoscopy test is an endoscopic procedure used to visually inspect the inner lining of the large intestine (colon and rectum) and sometimes the terminal ileum (end of the small intestine). It is carried out using a flexible tube called a colonoscope, which contains a camera, light, and channels for instruments. This allows diagnosis (visualization, biopsy) and therapy (polyp removal, hemostasis) in the same setting. Colonoscopy procedure is considered as the golden standard for detecting colorectal neoplasms (cancers and precursor lesions) because of its capacity for both detection and intervention.
Colonoscopy test is performed by an experienced gastroenterologist, a medical specialist who focuses on diseases of the digestive system and receives advanced training in colonoscopy. Gastroenterologists perform the majority of these procedures owing to their specialized expertise and extensive experience.
Types of colonoscopy
The type of colonoscopy conducted depends on the purpose of the examination, patient history, and need for advanced visualization or treatment. The main types of colonoscopy are:
- Diagnostic colonoscopy
- Screening/Surveillance colonoscopy
- Therapeutic colonoscopy
- Chromoendoscopy or methylene blue chromoendoscopy colonoscopy
- Virtual chromoendoscopy (Narrow Band Imaging (NBI), i-Scan, FICE)
- Water-assisted colonoscopy
- Retrograde viewing colonoscopy
- Computed tomography(CT) colonography, or (virtual colonoscopy)
Diagnostic colonoscopy
This is the most commonly performed colonoscopy, used to evaluate gastrointestinal symptoms such as rectal bleeding, chronic diarrhea, unexplained weight loss, or iron deficiency anemia. The aim is to directly visualize the colon and rectum for any structural abnormalities, inflammation, ulcers, or any growths. A biopsy can be taken during the procedure if necessary. Diagnostic colonoscopy is considered the gold standard for investigating lower GI tract disorders.
Screening / Surveillance colonoscopy
Screening colonoscopy is carried out in individuals without symptoms to detect early signs of colorectal cancer or precancerous polyps, often starting at age 45–50 for average-risk adults. Surveillance colonoscopy is recommended at scheduled intervals in patients with a history of polyps, colorectal cancer, or conditions such as inflammatory bowel disease (IBD) (e.g., ulcerative colitis). These procedures aim to prevent cancer by identifying and removing lesions before they progress.
Therapeutic colonoscopy
This type of colonoscopy is used not just for diagnosis, but also for treatment. Therapeutic procedures include polypectomy (removal of polyps), control of active bleeding (hemostasis), balloon dilation of strictures, decompression of volvulus, or endoscopic stent placement. It is commonly performed when abnormalities are detected during a diagnostic or screening colonoscopy.
Chromoendoscopy
Chromoendoscopy involves the application of special dyes such as indigo carmine or methylene blue onto the mucosal surface during colonoscopy. This enhances the contrast and allows for better identification of subtle lesions or flat dysplastic areas, particularly useful in long-standing inflammatory bowel disease or high-risk cancer surveillance. It may increase the detection rate of dysplastic precancerous polyps.
Virtual chromoendoscopy (NBI, i Scan, FICE)
This advanced imaging technique uses optical filters and light spectrum modifications to enhance visualization of the mucosa and vascular patterns without using dyes. Narrow Band Imaging (NBI), Flexible Spectral Imaging Color Enhancement (FICE), and i Scan are examples. These techniques are quick to activate and improve lesion ccharacterization and differentiation, especially for flat or subtle polyps.
Water-assisted colonoscopy
In this technique, water is used instead of air or CO₂ to distend the colon during insertion of the colonoscope. There are two methods: water immersion and water exchange. These reduce patient discomfort, improve visualization in poorly prepped colons, and may assist in completing difficult procedures. This approach is especially helpful in patients with high sensitivity, including elderly or those unable to tolerate air insufflation well.
Retrograde viewing colonoscopy
This involves the use of additional retrograde (rear-viewing) devices such as the Third Eye® Retroscope, which can be inserted through the working channel of the colonoscope. These tools allow visualization behind folds and flexures where lesions may be hidden from the forward-viewing camera, helping reduce missed polyps and improve detection rates. However, use of such devices is less common today with improvements in high-definition and wide-angle colonoscopes.
Virtual colonoscopy
It is often referred to as CT colonography, is a less invasive imaging method that enables internal visualization of the colon and rectum by using a series of x-rays called computed tomography (CT) data to render endoluminal views in both two and three dimensions. Some clinical trials testing whether drinking a contrast material that coats the stool, instead of using laxatives to empty the colon, shows polyps clearly. Compared with traditional colonoscopy, it generally requires no sedation and can be more comfortable for patients, while also allowing concurrent detection of abnormalities outside the colon. Its diagnostic strength is especially high for polyps or masses equal to or above about 10 mm, though sensitivity decreases for smaller lesions.
Colonoscopy Indications
Colonoscopy is widely regarded as the most effective procedure for direct visualization and management of colorectal diseases. It offers both diagnostic and therapeutic capabilities, making it indispensable in clinical practice. Below are some key indications for colonoscopy:
- Lower gastrointestinal bleeding: Colonoscopy is essential for evaluating suspected sources of lower GI bleeding such as occult blood, melena following a negative upper endoscopy, or hematochezia. In patients who are hemodynamically stable but present with significant bleeding, urgent colonoscopy (ideally within 24 hours) is recommended to facilitate diagnosis and endoscopic management.
- Colorectal cancer or polyps screening: Routine screening is advised for average-risk adults beginning at age 45 (previously 50) and earlier for high-risk populations, such as those with a family history of colorectal cancer or hereditary cancer syndromes (e.g., Lynch syndrome, which is also associated with endometrial, ovarian, gastric, biliary, and urothelial cancers, or Familial Adenomatous Polyposis). Individuals with positive stool-based tests or abnormal sigmoidoscopy need to undergo a full colonoscopy for further evaluation.
- Post-polypectomy surveillance: Repeat colonoscopy schedules depend on initial polyp characteristics: every 3 years for patients with high-risk adenomas, and up to 7–10 years for those with only low-risk adenomas. Surveillance helps detect and prevent further polyp development, advanced neoplasia, or progression to colorectal cancer.
- Post-colorectal cancer resection surveillance: Follow-up colonoscopy is typically performed at 1 year after curative resection, then at 3 years, and subsequently at 5-year intervals if no recurrence is found, ensuring prompt detection of metachronous or recurrent neoplasia.
- Inflammatory bowel disease diagnosing: Colonoscopy is vital for diagnosing IBD, assessing its extent and severity, and obtaining biopsies. Long-term cancer surveillance via colonoscopy begins 8–10 years after symptoms onset in patients with extensive ulcerative colitis or Crohn’s disease involving the colon.
- Diarrheal disorders (acute & chronic): Persistent acute or chronic diarrhea-unexplained by initial stool studies-warrants colonoscopy with biopsy, enabling diagnosis of underlying conditions like microscopic colitis, IBD, or infections.
- Endoscopic lesion removal: Advanced endoscopic techniques like Endoscopic Mucosal Resection (EMR) or Endoscopic Submucosal Dissection (ESD) (EMR/ESD) allow for minimally invasive removal of adenomas and select early colorectal cancers during colonoscopy, reducing the need for any surgical intervention.
- Bleeding control: Endoscopic therapy using clips, thermal coagulation, or injections is frequently employed for diverticular, vascular, or other sources of colonic bleeding detected during colonoscopy.
- Colonic decompression: Colonoscopy can be used for decompression of acute colonic obstruction (such as sigmoid volvulus or pseudo-obstruction) and as a bridge to surgical management in selected patients.
- Stricture dilation: Benign colonic strictures-often resulting from previous surgery or chronic IBD-can be treated with balloon dilation or incision during colonoscopy to relieve obstruction.
- Foreign body extraction: Endoscopic retrieval of colonic foreign bodies, when safely accessible, minimizes surgical risk and expedites removal.
- Clarifying abnormal imaging: Colonoscopy helps differentiate or confirm suspicious findings on Computed Tomography (CT) scans, Positron Emission Tomography (PET) studies, or barium enemas, once any acute inflammation has resolved, guiding further management.
- Unexplained abdominal pain: In selected cases, colonoscopy is performed in patients with ongoing abdominal pain after negative noninvasive workup, although diagnostic yield is generally low unless alarm features (e.g., anemia, weight loss, bleeding) present.
- Chronic constipation with alarm features: Colonoscopy is indicated for adults aged ≥45, or those with rectal bleeding, iron-deficiency anemia, unexplained weight loss, or positive stool tests, to exclude organic pathology, including malignancy.
- Pre- or Intra-operative localization: Endoscopic tattooing or clip placement is routinely used during colonoscopy to mark lesions for surgical resection, improving intraoperative identification and outcomes.
Colonoscopy Contraindications
Colonoscopy is generally safe but is contraindicated or deferred in certain clinical settings where the procedure poses significant risk or is unlikely to provide benefit. Following are the contraindications of colonoscopy :
Absolute contraindications
- Patient refusal: A colonoscopy should never be performed without the patient's informed consent or if the patient withdraws consent during the procedure.
- Known or Suspected colonic perforation: Introducing a colonoscope into a perforated or ruptured colon can worsen leakage, cause peritonitis, and deteriorate patient outcomes. So, colonoscopy must be avoided in such cases.
- Severe toxic megacolon or fulminant colitis: Marked dilation and severe inflammation of the colon increase the risk of rupture during insufflation, so colonoscopy is contraindicated until the patient is stabilized.
- Generalized peritonitis: The presence of severe abdominal pain, guarding, rigidity, or signs of peritoneal inflammation suggests an emergency condition. Colonoscopy could precipitate or worsen perforation and need to be avoided.
- Complete large bowel obstruction: Mechanical obstruction caused by malignant neoplasms or strictures elevates perforation risk, making colonoscopy unsafe.
- Acute diverticulitis or diverticular perforation with abscess: Active inflammation and abscess formation contraindicate colonoscopy due to the risk of spreading infection.
- Active flare of inflammatory bowel disease: Colonoscopy during severe disease activity heightens mucosal injury and perforation risk.
- Recent colorectal surgery or fresh anastomosis: Early colonoscopy may jeopardize healing at surgical sites and is generally contraindicated until sufficient healing has occurred.
Relative contraindications
- Clinically unstable patients: Patients in shock, severe hypotension, or ongoing hemodynamic instability need to be stabilized before undergoing colonoscopy.
- Recent myocardial infarction: Colonoscopy performed within 4–6 weeks after a heart attack carries increased risk of arrhythmias and cardiovascular compromise and need generally be deferred.
- Inadequate bowel preparation: Poor bowel cleansing reduces visibility and increases the risk of missed lesions, prolonged procedure time, and complications. Rescheduling with adequate preparation is recommended.
- Uncooperative patients or Inadequate sedation: Patients unable to tolerate positioning or sedation pose safety concerns that may contraindicate the procedure.
- Acute renal failure and decompensated hepatic disease: These conditions increase the risk of complications from bowel preparation and sedation, requiring risk–benefit assessment.
- Uncorrected coagulopathies and bleeding disorders: Abnormal clotting increases bleeding risk during biopsies or therapeutic procedures and need to be corrected before colonoscopy.
Benefits of Colonoscopy
Colonoscopy is regarded as the gold standard for colorectal cancer (CRC) screening, prevention, and diagnosis. Below are the key advantages of colonoscopy:
- Cancer prevention: Colonoscopy enables the detection and removal of precancerous polyps before they progress to colorectal cancer, significantly lowering incidence and preventing malignant transformation.
- Early cancer detection: By visualizing the entire colon, colonoscopy allows identification of cancers at earlier conditions, more treatable stages, improving survival outcomes.
- Therapeutic potential: Besides diagnosis, colonoscopy allows therapeutic interventions such as polyp removal, bleeding control, dilation of strictures, and stent placement.
- Reduced mortality: Meta-analyses show colonoscopy reduces colorectal cancer (CRC) mortality by up to 68% and incidence by nearly 65% compared with no screening.
- Comprehensive evaluation and diagnosis: Colonoscopy offers a complete evaluation of symptoms such as rectal bleeding, anemia, or altered bowel habits, and helps diagnose conditions like IBD,
diverticulosis, and strictures.
- Surveillance and follow-up: It is highly effective for monitoring patients after polyp removal, those with hereditary colorectal cancer (CRC) syndromes (e.g., Lynch syndrome, FAP), or long-standing inflammatory bowel disease.
Colonoscopy Procedure
Colonoscopy is a safe and effective test used to examine the colon for diagnosis, screening, and treatment purposes. Colonoscopy procedure steps include the following methods mentioned:
Before Colonoscopy Procedure
- To achieve an effective examination, it is advised to patients must prepare their bowels in advance. This typically includes following a clear liquid diet for about 24 hours before the procedure and taking prescribed laxatives or split-dose polyethylene glycol solutions to cleanse the colon.
- The patients will be asked to remove any jewellery or objects that may interfere, and may need to change into a hospital gown.
- It is required that solid foods are avoided the day prior, and patients are encouraged to drink only clear fluids such as broth, tea, or apple juice. Red or purple-colored drinks are not recommended because they may interfere with the visual assessment of the colon lining.
- It is advised that blood-thinning agents, including anticoagulants and certain antiplatelet drugs, might need to be paused for a few days to lower the risk of bleeding if polyp removal is anticipated. However, this should only be done under the guidance of the prescribing physician / gastroenterologists. The patients should also review all current medications, vitamins, and supplements with their doctor/ gastroenterologists, as some essential drugs (like those for heart disease or hypertension) may still be taken with small sips of water on the day of the exam. Some bowel preps may also include the use of an enema, depending on individual cases.
During Colonoscopy Procedure
- On the day of the procedure, patients usually receive either moderate sedation or anesthesia so they remain comfortable and relaxed. Throughout the procedure, healthcare staff closely monitor vital signs including heart rate, oxygen levels, and blood pressure.
- The colonoscope, a flexible tube equipped with a light and camera, is gently passed through the rectum and advanced through the colon. To improve visibility, the colon is inflated with air or carbon dioxide. If any suspicious areas are identified, interventions such as biopsy, removal of polyps, control of bleeding, or dilation of narrowed segments can be performed at the same time.
- The average time required for the procedure ranges from half an hour to about an hour, depending on findings and the need for additional treatments.
After Colonoscopy Procedure
- Following completion, patients are moved to a recovery area until the sedative effects wear off. It is common to experience mild cramping, gas, or bloating as a result of the air used during the exam. Some patients usually stay in the hospital or outpatient centre for about 30 to 60 minutes until the sedatives wear off.
- Because of lingering drowsiness, patients are advised not to drive, operate heavy equipment, or make important decisions for the rest of the day. A responsible adult need to be available to accompany them home.
- Most people can resume eating light meals soon after leaving the facility. Drinking fluids is important to restore hydration lost during the preparation process. In cases where polyps have been removed, doctors or gastroenterologist may give special instructions, such as temporarily avoiding certain medications or foods. A small amount of blood in the stool is not unusual, but heavy bleeding, severe abdominal pain, or fever require urgent medical evaluation.
- The physician/ gastroenterologist will explain post-procedure care, when to restart medications, and when to return for the next screening or surveillance exam. Biopsy results are typically available in a few days, and further management will be based on pathology findings.
Colonoscopy Complications
Although colonoscopy is considered safe and widely used, complications may occur. These depend on patient factors, the type of intervention performed (diagnostic vs therapeutic), and the skill of the endoscopist. Various colonoscopy risks include:
- Cardiopulmonary events: The most frequent complications, making up more than 50% of adverse events, include low blood pressure, reduced oxygen levels, fainting episodes, heart rhythm disturbances, and rarely acute cardiac or respiratory crises. Sedation-related side effects such as drowsiness, restlessness, aspiration, or respiratory depression may also occur.
- Perforation: A rare but critical situation where the colon wall is torn. This may result from mechanical pressure of the scope, excessive inflation, or during polyp removal. The symptoms can be from abdominal pain and bloating to severe peritonitis and shock. Early recognition is critical, and management may involve endoscopic closure or surgery, depending on the size and severity of the perforation.
- Post-polypectomy syndrome: This occurs after the use of electrocautery during polyp removal, where heat injury affects the colon wall without a visible perforation. Some patients may develop fever, abdominal pain, and an elevated white cell count. Treatment usually includes antibiotics, bowel rest, and observation.
- Bleeding: In some cases bleeding can occur during or after colonoscopy, particularly following polyp removal. It is more likely with large or stalked polyps, deep resections, or in patients on blood-thinning medications. Mild bleeding often resolves on its own, while more significant bleeding may require endoscopic treatment.
- Splenic injury: An uncommon but potentially fatal complication is splenic injury, often linked to stretching or traction during scope advancement. Some patients may experience pain in the upper left abdomen or referred pain to the left shoulder, sometimes accompanied by low blood pressure or shock. Treatment may include supportive care, embolization, or surgery.
- Worsening of pre-existing bowel conditions: Frequent bowel movements from colonoscopy preparation can sometimes aggravate conditions such as hemorrhoids, chronic constipation, irritable bowel syndrome (IBS), or diverticulosis.
After a colonoscopy, urgent evaluation is needed if a patient experiences intense abdominal pain, a lasting fever, continued passage of blood in the stool, rectal bleeding that does not ease, sudden lightheadedness, or unexpected weakness.
Colonoscopy Test Preparation
Proper colonoscopy test preparation is important to ensure a clear view of the colon lining and maximize the accuracy of the exam. Below are the key steps:
Diet and fluid restrictions
- One to two days before the procedure, individuals may be asked to follow a low-fiber or low-residue diet, avoiding whole grains, nuts, raw vegetables, beans, and seeds. Studies suggest a low-fiber diet on the day before colonoscopy can be equally effective as a full clear-liquid diet, with better patient tolerance.
- Many guidelines now recommend restricting dietary changes to the day before the procedure, rather than multiple days in advance.
- A clear-liquid diet is usually prescribed for the entire day before the colonoscopy. Acceptable fluids include water, broth, plain tea or coffee (without addition of milk or cream), clear juices (no pulp added), gelatin (non-reddened colors), and electrolyte drinks. Red or purple liquids need to be avoided to prevent misinterpretation as blood.
- It is important to have adequate hydration, because the bowel prep laxatives cause fluid loss.
Selection and timing of bowel prep agents
- The choice of laxative or bowel-cleansing agent is individualized, taking into account safety, tolerability, patient comorbidities (renal, cardiac, electrolyte issues), and prior experiences with prep regimens.
- Preparations are categorized into isosmotic, hypoosmotic, and hyperosmotic agents. High-volume polyethylene glycol (PEG) isosmotic regimens are commonly used because they minimize fluid and electrolyte shifts.
- Many centers now prefer a split-dose regimen, where the bowel prep is divided into two parts: one taken the evening before, and the remaining portion several hours before the colonoscopy. This approach improves cleansing quality and tolerability compared to a day-before dosing alone.
- For afternoon procedures, a same-day regimen (taking the prep the morning of) may be acceptable, though some guidelines view it as less ideal than split dosing.
- The “runway time” - the interval between finishing the bowel prep and the start of colonoscopy - matters. Shorter intervals (e.g. finishing prep 2–5 hours before the procedure) are associated with better cleansing quality.
Patient adherence and instruction strategies
- Following instructions exactly is critical. The patients who miss doses or misunderstand timing are more likely to have inadequate bowel prep, which may lead to missed lesions or the need to repeat the exam.
- Enhanced education techniques - such as reinforced verbal instructions, reminders (via phone or digital tools), simplified leaflets - have been shown to improve bowel prep quality and patient compliance.
Monitoring the rate of adequate bowel preparation (e.g. aiming above 90%) at both individual endoscopist and endoscopy-unit levels is recommended to some individuals.
Colonoscopy Recovery Time
Colonoscopy is generally a safe outpatient procedure, and most patients begin to resume normal activities within a short period of time. Recovery primarily depends on the type of sedation used, whether therapeutic interventions such as polyp removal were performed, and individual patient factors. Colonoscopy recovery time depends on factor as follows:
- Immediate recovery: Most patients are discharged from the recovery area within less than 70 minutes after the procedure, once sedation wears off and vital signs stabilize.
- Extended recovery in some cases: In a subset of patients, particularly those who undergo deeper sedation or therapeutic interventions, recovery may extend beyond 100 minutes.
- Sedated vs. unsedated procedures: For sedated procedures, average recovery times are about 45–60 minutes. In unsedated colonoscopies, patients do not have sedation-related drowsiness but often report more discomfort and fatigue, so return to routine activity still may take several hours.
- Return to daily activities: While most patients return to eating and light activity the same day, some may miss work for the day before due to bowel preparation or the day after as a precaution. However, serious complications causing longer downtime are uncommon.
Questions that the patients can ask the healthcare team about colonoscopy?
- When can I go home after the procedure?
- How long will I need to stay in the recovery area?
- When do I need to schedule my next follow-up appointment?
- What side effects should I expect after colonoscopy?
- When can I resume eating regular food and drinking fluids?
- How soon can I return to work and do daily activities?
- What precautions should I take after the procedure?
- What problems or complications can occur after colonoscopy?
- Is it normal to see some blood in my stool after the procedure?
- When will I receive the results of my biopsy or polyp removal?
- Do I need another colonoscopy, and if so, when?
- Are there any medicines I should avoid after colonoscopy?
Difference between Sigmoidoscopy and Colonoscopy
Sigmoidoscopy vs Colonoscopy
Both sigmoidoscopy and colonoscopy are procedures used to examine the inside of the colon. While sigmoidoscopy looks at the lower part of the colon, colonoscopy provides a full view of the entire large intestine. Knowing the differences helps patients choose the right test for screening or diagnosis.
| Aspect | Sigmoidoscopy (Flexible Sigmoidoscopy) | Colonoscopy |
|---|---|---|
| Area examined | Lower colon: rectum, sigmoid, and sometimes part of descending colon | Entire colon: from rectum to terminal ileum |
| Bowel preparation | Simpler preparation | Longer preparation |
| Procedure time & comfort | Generally quicker and more comfortable | Longer procedure time; requires more technical expertise |
| Cancer outcomes (evidence) | Proven in large studies to reduce colorectal cancer incidence and mortality, especially in the distal colon | Screening colonoscopy significantly reduces colorectal cancer rates and mortality, offering broader protection |
| Ability to view proximal colon | Cannot view the upper (proximal) colon; some lesions may be missed | Detects proximal lesions |
| Next step if abnormal | Abnormal findings → referral for full colonoscopy | Further management such as polyp removal, biopsy, or follow-up treatment within the same procedure |
| Therapeutic capabilities | Limited; mainly diagnostic; polyp removal not usually performed | Both diagnostic and therapeutic – can remove polyps, take biopsies, and place stents |
| Risks | Minimal; lower complication risk compared to colonoscopy | Slightly higher risk of complications (bleeding, perforation); overall risk remains low |
Difference between Endoscopy and Colonoscopy
Endoscopy vs Colonoscopy
Endoscopy is a broad term for procedures that use a flexible tube with a camera to view the inside of the digestive tract. Colonoscopy is a type of endoscopy specifically designed to examine the colon and rectum. Below are some parameters that gives difference between endoscopy and colonoscopy:
| Parameters | Endoscopy | Colonoscopy |
|---|---|---|
| Meaning | A diagnostic procedure using a flexible endoscope to visualize the gastrointestinal tract. Types include upper GI endoscopy (esophagus, stomach, duodenum) and lower GI endoscopy. | A specific form of lower GI endoscopy that examines the rectum, colon, and terminal ileum. |
| Scope of examination | Can evaluate different parts of the GI tract (upper or lower) depending on the type of endoscopy performed. | Evaluates the entire colon and rectum, allowing both diagnosis and therapy. |
| Indications | Used to investigate symptoms such as bleeding, abdominal pain, swallowing, unexplained nausea, or chronic diarrhea. | Primarily used for colorectal cancer screening, polyp detection and removal, evaluation of GI bleeding, IBD, and therapeutic interventions. |
| Diagnostic role | Identifies mucosal abnormalities, ulcers, strictures, or tumors in the GI tract. | Detects polyps, early colorectal cancers, colitis, strictures, and sources of bleeding with higher diagnostic yield in the large bowel. |
| Therapeutic role | Limited, but may allow dilation, biopsy, or removal of small lesions. | Offers both diagnosis and extensive therapy: polypectomy, hemostasis, stricture dilation, foreign body removal, and decompression. |
| Preparation | Preparation depends on the type: fasting for upper endoscopy; bowel prep for lower endoscopy. | Requires strict bowel preparation for clear visualization of the colon. |
| Invasiveness and Recovery | Minimally invasive; recovery is usually quick. | More invasive than standard upper GI endoscopy; recovery is slightly longer due to bowel prep and sedation. |
Colonoscopy Cost in Hyderabad, Telangana, India
The cost of a Colonoscopy in Hyderabad generally ranges from ₹5,000 to ₹24,000 (approximately US $60 – US $290).
The exact colonoscopy test cost depends on whether the procedure is diagnostic or therapeutic, the requirement of biopsy or polyp removal, the type of sedation/anesthesia used, bowel preparation quality, gastroenterologist expertise, and the hospital facilities chosen including – cashless treatment options, TPA corporate tie-ups, and assistance with medical insurance approvals wherever applicable.
Cost breakdown according to type of colonoscopy / procedure:
- Diagnostic Colonoscopy (Without Biopsy) – ₹5,000 – ₹14,000 (US $60 – US $170)
- Colonoscopy with Biopsy – ₹10,000 – ₹18,000 (US $120 – US $215)
- Colonoscopy with Polypectomy (Polyp Removal) – ₹12,000 – ₹22,000 (US $145 – US $265)
- Therapeutic Colonoscopy (Bleeding Control / Lesion Removal) – ₹14,000 – ₹24,000 (US $170 – US $290)
- Colonoscopy under General Anaesthesia (GA) – ₹15,000 – ₹22,000 (US $180 – US $265)
How much does colonoscopy cost in PACE Hospitals?
The price of a colonoscopy test at PACE Hospitals is ₹5,125 (≈ $61 USD) at the HITEC City branch and ₹5,100 (≈ $61 USD) at the Madinaguda branch. However, the cost may vary depending on whether the procedure is performed with sedation or without sedation.
Frequently Asked Questions (FAQs) on Colonoscopy
What diseases can be detected by a colonoscopy?
Colonoscopy can detect colorectal cancer, adenomatous and serrated polyps, inflammatory bowel diseases (ulcerative colitis, Crohn’s disease), bowel cancer, diverticulosis, vascular lesions, strictures, and microscopic colitis when biopsies are taken. It can also help identify sources of lower gastrointestinal bleeding and unexplained chronic diarrhea.
Which is the best hospital for Colonoscopy in Hyderabad, India?
PACE Hospitals, Hyderabad, is one of the most trusted centres for colonoscopy and advanced gastroenterology procedures. Our expert gastroenterologists specialise in diagnosing colorectal cancer, polyps, inflammatory bowel disease (IBD), rectal bleeding, chronic diarrhea, abdominal pain, and other lower gastrointestinal conditions.
With state-of-the-art endoscopy units, high-definition colonoscopes, advanced imaging capabilities, and dedicated pre- and post-procedure monitoring, PACE Hospitals ensures safe, accurate, and comfortable colonoscopy procedures for all age groups — supported by cashless facilities, TPA corporate tie-ups, and assistance with medical insurance processing for eligible patients.
How many polyps are normal in a colonoscopy?
The number of polyps detected during a colonoscopy varies among patients, but studies show the average number is about 1 to 2 polyps per procedure which are considered as normal . Research indicates that detecting three or more polyps increases the risk of advanced neoplasia (pre-cancerous or cancerous lesions), making the number of polyps an important factor in assessing colorectal cancer risk. For quality colonoscopy practice, multiple polyps (more than two) may call for closer surveillance and follow-up.
Why colonoscopy is required?
Colonoscopy is required for colorectal cancer screening, investigation of rectal bleeding, chronic diarrhea, unexplained anemia, or abnormal imaging findings. It also plays a role in surveillance after polyp removal or cancer surgery, and in diagnosing and monitoring inflammatory bowel disease.
How long does a colonoscopy take?
A colonoscopy procedure typically takes about 30 to 60 minutes. However, patients need to plan to spend 2 to 3 hours at the hospital or endoscopy center to account for preparation, sedation, the procedure itself, and recovery. The additional time is necessary for pre-procedure prep and post-procedure monitoring until sedation effects wear off.
What is the cost of Colonoscopy in Hyderabad, India?
At PACE Hospitals, Hyderabad, the cost of colonoscopy typically ranges from
₹5,000 to ₹18,000 and above (approximately US $60 – US $215), making it slightly more affordable. However, the final cost depends on:
- Whether biopsy or polyp removal is required
- Diagnostic vs therapeutic procedure
- Sedation/anaesthesia requirements (local, MAC, or GA)
- Pre-procedure tests and bowel preparation
- Complexity of findings during the procedure
For routine diagnostic colonoscopy, PACE offers one of the most cost-effective packages in Hyderabad, while biopsies, therapeutic interventions, or polypectomy may increase the cost.
After a gastroenterology consultation and review of symptoms, our team provides a clear, personalised cost estimate based on the procedure type and clinical need.
Is colonoscopy painful?
Most people do not experience significant pain during colonoscopy because sedatives and analgesics are usually given to make the procedure comfortable. Some patients may feel mild cramping or pressure from air or CO₂ insufflation used to expand the colon for visibility, but this typically resolves quickly. Recovery is also generally smooth, with little discomfort afterward.
What is a colonoscopy?
A colonoscopy is a specialized test used to look inside the large intestine. During the procedure, an endoscopist guides a thin, flexible instrument with a light and camera through the rectum, providing a clear view of the colon’s inner surface. It not only helps identify issues such as bleeding, ulcers, or growths but also allows removal of polyps and tissue sampling. This makes it the gold standard tool for diagnosing and preventing colorectal cancer and related diseases.
Does colonoscopy require anesthesia?
Colonoscopy typically uses conscious conscious / moderate sedation with medications to reduce discomfort and anxiety. In some centres, deep sedation may be used, which requires anesthesiologist monitoring. General anesthesia is rarely needed except in special circumstances where airway protection or complete unconsciousness is necessary.
Can you have colonoscopy with a hernia?
Colonoscopy is usually safe for patients with hernias. However, large abdominal or parastomal hernias may complicate the procedure or bowel prep, requiring individual evaluation. Rarely, the scope can get trapped in an inguinal hernia, precautions and gastroenterologists’ assessment are needed in such cases.
How clear should stool be for colonoscopy?
Before colonoscopy, stool need to be clear, watery, or light yellow for optimal visualization of the colon lining. Solid particles or brown coloration can interfere with the exam and may require additional bowel preparation or rescheduling.
What are high fiber foods to avoid before colonoscopy?
High-fiber foods such as nuts, seeds, whole grains, raw vegetables, and fruits with skins need to be avoided for 1-3 days before colonoscopy. These foods leave residue in the colon, which can obscure visualization and reduce the effectiveness of bowel preparation.
What is the maximum age for a colonoscopy?
Most guidelines vary, but most recommend routine colorectal cancer screening colonoscopy up to age 75. Beyond this age, the decision is individualized, weighing life expectancy, comorbidities, and the risks versus benefits of the procedure. Routine screening is generally not advised after age 85.
Can colonoscopy and endoscopy be done together?
Yes, upper GI endoscopy and colonoscopy can be performed in the same session, particularly if symptoms suggest disease in both the upper and lower gastrointestinal tract. This approach avoids repeating sedation and is safe when clinically indicated.
Do you get put to sleep for a colonoscopy?
Most colonoscopies are done under conscious sedation, where patients are drowsy but not completely asleep. Some centers use deep sedation with an intravenous anesthetic formulation or agent used for procedural sedation, which induces a sleep-like state. General anesthesia is rarely needed unless there are special circumstances.





