Diabetes – Types, Symptoms, Causes and Complications
Pace Hospitals
Diabetes definition
Diabetes is an acute or chronic, hereditary or acquired condition characterised by abnormal or excess urine formation that passes through the kidneys. Depending on the presence or absence of glucose in the urine, diabetes is classified into diabetes mellitus and diabetes insipidus.
Diabetes meaning
The term "diabetes" dates back to Ancient Greece; it means "pass through." As the Latin name "mellitus” states, "honey or sweet," therefore, diabetes mellitus can be defined as an increase in the formation of glucose content in urine. In the case of diabetes insipidus, the word "insipidus" means "tasteless," Hence, it can be defined as the excess formation of non-glucose urine.
Types of Diabetes
As mentioned above, based on the presence of glucose in the urine, they are classified into two types, namely:
- Diabetes mellitus
- Diabetes insipidus
Diabetes mellitus
Diabetes mellitus is a set of metabolic disorders characterised by hyperglycemia (elevated blood sugar levels). Hyperglycemia is caused by decreased insulin secretion, poor glucose utilisation, and increased glucose production, all of which can be related to the underlying cause of diabetes mellitus. Genetic and environmental factors interact to cause the various forms of diabetes mellitus.
Types of diabetes mellitus
The types of diabetes mellitus are classified based on the pathogenic process leading to hyperglycaemia:
- Type 1 diabetes mellitus
- Type 2 diabetes mellitus
- Gestational diabetes mellitus
- Genetic defects (beta cell development and insulin action)
- Transient neonatal diabetes mellitus
- Endocrinopathies
- Infections associated with diabetes mellitus
- Drug-induced diabetes mellitus
- Immune-mediated diabetes mellitus
- Other genetic syndromes
Diabetes insipidus
Diabetes insipidus is a rare hereditary disorder that produces excessive urine. It is characterised by polyuria (frequent urination) and polydipsia (extreme thirst). People with diabetes insipidus often urinate more than 15 to 19 liters daily. In contrast, healthy individuals typically urinate between 2 and 3 liters daily.
Types of diabetes insipidus
The types of diabetes insipidus are based on the decrease in anti-diuretic hormone (ADH) concentration or its binding abnormality to the kidney cells, they are classified into four types:
- Central diabetes insipidus
- Nephrogenic diabetes insipidus
- Gestational diabetes insipidus
- Dipsogenic diabetes insipidus or psychogenic polydipsia
Prevalence of diabetes in India
Diabetes mellitus prevalence in India is top-notch, and it is considered the diabetes hub of the world, with a stake of 17% of the total number of diabetes patients globally. In 2019, it was reported diabetes mellitus affects nearly 7.7 crore people in India, with the number expected to rise to 13.4 crores by 2045. As per World Health Organization (WHO) and Non-communicable diseases (NCDs), diabetes mellitus ranked ninth among the top 10 leading causes of death globally in 2019.
Diabetes insipidus is rare in India and globally, affecting about 1 in 25,000 people worldwide.
Causes of diabetes
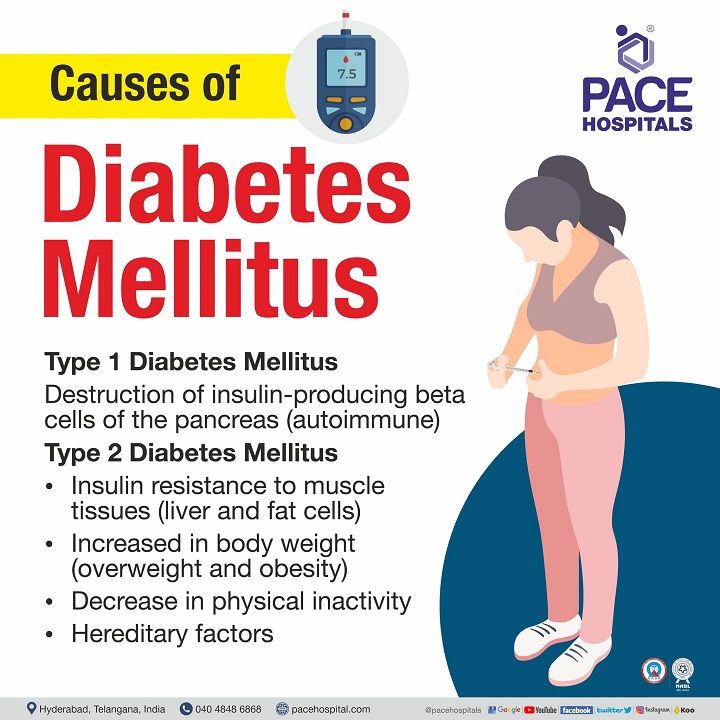
Causes for diabetes mellitus
The endocrine cells (beta and alpha) of islets of Langerhans present in the pancreas secrete insulin hormone from the beta cells and glucagon hormone from the alpha cells. Both beta and alpha cells adjust their hormone release levels in response to their surrounding glucose concentration and maintain normal glucose levels in the blood.
In normal conditions, when the glucose concentration is higher in the blood, beta cells release more insulin. In the case of low blood glucose, glucagon is released in excess from alpha cells. Diabetes mellitus is caused by hyperglycaemia (increase in blood sugar levels) which occurs either due to low or no amount of insulin production (type 1 diabetes) or reduced insulin activity or insulin resistance (type 2 diabetes).
Damage to the pancreatic beta cells, resulting from an autoimmune response (unknowingly attacking the own cells), leads to type 1 diabetes. As a result, the beta cells in the body are damaged, and insulin levels drop severely low.
In type 2 diabetes, an imbalance between insulin levels and insulin sensitivity results in a functional insulin deficit. The insulin released from the beta cells cannot be utilised by the body (skeletal muscle and adipose tissues), signifying insulin resistance. Insulin resistance is complex; however, it is most typically caused by increased body weight and aging.
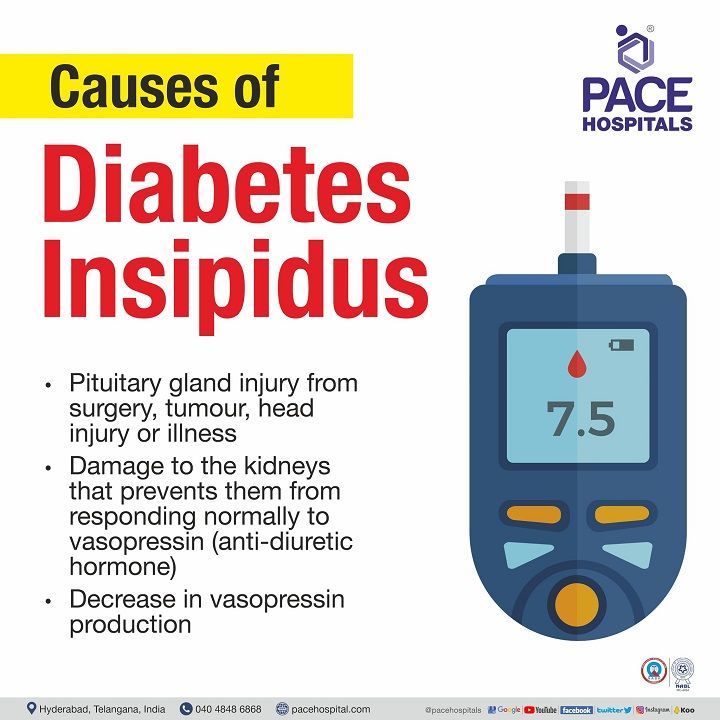
Causes for diabetes insipidus
Diabetes insipidus is caused either by inadequate or impaired secretion of arginine vasopressin (anti-diuretic hormone) from the pituitary gland or by an insufficient kidney response to the arginine vasopressin, leading to polyuria (excessive urine formation) and underlying polydipsia (a feeling of extreme thirst).
Anti-diuretic hormone or vasopressin that is released from the pituitary gland reaches the kidney (digital convoluted tubule) and binds to arginine vasopressin receptor 2 (AVPR2) in the kidney. This, AVPR2, stimulates the transfer of water (reabsorption) into the bloodstream from the kidney and maintains the blood concentration (osmolality). The unabsorbed waste and a small amount of water from urine are excreted from the body.
During diabetes insipidus, very little water is reabsorbed from the kidney (digital convoluted tubule) to blood vessels, either due to a decrease in pituitary gland vasopressin secretion (which may be due to autoimmune) or because kidney cells are unable to bind with the released vasopressin. This causes an increased amount of urine formation in the kidney, which is commonly called polyuria.
Due to the low amount of water present in the renal blood vessels (due to the low amount of water transported back to the blood vessels from the kidney), the blood osmolality gets disturbed, requiring more water to get balanced in the body. As a result, the osmoreceptors in the hypothalamus trigger the sensation of thirst, causing the person to feel thirsty (polydipsia).
Diabetes symptoms
Symptoms of diabetes are characterised by excessive thirst and urination. In addition to this, the symptoms are as follows:
Diabetes insipidus symptoms in adults
- Polydipsia (feeling extremely thirsty)
- Nocturia (waking up middle of the night to urinate frequently)
- Excessive production of pale urine
- Diabetes insipidus symptoms in children
- Nocturnal enuresis (involuntary urination at sleep)
- Difficulty to sleep
- Increased body temperature or fever
- Difficulty in passing stools
- Decrease in weight
- Slow growth
- Vomiting
Diabetes mellitus symptoms
- Frequent urination
- Ketonuria (high ketone levels in urine)
- Fluctuations in mood
- Blurred vision
- Weight loss
- Weakness
- Excessive thirst
- Slower rate in healing of sores
Risk factors of diabetes
The following are the factors associated with diabetes risk; they may vary depending on the type of diabetes.
Risk factors of diabetes mellitus
- The presence of inherited autoantibodies (auto-antibodies in family or parents) increases the risk of developing type 1 diabetes.
- Being overweight (body mass index >25 kg/m²) or obese (body mass index > 30 kg/m²) is the major risk factor for type 2 diabetes mellitus and gestational diabetes
- Family history of having diabetes mellitus (type 1 and type 2)
- Low physical activity
- History of having gestational diabetes
- The presence of polycystic ovary syndrome act as a risk factor for gestational diabetes
- Given birth to a child weighing more than 4 kilograms
Risk factors of diabetes insipidus
Presence of nephrogenic diabetes insipidus (permanent failure of kidney’s ability to concentrate urine) gene in women that can pass to their male babies.
Diabetes prevention
Diabetes cannot be prevented if it results from a hereditary or an autoimmune disease. The prevention factors differ based on the type of diabetes.
Prevention of diabetes mellitus
Diabetes mellitus, caused by an autoimmune antibody (type 1), is hard to prevent as it is caused by abnormal immune system functions.
In type 2 diabetes mellitus, gene or hereditary-associated diabetes mellitus is unpreventable. However, if a person is diagnosed with prediabetes, the following precautions can be taken to slow down the progression of type 2 diabetes mellitus.
- Consume healthy food (in smaller proportions) that is lower in fat (saturated and trans-fat), carbohydrate and rich in fiber, including fruits and vegetables
- Increase physical activity by a least 150 minutes per week (30 minutes a day, five days a week) of moderate aerobic activity (brisk walking or cycling)
- Losing 5% to 7% of body weight in the case of overweight or obese individuals
Prevention of diabetes insipidus
Diabetes insipidus prevention is primarily concerned with avoiding or resolving the underlying causes. This includes avoiding certain medicines, addressing underlying medical concerns, and regulating fluid intake and output to avoid dehydration. In cases where the cause is uncertain, regular monitoring and management of symptoms might help avert issues.
Difference between diabetes mellitus and diabetes insipidus | diabetes mellitus vs diabetes insipidus
| Elements | Diabetes mellitus | Diabetes insipidus |
|---|---|---|
| Definition | Group of metabolic disorders characterised by an increase in blood glucose levels | It is a rare genetic condition that causes excessive urine production and the sensation of thirst. |
| Causes | Caused either by due to deficiency of insulin production from the pancreatic cells or insulin resistance to muscle tissue. | Caused by a reduction in anti-diuretic hormone (ADH) levels or an impairment in ADH binding to kidney cells. |
| Glucose in urine | Presence of glucose in urine. | Absence of glucose in urine. |
| Diet restriction | Diet rich in sugar, fat, and processed meat | Diet had no role in the cause |
| Incidence | Incidence is more | Rare incidence |
Diabetes diagnosis
The diagnostic tests used for the detection of diabetes vary based on the type of diabetes.
Diabetes mellitus diagnosis
Diagnosis of diabetes mellitus is made through any of the following, according to American Diabetes Association (ADA):
- Glycated haemoglobin (HbA1c) test
- Fasting plasma glucose (FPG)
- Oral glucose tolerance test (OGTT)
- Random blood sugar test (RBS)
Diabetes insipidus diagnosis
Diagnostic tests used to detect diabetes insipidus include:
- Water deprivation test
- Magnetic resonance imaging (MRI)
Diabetes treatment
The treatment for diabetes is managed by treating underlying conditions through therapeutic therapy and lifestyle management. In a few cases, surgical intervention might be required.
Diabetes mellitus treatment
- Type 1 diabetes treatment: Treatment for type 1 diabetes includes monitoring blood sugar levels often, measuring the intake of carbohydrates in meals, and injecting insulin. In some cases, pancreas or islet cell transplantation may be a surgical option.
- Type 2 diabetes treatment: Lifestyle modifications that include diet and exercise, blood sugar monitoring, and the use of oral diabetic medications or oral hypoglycaemic agents, insulin, or both, are the cornerstones of care for people with type 2 diabetes.
Diabetes insipidus treatment
Based on the causative factor of diabetes insipidus, the treatment may vary.
Central diabetes insipidus treatment
- If there is any abnormality in the pituitary gland that releases ADH hormone, the underlying cause should be resolved.
- Medical management includes synthetic hormones that replace the functions of anti-diuretic hormone (ADH) and reduces urine formation.
Nephrogenic diabetes insipidus treatment
- Medical management includes diuretics, nonsteroidal anti-inflammatories, and synthetic hormones.
- Daily intake of water should be sufficient in order to avoid dehydration.
Complications of diabetes
The complications of diabetes might develop slowly or due to a misdiagnosis of the condition.
Complications of diabetes mellitus
Long term diabetes mellitus leads to complications that develops slowly. The long-term effects of diabetes can be life-threatening that include microvascular and macrovascular complications such as:
- Cardiovascular diseases
- Diabetic nephropathy (kidney damage)
- Diabetic retinopathy (eye damage)
- Diabetic neuropathy (nerve damage)
- Skin infections
- Depression
- Alzheimer's disease
Complications of diabetes insipidus
Complications of diabetes insipidus are more likely to occur if the condition is misdiagnosed or inadequately managed. As diabetes insipidus is characterised by excessive urination and increased sensation of thirst, two major complications can be observed.
- Dehydration
- Imbalance in electrolytes
Frequently asked questions:
Related Articles

Share on
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868
Appointment request - health articles
Recent Articles