Hypothyroidism – Signs, Symptoms, Causes, Complications and Prevention
PACE Hospitals
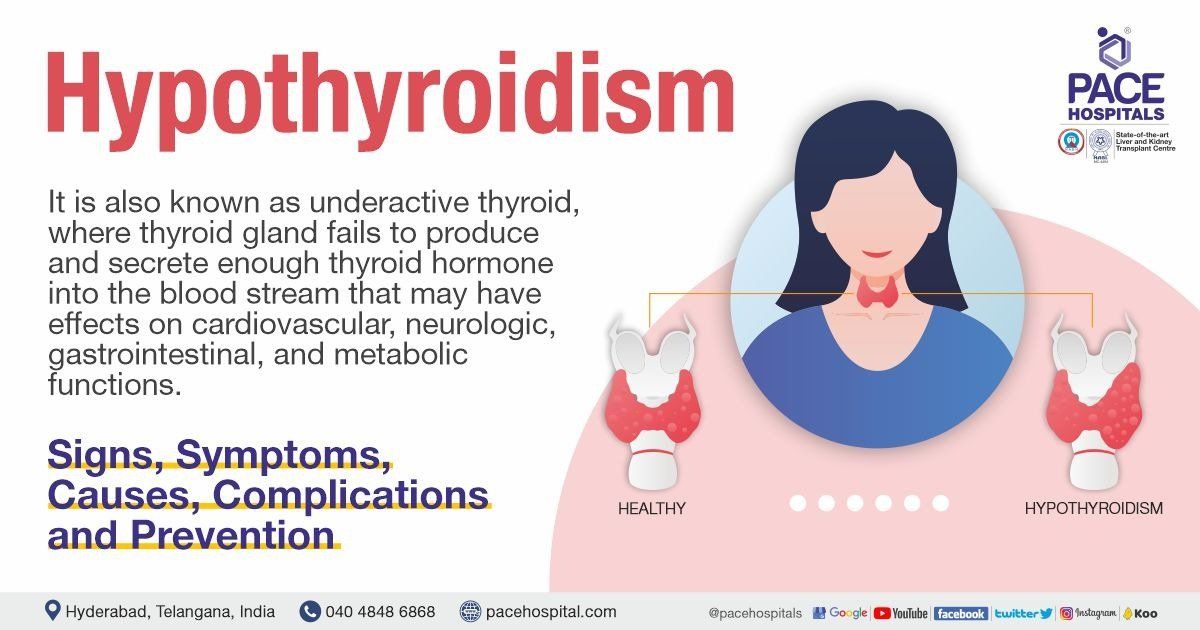
What is a Hypothyroidism?
Hypothyroidism is also known as underactive thyroid, is a condition in which the patient’s thyroid gland (a butterfly-shaped gland in the front of the neck) fails to produce and secrete enough thyroid hormone (thyroxine) into the blood stream. Almost every system in the body responds to thyroid hormone. The consequences of hypothyroidism include effects on cardiovascular, neurologic, gastrointestinal, and metabolic functions. Hypothyroidism is typically caused by autoimmune illness, thyroid removal surgery, or radiation therapy.
Clinically, hypothyroidism is characterised by a high level of thyroid-stimulating hormone (TSH) and a low level of thyroxine (T4), but in some cases, there will be a normal level of thyroxine (T4) with an abnormal level of thyroid-stimulating hormone and patients will have few or no signs of hypothyroidism. Such conditions are known as subclinical hypothyroidism.
Prevalence of Hypothyroidism
- Globally, the prevalence of hypothyroidism is reported as 4 to 5%, whereas, subclinical hypothyroidism reported as approximately 4-15%.
- Pregnancy is one of the risk factors for hypothyroidism, accounting for 1.5%-4% of the prevalence rate. Among them, 0.3% to 0.5% had overt hypothyroidism and the rest had subclinical hypothyroidism.
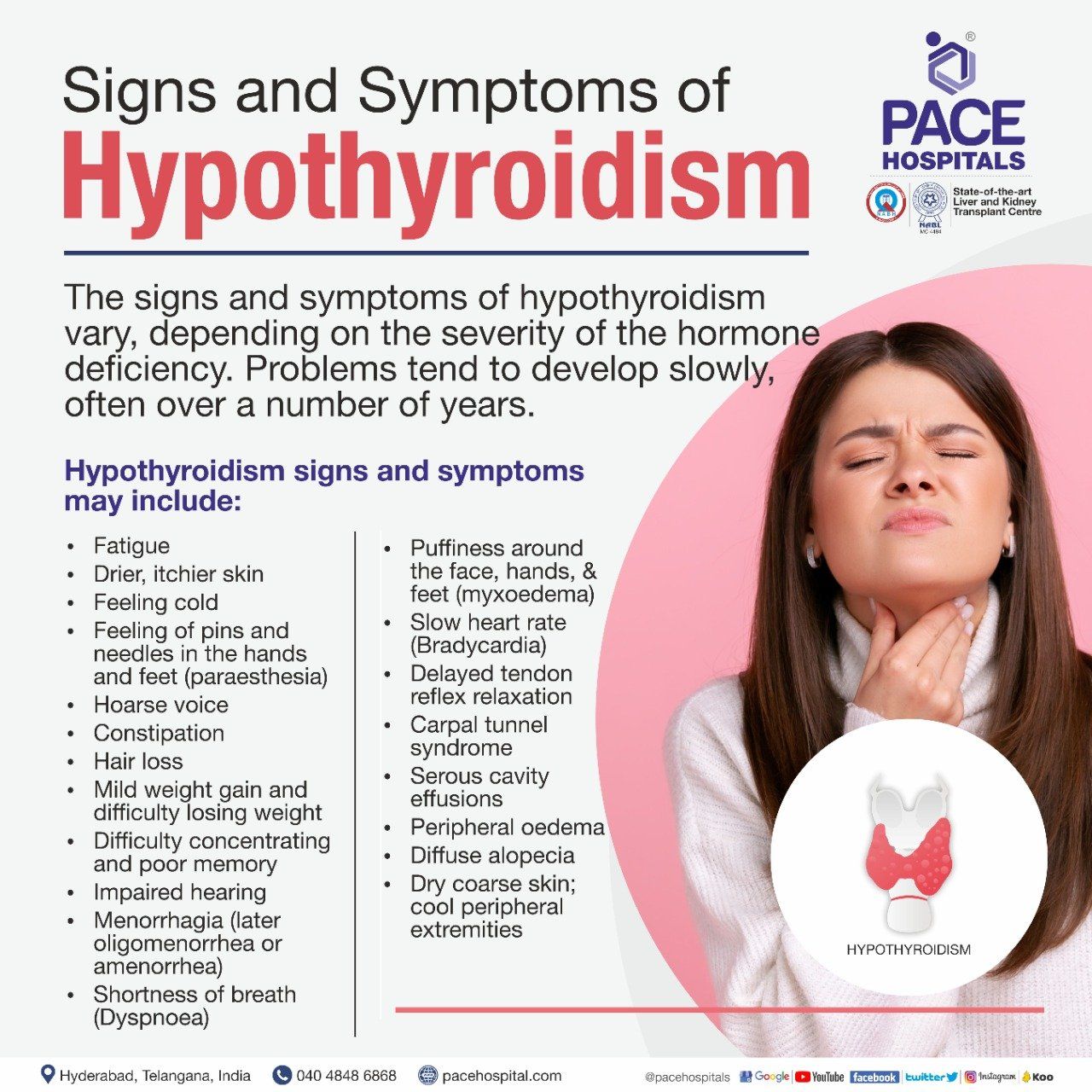
Signs and Symptoms of Hypothyroidism
The signs and symptoms of hypothyroidism depends upon how severe is the hormone deficiency in a person. It's slow and progressive and take the number of years to develop. Initially a person may notice signs of weight gain or feeling overtired and this can be related to other causes as well, over the period more problems will be noticed as years pass by. It's advised to look for these signs and symptoms of hypothyroidism:
Symptoms of hypothyroidism
- Fatigue (a feeling of overtired or weakness)
- Drier, itchier skin
- Feeling cold
- Feeling of pins and needles in the hands and feet (paraesthesia)
- Hoarse voice
- Constipation
- Hair loss
- Mild weight gain and difficulty losing weight
- Difficulty concentrating and poor memory
- Impaired hearing
- Menorrhagia (later oligomenorrhea or amenorrhea)
- Shortness of breath (Dyspnoea)
Signs of hypothyroidism
- Puffiness around the face, hands, and feet (myxoedema)
- Slow heart rate (Bradycardia)
- Delayed tendon reflex relaxation
- Carpal tunnel syndrome
- Serous cavity effusions
- Peripheral oedema
- Diffuse alopecia
- Dry coarse skin; cool peripheral extremities
Symptoms of hypothyroidism in children
Hypothyroidism affects all age groups, including new-borns. It is more severe in premature infants in comparison to term infants. In children, thyroid hormone is also essential for their healthy growth and development; its deficiency causes serious delays in these processes. Symptoms of hypothyroidism in children include:
- Yellowing of the skin and the eyes (jaundice)
- A large, protruding tongue.
- Difficulty breathing.
- Hoarse crying.
- An umbilical hernia
Population at risk of developing Hypothyroidism
- Women, and especially young women, and older people (age above 60 years) are more likely to develop hypothyroidism.
- Pregnancy condition for the last 6 months.
- Presence of prior thyroid problems, such as goiter.
- Previous surgery or radioactive iodine to correct a thyroid problem
- Occurrence of Down syndrome or Turner syndrome
- Family history of autoimmune diseases.
- Having another autoimmune disorder, such as type 1 diabetes, rheumatoid arthritis, multiple sclerosis, celiac disease,
- Having bi-polar disease (manic depression)
- Taking certain medications, such as which can cause hypothyroidism.
Causes of Hypothyroidism
In general, iodine deficiency continues to be one of the leading causes of hypothyroidism, followed by autoimmune disease (Hashimoto's thyroiditis) and iatrogenic causes (treatment of hyperthyroidism). The causes are broadly classified into three categories:
- Primary causes
- Secondary causes
- Transient causes
1. Primary causes
- Autoimmune diseases: Hashimoto’s thyroiditis
- Radiation treatment: Treatment with Iodine-131, surgical removal of the thyroid gland, external irradiation of the neck for lymphoma or cancer
- Drugs: Iodine excess, Lithium, antithyroid Drugs
- Congenital hypothyroidism: Absent or ectopic thyroid gland, dyshormonogenesis (hereditary defects in the steps of thyroid hormone synthesis and secretion), TSH-R mutation Iodine deficiency
- Infiltrative disorders: amyloidosis, sarcoidosis, hemochromatosis, scleroderma, cystinosis, Riedel’s thyroiditis
Primary hypothyroidism is defined as low thyroid hormone levels in the blood caused by thyroid gland destruction. Autoimmunity or an intervention such as surgery, radioiodine, or radiations are typically responsible for this destruction.
Autoimmune disease: The immune system's normal function is to defend the body from foreign substances like bacteria and viruses. Autoimmune diseases, known as "autoimmune," meaning "self," occur when the immune system mistakenly targets healthy tissue. In the case of hypothyroidism caused by autoimmune disease, the patient’s immune system attacks the healthy thyroid cells. This leads to inflammation (thyroiditis) and damage, thereby preventing the thyroid gland from producing thyroid hormone. When a sufficient number of thyroid cells are lost, there is no longer enough to supply the body with thyroid hormone. Hashimoto's disease is the most prevalent type of autoimmune hypothyroidism.
Medications: Hypothyroidism can be caused by several different medications.
- Drugs that suppress serum TSH levels
- Drugs that alter thyroid hormone secretion
- Drugs that alter t3 and t4 metabolism
- Drugs that reduce T4 and T3 binding
- Drugs that Increase thyroglobulin levels
Radiation treatment: People with Graves' disease, nodular goitre, or thyroid cancer are sometimes subjected to or treated with radioactive iodine, which can destroy the thyroid. Hypothyroidism may develop as a result of the radioactive iodine's (131) destruction. In some patients with Hodgkin's disease, lymphoma, or head and neck cancers, radiation therapy has the potential to affect the thyroid, resulting in hypothyroidism.
Congenital (from birth) hypothyroidism: Every year, there are some babies or infants whose thyroids are not fully developed at birth. Some infants are born with a misplaced thyroid or even an incomplete thyroid (ectopic thyroid), and in some infants, thyroid cells or enzymes do not work properly, either because of a genetic defect or because of certain types of medications consumed by the mother.
Too little or too much iodine: Thyroid hormone production requires iodine in the thyroid. Seafood, seaweed, plants cultivated in iodine-rich soil, and iodized salt are good dietary sources of iodine. Optimal levels of thyroid hormone production rely on adequate iodine intake. Insufficient iodine can cause hypothyroidism, while excess iodine can make the condition worse.
2. Secondary causes
- Hypopituitarism: tumours, pituitary surgery or irradiation, infiltrative disorders,
- Sheehan’s syndrome, trauma, genetic forms of combined pituitary hormone deficiencies
- Isolated TSH deficiency or inactivity
- Bexarotene treatment
- Hypothalamic diseases: tumours, trauma, infiltrative disorders, idiopathic
Secondary hypothyroidism occurs as a result of pituitary or hypothalamic damage and results in insufficient TSH production.
Hypopituitarism: In the extremely rare condition, where the pituitary gland (a pea-sized gland located at the base of the patient’s brain below the hypothalamus) fails to produce one, multiple, or any hormone. As a result, there will be a lack of TSH (thyroid stimulating hormone), which stimulates the thyroid gland to secrete hormones like T3 and T4.
Isolated TSH deficiency: A rare condition, where there will be a decrease in TSH with the absence of other pituitary hormonal deficiencies or structural pituitary abnormalities.
Bexarotene treatment: Severe central hypothyroidism was found to be a common side effect of bexarotene, and it was connected to a significant drop in thyroid-stimulating hormone (TSH) and thyroxine levels in the blood.
Hypothalamic disease: Tumours or diseases of the hypothalamus can directly affect the activity of the pituitary gland, resulting in low secretion of TSH.
3. Transient causes
- Postpartum thyroiditis (Hypothyroidism in pregnancy)
- Subacute thyroiditis
- Thyroidectomy
Postpartum Thyroiditis: Some pregnant women and those who have recently given birth (postpartum) experience hypothyroidism because their bodies start making antibodies against their thyroid gland. Miscarriage, premature delivery, and preeclampsia (a condition that causes a significant rise in a woman's blood pressure during the last three months of pregnancy) are more likely if hypothyroidism is left untreated.
Subacute thyroiditis: Subacute thyroiditis is an immune reaction of the thyroid gland that commonly occurs after an upper respiratory infection caused by a virus. The condition usually expresses itself a few weeks after a viral infection of the ear, sinuses, or throat, such as mumps, the flu, or a common cold. This leads to the occurrence of neck pain caused by a swollen and inflamed thyroid gland, which releases too little hormone as it heals.
Thyroidectomy: It refers to the removal of all or part of the thyroid gland in patients due to the occurrence of thyroid nodules, thyroid cancer, or Graves' disease. In such cases, removal of the entire or part of the thyroid gland can lower or halt the production of thyroid hormone.
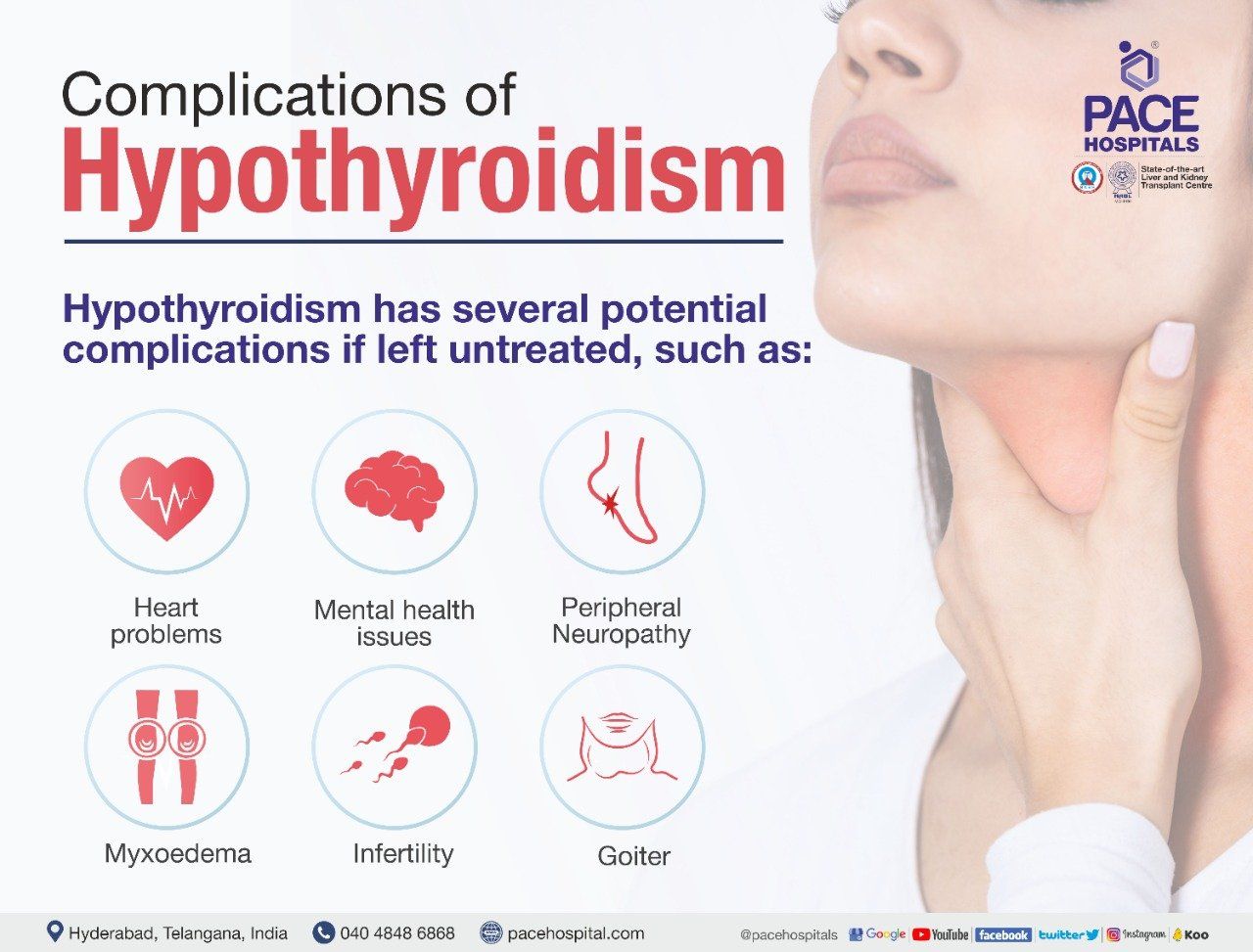
Complications of Hypothyroidism
Hypothyroidism has several potential complications if left untreated, such as:
- Heart problems
- Mental health issues
- Peripheral neuropathy
- Myxoedema
- Infertility
- Goiter
Heart problems: People with an underactive thyroid can have high levels of low-density lipoprotein (LDL) cholesterol (bad cholesterol). As a result, there will be a fatty deposit in the arteries, restricting blood flow. This causes severe heart problems.
Mental health issues: The symptoms of depression can appear early on in hypothyroidism and worsen over time. Mental slowing is another symptom of hypothyroidism.
Peripheral neuropathy: Untreated hypothyroidism over a long period of time can be harmful to peripheral nerves. These are the nerves responsible for transmitting signals from the brain and spinal cord to the rest of the body. Peripheral neuropathy causes pain, numbness, and tingling as its effects.
Myxoedema: In extremely rare cases, a severely underactive thyroid can cause myxoedema, a potentially fatal condition. This is the stage at which thyroid hormone levels plummet, resulting in symptoms such as confusion, hypothermia, and drowsiness.
Infertility: Anovulatory cycles, a defect in the luteal phase, elevated levels of prolactin, and sex hormone imbalances are always in which thyroid dysfunction can negatively impact fertility.
Goitre: A lump in the throat, or goitre, is the result of an abnormal swelling of the thyroid gland. Individuals with an underactive thyroid may develop goitres as a result of the body's attempts to stimulate thyroid hormone production.
Pregnancy related complications in hypothyroidism
Women with hypothyroidism have low chances of fertility. However, even if a patient does become pregnant, the patient faces a higher risk of complications like gestational hypertension, anaemia, abruptio placenta, and postpartum haemorrhage. Women with clinically noticeable hypothyroidism have a higher risk of these complications than women with subclinical hypothyroidism
Hypothyroidism vs Hyperthyroidism | Difference between Hypothyroidism and Hyperthyroidism
| Elements | Hypothyroidism | Hyperthyroidism |
|---|---|---|
| Definition | The thyroid gland doesn’t create and release enough thyroid hormone into the bloodstream. | The thyroid gland makes and releases high levels of thyroid hormone in to the blood stream. |
| Signs and symptoms | • Lean and thin look • Difficulty in concentration and poor memory • Dry coarse skin and hair loss • Feeling cold • Weight gain • Poor appetite • Constipation • Decreased heart rate • Heavy abnormal bleeding at menstruation • Feeling of pins and needles in the hands and feet (paraesthesia) • Swelling/puffiness of face, feet and hand (myxoedema) | • Hyperactivity, irritability, dysphoria • Increase sweating • Feeling hot • Weight loss • Increased appetite • Diarrhoea • Increased heart rate • Scanty and infrequent periods (Oligomenorrhea) in women • Muscle weakness and tremor |
| Diagnostics | • High TSH levels | • High Total T3/T4, T3 Resin Uptake, Free Thyroxine Index levels • Low TSH levels • Low T3/T4, T3 Resin Uptake, Free Thyroxine Index levels |
| Treatment | • It can be treated permanently • No surgical treatment, only pharmacotherapy (medical management) is available. | • Includes thyroidectomy (surgical removal of all or part of thyroid gland) and pharmacotherapy (medical management) as a part of treatment. |
The following steps may be taken by the doctor to diagnose hypothyroidism:
- Physical exam: In addition to patient symptoms and medical history, the physician will check for the presence of physical symptoms like preorbital puffiness, non-pitting oedema, dry skin etc.
- The physician might ask for the patient’s medical and family history.
- Blood test:
- Thyroid-stimulating hormone (TSH)
- Total Thyroxine (T4)
- Free Thyroxine (T4)
- Total Triiodothyronine (T3)
- Free Thyroxine Index
- Thyroid antibody test
Hypothyroidism can be treated with thyroid hormone replacement therapy. It is the administration of synthetic thyroid hormones to treat hypothyroidism. Pure synthetic thyroxine is the most widely prescribed thyroid hormone replacement (T4).
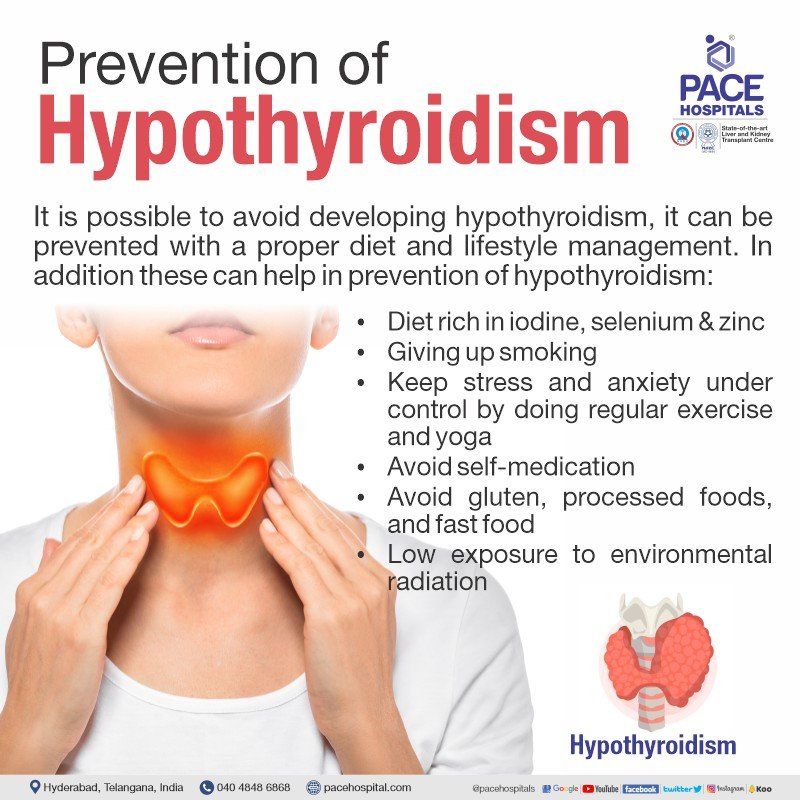
Prevention
It is possible to avoid developing hypothyroidism, it can be prevented with a proper diet and lifestyle management. In addition these can help in prevention of hypothyroidism:
- Diet rich in iodine, selenium, and zinc
- Giving up smoking
- Keep stress and anxiety under control by doing regular exercise and yoga
- Avoid self-medication
- Avoid gluten, processed foods, and fast food
- Low exposure to environmental radiation
Frequently asked questions
Can hypothyroidism be cured?
Yes, hypothyroidism can be completely cured, it is possible only in iodine deficient hypothyroidism. Hypothyroidism can be managed with a life time replacement of thyroxine. Synthetic thyroxine (oral medication) aids in increasing T4 levels and thereby reversing the signs and symptoms of hypothyroidism in iodine deficient hypothyroidism.
What is subclinical hypothyroidism?
When there is biochemical evidence of thyroid hormone deficiency in patients who have few or no features of hypothyroidism. There is no standard recommendation for treating these patients.
Treatment should be offered only when TSH levels are elevated for over 3 months in the following selected patients (Starting with a low dose of thyroxine, 25-50 mcg per day, with the goal of normalising TSH):
- Female with TSH > 10 m IU/L who wishes to conceive.
- With positive TPO (Thyroid peroxidase) antibodies
- Any evidence of heart disease
- Other asymptomatic patients do not require treatment, and thyroid function should be followed annually.
How to control hypothyroidism?
If the patient takes their thyroid hormone medication as directed, their hypothyroidism can be controlled. Medication adherence (taking medication without missing doses) is critical in the treatment of hypothyroidism. Before skipping doses, the patient should notify the
doctor.
How to prevent Hypothyroidism?
Hypothyroidism can be prevented by a diet rich in iodine and selenium, as well as by quitting smoking and keeping stress and anxiety under control.
What is some differential diagnosis for hypothyroidism?
- Thyroid Function test- T3, T4 will be low & TSH will be high.
- TPO Antibody levels will be high in case of Hashimoto thyroiditis.
- Diffuse thyroid swelling or goitre can be seen in iodine deficiency or physiological hypothyroidism
What are the side effects of hypothyroidism?
Hypothyroidism does not have any side effects. However, it had some complications, such as goiter, severe heart problems, infertility, myxoedema, mental health issues, and peripheral neuropathy.
Does subclinical hypothyroidism need treatment?
Yes, if the patient’s thyroid stimulating hormone levels are greater than 10 mIU/L, treatment with synthetic thyroxine is indicated. In the case of mild subclinical hypothyroidism, withholding levothyroxine could be recommended when no clinical improvement occurs, or when the diagnosis is uncertain but follow-up is necessary.
Which salt is good for hypothyroidism?
Patients with hypothyroidism benefit from including iodized salt in their daily diet, as iodine contributes to the production of thyroid hormones in the body.
Can hypothyroidism go away without treatment?
Patients with mild, asymptomatic hypothyroidism may not always require treatment. In rare cases, the condition may improve on its own. However, hypothyroidism must be monitored over time, so subsequent visits are essential. Treatment for hypothyroidism is required if the condition does not resolve itself within a few months.
Is hypothyroidism treatment lifelong?
Yes, if the patient is diagnosed with an underactive thyroid (hypothyroidism) which is a lifelong condition. Therefore, the patient will be on treatment for the rest of their life.
When to start treatment for hypothyroidism?
Treatment with hormone replacement therapy should be initiated as soon as the patient is diagnosed with hypothyroidism. The patient will be having regular blood tests in order to determine the right dose.
How to self-diagnose hypothyroidism?
It can be done in 3 simple steps:
- Step 1: Have the patient stand in front of the mirror with their head back. The patient should make sure that their throat area (between the collar bone and Adams apple) is clearly visible in the mirror.
- Step 2: Pour some water in a glass.
- Step 3: The patient should drink some water and examine their throat (with their head back).
If the patient is suffering from hypothyroidism, there will be a formation of lumps or bumps in the area between the collar bone and Adam’s apple when they swallow the water. For women, as the Adam’s apple is not clearly visible, they need to look at the top of the collar bone.
What to do if after giving full dose still TSH is high?
In patients with normal body weight, on levothyroxine 200 micrograms per day and high TSH indicates: -
- Poor adherence to treatment
- Rule out Malabsorption Syndrome (Celiac Disease, surgery)
- Look for levothyroxine content of that particular brand
- Oral oestrogen
- Ingestion with meals
- With bile acid sequestrants.
How to follow up after starting treatment?
The patient should repeat TSH after 2 months of the initiation of treatment and adjust 12.5 to 25 micrograms if required. Once thyroxine replacement is complete and TSH is stable, TSH should be done annually.
What is treatment of hypothyroidism?
Whatever the cause, the treatment for hypothyroidism is oral thyroid hormone replacement. Medications will be initiated with the goal of keeping TSH in the lower half of the reference range. In the case of the elderly and patients with heart disease, start with a lower dose.
What are the effect of hypothyroidism in pregnancy on foetus?
Foetal development has hazardous complications as organogenesis and differentiation are impaired. Mental retardation, foetal malformation, and congenital birth defects may develop.
Is hypothyroidism a serious disease?
Hypothyroidism is a common condition of thyroid deficiency of thyroid hormone, which is easily diagnosed and managed but potentially fatal in rare cases; untreated hypothyroidism can lead to myxedema coma (a condition in which the body's functions slow down and become life-threatening).
Related Articles
Share on
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868
Appointment request - health articles
Recent Articles