Overactive Thyroid - Hyperthyroidism Disease - Symptoms, Causes and Complications
Pace Hospitals
Hyperthyroidism meaning
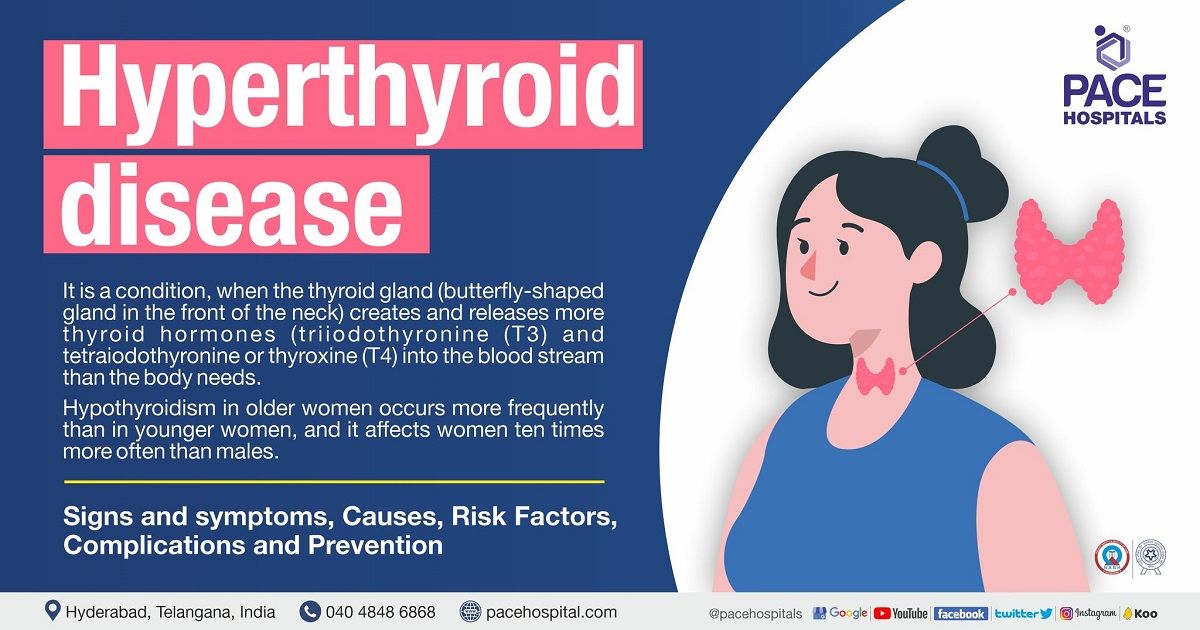
Hyperthyroid disease (overactive thyroid) is a condition when the thyroid gland (butterfly-shaped gland in the front of the neck) creates and releases more thyroid hormones (triiodothyronine (T3) and tetraiodothyronine or thyroxine (T4) into the blood stream than the body needs. Graves' disease and toxic nodular goitre are the two most common causes of hyperthyroidism disease. Hypothyroidism in older women occurs more frequently than in younger women, and it affects women ten times more often than males.
Clinically, the hyperthyroid disease is characterised by high levels of thyroxine (T4) and low or non-existent amounts of TSH, indicating an overactive thyroid and subclinical hyperthyroidism is characterised by low serum TSH, with normal serum T4 and T3 concentrations. This can cause the body's metabolism to speed up, leading to rapid weight loss, increased appetite, anxiety and irregular heartbeats.
Hyperthyroidism disease can be treated with a number of different approaches. The physician prefers to use anti-thyroid medications and radioactive iodine to minimise the production of thyroid hormones. In some cases, it requires surgical intervention to remove a part (sub-thyroidectomy) or complete (total thyroidectomy) thyroid gland as a part of hyperthyroidism treatment.
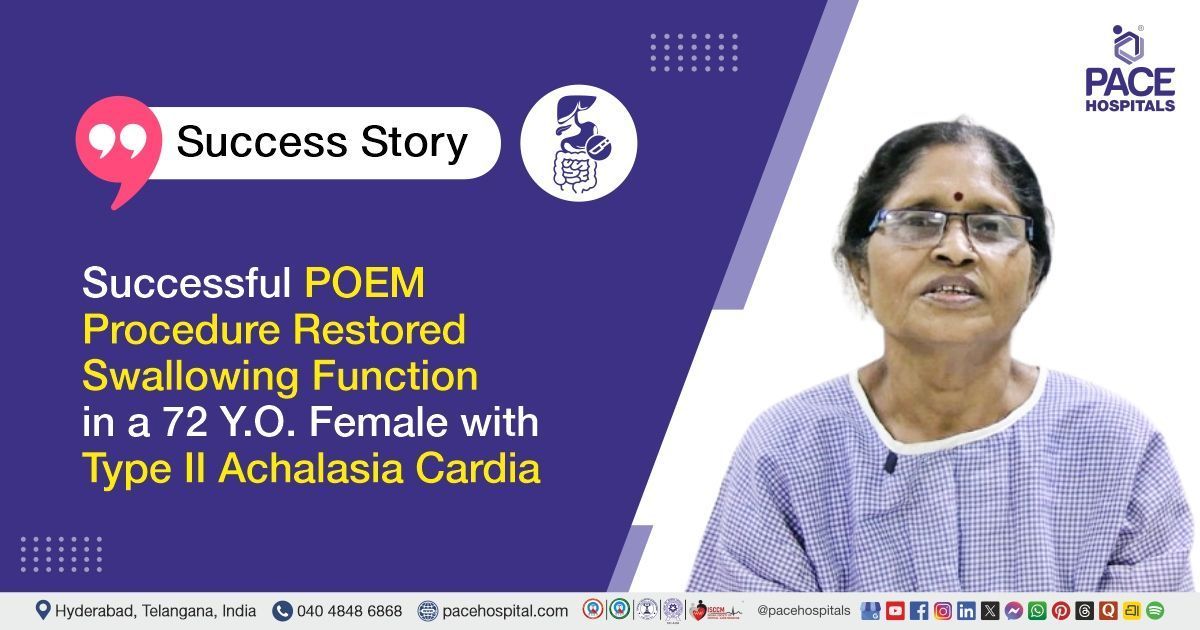
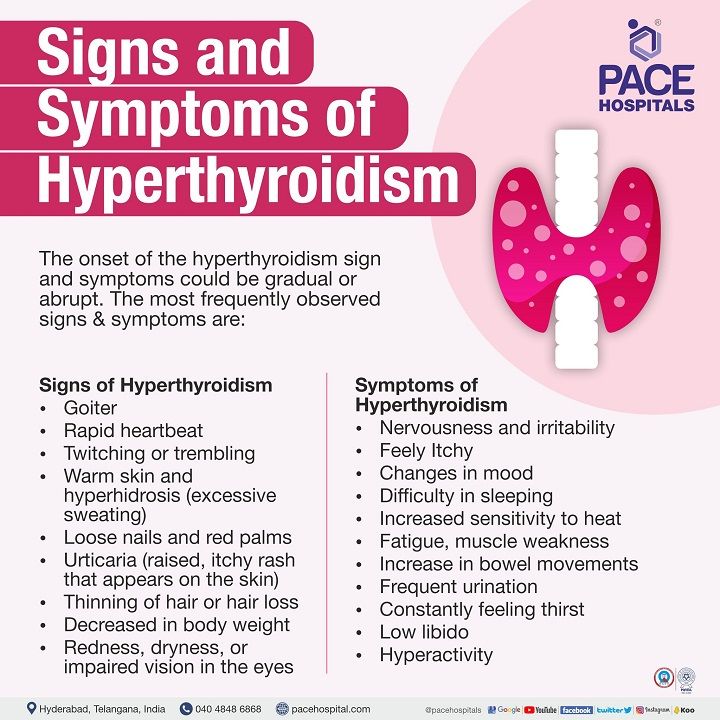
Overactive Thyroid or Hyperthyroidism Symptoms
The onset of the hyperthyroidism sign and symptoms in both males and females could be gradual or abrupt. The symptoms of hyperthyroidism can be mild for some people, but severe and have a big impact on their lives for others. Some may be clear, while others are subtle and difficult to detect at the initial stage. The most frequently observed signs and symptoms in men and women are:
Signs of Hyperthyroidism (Overactive Thyroid):
- Goitre (lump or swelling in the front of the neck, which is caused by a swollen thyroid)
- Rapid heartbeat
- Twitching or trembling
- Warm skin and hyperhidrosis (excessive sweating)
- Loose nails and red palms
- Urticaria (raised, itchy rash that appears on the skin)
- Thinning of hair or hair loss
- Decreased in body weight
- Redness, dryness, or impaired vision in the eyes
Symptoms of Hyperthyroidism (Overactive Thyroid):
- Nervousness and irritability
- Feely Itchy
- Changes in mood
- Difficulty in sleeping
- Increased sensitivity to heat
- Fatigue, muscle weakness
- Increase in bowel movements
- Frequent urination
- Constantly feeling thirst
- Low libido
- Hyperactivity
Causes of Hyperthyroidism (Overactive Thyroid)
Graves' disease is the primary common cause of thyrotoxicosis, followed by toxic multinodular goiter disease and toxic adenoma. The causes are mainly categorised into:
- Primary hyperthyroidism
- Secondary hyperthyroidism
Primary hyperthyroidism disease:
- Graves’ disease
- Toxic adenoma, toxic multinodular goiter or Plummer's disease
- Functioning thyroid carcinoma metastases
- Activating mutation of the TSH receptor
- Activating mutation of GSα (McCune-Albright syndrome)
- Struma ovarii
- Drugs: iodine excess (Jod-Basedow phenomenon)
Secondary hyperthyroidism disease:
- TSH-secreting pituitary adenoma
- Thyroid hormone resistance syndrome
- Chorionic gonadotropin-secreting tumours
- Gestational thyrotoxicosis
Primary cause of Hyperthyroidism disease
Primary hyperthyroidism develops when the thyroid gland is stimulated due to presence of pathological conditions resulting in increased thyroid hormones. The pathological conditions are:
Graves’ disease: In Graves' disease, the patient's immune system targets the thyroid, leading to the production of antibodies against the thyroid. The patient's thyroid is stimulated to produce an excessive amount of T4 by these antibodies. Graves’ disease, which has a prevalence of 75% of patients with over active thyroid gland disease, makes it one of the most prominent causes of hyperthyroidism. It is a hereditary condition (passed down through a family), and it primarily affects young or middle-aged women.
Toxic adenoma, toxic multinodular goiter or Plummer's disease: Hyperthyroidism is caused by one or more adenomas (isolated thyroid tissue) in the patient's thyroid. These adenomas are benign (non-cancerous) nodules or lumps that contain thyroid tissue and cause excess thyroid hormone production (tetraiodothyronine). Those over the age of 60 (elderly) are more vulnerable to this condition.
Functioning thyroid carcinoma metastases: Thyroid hormone production can be adversely affected by cancerous thyroid tumours, though it’s a rare condition.
Activating mutation of the TSH receptor (TSHr): Certain mutations like somatic cells, that constitutively activate the TSHr are the most common cause of benign toxic thyroid adenomas and, in some cases, multinodular goiters.
Activating mutation of GSα (McCune-Albright syndrome): It is a rare sporadic disorder characterised by hyper-functional endocrinopathies, which include hypercortisolism, hypersomatotropism, hypophosphatemic rickets, and hyperthyroidism.
Struma ovarii: It is a type of ovarian tumour in which thyroid tissue makes up more than half of the mass. Usually, this occurs as part of a teratoma. Hyperthyroidism occurs when the struma ovarii produces thyroid hormones despite the fact that the struma ovarii does not normally emit thyroid hormones.
Drugs: iodine excess (Jod-Basedow phenomenon):
Jod-Basedowphenomenon: It is a syndrome that refers to a perplexing phenomenon in which high levels of iodine can cause hyperthyroidism. It is widely common in people who are prone to get thyroid disease or haveunderlying kidney disease.

Secondary cause of Hyperthyroidism disease
Secondary hyperthyroidism develops when the thyroid gland is activated by an abundance of thyroid-stimulating hormone (TSH) in the blood, leading to an increase in thyroid hormones. The underlying conditions that trigger thyroid gland are:
Thyrotropin (TSH)-secreting pituitary adenoma: Hyperthyroidism due to this condition is unusual. Autonomous and resistant to negative feedback from thyroid hormones (inappropriate TSH secretion), which are responsible for hyperstimulation of the thyroid gland, which, in turn, leads to hypersecretion of T4 and T3, resulting in hyperthyroidism.
Thyroid hormone resistance syndrome (THRS): It is an extremely uncommon condition characterised by elevated levels of free thyroxine (FT4) and triiodothyronine (FT3) but normal or mildly elevated levels of thyroid-stimulating hormone (TSH). The most common cause is thought to be mutations in the thyroid hormone receptor gene.
Chorionic gonadotropin-secreting tumours: Human chorionic gonadotrophin (HCG)hormone has thyrotropic activity (increases thyroid hormone levels). The HCG levels will be high during early pregnancy, multiple pregnancies, or molar pregnancies (growth of abnormal cells in a group inside the womb in place of a healthy foetus). Therefore, this results in hyperthyroidism.
Gestational thyrotoxicosis:
Gestational thyrotoxicosis is a type of non-autoimmune hyperthyroidism that occurs during pregnancy and is associated with hyperemesis gravidarum. During pregnancy, the thyroid gland undergoes some changes, including an increase in thyroxine-binding globulin, increased sodium clearance in the kidneys, and thyroid gland stimulation by human chorionic gonadotropin, leading to hyperthyroidism.
Causes of Thyrotoxicosis
The most common causes of thyrotoxicosis are hyperthyroidism-induced Graves’ disease, toxic multinodular goiter, and toxic adenomas. In addition to that, the following can also cause thyrotoxicosis such as:
- Subacute thyroiditis
- Silent thyroiditis
- Other causes of thyroid destruction, such as treatment with antiarrhythmics and radiation
- Thyrotoxicosis factitia or thyroid tissue
Subacute thyroiditis: Subacute thyroiditis, unlike other kinds of thyroiditis, seems to be caused by a viral infection. Subacute thyroiditis can frequently arise within a few weeks of a viral infection of the ear, sinuses, or throat, like flu or a common cold and mumps. The thyroid expands in reaction to the infection, which can interfere with hormone synthesis, resulting in inflammation of the thyroid gland.
Silent thyroiditis: Silent thyroiditis, also known as painless thyroiditis, is an inflammatory disorder of the thyroid gland that can occur due to an immune reaction of the thyroid gland. Thyroid inflammation can result in the release of too many hormones into the bloodstream, leading to hyperthyroidism.
Other causes of thyroid destruction - Antiarrhythmics: Iodine is the essential mineral source required for the production of thyroid hormone. In some people, intake of excess amount of iodine might cause the thyroid to make too much thyroid hormone. Intake of an iodine-containing drug, such as antiarrhythmics, may increase the risk of developing hyperthyroidism (in each 200 mg tablet, there is 75 mg of iodine; approximately 10% of the iodine is released as free iodide daily), and intravenous iodinated contrast, can also cause hyperthyroidism.
Thyrotoxicosis factitial: Thyrotoxicosis factitial is a hyperthyroid condition caused by the accidental or intentional consumption of thyroxine in the form of pills or supplements, with one capsule containing between 0.97 μg to 1.1 μg of triiodothyronine and 3.4 μg to 4.5 μg of thyroxine respectively.
Complication of Thyrotoxicosis
The complication of thyrotoxicosis can be severe if it is not properly detected and treated, which includes:
- Delirium (confused mental abilities)
- Weak and brittle bones
- Muscle weakness
- Atrial fibrillation (irregular heart rhythm)
- Congestive heart failure
- Thromboembolic disease
- Death
Request an appointment for Hyperthyroidism Treatment
Appointment for Hyperthyroidism B
Overactive Thyroid or Hyperthyroidism in pregnancy
The prevalence of hyperthyroidism in pregnancy ranges from 0.05 to 0.2%. It has been associated with a significant increase in low-birth-weight children, congenital abnormalities, stillbirths, neonatal mortality, and maternal heart failure.
Causes of hyperthyroidism in pregnancy
Graves' disease is the primary cause of hyperthyroidism during pregnancy (autoimmune disorder). Graves' disease can first appear during pregnancy. If the patient already has Graves' disease, symptoms may decrease during the second and third trimesters due to decrease in the production of thyroid stimulating immunoglobulin (responsible for the secretion of excess thyroid hormone). Graves' disease often gets worse in the first few months following childbirth, when thyroid-stimulating immunoglobulin (TSI) levels rise.
In addition to Graves' disease, the following are the causes of hyperthyroidism in pregnancy:
- Iodide induced hyperthyroidism
- Single toxic adenoma
- Struma ovarii
- Subacute thyroiditis (thyroid gland inflammation, caused by viral infections)
- Thyrotrophin receptor activation
- Transient gestational hyperthyroidism (hyperthyroidism in pregnant women; non-autoimmune)
- Trophoblastic tumour
- Toxic multinodular goitre
Signs and symptoms of hyperthyroidism in pregnancy
Hyperthyroidism in pregnancy symptoms may be similar to those of pregnant women with normal thyroid function. The most distinctive features of hyperthyroidism in pregnancy are:
- Tachycardia
- Tremor
- Weight loss
- Systolic flow murmurs (an unusual heart sound that occurs when the heart contracts)
- Lid lag
- Exophthalmia (bulging of the eye anteriorly out of the orbit)
Graves' ophthalmopathy
Graves' ophthalmopathy, also known as Graves' orbitopathy or thyroid eye disease, is an eye disease that commonly affects individuals with hyperthyroidism or a history of hyperthyroidism owing to Graves' disease. In patients with Graves' ophthalmopathy, muscles and other tissues surrounding the eyes will be affected by inflammation and other immune system activities. Approximately 30% of persons with Graves' disease exhibit the signs and symptoms of Graves' ophthalmopathy, which includes:
- Dry or gritty eyes
- Eye inflammation
- Puffy eyelids
- Blurred or double vision
- Sensitivity to light.
- Pain or pressure in the eyes
- Vision loss
- Bulging eyes
Risk factors of Hyperthyroidism (Overactive Thyroid)
Hyperthyroidism risk factors may increase the likelihood of having an overactive thyroid, resulting in a high burden of thyroid disease in India.
The hyperthyroidism risk factors are as follows:
- Women have a higher risk than men and older than 60 years old.
- Pregnant or had a baby within the previous six months
- Previous thyroid issues such as surgery or a thyroid problem (goiter).
- Family history of thyroid problems, particularly Graves' disease
- Medical history of type-1 diabetes and primary adrenal insufficiency (Addison’s disease), a hormonal disorder
- Patients with pernicious anaemia
- Intake of too many iodine-rich foods or medicines
- Since hyperthyroidism is the primary cause of thyrotoxicosis, the risk factors for thyrotoxicosis are the same.
Complications of hyperthyroidism (Overactive Thyroid)
Hyperthyroidism complications can be severe if the thyroid condition is not treated. They could lead to:
Heart problems: High thyroid hormone levels have been linked to changes in cardiovascular hemodynamic, which can lead to high-output heart failure and, in advanced stages, dilated cardiomyopathy.
Brittle bones: If left untreated, hyperthyroidism can cause osteoporosis (weak and brittle bones). Calcium and other minerals contribute to bone strength. When thyroid hormone levels are high, the body's ability to incorporate calcium into bones is reduced.
Eye problems: Graves' ophthalmopathy, also termed as thyroid eye disease, is a condition that damages the eyes and causes hyperthyroidism symptoms such as eye redness, eyes feeling dry and gritty, watering eyes, swelling, bulging eyes, sensitivity to light, blurred or double vision. Severe vision loss can occur if eye problems are left untreated. Around one in every three people with Graves' disease has an overactive thyroid.
Red, swollen skin: Rarely, those who suffer from Graves' disease may also experience the skin condition known as Graves' dermopathy. The skin becomes red and swollen, most frequently affecting the shin (the front part of the leg below the knee) and feet.
Thyrotoxic crisis or Thyroid storm: There is a risk of thyrotoxic crisis, which is a rare phenomenon but serious complication of hyperthyroidism. In this condition, the thyroid produces and secretes an abnormally excessive amount of thyroid hormone in a short span of time. High fever, rapid heart rate, congestive heart failure, loss of consciousness and delirium are the symptoms of a thyroid crisis.
The complication of thyrotoxicosis can be severe if it is not properly detected and treated, which includes:
- Delirium (confused mental abilities)
- Weak and brittle bones
- Muscle weakness
- Atrial fibrillation (irregular heart rhythm)
- Congestive heart failure
- Thromboembolic disease
- Death
Diagnosis of hyperthyroidism
The diagnostic evaluation of hyperthyroidism can be done through the following:
- Medical history and physical exam: The physician might take note of the patient’s current medications in order to assess drug-induced hyperthyroidism. Through physical examination, the physician might look for a tiny tremor in the patient's extended fingers, check for the patient’s heartbeat (rapid or irregular), overactive reflexes, changes in the eye, the presence of warm and wet skin, and examine the thyroid gland when the patient swallows, to see if it is swollen, bumpy, or sensitive.
- Blood test: It is used to measure the levels of TSH, free thyroxine index, triiodothyronine (T3), tetraiodothyronine (T4), and thyroid-stimulating immunoglobulin.
- Radioactive iodine uptake test: This test measures the uptake or absorption of radioactive iodine by the thyroid gland from the bloodstream.
- Thyroid scan: It is used to take pictures of the patient’s thyroid gland with the help of a special camera (gamma).
- Thyroid ultrasound: It is used to examine the thyroid gland and associated abnormalities with the help of high-frequency ultrasonic waves.
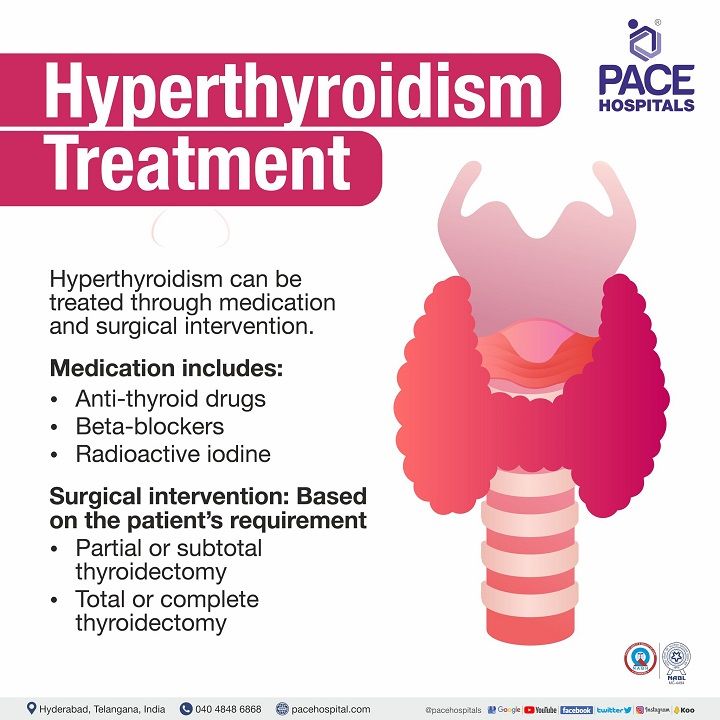
Hyperthyroidism treatment
The primary goal of hyperthyroidism treatment is to restore thyroid hormone levels to normal while avoiding long-term complications. Many treatment options are available for hyperthyroidism. The selection of therapy is purely based on the patient’s age, severity, pregnancy status, and the underlying cause of hyperthyroidism. Hyperthyroidism can be treated through medication and surgical intervention.
Medication includes:
- Anti-thyroid drugs
- Beta-blockers
- Radioactive iodine
Surgical intervention: Based on the patient’s requirement
- Partial or subtotal thyroidectomy
- Total or complete thyroidectomy
Prevention of hyperthyroidism (Overactive Thyroid)
The prevention of hyperthyroidism cannot be done completely. However, one form of primordial prevention is to understand and identify the potential risk factors of hypothyroidism and to prevent its occurrence.
The following points can be considered to prevent hyperthyroidism.
- Quit smoking
- Avoiding food rich in iodine, gluten, soy, and caffeine
- Taking a diet rich in vitamins, iron selenium, zinc and calcium
- Change in lifestyle modifications by including daily yoga and exercise
Frequently asked questions
Related Articles
Share on
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868