Pancreatic duct stricture: Symptoms, Causes, Complications, Treatment & Prevention
Pace Hospitals
Pancreatic duct meaning
The pancreatic duct, also termed the "duct of Wirsung", is a tubular structure in the Pancreas, carrying the digestive enzymes from the Pancreas to the duodenum (initial segment of the small intestine).
The pancreatic duct covers the length of the Pancreas from the head to the tail, with a thickness of 3 mm wide at the head and 1 mm wide at the tail. Also, the duct combines with the common bile duct (a duct carrying bile from the liver and gallbladder) just before entering the duodenum. The duct is surrounded by a muscle called the "sphincter of Oddi", which controls the movement of bile juice and pancreatic juice into the duodenum.
The Pancreas is a gland having exocrine and endocrine functions. As a part of endocrine function, it produces hormones like insulin to regulate sugar levels in the bloodstream, and as an exocrine function, it stimulates digestive enzymes for digestion. The digestive enzymes produced are secreted into the pancreatic duct, carrying to the duodenum, which helps break down the food.
Functions of the Pancreatic Duct
The pancreatic duct plays crucial role in the digestion. It carries digestive enzymes from the pancreas to the duodenum, where they help to break down food.
The pancreatic enzymes include:
- Amylase: helps in breaking down carbohydrates into sugars
- Lipase: helps in breaking down fats into fatty acids and glycerol
- Protease: helps in disintegrating proteins into amino acids
Conditions that can impair the functionality of Pancreatic Duct
A various condition that can affect the pancreatic ducts are:
- Pancreatitis (inflammation of the pancreas)
- Pancreatic cancer
- Pancreatic stones
- Pancreatic strictures (narrowing of the duct)
- Pancreatic duct cysts
What are pancreatic duct strictures?
Pancreatic duct stricture definition
The pancreatic duct is a tube through which digestive fluids pass from the pancreas to the small intestine. The narrowing of the pancreatic duct characterises the condition of pancreatic duct stricture. The narrowing area in the pancreatic duct is called the stricture. This condition arises due to scarring or blockages in the pancreatic duct and thus obstructs the flow of the digestive fluids.
Classification of pancreatic duct strictures
Pancreatic duct strictures are mainly classified based on clinical presentation, aetiology, location, and morphology.
Classification of pancreatic duct strictures based on the clinical presentations:
- Symptomatic pancreatic duct strictures: Shows the symptoms of the condition.
- Asymptomatic pancreatic duct strictures: Doesn’t show any symptoms.
Classification of pancreatic duct strictures based on the etiology:
- Benign pancreatic stone strictures: These are non-cancerous and are caused due to underlying conditions.
- Malignant pancreatic stone strictures: These are cancerous and show metastasis. They are mainly caused by pancreatic cancer.
Classification of pancreatic duct strictures based on the location:
- Main pancreatic duct strictures: This is a common type of condition where the narrowing is seen in the main pancreatic duct.
- Branch duct strictures: Strictures are seen in the branch ducts.
Classification of pancreatic duct strictures based on the morphology:
- Focal strictures: Involves the limited segment of the pancreatic duct.
- Segmental strictures: Involves the longer segment of the pancreatic duct.
- Diffused strictures: Involves the entire pancreatic duct.
Secondary to these classifications, pancreatic duct strictures are dominant or non-dominant.
- Dominant pancreatic duct strictures: Severe grade narrowing is seen with upstream dilation of the main pancreatic duct ≥ 6mm. Endoscopic therapy is needed to treat this type of stricture.
- Non-dominant pancreatic duct strictures: Less severe and don't require surgery or endoscopic therapy. It may or may not cause the symptoms and is usually treated with medications and dietary changes.
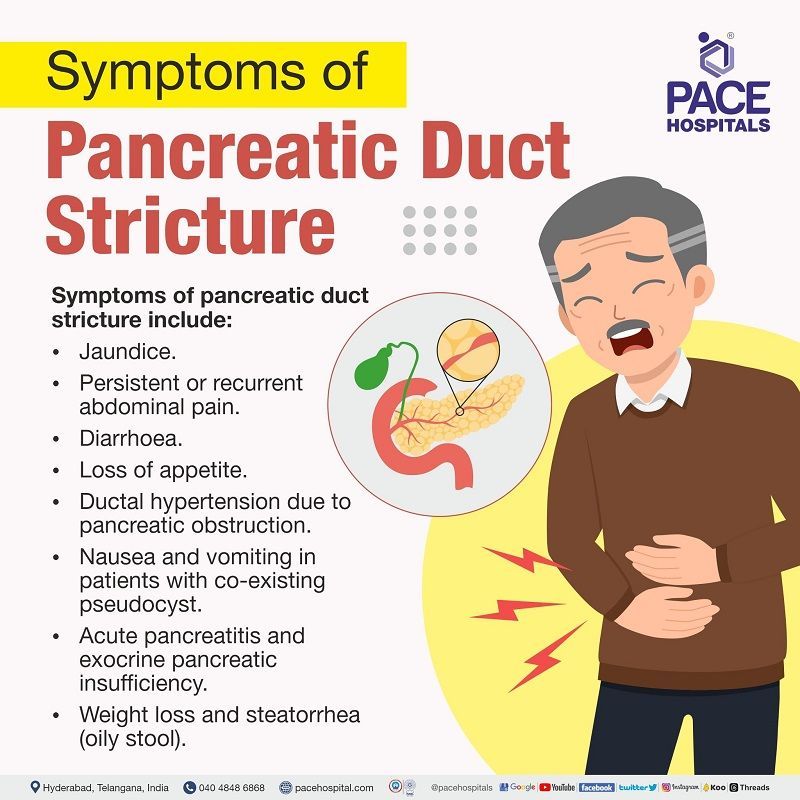
Symptoms of pancreatic duct stricture
The symptoms of pancreatic duct strictures might differ based on the severity and location of the stricture. Some of the common pancreatic stricture symptoms include:
- Jaundice (yellowing of the skin, whites of the eyes & mucous membranes)
- Persistent or recurrent abdominal pain
- Diarrhoea
- Loss of appetite
- Ductal hypertension due to pancreatic obstruction
- Nausea and vomiting in patients with co-existing pseudocyst
- Acute pancreatitis and exocrine pancreatic insufficiency
- Weight loss and steatorrhea (oily stool)
The above symptoms might not occur in every individual. However, the symptoms might occur based on the severity and type. In some cases, the pancreatic duct strictures don't show any symptoms (asymptomatic) and are discovered unintentionally by other diagnostic conditions.
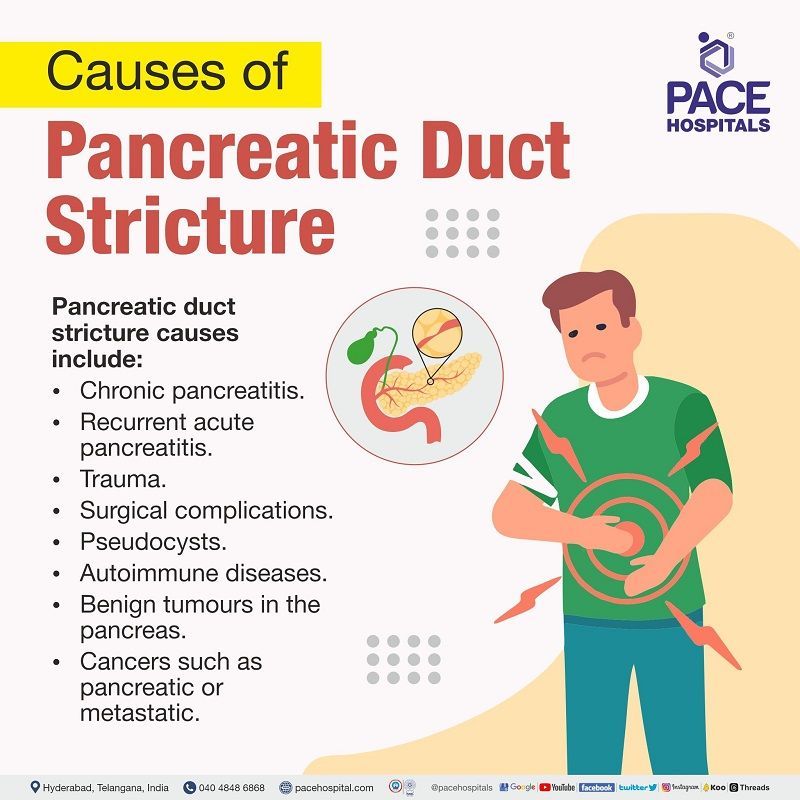
Causes of pancreatic duct stricture
Pancreatic duct stricture causes include:
- Chronic pancreatitis
- Recurrent acute pancreatitis
- Trauma
- Surgical complications
- Pseudocysts
- Autoimmune diseases
- Benign tumours in the pancreas
- Cancers such as pancreatic or metastatic
Pancreatic duct stricture risk factors
There are several aetiological factors that might cause pancreatic duct strictures. Based on the etiology, the pancreatic duct strictures are classified into benign and malignant pancreatic duct strictures:
Risk factors for benign pancreatic duct strictures:
- Trauma: The most common cause of pancreatic injuries, which include contusion, laceration, and transection (fracture), is pressure of the pancreatic body against the spine. These pancreatic injuries frequently result in traumatic pancreatitis, pseudocyst development, abscesses, and pancreatic duct stricture.
- Chronic or recurrent acute pancreatitis: Due to obstruction, scarring, or occlusion caused by pancreatitis, the ducts become constricted and narrow.
- Previous pancreatic surgery: Strictures, haemorrhages, and pancreatic fistulas are the most common complications of pancreatic surgeries. They result in ductal obstruction.
- Pancreatic pseudocyst: Fluid from the pancreas that has leaked forms pancreatic pseudocysts. This condition arises during pancreatitis. When pancreatic cells become inflamed or damaged, pancreatic enzymes begin to leak, pseudocysts occur, and damage to pancreatic tissue results.
- IgG4-related disease (Autoimmune pancreatitis and IgG4-related sclerosing cholangitis): The IgG4 antibody plays a major role in autoimmune pancreatitis. In an autoimmune pancreatitis condition, the pancreatic ducts narrow due to the severe lymphoplasmacytic infiltration that surrounds them.
- Iatrogenic (Placement of PD stent, previous ERCP instrumentation): These procedures have the risk of developing pancreatic duct strictures. According to the studies, symptomatic stent-induced pancreatic stricture was seen in 2.4% of the patients who underwent stent placement procedures. Moreover, patients with a main pancreatic duct diameter of <3mm are more susceptible to pancreatic duct stricture.
- Benign pancreatic neoplasm (benign tumours): Tumours and lesions tend to increase the risk of pancreatic duct strictures.
Risk factors for malignant pancreatic duct strictures:
- Pancreatic and metastatic cancer: Pancreatic adenocarcinoma is the most frequent cause of stricture. When the pancreatic tumour invades the duct, stricture arises.
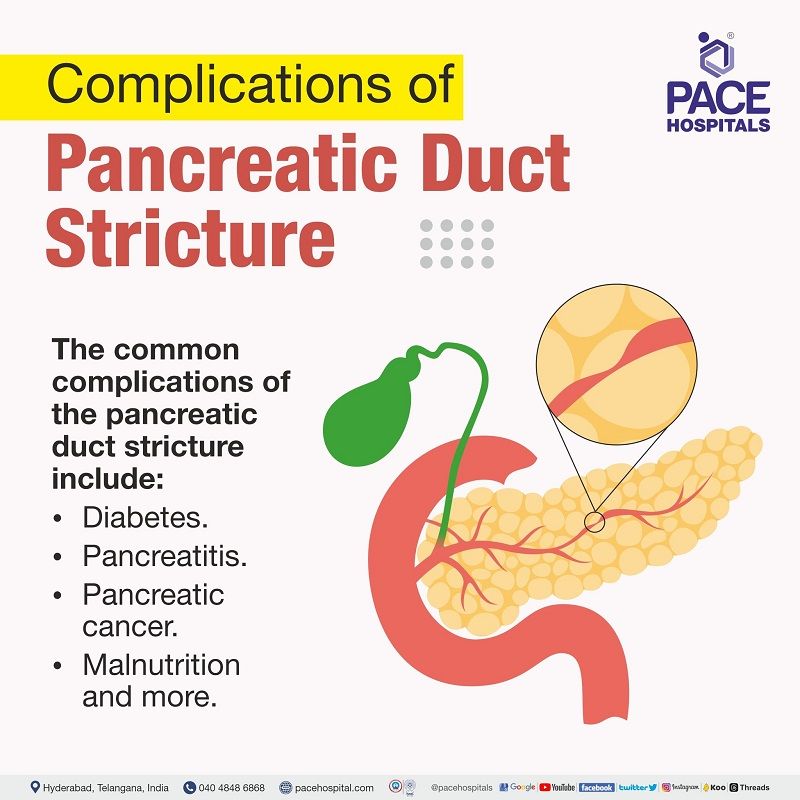
Complications of pancreatic duct stricture
Some of the common complications of the pancreatic duct stricture include:
- Diabetes: Damage to the pancreas makes it unable to regulate blood sugar levels and results in diabetes. By releasing the insulin hormone into the blood stream, the pancreas aids digestion and regulates blood sugar levels. The blood sugar levels increase very high, and may develop diabetes if the pancreas isn't functioning properly or if the body can't utilise the insulin it produces.
- Pancreatitis: Pancreatic duct strictures increase the risk of inflammation and cause pancreatitis.
- Pancreatic cancer: In some circumstances, pancreatic duct stricture leads to pancreatic cancer.
- Malnutrition: Improper absorption of nutrients due to pancreas damage leads to malnutrition.
Pancreatic duct stricture diagnosis
The diagnostic approaches for pancreatic duct stricture are as follows:
- Blood tests: Blood tests are required to identify the elevated pancreatic enzymes and serum markers (IgG4, CA 19-9).
- Imaging tests: Pancreas and pancreatic duct can be seen through imaging examinations. Pancreatic duct strictures can often be identified using the following imaging procedures.
- Endoscopic ultrasonography with fine needle aspiration (EUS-FNA)
- Magnetic resonance cholangiopancreatography (MRCP)
- CT scan (computed tomography scan)
- Endoscopic retrograde cholangiopancreatography (ERCP): A thin, flexible tube with the camera on the end (endoscope) is used during ERCP; it is a minimally invasive technique to view the pancreatic and bile ducts. In order to make the pancreatic duct and bile duct more apparent on X-rays, a contrast dye is injected during ERCP.
The diagnostic approach for pancreatic duct stricture depends on the patient's symptoms, condition and medical history. Sometimes, the
gastroenterologist suggests a combination of diagnostic approaches to diagnose the condition. Imaging studies are typically the first step in diagnosis, followed by endoscopic procedures such as ERCP.
Pancreatic duct stricture treatment
Treatment for pancreatic duct stricture includes medical, endoscopic, and surgical management. The specific conditions of every patient determine the appropriate type of treatment for pancreatic duct strictures. In order to determine the best course of therapy, it is crucial to talk with the gastroenterologist about all the possibilities for treatment.
Medical management
- Pain relievers
- Analgesics
- Pancreatic enzyme supplements
Endoscopic management
- Endoscopic retrograde cholangiopancreatography (ERCP) followed by stent.
- Pancreatic sphincterotomy followed by dilation and pancreatic duct stent placement (PD stent)
- EUS (endoscopic ultrasonography) guided pancreatic duct drainage (EUS‑PD): EUS-guided rendezvous (EUS-RV), EUS-guided pancreatic transmural stenting (EUS-PTS)
Surgical management
Surgical management includes resection procedures, drainage procedures, or a combination of both.
Resection procedures:
- Whipple's procedure
- Distal pancreatectomy
- Duodenum-preserving pancreatic head resection surgeries such as the Beger procedure and Berne procedure
- Total pancreatectomy with islet cell auto-transplantation (In case of high risk of malignancy)
Drainage procedures:
- Lateral pancreatojejunostomy
Combination procedures:
- Frey’s procedure - The type of surgery to be performed is determined by the stricture's aetiology, size, location, and existence of a pancreatic head tumour.

Prevention of pancreatic duct stricture
Preventive measures for pancreatic duct stricture include:
- Abstinence from alcohol and smoking: Alcohol and smoking can aggravate the pancreas and increase the chance of developing pancreatitis.
- Taking a low-fat diet and avoiding fried or fatty foods: A diet low in fat and high in fibre is considered healthful. As pancreatitis is a major contributor to pancreatic duct strictures, taking this helps minimise the risk of developing disease.
- Taking small frequent meals: Eating small, frequent meals is a well-planned approach to treat pancreatic constriction. This is due to the fact that it lowers the pancreas' burden and keeps it from having to create an excessive amount of digesting enzymes all at once.
- Taking pancreatic enzyme supplements for exocrine insufficiency: To aid the body with digestion, pancreatic enzyme supplements are advised to be taken with meals. The enzymes in the supplements aid in the breakdown of carbohydrates, proteins, and lipids.
- Maintaining a healthy weight: Obesity can put more stress on the pancreas and raise the risk of developing pancreatitis.
- Managing underlying comorbidities or medical conditions: The risk of pancreatitis might be increased by illnesses including diabetes and gallstones. In order to lower the chance of pancreatic duct strictures, it is crucial to manage these disorders carefully.
Pancreatic duct stricture vs pancreatic cancer | difference between pancreatic duct stricture and pancreatic cancer
Pancreatic duct stricture and pancreatic cancer are two different conditions that can affect the pancreas. Both pancreatic duct stricture and pancreatic cancer can cause similar symptoms, such as abdominal pain, jaundice (yellowing of the skin and eyes), weight loss, loss of appetite, nausea and vomiting.
| Parameters | Pancreatic duct stricture | Pancreatic cancer |
|---|---|---|
| Definition | Pancreatic duct stricture is a narrowing of the pancreatic duct, the tube that carries digestive enzymes from the pancreas to the duodenum. Pancreatic duct strictures can be caused by a number of factors, such as pancreatitis, pancreatic cancer, pancreatic stones, pancreatic duct cysts, trauma to the pancreas, certain autoimmune diseases. | Pancreatic cancer is a type of cancer that begins in the cells of the pancreas. There are two main types of pancreatic cancer - pancreatic ductal adenocarcinoma and pancreatic neuroendocrine tumors (PanNETs). |
| Benign or malignant | Pancreatic duct stricture is typically a benign condition, meaning that it is not cancerous. However, it can cause significant pain and other symptoms if it is severe. | Pancreatic cancer is a serious and potentially life-threatening malignant condition. It is often diagnosed at a late stage, when it is more difficult to treat. |
| Treatment | Pancreatic duct stricture is often treated with endoscopic stenting procedure, a minimally invasive procedure that involves placing a small tube in the pancreatic duct to keep it open. | Pancreatic cancer is typically treated with surgery, chemotherapy, and radiation therapy. |
Share on
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868