Endoscopic Ultrasound (EUS) Procedure - Test & Cost
At PACE Hospitals, latest endoscopic suite is equipped with world-class endoscopic equipment to perform all types of EUS procedure such as EUS guided biopsy, EUS FNA, EUS guided FNAC, EUS FNB, EUS ERCP etc.
Our team of the experienced gastroenterologist in Hyderabad are having extensive experience in performing Endoscopic Ultrasound - EUS Procedure.
Request an Appointment for EUS Test
EUS Procedure appointment
Why Choose PACE Hospitals for Endoscopic Ultrasound (EUS) ?
State-of-the-art facility with advanced Endoscopic Suite
Team of the best gastroenterologist doctors
Cost-effective treatment with 99.9% success rate
All insurance accepted for cashless treatment facility
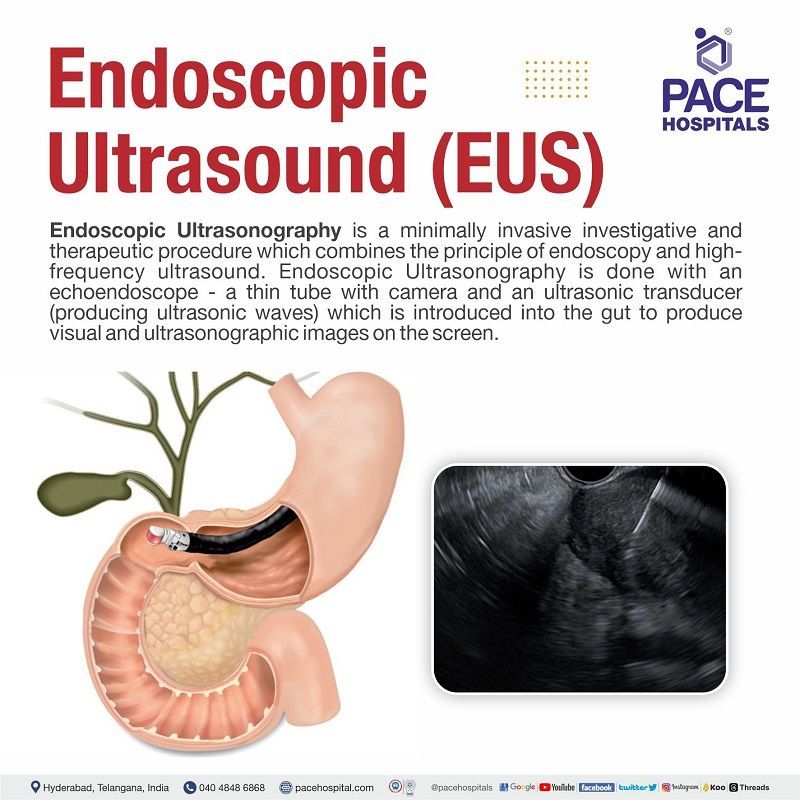
What is EUS?
EUS full form - Endoscopic Ultrasonography
Endoscopic Ultrasonography / Endoscopic Ultrasound is a minimally invasive investigative and therapeutic procedure which combines the principle of endoscopy and high-frequency ultrasound, used to examine the digestive tract and nearby organs.
Endoscopy is a clinical procedure in which a thin tube containing a camera and light is introduced into the gut either through the mouth or through the anus. In endoscopic ultrasonography, a special endoscope called echoendoscope is used. Echoendoscope is incorporated with an ultrasonic transducer into the tip of endoscope. The ultrasound probe at the tip of the endoscope then create images of the surrounding tissues.
EUS Meaning
The EUS medical abbreviation stands for endoscopic ultrasound (EUS), also called EUS endoscopy. The word endoscopy has Greek origins and is an amalgamation of "endo" meaning "within" and the verb "skopein", "to view or observe". Thus, it arrived at the adequate term of “peering into the body” through attaching a camera at the end of the long thin probe.
Sonography can be broken into Greek words “sonos” for sound and “graphia" writing /describing. “Ultra” stands for beyond and subsequently ultrasonography can be termed as the utilisation of sound waves which exist in the frequency beyond the audible range
Endoscopic Ultrasound Uses / indications
EUS uses / indications (endoscopic ultrasound uses) can be broadly divided into two types – therapeutic and investigative, which mainly serve the following objectives.
- Rooting the cause of symptoms.
- Estimating the size of the cancer is and whether it has spread.
- Tissue biopsy of a specific lesions.
- Lodging a stent to open up a blockage etc
Organ-Specific Uses of Endoscopic Ultrasound (EUS)
The endoscopic ultrasound uses differ with various organs and conditions such as:
- EUS oesophagus: endoscopic ultrasonography is mainly used in esophageal cancer EUS staging and esophageal duplication cyst EUS. The use of EUS guided FNA has further improved the accuracy.
- EUS stomach: The main indication of endoscopic ultrasound stomach is the evaluation and staging of carcinoma. Gastric cancer appears as diffuse thickening of the gastric wall on the EUS report.
- EUS bile duct: The endoscopic ultrasound bile duct includes staging of cholangiocarcinoma, detection of common bile duct stones, and evaluation of biliary strictures. The EUS for dilated bile duct usually reveals stone formations. Intraductal ultrasound (IDUS) combined with biopsy increases the accuracy of ERCP for diagnosing EUS biliary stricture (narrowing of bile ducts).
- EUS gallbladder: The endoscopic ultrasound gallbladder is usually done to find gallstones and sludge. Gallbladder can be visualized from the stomach or duodenum. EUS gallbladder drainage is done to treat acute cholecystitis (gallbladder inflammation). Endoscopic ultrasound-guided biliary drainage is widely accepted especially in the cases of biliary drainage with complications. Endoscopic ultrasound gallstones are hyperechoic (increased density of sound waves compared to surrounding structures) in EUS report.
- EUS liver: Endoscopic ultrasound in liver is the gold standard for the diagnosis of parenchymal liver disease. EUS liver biopsy frequently performed by radiologists and is ideal for obese patients suffering from ascites (fluid accumulation in abdomen) or coagulopathy (difficulty in forming clots).
- EUS duodenum: Endoscopic ultrasound in duodenum (first part of small intestine) can be used for predicting depth of duodenal tumour invasion and to analyse outcomes after an endoscopic and transduodenal resection.
- EUS pancreatic duct: The endoscopic transpapillary or transanastomotic pancreatic duct drainage is the most common technique for drainage in the cases of symptomatic pancreatic duct obstruction or leakage.
- EUS pancreas: The combination of endoscopy and ultrasound were initially developed to improve sonographic imaging of the pancreas. EUS has been useful in identifying biliary microlithiasis (small stones in bile duct) in patients with pancreatitis. The endoscopic ultrasound pancreas biopsy remains the most sensitive and specific method in identifying a pancreatic lesion (extra growths on pancreas – could be cancer). In chronic pancreatitis, EUS is done to distinguish between pancreatic carcinoma and chronic pancreatitis.
- EUS intestines: The endoscopic ultrasound is mainly used to find the stage of gastrointestinal stromal tumour, through a contrast-enhanced harmonic endoscopic ultrasonography. EUS has been useful in finding obscure gastrointestinal bleeding, small-bowel tumours, polyposis syndromes. The interventional uses of EUS in intestine include intestinal stent placement, polypectomy, stricture dilation, foreign body retrieval etc.
- EUS Rectum:
Rectal endoscopic ultrasound test is used to evaluate benign rectal villous tumours, anal incontinence (not being able to control bowel movements) etc. Through rectal EUS procedure (anal ultrasound specifically) the identification of perianal abscesses (a swollen area with pus) and complex fistulas is done.
Endoscopic Ultrasound - EUS contraindications
The procedure of endoscopic ultrasound varies with the indication for which it is used. Given below are some of the common contraindications for therapeutic endoscopic ultrasound procedure:
- Haemodynamic instability (insufficient blood flow in the body)
- Severe coagulopathy unable to be reversed (condition of blood's inability to form clots)
- Large volume ascites (fluid collection in the abdomen causing abdominal pain, swelling, etc.)
- Inability to obtain access to the target site.
EUS vs EGD | Difference between EUS and EGD
EUS and EGD are two minimally invasive procedures that are used to diagnose and treat conditions of the digestive tract. Both procedures involve the insertion of a thin, flexible tube through the mouth or nose.
| Elements | EUS | EGD |
|---|---|---|
| Medical abbreviations | Endoscopic Ultrasound | Esophagogastroduodenoscopy |
| Technologies used | Ultrasonography through endoscopy | Videography through endoscopy |
| Modality | Both investigative and therapeutic | Only investigative |
| Uses | Can be used to perform fine needle aspiration (FNA) biopsy, cyst drainage, stent placement, and alcohol ablation | Can be used to remove polyps, stop bleeding, and place stents |
Types of EUS Procedure
The evolution of Endoscopic Ultrasound (EUS) since its conception in the 1980s has continued persistently. Currently, various procedures of EUS are at the forefront of gastroenterological procedures, helping in both diagnostic and therapeutic use for various diseases and clinical presentations. The following list contains a few of the common types of EUS procedures:
- EUS guided biopsy: The endoscopic ultrasound guided biopsy is a procedure of taking a small sample of lesion/tissue (gut), which can be sent for analysis. In this investigative procedure, the principles of endoscopic ultrasound - EUS and biopsy both are combined.
- EUS FNA: Endoscopic ultrasound fine-needle aspiration (EUS FNA) (also called EUS guided FNAC or endoscopic ultrasound guided FNAC) is a procedure to obtain the cells of the gastrointestinal tract and abdomen at different locations. This EUS procedure (EUS guided FNAC procedure) is usually done once an unusual tissue mass is discovered through other diagnostic imaging methods.
- EUS FNB: The Endoscopic ultrasound guided-fine needle biopsy (EUS FNB) procedure is used to obtain tissue samples, which cannot be obtained from EUS FNA.
- EUS guided cystogastrostomy: After pancreatic injury, pancreatic pseudocysts (collections of leaked pancreatic fluids during pancreatitis) are commonly seen, which are usually resolved with supportive treatment. Nevertheless, if there is a failure in the treatment, cystogastrostomy has to be performed. Earlier open standard procedure was the norm, but with modern endoscopes, EUS guided cystogastrostomy was possible to safely drain the pseudocysts using minimal access techniques.
- EUS guided gastrojejunostomy: The clinical syndrome - gastric outlet obstruction (GOO) has symptoms of gut obstruction (could be at the distal stomach or starting part of the intestine), which could be due to a variety of disorders such as peptic ulcer, gastric cancer etc. Conventionally, surgical gastrojejunostomy was the 1st choice of treatment, but high rates of morbidity and mortality made EUS guided gastrojejunostomy the better alternative.
- EUS gallbladder drainage: A recent treatment for acute cholecystitis (gallbladder inflammation) in high-risk patients, originated in 2007, is the EUS guided gallbladder drainage (EUS-GBD). Currently, it has a clinical and technical success rate of 100% and 97%, respectively.
- EUS angiotherapy: The EUS-guided angiotherapy is a growing procedure which allows the targeted delivery of intravascular therapies to blood vessels (mainly to veins) and real-time confirmation of thrombosis (blood clot formation). It is a technically feasible, safe, and effective procedure for managing the bleeding of a variety of gastrointestinal lesions.
- EUS bronchoscopy: The endoscopic ultrasound with bronchoscope-guided fine needle aspiration (EUS-B-FNA) is a diagnostic procedure to obtain cells of suspected lung cancer located in the paraesophageal region. The result of EUS-B-FNA adds value to bronchoscopy and endobronchial ultrasound (EBUS).
- EUS guided LAMS: Lumen-apposing metal stents (LAMS) are some of the common tools which are deployed with endoscopic ultrasound guidance for draining the fluid collected in the abdominal region, decompressing any obstructed ductal systems, the establishment of anastomosis (the surgical connection between two structures) to facilitate any necessary endoscopic interventions. With the usage of EUS-guided LAMS, the potential for leak and perforation is minimised.
- CEUS/CH EUS: An amalgamation of two technologies, i.e., contrasting agents and ultrasonography, the contrast-enhanced endoscopic ultrasound (CEUS or CH EUS) provides detailed, accurate images of internal organs. This EUS test (CEUS) has the potential to replace MRI scans or CT scans of various organs such as the kidneys, liver, bladder, etc.
- EUS ERCP: The endoscopic ultrasound-guided endoscopic retrograde cholangiopancreatography – ERCP is usually the first choice for the treatment of various pancreaticobiliary duct diseases, especially in patients who underwent surgery resulting in the alteration of internal organs of the gut. EUS ERCP is the primary choice in these cases as ERCP proved to be challenging. Billroth II and Roux-en-Y gastric bypass (RYGB) are a couple of surgeries which leave the patient’s internal anatomy altered. It is called surgically altered anatomy (SAA).
- EUS PBD: The endoscopic ultrasound guided pancreaticobiliary drainage (also called the EUS-guided pancreaticobiliary drainage) is primarily a therapeutic procedure to access the pancreatic or biliary system using an EUS needle. This procedure is used especially in surgically altered anatomy (SAA) patients as the pancreaticobiliary access is done transmurally (passing through the walls of) either the stomach or proximal duodenum.
- EUS BD: The endoscopic ultrasound guided biliary drainage (also called the EUS guided biliary drainage or EUS biliary drainage) was first published in 2001 for the treatment of obstructive jaundice (jaundice developed due to either a narrowed or blocked bile or pancreatic duct, which prevents the bile drainage into the intestines. In many cases, the common bile duct is dilated). EUS BD is an alternative for various therapeutic procedures such as laparoscopic-assisted ERCP, enteroscopy-assisted ERCP, and percutaneous transhepatic biliary drainage.
- EUS guided gastroenterostomy: One of the technically demanding techniques in endoscopic ultrasonography (EUS) is the EUS-guided gastroenterostomy. This procedure is utilised in cases such as malignant gastric outlet obstruction (mechanical obstruction of the duodenum due to blockage by impending cancer) or in bariatric surgery in morbidly obese patients.
- EUS biopsy pancreas: Stands for endoscopic ultrasound pancreas biopsy. For pancreatic solid lesions, endoscopic ultrasound guided sampling is used as a first-line procedure to establish a diagnosis. EUS guided FNAC pancreas has better accuracy over other imaging procedures as it can detect lesions <3 cm.
- EUS guided liver biopsy: Endoscopic ultrasound guided liver biopsy (EUS-LB) is a sample-procuring technique which is an effective alternative to various traditional methods of getting liver tissue for tests. Apart from an improved safety profile, EUS guided liver biopsy has various advantages over guided percutaneous and fluoroscopy guided transjugular routes of biopsy.
- EUS biopsy lymph node and EUS lung biopsy: The staging of the mediastinal lymph node is necessary in order to consider the optimal treatment strategy for lung cancer. In such cases of mediastinal lymphadenopathy, the endoscopic ultrasound-guided transesophageal fine needle aspiration (FNA) procedure is the only remaining alternative apart from surgical intervention.
- EUS adrenal biopsy: While the conventional image-guided fine-needle aspiration (FNA) performed through ultrasonography could deliver at times non-diagnostic samples, the endoscopic ultrasound (EUS)-guided FNA of the adrenal gland is less invasive but provides a more accurate method to obtain samples of adrenal with a few adverse effects and complications.
- Rectal EUS: Historically, the endoscopic ultrasound of the lower gastrointestinal tract was limited to the anal canal and rectum, as the liner and radial echoendoscopes are side-viewing instruments. The recently introduced forward-viewing linear echoendoscopes allow for ultrasound evaluation of not only the rectal EUS procedure but also the entire colon, as they can be advanced under direct vision and have the capacity for tissue acquisition via FNA or FNB.
- EUS colonoscopy: Lesions can be discovered during colonoscopy. Through endoscopic ultrasound colonoscopy (EUS colonoscopy), an ideal investigation can be done which provides an accurate diagnosis of these lesions either by flexible mini-probes or the more recently introduced forward-viewing radial echoendoscope.
- EUS-Trucut biopsy (EUS-TCB): Once the location of lesions in the colon are located through EUS colonoscopy, to understand the nature of the lesion, either EUS-FNA or EUS-Trucut biopsy (EUS TCB) is performed. This reveals the cytological or histological confirmation of the tumour.
- EUS rendezvous: The EUS guided rendezvous procedure (EUS RV) is an alternative procedure used in endoscopic retrograde cholangiopancreatography (ERCP) especially if the deep biliary cannulation is failed. Through this rendezvous technique, the biliary drainage is salvaged by the EUS.
EUS Procedure
Before the EUS procedure - Endoscopic ultrasound preparation
Since there are various types of EUS procedures, the patients may be presented with various types of pre-procedural steps. Given below is a general set of instructions for EUS procedures.
- The patient undergoing EUS procedures will be given the exact instructions by the healthcare team.
- It could be an inpatient or outpatient procedure, depending on the type of EUS procedure the patient is prescribed.
- The patient is strictly to remain NPO (nil per os in Latin which means nothing to be taken through mouth) for at least 6–8 hours pre-procedure. Solid food is to be avoided for 6–8 hours.
- The patient can drink sips of water, but should refrain from 2 hours before the appointment.
- The healthcare team may prescribe a few antibiotics as a prophylaxis, especially in high-risk patients (such as diabetics, etc), to avoid any infection from possible complications.
- The healthcare team reviews the medicines the patient takes and may alter the prescription for a few days to conduct the EUS procedure.
During the EUS procedure
- Heart rate measurements and blood pressure readings are noted. The patients may be asked about their allergies.
- After explaining everything about the EUS procedure, the patient is presented with a consent form for signing. Spectacles/jewellery etc. are to be removed.
- The EUS procedure is usually done within 30 minutes. Sophisticated procedures may be longer.
- Post consent, the patient is expected to change into a hospital gown in many hospitals.
- A plastic guard kept the patient's mouth to protect the teeth from the endoscope.
- Depending on your gag reflex among various other priorities, the endosonographer may or may not provide you with anaesthesia. Usually, it is dependent on the health status of the patient. General anaesthesia may complicate the procedure by inducing respiratory distress among other side effects which is why only after careful consideration, the sedatives are provided.
- In case the general anaesthesia is not given, a local anaesthesia is sprayed on the throat to allow the smooth passage of the endoscope by numbing the upper oesophagus.
- The endoscope is passed through the mouth and subsequently, images are visualised on the screen. Once the EUS procedure is finished, the endoscope is gently removed.
After the EUS procedure
- A little bit of bloating and discomfort may be endured after the endoscopy, which goes away after a few hours.
- Eating or drinking will not be possible until the local anaesthetic spray has worn off in an hour.
- The patient can return home if not sedated. In case of a sedated EUS procedure, the patient needs to stay back till the drowsiness wears off or can be assisted by friends or family.
Endoscopic Ultrasound - EUS complications
There are various types of EUS side effects and major complications associated with various procedures linked with investigation or therapy. The common EUS FNA complications are:
- Haemorrhage (blood loss)
- Perforation (rupture or hole especially through the gut)
- Infection (usually due to perforation)
- Needle tract seeding (spread of cancer to other areas through contaminated needle)
- Organ-specific complications, such as
- Acute pancreatitis (pancreas inflammation) due to puncture at pancreatic lesions.
- Fatal haemorrhage due to duodenal perforation (hole at starting part of small intestine) could be one of the common complications leading to death, which could occur after the EUS-FNA procedure.
FAQs of patient after the EUS procedure
- What are the risks of EUS?
- What should I expect after EUS?
- When will I get my results?
- What are the possible complications of EUS?
- Is there anything else I should know about EUS?
- What will happen if I experience any complications? Whom to contact?
- When will the sedation wears off?
- Will I be able to eat or drink after the procedure?
- What are the next steps after the procedure?
- What are the possible findings of the EUS?
- What will the findings mean for my treatment plan?
- What are the chances of a positive biopsy?
- What are the next steps if the biopsy is positive?
EUS vs ERCP | Difference between EUS and ERCP
EUS (Endoscopic Ultrasound) and
ERCP (Endoscopic Retrograde Cholangiopancreatography) are both minimally invasive endoscopic procedures that are used to diagnose and treat conditions of the gastrointestinal (GI) tract and nearby organs, particularly related to the pancreas, bile ducts, and adjacent structures. Both procedures involve the insertion of a thin, flexible tube through the mouth.
| EUS (Endoscopic Ultrasound) | ERCP (Endoscopic retrograde cholangiopancreatography) |
|---|---|
| Ultrasonography through endoscopy | X-rays through endoscopy |
| Can be used to perform fine needle aspiration (FNA) biopsy, cyst drainage, stent placement, and alcohol ablation | Exclusively in the treatment of bile and pancreatic duct problems, can be used to remove gallstones, open narrowed ducts, and place stents |
EBUS vs EUS | Difference between EBUS and EUS
EBUS (Endobronchial Ultrasound) and EUS (Endoscopic Ultrasound) are two different medical procedures that are used for diagnosing and staging diseases, particularly those affecting the chest and gastrointestinal tract, respectively.
| EBUS (Endobronchial Ultrasound) | EUS (Endoscopic Ultrasound) |
|---|---|
| EBUS is a minimally invasive procedure used to evaluate and diagnose conditions within the airways and structures near the lungs, such as lymph nodes and tumors. | EUS is a minimally invasive procedure used for imaging and diagnosing conditions in the gastrointestinal (GI) tract and adjacent structures, such as the pancreas, liver, bile ducts, and lymph nodes. |
| It involves the use of a bronchoscope with an ultrasound probe attached to its tip. This allows the doctor to see real-time ultrasound images of the structures in and around the bronchial tubes. | It involves the use of an endoscope equipped with an ultrasound transducer at its tip. This allows for high-resolution imaging of the GI tract and surrounding tissues. |
| EBUS is commonly used to diagnose lung cancer, assess lymph nodes for metastasis, and identify other pulmonary diseases. | EUS is used for a variety of purposes, including the evaluation of pancreatic tumors, the staging of esophageal and gastric cancers, the assessment of gallbladder and bile duct diseases, and the sampling of lesions for biopsies. |
| EBUS is typically performed by pulmonologists and is a valuable tool for determining the extent of lung cancer and guiding the sampling of tissue for biopsy. | EUS is typically performed by gastroenterologists or interventional endoscopists. |
MRCP vs EUS | Difference between MRCP and EUS
MRCP (Magnetic Resonance Cholangiopancreatography) and EUS (Endoscopic Ultrasound) are medical imaging and diagnostic procedures used to evaluate the bile ducts, pancreatic ducts, and surrounding structures in the abdomen.
| MRCP (Magnetic Resonance Cholangiopancreatography) | EUS (Endoscopic Ultrasound) |
|---|---|
| MRCP is a non-invasive imaging technique that uses magnetic resonance imaging (MRI) to create detailed images of the bile ducts, pancreatic duct, and surrounding anatomy. | EUS is another endoscopic procedure that utilizes ultrasound technology for imaging the gastrointestinal tract and adjacent structures. |
| It is used primarily for diagnostic purposes and is particularly useful for evaluating biliary and pancreatic disorders without the need for invasive procedures. | It provides high-resolution images and is useful for evaluating the pancreas, liver, bile ducts, lymph nodes, and nearby blood vessels. |
| MRCP can provide information about the presence of stones, strictures, tumors, and other abnormalities in the bile and pancreatic ducts. | EUS is valuable for diagnosing and staging various GI and pancreatic diseases, as well as for guiding fine-needle aspiration (FNA) biopsies. |
| It does not involve any insertion of instruments or contrast agents into the body and is often preferred when there is a need for non-invasive evaluation. | It is a versatile procedure that can provide detailed information about the anatomy and pathology of the upper GI tract. |
EUS Test Cost in Hyderabad, India
Endoscopic Ultrasound price in Hyderabad generally ranges from ₹18,000 to ₹42,000 (approximately US $215 – US $505).
The exact endoscopic ultrasound cost varies depending on factors such as whether it is a diagnostic EUS or EUS-guided biopsy/FNA, the organ being evaluated (pancreas, stomach, esophagus, bile duct, rectum), the need for contrast or Doppler imaging, the complexity of the case, endoscopist expertise, and the hospital facilities chosen including cashless treatment options, TPA corporate tie-ups, and assistance with medical insurance approvals wherever applicable. Cost Breakdown According to Type of Procedure
- Diagnostic Endoscopic Ultrasound (Upper GI / Lower GI) – ₹18,000 – ₹28,000 (US $215 – US $335)
- EUS-Guided Biopsy / Fine Needle Aspiration (FNA) – ₹25,000 – ₹35,000 (US $300 – US $420)
- EUS for Pancreatic/Biliary Evaluation – ₹28,000 – ₹40,000 (US $335 – US $485)
- EUS-Guided Cyst Drainage / Therapeutic EUS – ₹30,000 – ₹42,000 (US $360 – US $505
Frequently Asked Questions (FAQs) on Endoscopic Ultrasound (EUS)