Liver Cirrhosis – Symptoms, Causes, Complications and Prevention
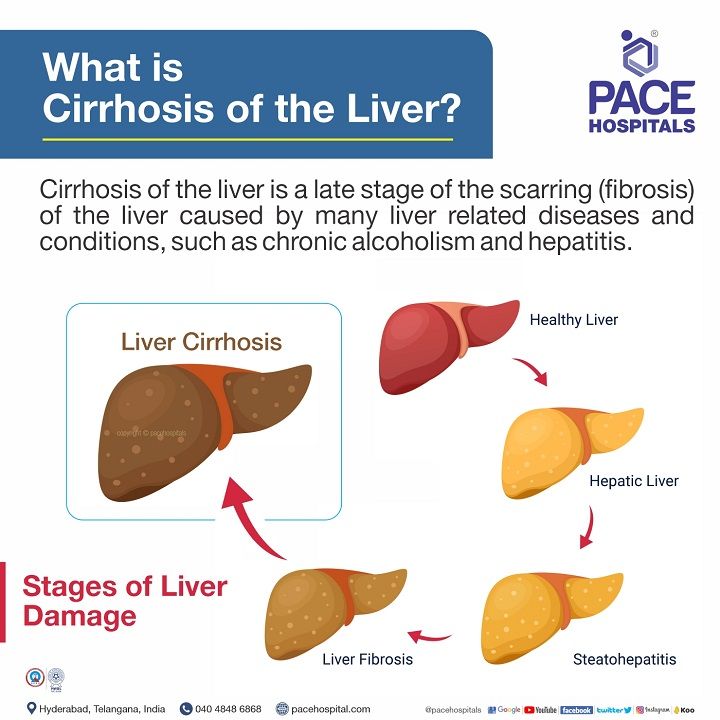
Cirrhosis of the liver is a late stage of the scarring (fibrosis) of the liver caused by many liver related diseases and conditions, such as chronic alcoholism and hepatitis. The liver performs several necessary functions, including harmful detoxifying substances in your body, cleaning your blood and making vital nutrients.
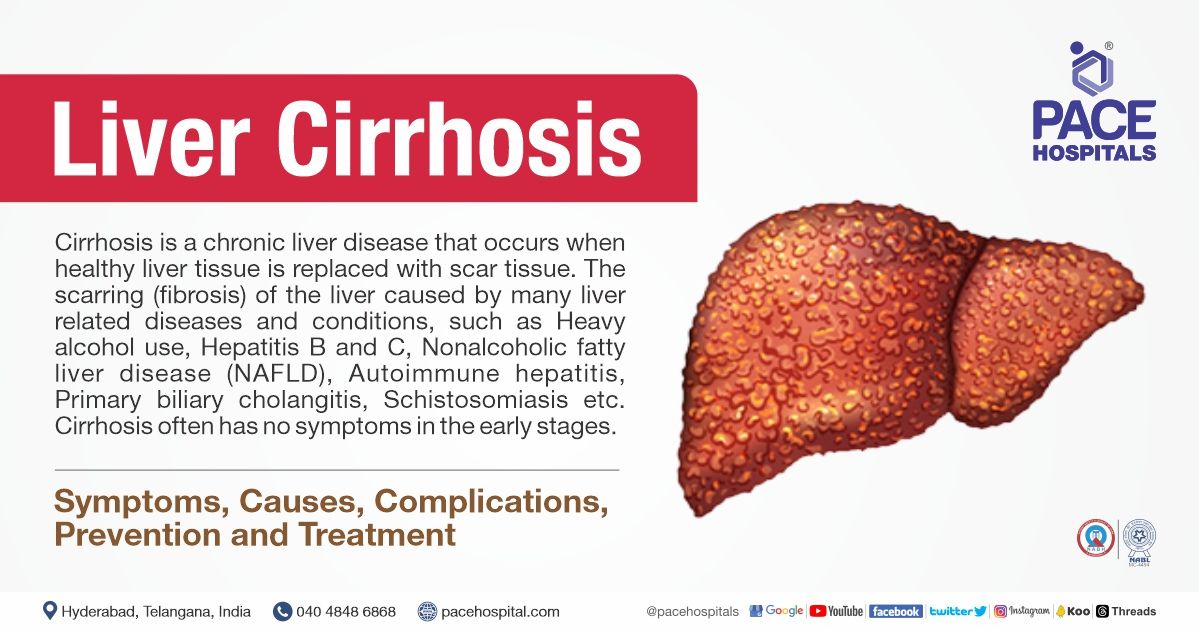
What is Liver cirrhosis?
Cirrhosis is a complication of many
liver related diseases characterized by abnormal structure and function of the liver. The diseases that lead to cirrhosis of the liver do so because they injure and kill liver cells, after which the inflammation and repair that is associated with the dying liver cells causes scar tissue to form.
The liver cells that do not die multiply in an attempt to replace the cells that have died. This results in clusters of newly-formed liver cells (regenerative nodules) within the scar tissue. There are many causes of liver cirrhosis including chemicals (such as alcohol, fat, and certain medications), viruses, toxic metals (such as iron and copper that accumulate in the liver as a result of genetic diseases), and autoimmune liver disease in which the body's immune system attacks the liver.
Types of Liver Cirrhosis
Liver cirrhosis can be divided into two types depending on its morphology (form) and aetiology (causes).
Under Morphologic classification; cirrhosis of the liver are of 3 types:
- Micronodular cirrhosis
- Macronodular cirrhosis
- Mixed cirrhosis
Under Aetiologic classification, cirrhosis of the liver is of 12 types:
- Alcoholic cirrhosis (the most common, 60-70%)
- Post-necrotic cirrhosis (10%)
- Biliary cirrhosis (5-10%)
- Pigment cirrhosis in haemochromatosis (5%)
- Cirrhosis in Wilson’s disease
- Cirrhosis in α-1-antitrypsin deficiency
- Cardiac cirrhosis
- Indian childhood cirrhosis (ICC)
- Cirrhosis in autoimmune hepatitis
- Cirrhosis in non-alcoholic steatohepatitis
- Miscellaneous forms of cirrhosis (metabolic, infectious, gastrointestinal, infiltrative) diseases
- Cryptogenic cirrhosis
Signs and Symptoms of Liver Cirrhosis
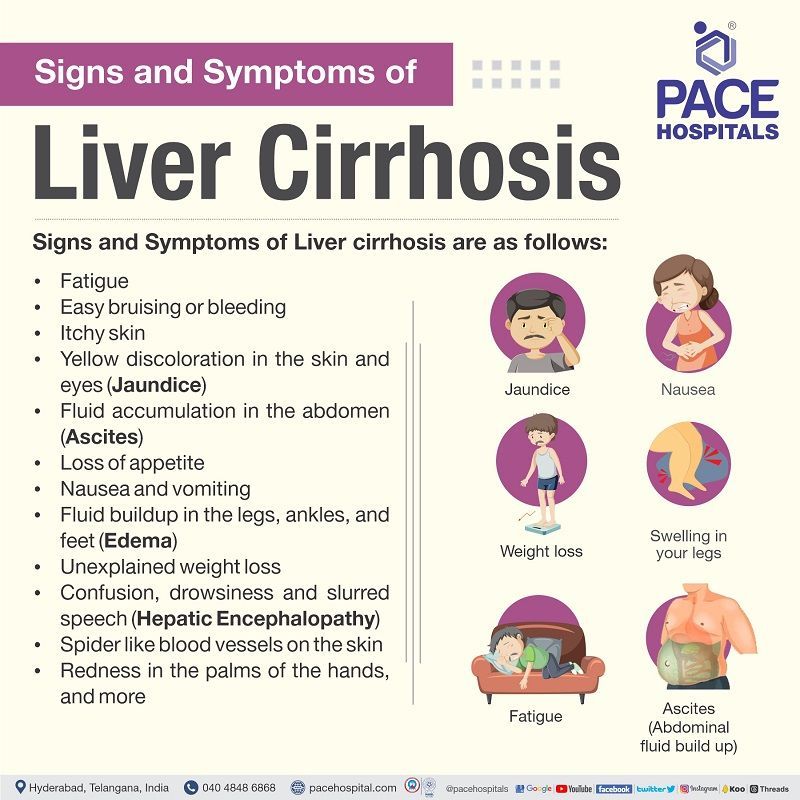
Individuals with cirrhosis of the liver may have few or no symptoms and signs of
liver related disease. Some of the symptoms may be nonspecific, that is, they don't suggest that the liver is their cause. Some of the more common signs and symptoms of liver cirrhosis include:
- Fatigue
- Bleeding easily
- Bruising easily
- Itchy skin
- Yellow discoloration in the skin and eyes (jaundice)
- Fluid accumulation in your abdomen (ascites)
- Loss of appetite
- Nausea
- Swelling in your legs
- Weight loss
- Confusion, drowsiness and slurred speech (hepatic encephalopathy)
- Spiderlike blood vessels on your skin
- Redness in the palms of the hands
- Testicular atrophy in men
- Breast enlargement in men
Causes of Liver Cirrhosis
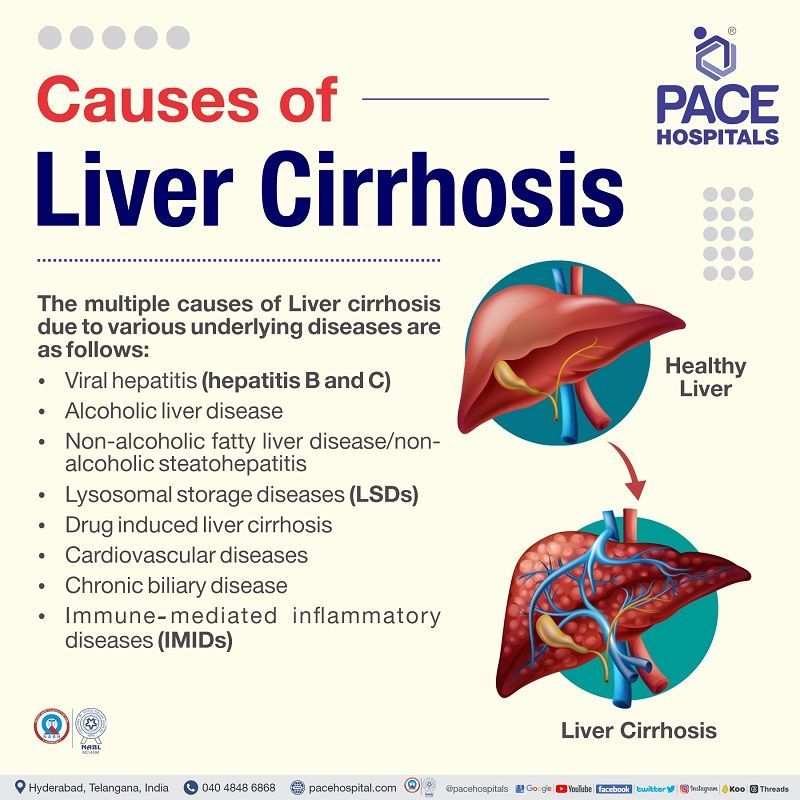
The liver is one of the primary organs in the body, the cause of cirrhosis of the liver can start from any abnormality in the normal physiology of the body. The cause of liver cirrhosis need not have a linear origin. The multiple liver cirrhosis causes due to various underlying diseases such:
- Viral hepatitis (hepatitis B and C)
- Alcoholic liver disease
- Non-alcoholic fatty liver disease/non-alcoholic steatohepatitis
- Lysosomal storage diseases (LSDs) - Hemochromatosis, Wilson's disease, Alpha1-antitrypsin deficiency, Type IV glycogen storage disease (Andersen disease)
- Immune‐mediated inflammatory disease (IMID) - Autoimmune hepatitis (types 1, 2, and 3), Primary biliary cholangitis, Primary sclerosing cholangitis, Immunoglobulin G4 cholangiopathy
- Cardiovascular disease - Venous outflow obstruction, Chronic right-sided heart failure, Hereditary haemorrhagic telangiectasia (Osler-Weber-Rendu disease), Tricuspid regurgitation
- Chronic biliary disease - Recurrent bacterial cholangitis, Bile duct stenosis
- Other - Medications (e.g., methotrexate, amiodarone), Erythropoietic protoporphyria, Granulomatous disease (e.g., Sarcoidosis), Schistosomiasis
Viral hepatitis (hepatitis B and C): When a virus damages hepatocytes, inflammatory cells are deregulated, which can cause an increase in the build-up of excessive metabolites. Increased levels of toxic metabolites activate the hepatic stellate cells, creating an abnormally high extracellular matrix as a defence or compensatory mechanism. The increase of extracellular matrix causes fibrosis, and liver cirrhosis follows if the insult is still prolonged.
Alcoholic liver disease (ALD): One of the common causes of liver cirrhosis and liver failure, which includes a broad spectrum of disorders (such as steatosis and acute alcoholic hepatitis) with or without cirrhosis of the liver. Liver cancer is a cirrhotic complication.
Non-alcoholic fatty liver disease (NAFLD) / non-alcoholic steatohepatitis (NASH): Non-alcoholic fatty liver disease is a hepato-metabolic syndrome risk factor for various metabolic diseases such as type 2 diabetes, dyslipidaemia, and hypertension. The progression of NAFLD includes simple steatosis to non-alcoholic steatohepatitis (NASH), leading to cirrhosis of the liver or hepatocellular cancer.
Lysosomal storage diseases (LSDs): These diseases occur due to inherited metabolism defects characterised by issues in the accumulation of storage material in the body.
- Hemochromatosis: Excess iron build-up in the body to harmful levels and can cause liver cirrhosis due to the deficiency of pyruvate kinase, causing easy rupture of blood cells (haemolytic anaemia).
- Wilson's disease: Wilson's disease, if left untreated, can cause liver cirrhosis characterised by impaired hepatic synthesis, reduced white cells, and thrombocytes.
- Alpha1-antitrypsin deficiency: A common inherited cause of protein-folding disorder resulting in liver cirrhosis.
- Type IV glycogen storage disease (Andersen disease): In patients with Andersen disease, abnormal glycogen is created, which has the potential to trigger the body's immune system resulting in the scarring (cirrhosis) of various organs such as the liver, muscle and the heart.
Immune‐mediated inflammatory disease (IMID): An attack by the immune system against hepatocytes which are mediated by diverse mechanisms, results in primary biliary cirrhosis, primary sclerosing cholangitis or autoimmune hepatitis.
- Autoimmune hepatitis: Untreated autoimmune hepatitis may result in liver scarring (cirrhosis) and liver failure. If diagnosed and recognised early, immune-suppressing medicines can be used to treat autoimmune hepatitis.
- Primary biliary cholangitis, primary sclerosing cholangitis: Damaged bile ducts can damage liver cells by blocking the transfer of bile piling up into the liver. Slow damage to liver cells can cause cirrhosis of the liver and, eventually, liver cancer.
- Immunoglobulin G4-cholangiopathy: A bile duct disorder due to an attack of immunoglobulins. While steroids can be given to treat, any delay can result in fibrosis, organ dysfunction and failure, venous thrombosis, portal hypertension, liver cirrhosis, and mortality.
Cardiovascular diseases: Hepatic problems caused by cardiac malfunction are called cardiac cirrhosis (particularly in the right heart chambers). Valvular disease, severe pulmonary hypertension, biventricular heart failure, pericardial disorders, cardiac tamponade, and constrictive pericarditis may induce cardiac cirrhosis.
- Venous outflow obstruction: Obstruction of the hepatic vein (such as Budd-Chiari syndrome, venous-occlusive disease) blocks the hepatic vein, which upon worsening and leads to liver cirrhosis and, ultimately, liver failure.
- Chronic right-sided heart failure: Right-sided heart dysfunction can increase the back pressure to the hepatic system and preload. Stress on the hepatic system can induce hepatic congestion. Long-standing hepatic congestion eventually leads to liver cirrhosis.
- Hereditary haemorrhagic telangiectasia (Osler-Weber-Rendu disease): A rare disorder characterised by epistaxis (bleeding from the nose) commonly affecting the liver. This disorder's liver disease can manifest as a high-output cardiac failure, portal hypertension and liver cirrhosis.
- Tricuspid regurgitation: Valve disorders such as tricuspid regurgitation, mitral stenosis, left-sided heart failure, or reduced cardiac relaxation can cause right-sided heart dysfunction. Right-sided heart dysfunction can increase the back pressure to the hepatic system and preload. Stress on the hepatic system can induce hepatic congestion. Long-standing hepatic congestion eventually leads to liver cirrhosis.
Chronic biliary disease
- Recurrent bacterial cholangitis: The chronic bacterial infection of the biliary tree causing primary hepatolithiasis (multiple intraductal stones). Due to bile blockage, it is piled up in the liver causing cirrhosis and cancer.
- Bile duct stenosis: narrowing the bile duct also causes occlusion of bile in the liver causing cirrhosis and cancer.
Other miscellaneous causes
- Erythropoietic protoporphyria: results in liver disease (cirrhosis) due to the deposition of insoluble protoporphyrin IX in liver cells.
- Granulomatous disease (e.g., Sarcoidosis): granulomatous hepatitis (e.g., Sarcoidosis), depending on the severity, can further progress to fibrosis, cirrhosis or portal hypertension. Early diagnosis and appropriate therapy (at times lifelong) can prevent significant hepatic dysfunction or fatal infection.
- Schistosomiasis: an infection of trematodes (Schistosoma), which deposits eggs in the small portal venules resulting in periportal fibrosis and liver cirrhosis.
- Drug-induced liver cirrhosis (e.g., antimetabolites such as methotrexate, antiarrhythmics such as amiodarone)
Risk factors of Liver Cirrhosis
There are various risk factors which can increase the chances of liver cirrhosis, such as:
- Alcoholism
- Viral hepatitis
- Diabetes
- Unhealthy body mass index (BMI)
- Gender
- Malnutrition
Alcoholism: A study showed that individuals having 1-7 drinks/per week are less likely to get contracted liver cirrhosis when compared with individuals having more than seven drinks per week. Intermittent drinking for a long duration is less harmful as the liver is given a chance to recover. The alcohol content in an alcoholic beverage is provided on the container's label. Still, in general, it is about 4-6% in beer, 10-12% in wine, and about 40-50% in brandy, whisky and scotch.
Viral hepatitis: Injecting drugs using shared needles and unprotected sex can cause viral hepatitis. Concurrent viral infection in a chronically alcoholic individual leads to the development of alcoholic liver disease even with much less alcoholconsumption (20-50 g/day).
Diabetes: Around 30% of cirrhotic individuals have diabetes, which increases the mortality in these patients. The risk of liver cirrhosis is higher in people with type 2 diabetes, even in patients with healthy BMI.
Unhealthy BMI (overweight 25- <30 and obese ≥30): Non-alcoholic fatty liver disease (NAFLD) is a liver condition characterised by fatty infiltration with or without inflammation (non-alcohol steatohepatitis or NASH). Although obesity may strike as a harmless annoyance in the path of liver cirrhosis, long-standing obesity may proceed to fibrosis, eventually liver cirrhosis and ultimately liver cancer. Obesity, type 2 diabetes, hypertension, and hypertriglyceridemia are all linked to the development of NASH and fibrosis. European and American research reflected that NAFLD affects 3-30% of the population.
Gender: Women have increased susceptibility to developing advanced alcoholic liver disease, even with much lesser alcohol intake (20-40 g/day). This gender difference in diseaseprogression is unclear, but could be linked to the effects of oestrogen.
Malnutrition: Absolute or relative malnutrition of proteins and vitamins contributes to the evolution of liver cirrhosis. The combination of chronic alcoholingestion and impaired nutrition leads to alcoholic liver disease. It appears that calories from alcohol displace other nutrients, leading to malnutrition and deficiency of vitamins in alcoholics. Additional factors contributing to malnutrition in alcoholics are chronic gastritis and pancreatitis. The evidence favouring the synergistic effect of malnutrition in chronic alcoholism comes from clinical and morphologic improvement in cases of alcoholic cirrhosis on treatment with protein-rich diets.
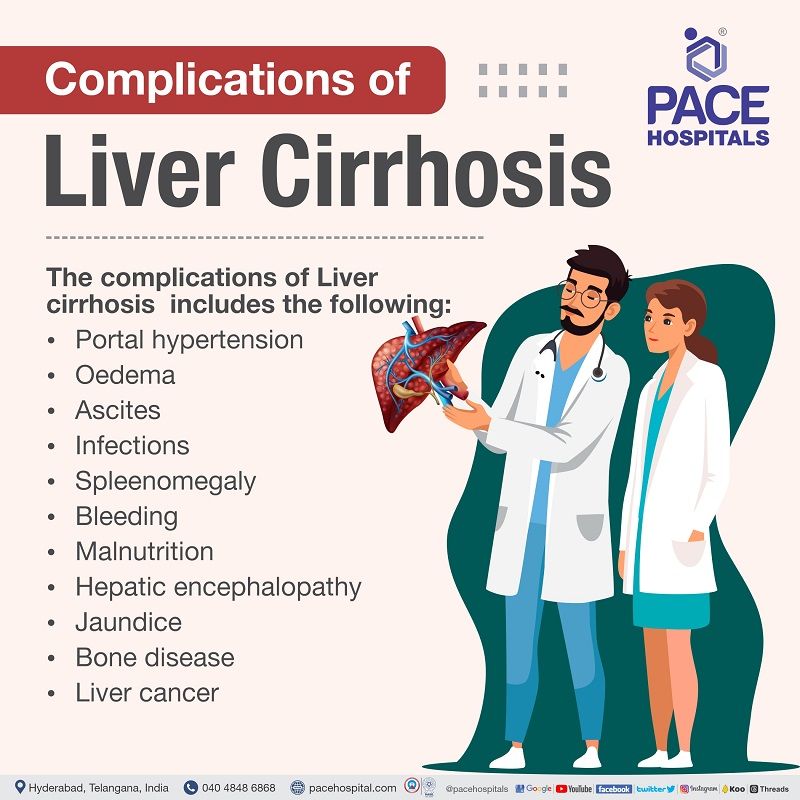
Complications of Liver Cirrhosis
Cirrhosis of the liver can increase the risk of various complications, leading to increased patient mortality risk. The multiple complications of liver cirrhosis can include:
- Portal hypertension (high blood pressure in the veins supplying the liver).
- Oedema (swelling in the legs and abdomen).
- Ascites (accumulation of fluid in the abdomen).
- Infections (due to reduced WBC, the patient is easily infected).
- Splenomegaly (enlargement of the spleen and reduced lymphocytes).
- Bleeding (portal hypertension creates pressure in veins which can burst and bleed).
- Malnutrition (due to difficulty in processing nutrients, cachexia and weakness is seen).
- Hepaticencephalopathy (toxins build up in the brain as impaired liver can’t clear them).
- Jaundice (increased bile levels in the bloodcausing yellowing of the skin).
- Bone disease (cirrhotic patients may lose bone strength and therefore are at greater risk of fractures).
- Increased risk of
liver cancer
Why does cirrhosis cause discomfort?
The liver is one of the body's most important organs performing many vital roles, such as the production of the body’s essential substances for its smooth maintenance (such as clotting proteins for blood clotting in emergencies). Getting rid of harmful substances that can be toxic to the body and ensuring the body has enough glucose (sugar) and lipids (fat) to use as fuel are also a few other important roles taken up by the liver.
To perform these aforementioned jobs, the hepatocytes (liver cells) must be healthy and close to the blood, as only through the blood can the substances be added by or removed from the liver.
To understand liver cirrhosis causes discomfort, its physiology and pathophysiology must be understood in brief.
The hepatic circulation:
A unique relationship can be seen between the liver to its blood supply. Unlike other organs, which receive blood from the heart, the liver receives just a limited amount of blood through arteries from the heart as most of the supply comes from the intestinal veins as the blood returns to the heart.
The portal vein is the major vein that transfers blood from the intestines to the liver by dividing into smaller and smaller veins (also known as sinusoids). These sinusoids line up with the hepatocytes. The interaction between the sinusoids and the hepatocytes facilitates the removal or addition of compounds to the blood.
After passing through the sinusoids, the blood is gathered in progressively bigger veins that eventually form a single vein. This hepatic vein returns the blood from liver to the heart for it to circulate to the body.
Bile duct cannulation (the bile gateway):
Bile is a fluid generated by liver cells that, apart from aiding digestion, also removes toxins from the body. Bile is generated by hepatocytes and is released into canaliculi (very small channels running between hepatocytes lining with sinusoids). The canaliculi drain into bigger ducts, which ultimately merge to produce a single bile duct that drains bile into the small intestine. Thus, bile transported into the gut aid in digesting meals (especially fats). Simultaneously, hazardous chemicals contained in the bile are absorbed by the colon and subsequently removed by faeces.
The impaired circulation (Chaos and destruction):
In liver cirrhosis, the unique relationship between blood and hepatocytes is destroyed, which makes it harder for the hepatocytes to add or remove substances from the blood. Scarring in liver tissue (fibrosis) also makes it hard for blood to transverse through the liver and to the hepatocytes.
As the blood flow through the liver is blocked, it is accumulated in the portal vein, increasing its pressure (portal hypertension). The pressure build-up in the portal vein makes the blood search for other low-pressured veins to return to the heart.
Since the blood flow is now redirected, the liver can't add or remove substances. Many signs and symptoms of liver cirrhosis are caused by fewer hepatocytes liver cells, less contact between the blood going through the liver and its cells, and blood that goes around the liver.
Damaged cannulation (the yellow ruins):
Apart from the damages raised due to altered blood path, another source of the complications induced by liver cirrhosis is the abnormal connection between the liver cells and the bile ducts.
Cirrhosis is characterised by aberrant canaliculi, the destruction of the interaction between liver cells and canaliculi, and the relationship between liver cells and blood in the sinusoids.
Consequently, the liver cannot remove hazardous chemicals properly, causing them to build up in the body. Additionally, digestion in the gut is diminished to a moderate degree.
Request an appointment for Liver Cirrhosis Treatment
Liver cirrhosis appointment
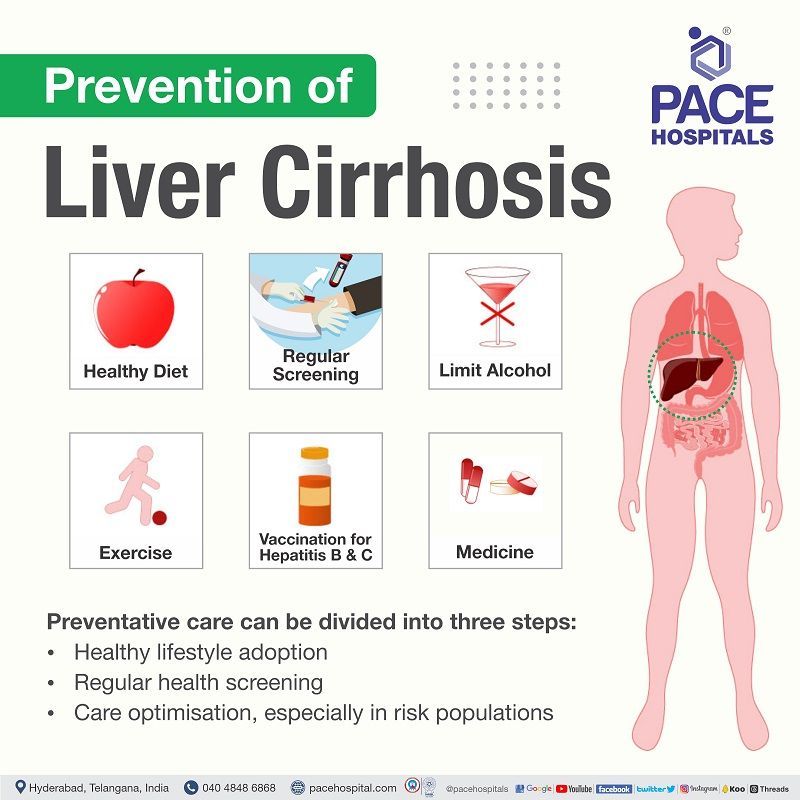
Prevention of Liver Cirrhosis
Preventative care can be taken by the patients themselves to avoid cirrhosis of the liver altogether. Preventative care can be divided into three steps:
- Healthy lifestyle adoption
- Regular screenings for liver disease
- Care optimisation, especially in risk populations
Healthy lifestyle adoption
A healthy lifestyle allows the efficient liver functioning, potentially reducing the risk of liver disease. Healthy weight maintenance and having a healthy balanced diet with regular exercise can ensure a healthy lifestyle. Also, alcohol abstinence is another important factor.
Regular screenings for liver disease
Screenings are necessary, especially in specific risk populations with greater possibility for signs of disease. The screenings could include a liver function test - a group of blood tests to check how well the liver is working. There are cases of accidental findings of liver impairment through the results of the tests.
Care optimisation, especially in risk populations
It's crucial that patients with liver disease or any other medical condition adhere to their doctor's orders and contact either their primary care physician for any questions or concerns. If the care is optimised, the likelihood of developing chronic liver cirrhosis is decreased.
The risk population includes:
- Diabetics
- Patients suffering from Hepatitis B and Hepatitis C virus
- Patients suffering from non-alcoholic steatohepatitis (NASH) (fatty build-up in the liver linked with alcoholism) etc.
Frequently asked questions for Liver Cirrhosis
Share on
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868