Bariatric Surgery - Types, Cost & Risk
Experience a transformative journey of weight loss with bariatric surgery in Hyderabad at PACE Hospitals. Our experienced bariatric surgeons perform advanced weight-loss procedures that address obesity and related health concerns with precision and care. We focus on long-term success, offering personalized treatment plans and support at an affordable cost. Take the first step toward sustainable weight loss, renewed confidence, and a healthier future with our dedicated team by your side.
Request an Appointment for Bariatric Surgery
Bariatric Surgery Appointment
Why Choose PACE Hospitals for Bariatric Surgery?

Advanced OT Facilities for Lap. & Minimally Invasive Bariatric Procedures
Expert Bariatric & Metabolic Surgeons Specializing in Safe, Effective Weight-Loss Surgery
Bariatric Surgery with High Success Rates, Quick Recovery & Health Benefits
Affordable Bariatric Surgery with Insurance & Cashless Payment Options
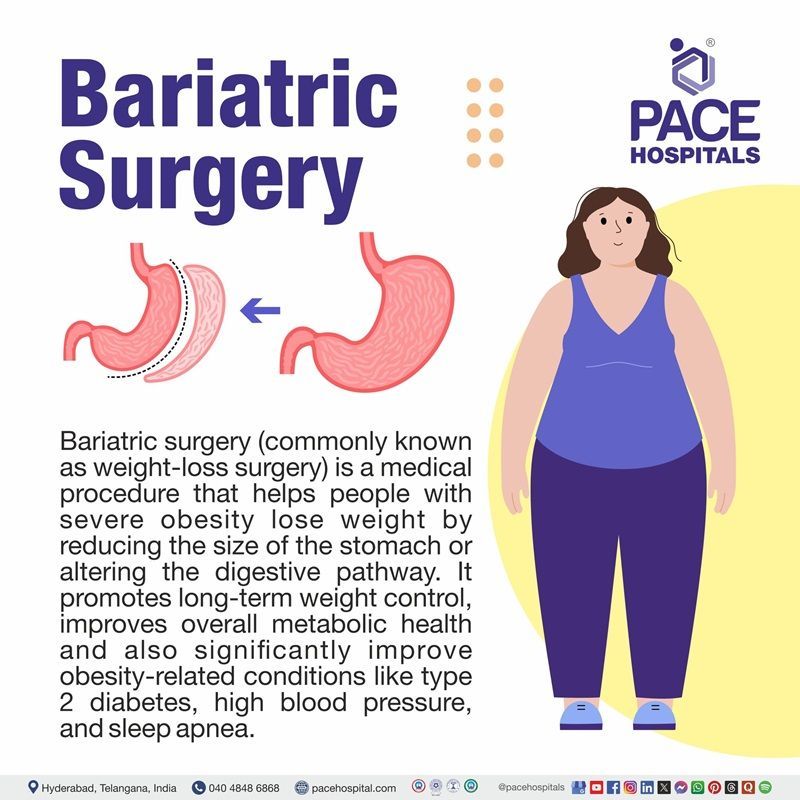
What is Bariatric Surgery?
Bariatric surgery is a surgical procedure which evolved as one of the most effective methods of treatment for morbid obesity. There are various types of bariatric surgeries which are successful in achieving and maintaining long-term weight loss in severe obese patients.
Optimal outcomes for weight reduction and co-morbidities remission after bariatric/metabolic surgery are seen with the mutual efforts of patients and gastroenterologists. The number of bariatric procedures performed each year is growing continuously. The field of bariatrics has slowly developed over time into a new subspecialty in the field of surgery.
Bariatric surgery is primarily performed by bariatric and metabolic surgeons who are specially trained in minimally invasive, laparoscopic, and advanced metabolic surgical techniques. These specialists work collaboratively with endocrinologists, dietitians, psychologists, physiotherapists, anaesthesiologists, and obesity-care physicians to assess the underlying causes of weight gain, evaluate associated comorbidities, and personalize the treatment approach.
Bariatric surgery meaning
The term “bariatric” comes from the Greek roots baros, meaning weight, heaviness, or burden, and iatric or iatreia, meaning medical treatment or healing. Together, they form a word that refers to the medical treatment of weight, which is the basis for the term “bariatric surgery.”
Types of Bariatric Surgery
Bariatric surgeries work by altering the digestive system to reduce food intake, limit nutrient absorption, or both. Each type of bariatric procedure offers unique benefits, risks, and suitability depending on a patient’s health status and weight-loss goals. Below is an overview of the most commonly performed bariatric surgery types-
- Lap Band / Gastric Banding
- Sleeve Gastrectomy
- Roux-en-Y gastric Bypass
- Biliopancreatic diversion
- Endoscopic sleeve gastroplasty (ESG)
- Adjustable gastric band
- Single-incision bariatric surgery
Lap Band / Gastric Banding
A band is placed around the upper stomach to create a small pouch with a narrow outlet, limiting food intake.
Sleeve Gastrectomy
A large portion of the stomach is removed, leaving a tube-shaped stomach with reduced capacity
Roux-en-Y gastric Bypass
The stomach is made smaller, and the small intestine is rearranged to limit caloric absorption.
Biliopancreatic diversion
A portion of the stomach is removed to create a banana-shaped stomach, with substantial portions of the small intestine bypassed.
Endoscopic sleeve gastroplasty (ESG)
A novel minimally invasive weight-loss procedure is done by suturing the stomach to reduce its volume.
Adjustable gastric band
A silicone band is surgically placed around the upper portion of the stomach to help restrict the quantity of food a person is allowed to consume.
Single-incision bariatric surgery
Initially, single incision laparoscopic surgery (SILS) was used in adjustable gastric banding (AGB) and sleeve gastrectomy due to the requirement of a trocar incision extension either for the placing a subcutaneous port or for the extraction of the resected gastric specimen.
In the beginning, a single-incision transabdominal (SITA) laparoscopic approach was followed, for which the incision was mainly done in the upper abdomen, but eventually, the researchers and surgical gastroenterologists performed the transumbilical incision near the umbilicus, which allowed a better cosmetic consequence for bariatric patients since there would be no visible abdominal scars as counting the umbilicus in hiding the surgical wound.
Indications for bariatric surgery
Although bariatric surgery is a weight reduction surgery, not everyone can be eligible for it. It is done in the patients as indicated below:
- Patients whose BMI ≥35 kg/m2 (class III obesity) without any obesity-related co-morbidities
- Patients whose BMI is 35–39.9 kg/m2 with type 2 Diabetes or any obesity-related co-morbidities
- BMI 30–34.9 kg/m2 with significant, life-limiting obesity-related conditions where weight loss is likely to improve health, in some programs.
- Patients with obesity-related health conditions such as type 2 diabetes, heart diseases, sleep apnea, high blood pressure, high cholesterol, and fatty liver disease.
- Patients with strong motivation to lose weight and committed to long-term follow-up
- Patients in whom conservative weight loss methods have failed
- Patient suffering from polycystic ovarian syndrome (PCOS) and infertility
- Patients whose ages fall between the age bracket of 18 - 65 years
- Patients above 65 years of age may be considered in special cases of severe obesity-related co-morbidities or disability
- Patients below 18 years of age who attained puberty/ skeletal maturity completion can be considered in special situations after paediatrician certification.
Bariatric Surgery Benefits
Bariatric surgery is the most effective medical intervention for peoples struggling with severe obesity, particularly when traditional weight-loss methods and medication have not produced sustainable results. By altering the digestive system, these procedures not only support significant and long-term weight reduction but also address many obesity-related health conditions.
Below are the key benefits of bariatric surgery:
- Provides effective and long-term weight loss
- Better control or remission of type 2 diabetes
- Lower blood pressure & improved heart health
- Improvement in sleep apnea
- Relief from joint pain
- Improvement in fatty liver disease
- Improved fertility & PCOS symptoms
- Better quality of life
Provides effective and long-term weight loss
This surgery helps patients lose a significant amount of excess body weight by reducing stomach size and altering hunger hormones.
Better control or remission of type 2 diabetes
After surgery, blood sugar levels improve quickly due to enhanced insulin sensitivity and reduced insulin resistance. Many patients reduce or completely stop diabetes medications, and some achieve full remission.
Lower blood pressure & improved heart health
Weight loss can reduce strain on the heart and blood vessels. Blood pressure decreases, cholesterol levels improve, and the risk of heart attack, stroke, and other heart diseases becomes significantly lower.
Improvement in sleep apnea
Losing extra body fat around the neck and airway helps to reduce airway blockage when sleeping. This results in fewer breathing pauses, increased oxygen levels, and a higher quality of sleep.
Relief from joint pain
Reduced body mass index decreases pressure on weight-bearing joints ( the knees, hips, and lower back). This may help to relieve pain, improves movement, and slows the progression of osteoarthritis (OA).
Improvement in fatty liver disease
Bariatric surgery promotes fat reduction in liver cells and decreases inflammation. This helps reverse non-alcoholic fatty liver disease (NAFLD) and improves or stabilises non-alcoholic steatohepatitis (NASH).
Improved fertility & PCOS symptoms
Weight loss helps balance hormones, restore regular menstrual cycles, and improve ovulation. Women with PCOS often experience better fertility outcomes and reduced symptoms like irregular periods and insulin resistance.
Better quality of life
Patients experience increased energy, confidence, and emotional balance. Most people can participate in daily activities more easily, have better mobility, and feel better overall.
Bariatric Surgery Contraindications
While there are few absolute contraindications to bariatric surgery procedures, patients who pose a prohibitive operative risk should not be offered surgery, including those with contraindications to general anaesthesia or uncorrectable coagulopathy (impaired blood clotting). The other contraindications include the following:
- Geriatric status: Patients more than 65 years of age as they have an increased risk of complications,
- Psychiatric illness: In patients with psychosis and suicidal ideation, bariatric surgery may not be helpful. Also, poor results are reported in patients with Prader-Willi syndrome or malignant hyperphagia.
- Cirrhosis: Although non-alcoholic fatty liver disease (around 90%) is common in severely obese patients, only cirrhotic patients risk periprocedural mortality.
- HIV/AIDS: Human immunodeficiency virus (HIV) and acquired immunodeficiency syndrome (AIDS) can be associated with cachexia (wasting and weakness of the body due to severe chronic illness), although antiretroviral therapy could be utilised.
- Non-ambulatory status: Poor functional capacity and non-ambulatory status can raise the risk of complications during surgery and lead to longer hospital stays.
- Pregnancy: Pregnant or those expecting to be pregnant within 12 months of surgery.
- Peptic ulcer: Active ulcers increase bleeding risk during or after surgery; typically optimized and treated prior to proceeding.
- Cardiac diseases: such as severe heart failure and unstable coronary artery disease.
- End-stage lung disease: Advanced-stage lung disease is associated with irreversible lung damage and significant lung dysfunction in providing adequate oxygen.
Bariatric Surgery Before and After
It includes the following steps:
Before Performing Bariatric Surgery
Excessive or abnormal fat accumulation (overweight and obesity) can impair health, which can occur when the rate of energy ingestion is higher than that of consumption. Apart from the regular pre-surgical tests, the candidates undergoing bariatric surgery procedures are to be assessed for their psychological, cardiopulmonary, and nutritional statuses, as these could alter the course of postsurgical outcomes and quality of life.
Psychological assessment: The psychological assessment of candidates is one of the pre-surgical evaluations necessary for the commencement of bariatric surgery. The psychological assessment is necessary for:
- Identifying any psychosocial contraindications to surgery helped in gaining weight before surgery.
- The screening of bariatric patients who benefit from psychological treatment before surgery
- Improvisation of quality of life and maximisation of long-term bariatric outcomes
- Selection of bariatric patients need for psychological support
Bariatric surgery can have poorer post-operative effects if the above psychological disturbances are not resolved.
Cardiopulmonary assessment: During the preoperative period, the gastroenterologist may prescribe bariatric patients with cardiorespiratory tests such as:
- Doppler-echocardiography
- Electrocardiogram (ECG),
- Exercise stress test,
- Sleep-wake study test
- Polysomnography
- Spirometry and blood gases
- Chest radiography
A high incidence of cardiorespiratory ailments with elevated morbidity and mortality could be associated with morbidly obese individuals. The gastroenterologist can understand the risk of diseases/disorders such as obstructive sleep apnoea-hypopnea syndrome (OSAHS), restrictive pulmonary syndrome, cardiac failure, and coronary heart disease through the above tests.
Nutritional Evaluation: The gastroenterologist team (qualified dietitian) can obtain information about the patients eating patterns, pathologies, healthy supplementation use, etc., by questioning their:
- Liquid intake
- Number and types of meals per day
- Dysregulated eating
- Eating patterns (e.g., vegetarian, lactose-free, gluten-free)
- Eating pace
- Food avoidance and/or aversions
- Nutrient intake evaluation (energy, macronutrients, and micronutrients intake by 24-h recall or food diary)
- Ability to swallow pills
- Patient needs to follow pre bariatric surgery diet, such as a high-protein, low-carbohydrate diet for about two weeks before surgery, followed by a two-day pre-operative liquid diet to shrink the liver.
- Type and dose of supplementation intake, etc.
Nutritional evaluation provides the opportunity to understand the patient's expectations for weight loss goals. The type of surgery also matters as 60-65% of extra body weight could be lost in two years in the case of sleeve gastrectomy, whereas gastric bypass patients could lose 70-75% of excess body weight. Diabetic patients often require postsurgical glycaemic supervision.
During Bariatric Surgery
Anaesthesia and monitoring
Bariatric surgery is performed under general anaesthesia, ensuring the patient is fully asleep and pain-free throughout the procedure. The anesthesiologist closely monitors airway, breathing, heart function, and oxygen levels, which is especially important in patients with obesity and related comorbidities.
Surgical Technique
The choice of bariatric surgical technique depends on the patient’s BMI, metabolic profile, comorbidities, and surgeon preference. Most procedures are performed laparoscopically (keyhole surgery) or with robotic assistance.
Common approaches include:=
- Sleeve Gastrectomy: In this 70–80% of the stomach is removed and the rest of the stomach is shaped into a narrow tube (sleeve).
- Roux-en-Y Gastric Bypass (RYGB): In this, a small gastric pouch is created and a section of the small intestine is bypassed.
- Endoscopic sleeve gastroplasty (ESG): This uses an endoscope with a suturing device to reduce the size of the stomach without incisions.
- Mini Gastric Bypass (One-Anastomosis Gastric Bypass): In this a long, narrow gastric pouch is created and a single anastomosis connects the pouch to the small intestine.
- Revision Bariatric Surgery: This surgery is performed when a previous bariatric procedure needs correction, conversion, or improvement.
Procedure Duration
In general, bariatric surgery takes 60 to 120 minutes, depending on the type of procedure, patient anatomy, and presence of adhesions from previous surgeries.
Intraoperative Care
During bariatric surgery, surgeons maintain careful hemostasis to reduce blood loss and perform leak tests to ensure the staple line or anastomosis is secured carefully. Trocars are properly positioned for laparoscopic access, and vessels and tissues are divided and sealed using staplers or energy devices. Absorbable sutures are used to strengthen staple lines and heal mesenteric defects without damaging nearby organs.
Completion of procedure
At the end of the procedure, the surgeon examines the abdomen for any bleeding or leaks. The carbon dioxide gas used during laparoscopy is released to help lessen postoperative discomfort. The small incisions are closed with sutures or skin adhesives. After this, the patient is moved to the recovery room for careful monitoring.
After Bariatric Surgery
- Patients are monitored in the recovery area for pain control, breathing, heart function, and overall stability.
- They are encouraged to walk within a few hours to reduce the risk of blood clots and improve lung function.
- Diet progresses gradually—from clear liquids to full liquids, soft foods, and then solid foods — over 4–6 weeks, while maintaining good hydration and starting lifelong vitamin and mineral supplements.
- Mild discomfort is common at the incision sites, and wounds usually heal within 1–2 weeks with simple care.
- Regular follow-ups are important to monitor weight loss, nutritional status, and improvement of conditions like diabetes, hypertension, sleep apnea, and fatty liver disease.
Bariatric Surgery Risks
Patients under 55 with BMIs below 50 kg/m2 had less than 1% mortality, but for people with >60 kg/m2 BMIs, the mortality rate is 2-4%. The rate of bariatric surgery side effects is less than 10%. The surgeon's experience and frequency (> 100 cases per year) can positively reduce the risk of morbidity and mortality. The complications given here are generalised and could be diversified depending on the types of bariatric surgery procedure performed. The bariatric surgery side effects of bariatric surgery for weight lossare divided into early and late complications.
Early complications:
Anastomotic or staple line leak: This leak occurs especially in 1.2-3% of bariatric patients who underwent a Roux En Y Gastric Bypass. It can be accompanied by fever, tachypnoea (rapid breathing), and sustained tachycardia (sustained heart rate of >120 beats/minute).
Post-operative bleeding: Approximately 3.1% of bariatric patients experience bleeding after bariatric surgery in which
- Spontaneous healing is seen in 22%,
- Blood transfusion requirement is seen in 55% and
- Operative intervention requirement is seen in 22%.
Late complications:
- Nausea or vomiting: Commonly seen with most surgeries and medications, nausea or vomiting can be improved with proper education about food selection and eating behaviour. The patient may be prescribed thiamine supplements in case of sickness or vomiting accompanied by neurologic symptoms.
- Excess or loose skin: A common, unwanted side effect of substantial weight loss accompanied by impaired mobility and self-care. A follow-up visit to a bariatric physician or occupational or physical therapist is recommended.
- Small bowel obstruction: Could be seen with abdominal bloating (gas build-up in the stomach and intestines), cramping, or pain and nausea to severe pain and emesis. It could be due to internal hernias (protrusion of small bowel loops into the abdominal and pelvic cavity) or severe constipation.
- Ulcers: Ulcers can be presented as upper epigastric pain or burning radiating to the back, with nausea or vomiting and food intolerances. Iron deficiency anaemia is common in these patients.
Bariatric Surgery Results
While weight loss is the primary outcome of successful bariatric surgery procedures, various other conditions are altered by bariatric surgery. They include:
- Weight loss durability: Most patients achieve long-term weight loss, with a significant number maintaining at least 20% total weight loss several years following surgery, while individual outcomes vary depending on treatment and adherence to follow-up regimens.
- Type 2 Diabetes: Obese patients are often associated with diabetes. Various studies demonstrated that outcomes for bariatric surgery procedures were better than medical therapy for glycaemic control and variable rates of remission for type 2 diabetes (anywhere from 1-5 years following treatment). The reduction of glycaemic control (HbA1c) from 1.8% to 3.5% is higher in surgery when compared with medical treatments (0.4% to 1.5%)
- Dyslipidaemia: Around 64% of obese individuals seeking bariatric surgery were diagnosed with dyslipidaemia (a high level of low-density lipoprotein, high triglycerides, and a low level of high-density lipoprotein). While short-term (1-2-year) improvements in dyslipidaemia can be seen with every bariatric surgery procedure, depending on the type of bariatric surgery, dyslipidaemia prevalence was still reduced even after seven years.
- Hypertension: At least 68% of obese individuals suffer from hypertension. It varies depending on the type of bariatric surgery procedure and lifestyle intervention. Hypertension remission rate is seen from 43-83% within one year of surgery.
- Obstructive Sleep Apnoea: Using the apnoea-hypopnea index, the severity of obstructive sleep apnoea is quantified. The apnoea-hypopnea index is as follows:
- <5 events/hour – Normal.
- 5-14.9 events/hour – Mild.
- 15-29.9 events/hour – Moderate.
- 30 events/ hour – Severe.
Body mass index (BMI) and apnoea-hypopnea index scores have a significant reduction with bariatric surgery procedure. Both daytime sleepiness and the severity of obstructive sleep apnoea are improved. - Osteoarthritis: Improvement in knee pain and functional status within the first 6-12 months after being seen after bariatric surgery procedures. However, short-term risks for arthroplasty-related wound infection or venous thromboembolism are not improved. It is the same case with long-term risks for dislocation, periprosthetic infection, periprosthetic fracture, and revision.
- Urinary Incontinence: An established risk factor for urinary incontinence, the reduction of obesity helps improve the former. After one year of bariatric surgery procedure, substantial bariatric surgery benefits, such as a reduction in the prevalence of urinary incontinence, were seen in women (49% to 18.3%) and (22% to 9.8%) men.
- Cancer risk: With obesity, an increased risk of various types of malignancy is seen, such as breast endometrial, colon, liver, pancreatic, and ovarian cancers. Bariatric surgery benefits are associated with a decreased risk of all types of cancers.
- Psychological health: Bariatric surgery benefits are also seen in the psychological status of the patient who underwent the procedure. Various studies with extensive reviews have indicated bariatric surgery benefits such as postoperative improvement in depressive symptoms, self-esteem, health-related quality of life, and body image.
Nutrition and supplementation are required for the maintenance of a healthy weight post-surgery
A well-balanced, calorie-reduced diet designed by a dietician must be part of a comprehensive weight management strategy. It could include:
- Limitation of solid intake to approximately 1 cup.
- Avoiding fluids within 30 min of pre and post-meals.
- Eating meals and snacks slowly (15-30 minutes) while chewing well.
- Avoiding difficult-to-chew food (e.g., tough meats, soft bread, stringy vegetables etc).
- Take meals (mostly solid food) 4-5 times daily (3 small meals + 1 or 2 small snacks).
- Abstinence from carbonated beverages (sodas, cool drinks, etc) and higher-sugar foods (pastries, confectionary, etc).
Life After Bariatric Surgery
With only a small number of contraindications, bariatric surgery seems to be recognized today as an effective therapeutic alternative for people with morbid obesity.
Beyond significant weight loss, the objective of bariatric surgery is also to improve patients’ postoperative well-being. It is especially recognized today that quality of life (QoL) is a relevant variable to consider in the weight loss process and psychologic monitoring of patients.
- Reduced BMI: Bariatric surgery resulted in a clinically meaningful reduction in BMI of 19.6% within the first three months of surgery and of almost 40% within 2 years.
- Evolution of quality of life: Beyond weight loss, the benefit of bariatric surgery is also seen in the improved quality of life among patients even a couple of years after the procedure.
- Physical activity: Around 68% of patients having undergone bariatric surgery become “active” after the operation, thus lowering their BMI by 8% more than those who continue a sedentary lifestyle. Moreover, it must be understood that physical activity is also associated with higher quality of life, both physically and mentally.
Bariatric Surgery Cost in Hyderabad, India
The cost of Bariatric Surgery in Hyderabad generally ranges from ₹1,40,000 to ₹4,80,000 (approx. US $1,680 – US $5,760).
The exact cost depends on the type of bariatric procedure (Sleeve Gastrectomy, Gastric Band, Roux-en-Y Gastric Bypass, Mini-Gastric Bypass, Revision Bariatric Surgery), patient’s BMI, associated diseases (diabetes, hypertension, sleep apnea, fatty liver), preoperative tests, anesthesia, hospital stay, surgeon expertise, and hospital facilities — including cashless options, TPA corporate tie-ups, and support with medical insurance documentation wherever applicable.
Cost Breakdown According to Type of Bariatric Procedures & Care
- Bariatric Surgeon Consultation – ₹800 – ₹2,500 (US $10 – US $30)
- Preoperative Tests (CBC, LFT, RFT, Thyroid, ECG, Echo, Chest X-ray) – ₹3,500 – ₹7,500 (US $42 – US $90)
- Endoscopy (If Recommended) – ₹2,000 – ₹4,500 (US $24 – US $54)
- Anesthesia Evaluation –
₹1,000 – ₹2,500 (US $12 – US $30)
Surgery Cost According to Procedure Type
- Sleeve Gastrectomy – ₹1,40,000 – ₹2,50,000 (US $1,680 – US $3,000)
- Roux-en-Y Gastric Bypass – ₹2,10,000 – ₹4,20,000 (US $2,500 – US $5,040)
- Mini-Gastric Bypass / One-Anastomosis Bypass – ₹1,80,000 – ₹3,20,000 (US $2,160 – US $3,840)
- Gastric Band Surgery – ₹1,20,000 – ₹2,10,000 (US $1,440 – US $2,500)
- Revision Bariatric Surgery – ₹2,50,000 – ₹4,80,000 (US $3,000 – US $5,760)
Additional Cost Factors
- High-BMI / Complex Case Surcharge – ₹15,000 – ₹45,000 (US $180 – US $540)
- Hospital Stay (2–4 Days) – ₹15,000 – ₹45,000 (US $180 – US $540)
- Postoperative Medications & Supplements – ₹4,000 – ₹12,000 (US $48 – US $144)
- Dietitian & Lifestyle Counseling – ₹1,500 – ₹4,000 (US $18 – US $48)
- Follow-up Blood Tests & Vitamin Levels – ₹1,500 – ₹5,000 (US $18 – US $60)
Frequently Asked Questions (FAQs) on Bariatric Surgery
How does bariatric surgery reverse diabetes?
Bariatric surgery has been a therapeutic option for severely obese adults associated with type 2 diabetes. The weight loss induced by bariatric surgery is superior to that of nonsurgical management. Nevertheless, it must be understood that a potent anti-diabetic effect was also observed in few cases. This anti-diabetic effect may extend beyond the period of perioperative caloric restriction, which demonstrates an independent effect of the surgery affecting glucose metabolism.
Which Is the best hospital for Bariatric Surgery in Hyderabad, India?
PACE Hospitals, Hyderabad, is one of the most trusted centers for bariatric and metabolic surgery (Weight loss surgery), offering comprehensive evaluation and advanced surgical solutions for obesity and obesity-related metabolic disorders.
We manage complicated cases of bariatric surgery with our highly dedicated team involving experienced bariatric surgeons, endocrinologists, anesthesiologists, dietitians, physiotherapists, and metabolic specialists skilled in treating:
- Severe obesity
- Type 2 diabetes
- Hypertension & dyslipidemia
- Sleep apnea
- PCOS-related weight gain
- Fatty liver (NAFLD/MASLD)
- Joint pain due to obesity
- Failed weight-loss attempts
Keeping view of patients’ pain control we opt for more laparoscopic surgical options, dedicated ICU care, structured dietary plans, and long-term follow-up programs, PACE Hospitals ensures safe, effective, and patient-centered bariatric care — supported by cashless insurance, TPA tie-ups, and complete documentation assistance.
Is bariatric surgery safe?
Yes, bariatric surgery is generally safe and effective when performed in appropriate patients at experienced, high-volume centers, but risks exist and vary by procedure and individual factors. Mortality is <0.1-0.3% and complications can occur, so informed consent and careful follow-up are essential.
What is the biggest impact of bariatric surgery?
The biggest impact of bariatric surgery is:
Significant and sustained weight loss
Improvement or resolution of obesity-related health conditions (e.g., type 2 diabetes, hypertension, sleep apnea)
Enhanced overall health and quality of life
Complications like dumping syndrome, kidney stones, or weight regain are possible but are side effects, not the primary impact.
How long is the recovery time from bariatric surgery?
Bariatric bypass surgery recovery time may depend on the procedure performed, but most patients return to normal activities within 2–4 weeks. Laparoscopic techniques allow shorter hospital stays—usually 2–3 days—and faster healing. Full recovery, including dietary progression and adaptation, typically takes 6–8 weeks.
What is the cost of Bariatric surgery in Hyderabad at PACE Hospitals?
At PACE Hospitals, Hyderabad, the cost of bariatric surgery typically ranges from ₹1,35,000 to ₹4,50,000 and above (approx. US $1,620 – US $5,400), making it a highly competitive and specialized option for weight-loss and metabolic surgery. However, the final cost depends on:
- Type of bariatric procedure
- Patient’s BMI & associated health conditions
- Need for endoscopy or advanced imaging
- Robotic vs. laparoscopic technique
- Duration of hospital stay
- Pre-existing comorbidities (diabetes, hypertension, sleep apnea)
- Postoperative supplements & follow-up requirements
- Nutritional and lifestyle counselling
Patients undergoing standard sleeve gastrectomy fall at the lower range, while complex bypass or revision surgeries fall toward the higher range.
After evaluation, diagnostic testing, and multidisciplinary consultation, our bariatric team provides a personalized surgical plan and a transparent cost estimate tailored to each patient’s health needs.
What is bariatric surgery?
Bariatric surgery types of weight loss surgery, helps with weight loss and can improve conditions like type 2 diabetes. Restrictive procedures reduce stomach size to limit food intake (e.g., sleeve gastrectomy).
Malabsorptive procedures decrease nutrient absorption by bypassing part of the intestine (e.g., biliopancreatic diversion). Some surgeries, like Roux-en-Y gastric bypass (RYGB), combine both methods.
Who is not an ideal candidate for bariatric surgery?
Individuals who are not ideal candidates for bariatric surgery include:
- Uncontrolled psychiatric illness
- Active substance abuse,
- Having severe untreated eating disorders
- Advanced heart or lung disease can have high surgical risk,
- Patients having inability to commit to long-term follow-up are also unsuitable.
Guidelines emphasize that patients must demonstrate medical stability, psychological readiness, and adherence to lifestyle changes for safe and effective outcomes.
What is the failure rate of bariatric surgery?
Despite being the most effective surgical treatment for severe obesity, 15-35% of bariatric patients do not attain their target weight. Unsuccessful bariatric surgery procedures could be attested to:
- Older age
- Initial BMI
- Behavioral and social factors
- Surgical type
How do you qualify for bariatric surgery?
According to the National Institutes of Health (NIH), bariatric surgery procedure is appropriate for people
- Have a BMI ≥ 40 kg/m² (severe obesity), or
- Have a BMI ≥ 35 kg/m² with at least one serious obesity-related health condition (comorbidity), such as:
- Type 2 diabetes mellitus
- Hypertension
- Mechanical joint problems in weight-bearing joints
- Hyperlipidemia
- Coronary artery disease
- Lower extremity lymphatic or venous obstruction
- Obstructive sleep apnea
- Pulmonary hypertension
Do you need to lose weight before bariatric surgery?
Yes. Preoperative weight loss can demonstrate a beneficial effect. A study showed that even weight loss in small proportions (i.e., >0 to <5%) was associated with a significant drop in mortality after the surgery. Also, the strict weight loss regimen before the bariatric surgery procedure helps acclimate the patient to post-operative life.
Can you ever drink soda again after gastric sleeve?
No. The patients may not drink soda after undergoing gastric sleeve as they could irritate the stomach. Along with carbonated beverages, coffee is also to be avoided for at least three months, and alcohol must be avoided for at least six months after surgery.
Can you have bariatric surgery after a heart attack?
Yes, bariatric surgery can be performed on people who have had a heart attack, but it must be carefully reviewed by a cardiologist and the surgical team. The timeframe is determined by the patient's cardiac function, recovery time, and general medical stability. Preoperative optimization and attentive monitoring are critical for risk minimization.
What are the 4 types of bariatric surgery?
The four commonly performed bariatric procedures are Sleeve Gastrectomy, where a part of the stomach is removed to reduce capacity; Roux-en-Y Gastric Bypass, which reroutes food to a small stomach pouch; Mini-Gastric Bypass (OAGB), a simplified bypass with one anastomosis; and Adjustable Gastric Banding, where a band restricts stomach size.
What age is best for bariatric surgery?
Bariatric surgery is most commonly recommended for adults between 18 and 65 years, although carefully selected adolescents and older adults may also benefit. Guidelines show that age alone is not a strict limitation—overall health, obesity severity, and presence of comorbidities are more important. With proper evaluation, even patients above 65 can undergo bariatric surgery safely with good outcomes.




