Urodynamic Study | Benefits & Cost
At PACE Hospitals, experience cutting-edge urodynamic testing procedure led by our team of expert urologists/urogynecologists. Guiding you to informed health decisions. Schedule your appointment today for leading-edge care in Hyderabad.
Why Choose PACE Hospitals for Urodynamic Study?
8900+ Urethrotomy Surgery performed
Team of the Best Urologist in Hyderabad
Precision Treatment with 99.9% success rate
All insurance accepted with No-cost EMI option
What is Urodynamic Study (UDS)?
Urodynamic studies (UDS) refer to a set of tests that check how well the parts of the lower urinary tract, such as the bladder, sphincters, and urethra, are working to store and release urine.
Most urodynamic tests may focus on how well the person's bladder can hold and empty the urine, and they also show why there could be blockages and whether the bladder is contracting when it is not supposed to, causing a leak of the urine.
A urologist or urogynecologist may recommend urodynamics or urodynamic testing if the person has:
- Urine leakage
- Painful urination
- Frequent urination
- Sudden, strong urges to urinate
- Problems emptying the bladder completely
- Problems starting a urine stream
- Have repeated urinary tract infections
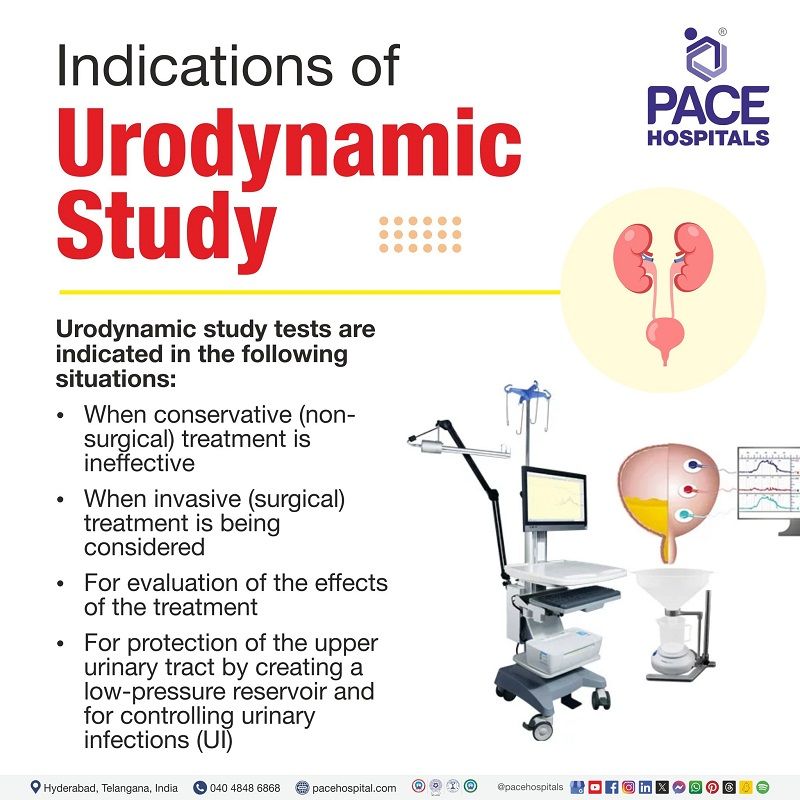
Patient Selection for Urodynamic Studies
The following factors suggest the need for urodynamic testing:
- Unclear or complicated history
- History of urinary retention
- Elderly patient (>65 y) with multiple possible diagnoses
- Advanced diabetes (bladder neuropathy or cytopathy)
- Previous failed incontinence surgery
- Nulliparous woman (woman having no previous births) with stress incontinence
- Male patient with multiple possible diagnoses
- Known or suspected neurologic disease as a cause or contributor to incontinence
- Nocturnal enuresis if other diagnostics are exhausted
- Continuous incontinence or leakage with minimal activity
Before Urodynamic Test (Preparation)
Most urodynamic study procedures don't require special preparation and planning. However, for some tests, a urologist may ask the patient to drink fluids before the test to keep the bladder full. It is recommended to ask the urologist any questions before the test.
The duration of each test varies. Usually, one can expect it to take 30–45 minutes on average. Urodynamic tests may not be painful. However, some may feel soreness for up to 24 hours afterward, but one cannot have severe pain. The patient may get the results from cystometry and uroflowmetry on the same day.
During Urodynamic Test
Urologists may perform urodynamic testing procedures invasively and noninvasively. The urodynamic study test involves non-invasive assessment of bladder emptying and invasive evaluation of bladder storage and emptying functions. Invasive assessment uses the insertion of catheters (a small medical tube for insertion into canals, body cavities for diagnostic or therapeutic purposes) into the bladder and other parts.
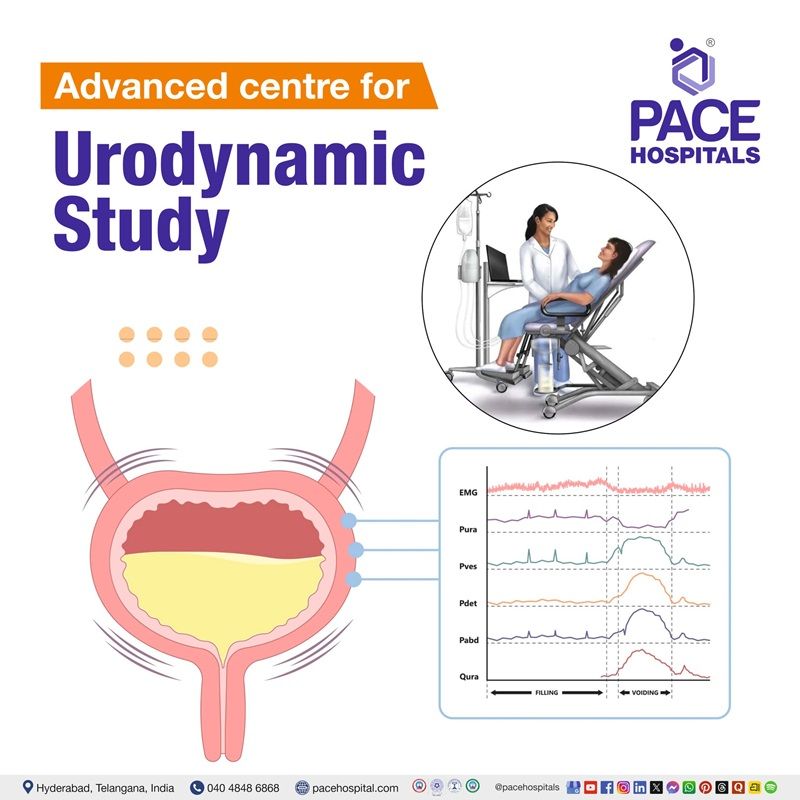
Standard urodynamic testing is performed in people with lower urinary tract (LUT) symptoms. It involves non-invasive uroflowmetry, followed by invasive cystometry and a pressure flow study. The addition of other tests like concurrent urethral pressure profiles and EMG of pelvic floor muscles may provide further clinical details.
Urodynamic Study Procedure
Test process of urodynamic studies involves continuous testing of the urine, to determine the diagnosis, plan treatment and to check whether the treatment is working or to monitor the disease over time. There are many types of urodynamic tests. A urologist may recommend one or more tests based on the person's symptoms. However, they are typically performed together as one test. The following are some of the common tests performed in the urodynamic study:
- Uroflowmetry
- Postvoid residual measurement:
- Cystometry or cystometrogram (CMG urodynamic study)
- Leak point pressure measurement
- Pressure flow study
- Electromyography
- Video urodynamic study
- Fluoroscopic urodynamic study
- Maximum urethral closure pressure (MUCP)
Uroflowmetry
Uroflowmetry measures the amount of urine in the patient's bladder and how fast the urine flows out (flow rate). It helps identify any difficulties in emptying the bladder. The results of the uroflowmetry may reveal any weakness of the bladder muscles or there is any blockage to the urine flow.
For this test, a urologist will ask the patient to arrive with a full bladder and to urinate into a special toilet or funnel (which has a container for collecting the urine and a measuring scale. The uroflowmetry equipment will help to measure the volume and speed of the urine and create a graph that shows modifications in the flow rate while the patient urinates.
A urologist uses a graph to visualize the flow rate's peak and the duration to reach it. The flow rate of the patient may also be estimated by recording how long it takes to urinate into a special container that precisely measures how much urine a patient release.
Postvoid residual measurement
This test measures the amount (how much) of urine left in the bladder after the patient urinates. Every person has a small amount of urine in the bladder after urination. If the patient has 100–150 milliliters of urine or more than that remains in the bladder, it indicates the bladder is not emptying completely. This test will be performed using ultrasound or by feeding a catheter (thin-flexible tube) into the patient's bladder to drain and measure the remaining urine.
Cystometry or cystometrogram (CMG urodynamic study)
It measures the bladder capacity (amount of urine a patient's bladder can hold), the amount of pressure that builds up inside the bladder as it stores urine, bladder elasticity, and how the patient's bladder feels during filling to detect if there are any abnormal bladder spasms during filling of the bladder. These tests help to identify problems with urine storage and how well the patient's bladder can hold urine without leaking.
During this process, a catheter will initially empty the bladder completely. Then a special, smaller catheter may use placed in the bladder, and another catheter will be positioned in the rectum or vagina to record pressure there. A manometer (pressure measuring device) will be used to calculate the pressure present with the catheter.
Once the patient completely empties the bladder, warm water will be used to fill the bladder slowly. Then, the patient will be asked to describe how the bladder feels, and when the patient begins feeling that urge to urinate, the volume of bladder pressure and water will be recorded. Afterward, the patient may be asked to cough or strain, stand up, or jog to see if the bladder pressure changes or if the patient leaks' urine. A cystometric test also identifies if the patient's bladder is contracting when it is not supposed to.
Cystometric abnormalities do not diagnose any underlying problem; however, they describe the functional disturbance itself.
Leak point pressure measurement
If the patient's bladder is being filled with warm water for the cystometric test, the bladder of that patient may suddenly contract and squeeze some water out without warning.
When the leakage occurs, a manometer measures the pressure inside the urinary bladder to identify the leak point pressure. This information may tell the urologists what kind of bladder problem a person has.
The patient may be asked to cough, shift position, or try to exhale while holding the nose and mouth. These actions help the urologist to evaluate the sphincters that help keep the patient's urine in:
- Abdominal leak point pressure: ALPP is the dynamic test, which measures the minimum (lowest) bladder pressure within the urinary bladder when the urine leaks due to increased abdominal pressure without a detrusor contraction during coughing.
- Valsalva leak point pressure: VLPP is a type of ALPP measurement. This test measures the minimum (lowest) bladder pressure causing urine leakage during the Valsalva maneuver (forceful exhalation) or coughing without muscle contractions.
These tests are helpful to assess urinary leakage without detrusor muscle contraction. A VLPP less than 60 cmH20 is thought to represent sphincter weakness, while over 90 cmH2O indicates sphincter competence. ALPP > 150cmH2O suggests incontinence is unlikely due to urethral weakness.
Pressure flow study
A pressure flow study is helpful to measure the amount of pressure needed for the bladder to urinate and how quickly the patient's urine flows at that pressure. This test finds any bladder outlet blockage that may be caused by prostate enlargement, cystocele, or urinary incontinence correction surgery.
During this procedure, the patient will be asked to pass urine using a small catheter inserted into the urethra. This test may help find the cause of a weak urinary stream. Normal values may be impacted by patient age and voided (urinating) volume. Flow patterns in pressure flow studies are the same as for another urodynamic study, such as uroflowmetry.
Electromyography (EMG)
EMG will be used to test the electrical activity of the muscles in the pelvic area. EMG may help identify if a urinary problem is from the pelvic nerve or muscle damage. A urologist may recommend this test if the patient's urinary problem is likely related to muscle or nerve damage. Electromyography utilizes special sensors to calculate the electrical activity of the muscles and nerves around and within the bladder and sphincters.
The sensors are placed on the patient's skin near the urethra and rectum or on an urethral or rectal catheter to record the nerve and muscle activity on a machine. These sensors measure the action of the bladder muscle and urethral sphincter muscle during the filling and emptying of the bladder.
The patterns of nerve impulses indicate correct coordination of messages to the bladder and pelvic floor muscles.
Bladder filling (cystometry) and emptying studies (uroflowmetry) can be combined with EMG measurement.
During rest, a healthy muscle may show no electrical activity (no signs of action potential) but will show when it contracts.
However, suppose the muscle is damaged or has lost input from nerves. In that case, it may show abnormal electrical activity during rest, and abnormal patterns may occur when damaged muscle contracts due to electrical activity.
Video urodynamic study
Video urodynamic tests use ultrasound or X-rays to take images and videos of the bladder while it fills and empties. For a better picture, a trained technician or urologist may use a catheter to fill the bladder with dye or contrast.
Fluoroscopic urodynamic study
Using X-ray (fluoroscopy) may help find problems that are more complicated. In this case, the bladder is filled with a contrast solution (not saline) that shows up on An X-ray to help see the bladder anatomy.
Maximum urethral closure pressure (MUCP)
This test is designed to measure the highest possible difference between the pressure in the urethra and the pressure inside the bladder (intravesical pressure).
- <20 cm H2O: suggests ISD (Intrinsic urethral sphincter deficiency: dysfunction of internal sphincter muscle of the bladder.
Urodynamic Study Findings
Five main types of information are gathered using urodynamic studies:
- Bladder emptying: Process of urinating the urine out from the urinary bladder.
- Bladder sensation: The first sensation of bladder filling (FSF) is the feeling when a person first becomes aware of bladder filling.
- Maximal bladder capacity: Maximum capacity (volume) of the bladder to hold urine
- Bladder compliance: It refers to the ability of the bladder to accommodate (to make fit) large volumes of urine
- Detrusor (bladder muscle) contractility
Before planning urodynamic studies, a urologist may thoroughly check the urological symptom history, patient's past medical history, and medications, and they perform physical examination and pelvic exam for females.
Patients being investigated for lower urinary tract symptoms (LUTS) are required to complete a validated symptom score that indicates the impact of symptoms on their quality of life.
After Urodynamic Test
After having urodynamic bladder tests, it is common for some patients to feel mild discomfort or pain for some hours when urinating. The medical team may recommend drinking some water every half-hour for 2 hours to reduce pain, and taking a warm water bath or holding a warm/damp washcloth over the urethral opening to relieve discomfort. They may also prescribe some drugs, such as antibiotics, to prevent infection.
It is recommended that a urologist be consulted if the patient experiences any signs of infection, including pain, chills, or fever. Results for simple tests such as uroflowmetry and cystometry are often available immediately after the test. However, results of other tests, such as video urodynamic tests and electromyography, may take a few days to return. The urologist will discuss with the patient about the results and possible treatments.
Urodynamic Testing Complications
Risks of invasive urodynamic testing may include as follows:
- Haematuria (blood in urine)
- Dysuria (difficult or painful urination)
- Urinary tract infection
- Urinary retention
Urodynamic Test Cost in Hyderabad, India
The cost of a Urodynamic Study (UDS) in Hyderabad generally ranges from ₹3,000 to ₹12,000 (approx. US $36 – US $145).
The exact cost depends on the type of urodynamic test performed (basic or advanced), whether single or multiple parameters are measured, use of pressure transducers, inclusion of uroflowmetry, cystometry, EMG, post-void residual assessment, and hospital facilities — including cashless insurance, TPA corporate tie-ups, and support with medical insurance documentation wherever applicable.
Cost Breakdown According to Type of Urodynamic Study
- Standard Uroflowmetry Test – ₹600 – ₹1,500 (US $7 – US $18)
- Post-Void Residual (PVR) Scan – ₹400 – ₹1,000 (US $5 – US $12)
- Complete Urodynamic Study (Cystometry + Pressure Flow Study + Uroflowmetry) –₹4,000 – ₹8,500 (US $48 – US $102)
- Advanced Multi-Channel Urodynamic Study (With EMG) – ₹7,000 – ₹12,000 (US $84 – US $145)
Frequently Asked Questions (FAQs) on Urodynamic Study
Is urodynamic testing necessary?
Urodynamic testing is necessary for assessing urinary problems in people with lower urinary tract (LUT) symptoms. This test involves the examination of the bladder and urethral sphincter functions using computerized equipment. This study aims to reproduce the troublesome urinary symptoms to diagnose the bladder problem more accurately and precisely plan further treatment.
Which Is the best hospital for Urodynamic testing in Hyderabad, India?
PACE Hospitals, Hyderabad, is one of the most trusted centers for performing Urodynamic Studies with high-precision diagnostic systems and experienced urologists.
We have experienced urology specialists skilled in using advanced multi-channel equipment to evaluate:
- Urinary incontinence (stress or urge)
- Overactive bladder
- Neurogenic bladder dysfunction
- Urinary retention
- Post-prostate surgery symptoms
- Bladder outlet obstruction
- Pediatric voiding dysfunction
We deliver results with expert interpretation, accurate reporting, and patient-friendly techniques, PACE Hospitals ensures reliable results for optimal treatment planning — supported by cashless insurance, TPA tie-ups, and complete documentation assistance.
Who requires urodynamics?
Urodynamics may be required in individuals who have medical problems or complex history, such as people with lower urinary tract (LUT) symptoms, getting UTIs (urinary tract infections often), a history of prior urological surgery or gynaecological surgery including surgery for urinary incontinence or prolapse, failed previous surgery.
What are the benefits of urodynamic testing?
Urodynamics helps find the cause of problems related to urine leaks or controlling the urine, weak urine flow, bladder not emptying completely, the need to go too often, the need to go suddenly, and urine flow stopping and starting.
Can urodynamic tests cause problems?
Most urodynamic tests have no significant risk of complications. However, during the procedure, if the patient had a catheter inserted into the bladder, there was a slight risk of developing a UTI- urinary tract infection.
How much does Urodynamic test cost in Hyderabad at PACE Hospitals?
At PACE Hospitals, Hyderabad, the cost of Urodynamic Study typically ranges from ₹3,000 to ₹11,000 and above (approx. US $36 – US $132), offering an affordable and specialized option for comprehensive bladder function testing. However, the final cost depends on:
- Whether a basic or advanced study is required
- Inclusion of EMG or multi-channel pressure recordings
- Complexity of the urinary condition
- Need for pediatric or geriatric assessment
- Additional pre-test or post-test evaluations
Simple tests such as uroflowmetry remain at the lower range, while advanced multi-channel studies fall toward the higher range.
Following clinical evaluation, our urology team recommends the most suitable urodynamic test and provides a transparent cost estimate based on the patient’s symptoms and diagnostic needs.
What type of doctor does urodynamic testing?
Urodynamics, or UDS, is a set of tests that doctors like urologists and urogynecologists commonly prescribe to see how well the lower urinary tract system is working and performed by physicians (urologists and urogynecologists), physician assistants, nurse practitioners, nurses, or medical technicians, or a medical professional who has been trained for urodynamics. A physician must review and interpret the findings (results) if a nurse or nurse technician may perform this test.
How is a urodynamic test performed?
Urologists may perform urodynamics invasively (surgically) and noninvasively (non-surgically). The urodynamic study test involves a non-surgical assessment of bladder emptying and invasive evaluation (surgical examination) of bladder storage and emptying functions. In contrast, the Invasive assessment uses the insertion of catheters into the bladder and other parts to measure the pressure and filling capacity.
Does urodynamic testing hurt?
Generally, one may not get any pain because this test is painless. However, sometimes, one may feel slight discomfort or soreness, urgency to pass urine, or embarrassment for several hours afterward. It does not involve the use of sedatives or anaesthesia, but some urologists use local anaesthetic gel to numb the opening of the urethra.
What does it include in a urodynamic studies?
The urodynamic studies include many tests such as uroflowmetry, cystometry, electromyography, pressure flow study, etc. Uroflowmetry is the test that is used to measure the flow of urine. Cystometry measures the pressure inside the bladder as it's being filled. Electromyography measures the activity of the pelvic floor muscles. A pressure flow study is used simultaneously to measure the pressure inside the bladder and urine flow while peeing.
What are the side effects of urodynamics?
Side effects of urodynamics testing may involve discomfort in passing urine, and the patient may notice a small amount of blood in the urine. Some people may have a small risk of developing a urine infection, inability to pass urine (retention of urine), and requiring temporary insertion of a catheter. It is recommended to consult the urologist if these symptoms continue for more than one day after the testing.
What size catheter is used in urodynamics?
Urologists usually use 5F and 6-7F catheters made of polyvinyl chloride or polyurethane. Using 5F catheters generally allows for a more accurate diagnosis of bladder outlet obstruction. However, urologists may avoid the larger size of 10F catheters, especially in patients with borderline symptoms.
What are the two types of urinary catheters?
There are two primary types of urinary catheters:
- Intermittent catheters: These are temporarily used catheters inserted into the bladder for a short time and removed once the bladder is empty.
- Indwelling catheters: These catheters are left in place for several days or weeks and are held in position by an inflated balloon inside the bladder.
Why should I go for a urodynamic testing?
A urodynamics test checks the bladder working and helps urologists investigate the cause of the urinary symptoms. The results of these tests can help the urologist to decide the best form of treatment for the patient, and it can be helpful when surgery is being considered and when previous treatments, such as medication, have not improved the patient's symptoms.
What can I expect after the test?
The patient may feel slight stinging or burning when passing urine. It is recommended to have plenty of fluids, mainly water, to help 'flush' the system through. Suppose the patient continues to experience burning or discomfort. In that case, the urine becomes cloudy and smelly or develops flu-like symptoms. Then, the patient should visit a urologist because the patient may have a urine infection that needs testing and antibiotic treatment.
What is the first sensation of urodynamics?
The lower urinary tract (LUT) has many nerves that transfer afferent information (signals) from various parts to the brain and spinal cord. The International Continence Society (ICS) and the International Urodynamic Basic Spinal Cord Injury data set have standardized terminology on sensations of bladder filling. The first sensation of bladder filling (FSF) is the feeling when a person first becomes aware of bladder filling. The first desire to void (FDV) is the first feeling that the person may want to pass urine soon, but one can hold if they wish to. A strong desire to void (SDV) is the intense feeling of urine without the fear of leakage.