Ascites - Symptoms, Causes, Complications, Prevention and Treatment
Pace Hospitals
Ascites definition
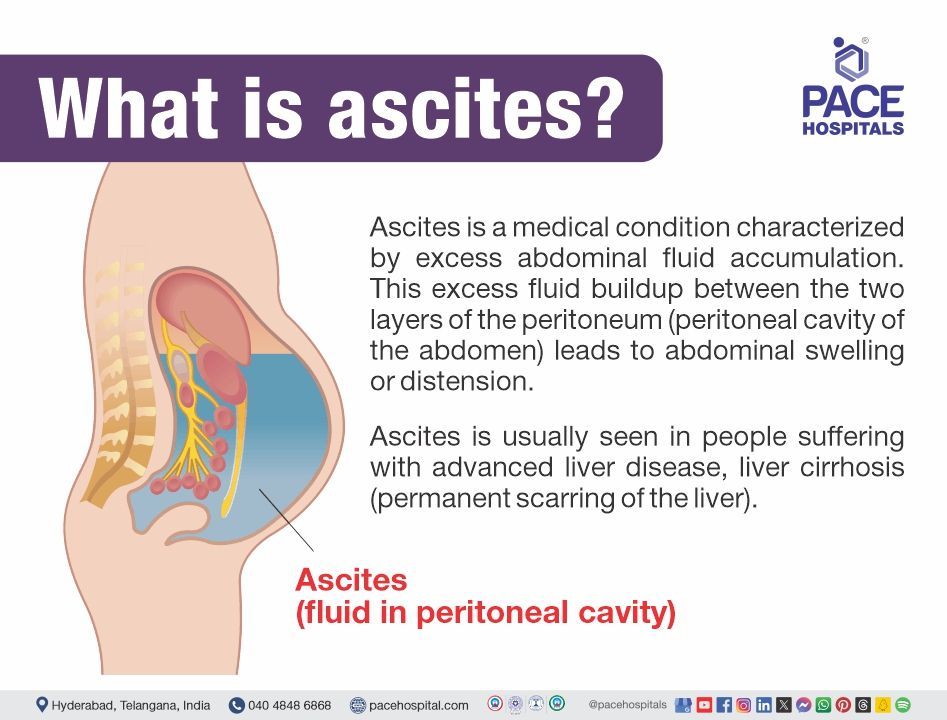
The condition known as "ascites" is defined as the fluid build-up in the space between the lining of the abdomen and abdominal organs.
Ascites meaning
The word ascites is of Greek origin and is derived from the word “askos”, literally a bag like dropsy or sac. Therefore, the word ascites describes the fluid collection in the abdominal cavity.
Ascites is a medical condition characterized by excess abdominal fluid accumulation. This excess fluid buildup between the two layers of the peritoneum (peritoneal cavity of the abdomen) leads to abdominal swelling or distension. The peritoneum is the tissue that covers the abdominal organs, such as the stomach, intestine, kidneys, and liver.
Ascites is usually seen in people suffering with advanced liver disease, liver cirrhosis (permanent scarring of the liver). Transitioning from compensated to decompensated cirrhosis is indicated by the development of ascites.
Incidence of ascites
Ascites is the common complication of the cirrhotic patients, from the past ten years cirrhosis of liver with ascites is seen in 50% of the decompensated cirrhotic patients. Approximately 50% of cirrhotic patients will have a 3-year death rate. Intraperitoneal ascites fluid is seen in a very low concentration in males, whereas up to 20 ml is seen in females based on the menstrual cycle. Though ascites is a complication or symptom of other conditions, there are no accurate, trusted values regarding the incidence rates in the normal population.
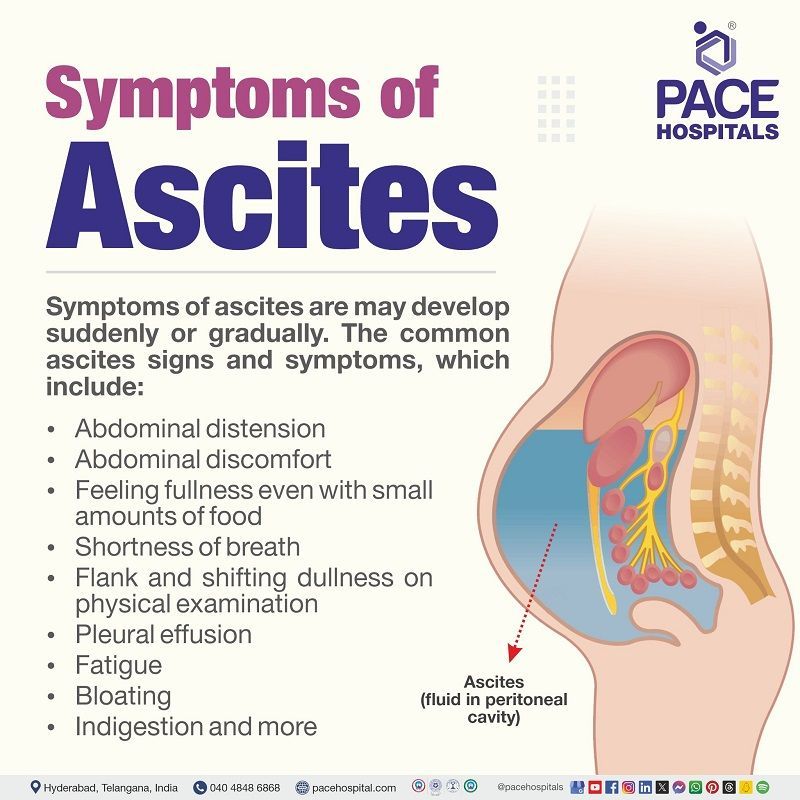
Ascites symptoms
Symptoms of ascites are indications that occur in the body; they might range from mild to severe and occur suddenly or gradually. However, there are some common ascites signs and symptoms, which include:
- Abdominal distension
- Abdominal discomfort
- Swelling in the abdomen
- Feeling fullness with small amounts of food
- Shortness of breath
- Flank and shifting dullness on physical examination
- Pleural effusion
- Fatigue
- Bloating
- Indigestion and more
Symptoms of ascitic patients with bacterial peritonitis include:
- Fever
- Tenderness on the abdomen
- Confusion
Symptoms of malignant ascites include:
- Weight loss
Symptoms of chylous ascites include:
- Steatorrhea (fatty stools)
- Diarrhoea (loose or watery stools)
- Nausea
- Oedema (swelling due to fluid accumulation)
- Night sweats
- Lymphadenopathy (enlargement of lymph nodes)
- Early satiety (unable to take full meals due to early fullness)
- Fever
Ascites causes
The accumulation of fluid in the abdomen, or ascites, can indicate a few underlying medical disorders, even though it can seriously impair daily life. The exact cause of ascites plays a crucial role in getting proper treatment. The key mechanisms that could cause ascites are as follows:
- Increased portal pressure: Portal hypertension is the condition where the portal vein blood pressure increases. The portal vein is the vessel that carry the blood from the spleen, pancreas, and intestine to the liver. Blood flow becomes harder in the liver when it gets scarred, resulting in a back-up of blood pressure in the portal vein. Finally, this leads to increased fluid pressure in the liver and other organs of the abdomen and forces the fluid from the capillaries into the peritoneal cavity.
- Sodium and water retention: Albumin is the protein that helps to manage the fluid in the bloodstream; if the liver gets damaged, it cannot produce enough albumin. Thus, it leads to low blood pressure and influences the kidneys to retain water and sodium in an attempt to compensate - these increased levels of sodium and water leak outside from the capillaries into the peritoneal cavity.
Ascites is caused by the following factors, such as:
- Liver cirrhosis
- Heart failure
- Kidney failure
- Cancers and more
Some of the main risk factors which contribute to the cause of ascites are explained in the section below.
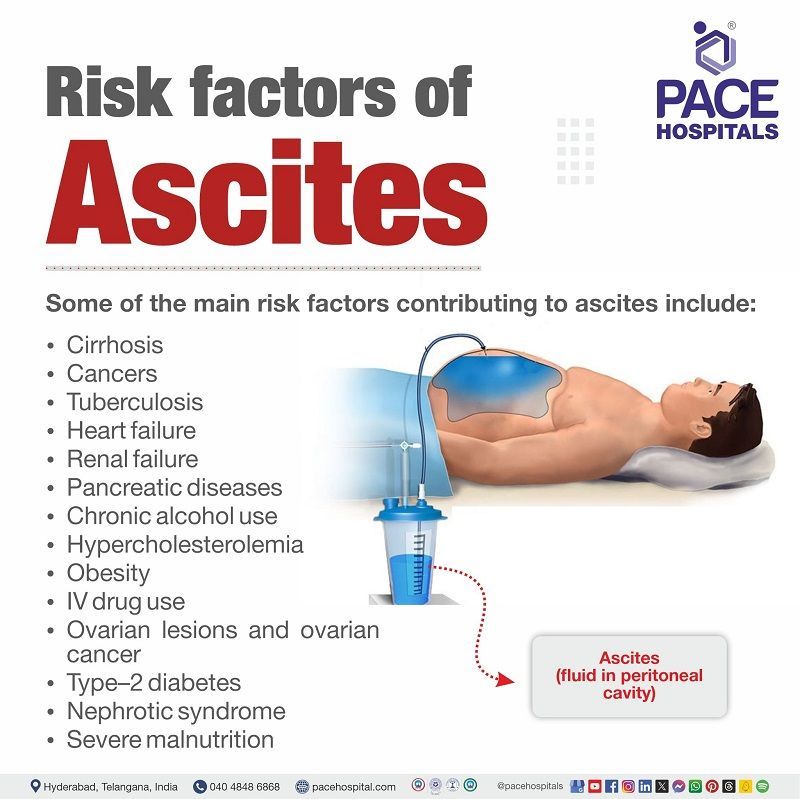
Ascites risk factors
The main risk factors that contribute to the cause of ascites are explained in the section below. Usually, risk factors are the factors that raise the probability of contracting a specific illness or condition; they are not the same as causes but influence the events positively. Some of the risk factors for ascites include:
- Cirrhosis: Portal hypertension is the fundamental factor that causes ascites in liver cirrhosis patients. Portal hypertension causes splanchnic vasodilation and activates the renin-angiotensin-aldosterone system, resulting in renal sodium retention.
- Cancers: The peritoneum may create excessive amounts of this fluid due to malignancy. The medical term for this is "malignant ascites". Cancer that has make progress to the lining of the abdominal organs is the cause of malignant ascites. Additionally, it may occur when liver cancer spreads.
- Tuberculosis: TB causes inflammation of the peritoneum and causes fluid leakage out of the capillaries; in addition to this, it also increases the portal pressure.
- Heart failure: Obstruction of venous flow is seen in heart failure, resulting in volume inflation and hydrostatic pressure. This condition leads to the filtration of the fluid into the peritoneal cavity.
- Renal failure: Patients with end-stage renal disease or chronic kidney disease are found to have impaired resorption of peritoneal fluids inferior to the peritoneal lymphatic drainage obstruction.
- Pancreatic diseases: Ascites caused by pancreatic injuries, pancreatitis or diseases is referred to as pancreatic ascites disease. This condition arises when pancreatic secretions are collected in the peritoneum due to a pancreatic injury.
- Chronic alcohol use: Ascites is the most common complication of alcoholic liver disease, in which the accumulation of fluid takes place in the peritoneal cavity. The patient presents with abdominal distension and pedal oedema in this condition.
- Hypercholesterolemia: Increased levels of ascitic cholesterol in peritoneal carcinomatosis are due to the movement of plasma HDL and LDL into the peritoneal cavity, resulting in ascites.
- Obesity: Obesity is indirectly linked to the ascites, as any health issue that causes liver damage or scarring could develop the ascites. Obesity leads to fat buildup and causes fatty liver disease, which might lead to the development of ascites.
- IV drug use: According to the studies, around 2% of the cases are due to IV drug usage, as these might develop hepatitis infections, which in turn lead to the development of ascites.
- Ovarian lesions and ovarian cancer: When ovarian cancer is in its advanced stages, ascites may develop. Previous studies from 2013 found that 90.1% of study population with third stage ovarian cancer and 100% of those with fourth stage ovarian cancer had ascites.
- Type–2 diabetes: Type 2 Diabetes could damage the blood vessels of the liver and might result in the development of portal hypertension, which causes ascites.
- Nephrotic syndrome: Ascites in the majority of adult nephrotic syndrome patients can be linked to elevated hepatic sinusoidal pressure, liver disease, or congestive heart failure in addition to hypoalbuminemia.
- Severe malnutrition:
Chronic liver disease (CLD) is often associated with altered nutrient metabolism, nutritional requirements, and decreased dietary intake. These worsen the progression to decompensation and ascites.
Complications of ascites
If left untreated, ascites could cause some complications, such as:
- Infections: The fluid can become infected and might cause a fever and stomach pain.
- Ascites-related hernias: Increased abdominal pressure due to the fluid buildup can lead to umbilical or inguinal hernias.
- Pleural effusion: Ascites can accumulate fluid between the lungs and chest cavity.
- Electrolyte imbalance: Portal hypertension and sodium-water imbalances in ascites conditions might lead to electrolyte imbalance.
- Weight loss and protein malnutrition: Due to the early satiety and impairment of protein synthesis, ascites might develop weight loss and protein malnutrition.
- Kidney failure: severe decompensated cirrhosis patients with ascites may develop hepato-renal syndrome.
- Bowel perforation: an increased risk of bowel perforation following the installation of an indwelling peritoneal catheter may exist in patients with intraperitoneal adhesions and septate ascites.
- Bleeding: Upper and lower gastrointestinal bleeding may be seen in ascitic patients.
- Hepatic hydrothorax: The lungs are filled with abdominal fluid, usually on the right side. Breathlessness, coughing, discomfort in the chest, and hypoxemia (low blood oxygen levels) are possible symptoms. Thoracentesis might be necessary to drain the fluid in this condition.
- Spontaneous bacterial peritonitis is a serious life-threatening bacterial infection of the ascites, characterised by fever and stomach pain. Bacterial peritonitis needs immediate IV antibiotic treatment to suppress sepsis and complicated conditions.
Ascites diagnosis
Ascitic fluid examination approaches are as follows:
- History taking and physical ascites examination
- Laboratory parameters (Lab tests):
- Complete blood count
- Serum albumin test
- Bacterial culture test by bedside inoculation
- Urinalysis
- Liver function tests
- Renal functional tests
- Coagulation tests
- Serum electrolytes
- Imaging techniques:
- Chest x-ray
- Ultrasound
- Computed tomography scan (CT scan)
- Magnetic resonance imaging (MRI scan)
- Diagnostic paracentesis for appearance, cell count, total protein, and serum-ascites albumin gradient
- Additional tests for specific diagnosis include:
- Lactate dehydrogenase (LDH)
- Amylase
- Mycobacterial culture test
Ascites treatment
Ascites management includes lifestyle changes, medical management, and surgical management.
- Lifestyle modifications:
- Diet should be taken with low sodium (<2000-4000 mg per day)
- Cessation of salty diet
- Cessation of alcohol
- Limiting fluid intake and more
- Medical management of ascites:
- Diuretics
- Antibiotics
- Invasive approaches and surgical management of ascites:
- Paracentesis (ascitic tap procedure)
- Trans jugular intrahepatic portosystemic shunt (TIPS)
- Liver transplant (In end stage liver disease or severe cirrhosis ascites cases)
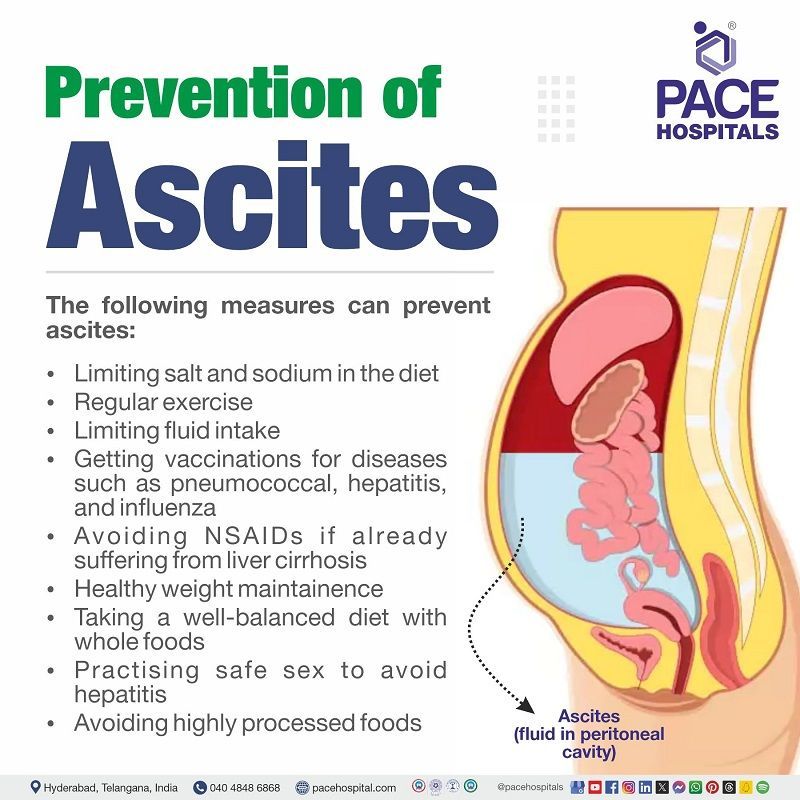
Prevention of ascites
The following measures can prevent ascites:
- Limiting salt in the diet
- Reducing sodium intake
- Exercising regularly
- Limiting fluid intake
- Getting vaccinations for diseases such as pneumococcal, hepatitis, and influenza
- Avoid taking NSAIDs (non-steroidal anti-inflammatory drugs) if the patient is suffering from liver cirrhosis
- Weight observation is to be done in order to get rid of weight gain
- Avoid recreational drugs in order to reduce the occurrence of hepatitis
- Taking a well-balanced diet
- Practising safe sex in order to prevent hepatitis
- Avoid highly processed foods and consume whole foods
Difference between transudate and exudate ascites
Transudate vs exudate ascites
Ascites can be represented as exudate or transudate ascites. Transudative ascites can result from portal hypertension, congestive heart failure, or hypoalbuminemia, whereas exudative ascites might be due to malignancy, infection, or inflammation.
Difference between ascites and belly fat
Ascites vs belly fat
Ascites and abdominal fat might appear the same; however, a medical professional can distinguish between the two.
- Fat and ascites feel and move differently. A physician can examine a patient's abdomen in both standing and lying-down positions. The abdomen's shape or appearance may indicate whether there is fat or fluid inside it.
- An enlarged, firm and bloated or swollen abdomen is another identical symptom of ascites. Patients with ascites might also see abrupt body shape and weight changes. These ascitic changes occur significantly faster than the average rate of increase in body fat mass.
Difference between anasarca and ascites
Anasarca vs ascites
Anasarca is often referred to as generalised oedema, whereas the ascites is characterised by fluid accumulation in the abdominal cavities (effusion in the abdominal cavity and hydrothorax).
FAQs - Frequently asked questions on ascites
Can ascites be reversed?
Usually, mild to moderate ascites can be treated by the treatment and some lifestyle modifications. However, ascites in severe cirrhotic or decompensated cirrhosis might not be cured completely but can be reversible temporarily with ascites medications and treatment. Complicated ascites with end-stage liver disease might eventually need a liver transplant.
When is ascites life threatening?
If the patient is experiencing sudden fever and belly pain with ascites, it could be a serious, life-threatening infection. Then, the patient should immediately seek a medical appointment by visiting the liver specialist (hepatologist).
What is the best treatment for ascites?
For minimal ascites, diuretic therapy and sodium restriction (20–30 mEq/d) are referred to as the standard treatments. According to the studies, this treatment is considered adequate in approximately 95% of the mild ascites patients. Severe and uncomplicated ascites cases might require some invasive treatment, such as paracentesis (ascitic fluid tapping), shunts, and surgeries.
Can liver recover from ascites?
Ascites in cases of alcohol-associated hepatitis might be resolved if the liver's function improves. However, in severe ascites cases, it depends on the severity of the ascites and the patient's condition.
How do you confirm ascites?
One can't confirm the ascites by themselves. Suppose the patient is assumed to have any ascites-like symptoms. In that case, one should visit the liver specialist (hepatologist) to make confirmation regarding the present condition.
Is drinking water good for ascites?
Usually, patients with ascites might be suggested to eat less salt and drink less water or fluids to prevent mild discomfort. Nevertheless, one should visit the surgical gastroenterologist or hepatologist (liver specialist) to get confirmation regarding these dietary changes.
What is Ehrlich ascites carcinoma?
EAC, or Ehrlich ascites carcinoma, is one of the most common tumours. EAC is known as an undifferentiated carcinoma; it initially emerged as hyperdiploid, has a high potential for transplantation, exhibits no regression, multiplies quickly has a shortened life span, and is 100% malignant. It lacks tumour-specific transplantation antigen (TSTA).
Why does cancer cause ascites?
Initially, malignant ascites can result from cancer spreading to the peritoneum, the lining that lines the organs, and causing it to leak. In addition, cancer has the potential to spread to the liver and raise its intrahepatic pressure. A number of cancers have an increased risk of causing ascites, particularly pancreatic, liver, colon, and ovarian cancers.
What happens if ascites doesn't go away?
If ascites is not treated properly, it might cause serious liver damage and complications that are usually life-threatening.
Which doctor treats ascites?
Ascites is usually treated by liver specialists (hepatologists) or surgical gastroenterologists.
Share on
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868