End Stage Liver Disease: Symptoms, Causes, Complications, Treatment
Pace Hospitals
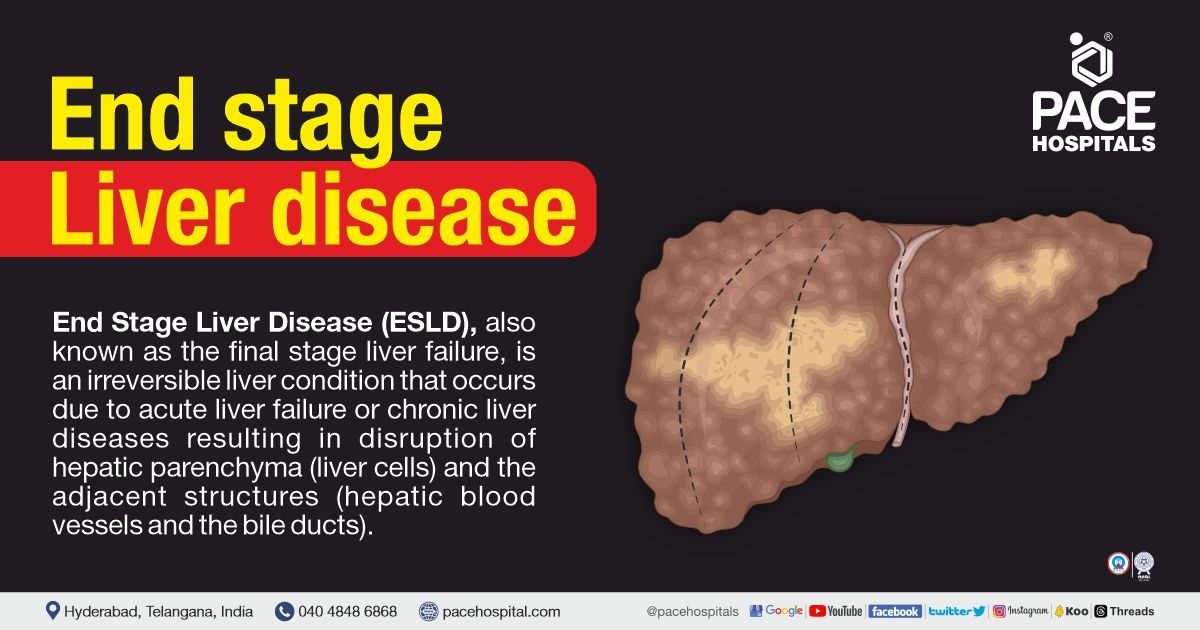
ESLD - End stage liver disease definition
End stage liver disease (ESLD), also known as the final stage liver failure, is an irreversible liver condition that occurs due to acute liver failure or chronic liver diseases resulting in disruption of hepatic parenchyma (liver cells) and the adjacent structures (hepatic blood vessels and the bile ducts). It is a culmination of chronic liver disease that progresses to cirrhosis, decompensation, and chronic liver failure, which might lead to portal hypertension or complications related to hepatic failure.
The end stage liver disease is characterised by the presence of (any) chronic liver failure, decompensated cirrhosis (scar tissue replaces damaged tissue in the liver), and stage 4 hepatitis. Patients with end stage liver disease usually have either decompensated or compensated cirrhosis.
- Decompensated liver disease: Cirrhotic patients under this category have an acute deterioration in liver function characterised by severe symptoms and complications that increase the risk of mortality.
- Compensated liver disease: Patients are often asymptomatic or have few symptoms, though the patient has progressed to cirrhosis (the last stage of liver failure). Some patients with compensated liver disease can develop hepatocellular cancer.
Pediatric End-Stage Liver Disease (PELD)
Pediatric end-stage liver disease (PELD) raises unique management challenges for paediatricians, as the complications associated with pediatric end stage liver disease are portal hypertension, encephalopathy, spontaneous bacterial peritonitis and ascites. The causes and natural history of ESLD in children vary depending on the age of presentation. Children are particularly prone to malnutrition, developmental delays, and fragility. Nutritional support plays a crucial role in the management of ESLD as it significantly impacts the clinical course and survival before and after liver transplantation.
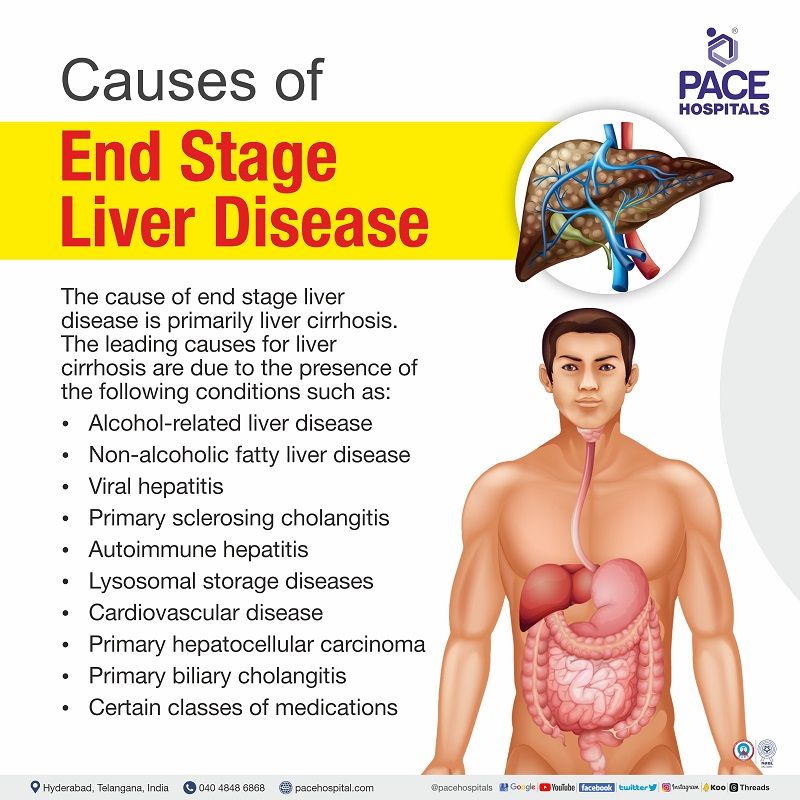
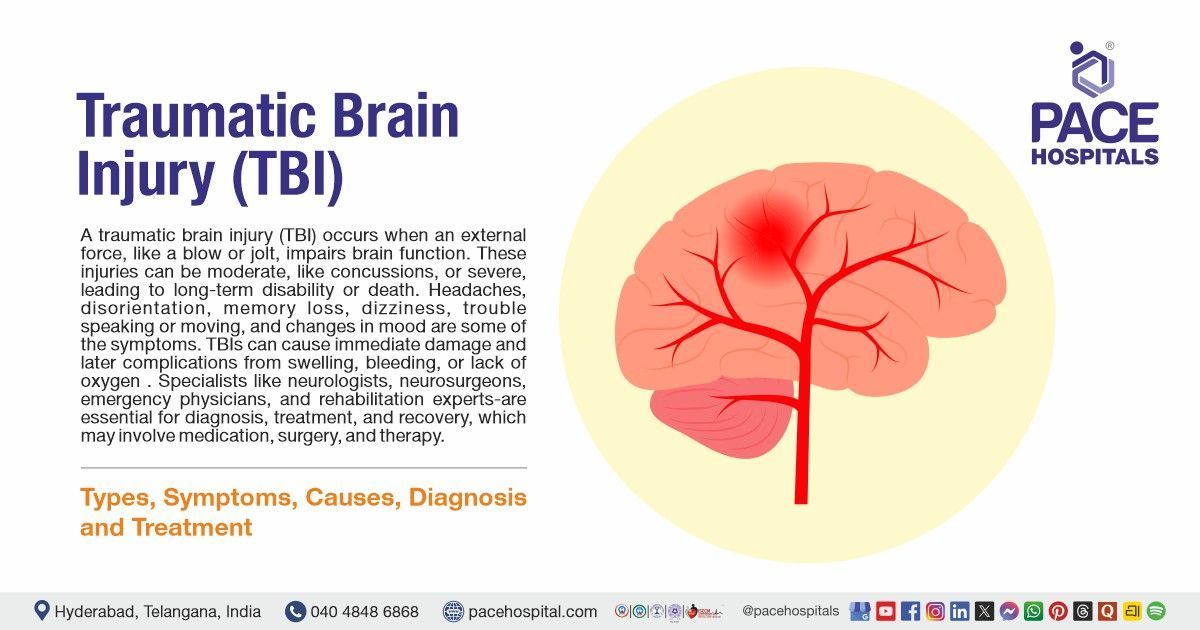
End Stage Liver Disease Causes
The cause of end stage liver disease (ESLD) is primarily liver cirrhosis (formation of scar tissue throughout the liver). The leading causes for liver cirrhosis are due to the presence of the following conditions, such as:
- Alcohol-related liver disease (ARLD)
- Non-alcoholic fatty liver disease (NAFLD)
- Viral hepatitis
- Primary sclerosing cholangitis (PSC)
- Autoimmune hepatitis
- Lysosomal storage diseases
- Cardiovascular disease
- Primary hepatocellular carcinoma
- Primary biliary cholangitis
- Certain classes of medications
End Stage Liver Disease Symptoms
The signs and symptoms of end stage liver disease are numerous, especially in the terminal phase of a patient's life. The following are some of the symptoms of ESLD such as:
- Peripheral oedema
- Dyspnoea (shortness of breath)
- Yellowish discoloration of the skin and sclera (jaundice)
- Disorientation and memory loss
- Vomiting sensation
- Muscle cramps
- Loss of hunger
- Insomnia (trouble falling asleep)
- Depression and anxiety
- Impaired brain functions
- Pruritus (itching)
Complications of End Stage Liver Disease (ESLD)
The end stage liver disease complications do have recognisable symptoms, including:
- Ascites
- Hepatic encephalopathy
- Oesophageal Varices
- Infections
- Kidney failure
- Bruising and bleeding
- Portal hypertension
- Splenomegaly
- Jaundice
- Gallstones
- Liver cancer
- Insulin resistance and type 2 diabetes
- Sensitivity to medications
Ascites: Fluid accumulation of the abdomen is a serious complication of liver disease that can lead to bloating, pain in the abdomen, abdominal swelling, and shortness of breath. Research reports show patients with liver disease and ascites die within 24 months.
Hepatic encephalopathy: Hepatic encephalopathy (HE) occurs when the brain's ability to function is hampered by the accumulation of toxins in the bloodstream. Patients with hepatic encephalopathy can survive for one year. The risk of HE increases as the patient’s condition (end stage liver disease) deteriorates.
Oesophageal varices: Oesophageal varices are dilated veins that arise when liver scar tissue restricts blood supply to the digestive tract. The oesophageal veins enlarge as the blood backs up. Varices can bleed and rupture without medical intervention, which is potentially fatal. The symptoms include hematemesis (blood vomiting), black and tarry stools, or lightheadedness.
Infections: End stage liver disease can lead to spontaneous bacterial peritonitis or pneumonia, which are also complications for ascites.
Kidney failure: 10% of the patients with liver failure may also develop kidney failure. Although kidney function is significantly hampered, the kidneys are unharmed. The exact cause for this complication is idiopathic (unknown); however, some researchers opine it might be due to blood pressure and blood flow variations.
Bruising and bleeding: In end stage liver disease, the liver's production of blood-clotting proteins is reduced, resulting in bruising and bleeding easily.
Portal hypertension: The portal vein is responsible for transporting blood from the digestive tract, pancreas and spleen to the liver. The congestion of the blood flow and augmented hepatic vascular resistance caused by chronic end stage liver disease result in elevated portal venous pressure (portal hypertension).
Splenomegaly: Due to portal hypertension, white blood cells and platelets are held in the enlarged spleen, resulting in a lower blood count. Cirrhosis, in some cases, might first be detected by a drop in platelet count.
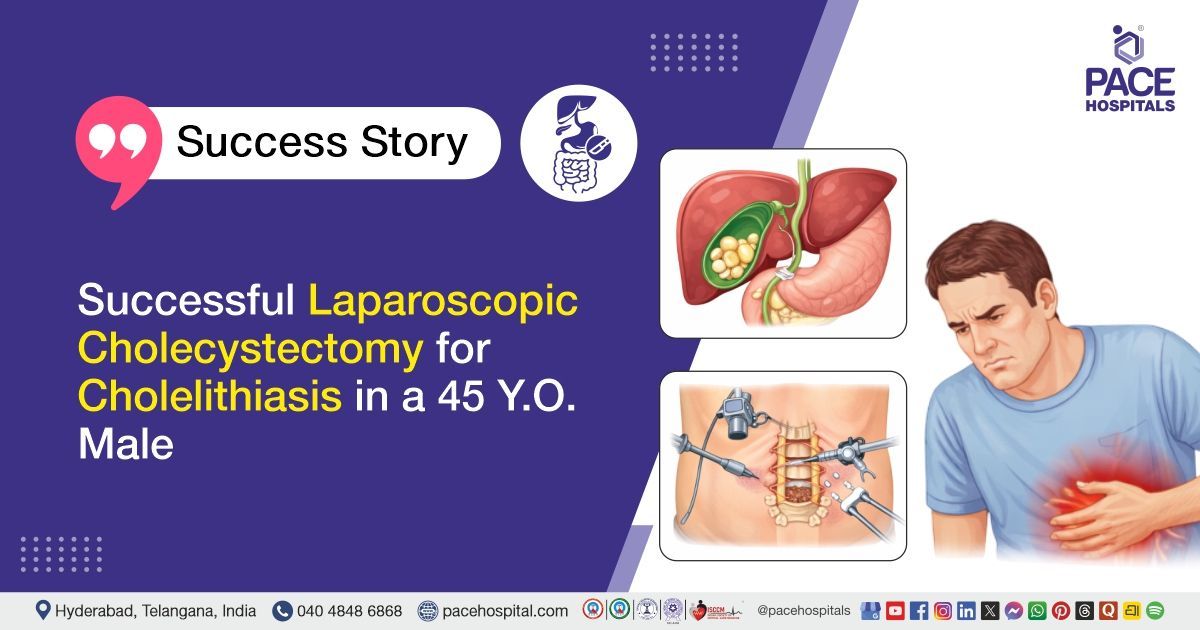
Gallstones: The liver's cirrhotic stage prevents bile's free flow, and the accumulation of bile hardens, resulting in the formation of gallstones.
Liver cancer: Hepatocellular carcinoma (HCC) develops in cirrhosis when cells in the damaged liver begin to proliferate uncontrollably.
Insulin resistance and type 2 diabetes: Insulin resistance is a consequence of cirrhosis; insulin (a hormone secreted by the pancreas) aids the human body to utilise glucose for energy production. In the case of insulin resistance, the body's fat, muscle and liver cells fail to respond normally to insulin. Despite the pancreas' best efforts in releasing insulin, glucose levels in the blood continue to rise, leading to type 2 diabetes.
Sensitivity to medications: Liver cirrhosis disables the liver function of filtering medications from the blood, resulting in longer actinons of medications and their accumulation in the body. This results in increased medication sensitivity.
Management of End stage liver disease complications
The hepatologist aims to provide personalised care to treat complications and prevent recurrence in patients with end stage liver disease. However, the management of end stage liver disease varies based on the patient's condition and medical history. The following are the management of some of the most common complications of end stage liver disease.
Ascites
The hepatologist would like to treat underlying conditions such as alcoholic liver disease (ALD), autoimmune hepatitis, and hepatitis B. In patients with portal hypertension–associated ascites, a daily dietary sodium intake restriction will be suggested (less than 2000 mg).
Hepatic encephalopathy
Ammonia is the toxin most frequently implicated in the pathophysiology of hepatic encephalopathy, as the liver fails to filter the toxins. Addressing precipitating factors, lowering gut-derived nitrogenous products, and implementing concurrent supportive treatment are the cornerstones of hepatic encephalopathy management. The hepatologist would like to prescribe nonabsorbable disaccharides as they lower gut pH and interfere with glutamine uptake, reducing both ammonia synthesis and its absorption.
Spontaneous bacterial peritonitis (SBP)
The hepatologists might prescribe prophylactic medications both for primary and secondary prevention in patients with primary SBP (in patients who never had SBP but are at high risk of SBP such as medical history of variceal bleeding or ascites fluid protein levels < 1.0 g/dL) and secondary SBP. Primary prophylactic medications have been linked to a reduced risk of bacterial infection and decreased mortality.
Oesophageal Varices
Management of primary prophylaxis (in patients who never had bled but are at high risk of bleeding) includes screening endoscopy, the results of endoscopy that characterise the size and features of the varices. Patients with Child B or C cirrhosis, who are thought to be at elevated risk of variceal bleeding, may be administered medical therapy for primary prevention with the goal of lowering portal hypertension.
Secondary prophylaxis (prevention of reoccurrence in patients who have a history of bleeding) focuses on supportive care and optimising medications.
End stage liver disease death timeline
The end stage liver disease (ESLD) life expectancy depends on various factors such as severity, causes, type, the severity of complications and associated comorbid conditions. Patients with compensated liver disease have a median survival time of more than 12 years, whereas in patients with decompensated liver cirrhosis, the median survival time is nearly two years .
The severity of hepatic decompensation is typically a significant prognostic factor. The prognosis of liver decompensation (ESLD prognosis) has been predicted by numerous research using clinical and laboratory evaluations of liver function. The Child-Pugh classification and the Model for End stage Liver Disease (MELD) score are often employed models.
Child-Pugh classification
It is also known as the Child-Pugh-Turcotte score; initially, it is used to assess the non-shunt operations risk in liver cirrhosis patients. In patients with cirrhosis, the Child-Pugh classification system correlates with cirrhotic patients' survival rates (one-year survival rates for Child-Pugh classes A, B, and C cirrhosis are nearly 100, 80, and 45%, respectively).
Patients with Child- Turcotte-Pugh scores greater than or equal to 7 are referred for a liver transplant.
Click here to learn "How to calculate the Child-Pugh-Turcotte score".
Model for End stage Liver Disease
- The severity of the patient’s liver disease can be assessed through the model for end stage liver disease (MELD) or end stage liver disease score. It is used to evaluate the probability of patient death from liver failure within three months (90 days) in patients with a transjugular intrahepatic portosystemic shunt placement.
- The sodium MELD (MELD-Na) evaluates the mortality among those placed on a liver transplant waitlist. Since 2015, the serum sodium level was added to determine MELD score after evidence emerged demonstrating that the serum sodium level is an independent predictor of death among cirrhosis patients who are on transplant waiting lists.
- MELD score is used to prioritise patients who require a liver transplant, in addition to aiding the hepatologists in prescribing alternative forms of treatment for liver failure patients.
- The MELD process involves testing patients’ bilirubin, International normalised ratio, sodium and creatinine levels. The resulting values will be entered into an algorithm to obtain a score between 0-40. Higher score indicates a more severe condition, abnormal liver function and increased mortality risk.
- The MELD score of more than or equal to 10 will be referred to a liver transplant.
Pediatric end stage liver disease score:
It is used to prioritise paediatric patients (aged less than 12 years) who require a
pediatric liver transplant. The pediatric end stage liver disease score is calculated based on the patient's bilirubin, International normalised ratio, albumin, age of the patient (if less than one year), presence of growth failure (height and weight less than two standard deviations). Similar to MELD, PELD also measures the probability of 90-day pretransplant death.
End Stage Liver Disease Diagnosis
Although symptomatic patients exist, most persons with compensated cirrhosis are asymptomatic. The patient’s history and physical examination are typically taken into account before prescribing lab tests, imaging tests, and liver biopsy tests.
Blood tests:
- To measure the values of liver diagnostic indicators such as Albumin, Bilirubin, Gamma-glutamyl Transferase, Aspartate transaminase (AST), Prothrombin time, Alkaline phosphatase (ALP), International normalised ratio, Alanine transaminase (ALT), Creatinine, Sodium, Serum ceruloplasmin, Immunoglobulins (IgA, IgG and IgM), Red and white blood cell counts.
- To screen for hepatitis (B&C) and genetic diseases presence.
Imaging tests:
To have a definitive diagnosis, the hepatologist might prescribe any of the following tests.
- Liver ultrasound
- CT Scan
- MRI Scan
- Endoscopy
- Transient elastography and Magnetic resonance elastography
End Stage Liver Disease Treatment
Treatment for ESLD will differ based on the disease underlying cause and the severity of the liver damage. Treatment goals include decreasing scar tissue progression in the liver, managing complications and preventing their recurrence. There is no medical treatment to cure End stage liver disease; however, medical management can help to control symptoms and delay the disease's progression, which aids in improving the patient's quality of life and extending their lifespan.
In case of difficulty in managing the complications, a liver transplant is considered. A liver transplant is a significant surgical procedure where a damaged liver is replaced with a healthy liver from an organ donor.
Palliative Care End Stage Liver Disease
Palliative care is an interdisciplinary medical speciality that aids in providing medical care focused on preventing and relieving pain, thereby promoting quality of life in patients with chronic diseases such as end stage liver disease (ESLD) waiting for a liver transplant.
Patients with ESLD, requiring a liver transplant, have severe complications, suffering and discomfort as the disease progresses, resulting in a reduction in the patient's quality of life. Many ESLD patients waiting for a liver transplant die, as the allocation of a donor is based on the patient’s severity, which places them in a sort of limbo (uncertain situations) where the disease cannot be cured, nor can they wait for their turn. For such patients, judicious application of palliative care can aid them in managing their condition.
Palliative care aligns with the patient's values and preferences in providing symptom management and harmonious communication between care providers and patients, in addition to providing psychosocial, spiritual, and emotional support to end stage liver disease patients and their family members. The benefit of end stage liver disease palliative care is to free from emotional distress and physical symptoms, thereby improving the patient's and their relative’s quality of life.
As per a 2022 research report, patients who received palliative care reported improvements in itching, well-being, hunger, anxiety, and depression, as well as an increase in the number of do-not-resuscitate orders, palliative care consultations and decreased hospitalisation.
Challenges of ESLD palliative care
There are various challenges in implementing palliative care in patients with ESLD.
- Some patients are asymptomatic for years following a cirrhosis diagnosis and develop ESLD symptoms abruptly, making it difficult for patients to prepare for the inevitable progression of their disease.
- Palliative care is sometimes equated with "end-of-life" care, a common misperception among patients and medical professionals. Due to this, there will be a delay in receiving palliative care, resulting in waiting until they are off the transplant list.
- Competing time demands and a lack of comfort in discussing goals of care and cultural competence pose barriers for physicians in providing palliative care.
Prevention of End Stage Liver Disease (ESLD)
The prevention of end stage liver disease includes avoidance of prolonged liver cirrhosis or liver damage.
The following are the measures that aid in preventing end stage liver disease (ESLD):
- Adoption of a healthy lifestyle that includes.
- Regular exercise
- Abstinence of alcohol
- Consumption of a balanced diet
- Prevention of consuming highly processed foods and a diet rich in salt.
- Regular screenings for liver disease
- Adherence to prescribed liver cirrhotic medications, thereby halting the liver disease progression to ESLD.
Diet for End Stage Liver Disease (ESLD)
Diet plays a crucial role in the overall management of ESLD, as malnutrition is common in patients with end stage liver failure that affects patients' survival, outcome, and quality of life. The metabolism of nutrients, their distribution, and the body's efficient utilisation of them are all processes that the liver plays a vital part in regulating.
The following are the dietary preferences in patients with liver cirrhosis or with end stage liver disease:
Diet rich in
- Fruits and vegetables such as beans, cauliflower, peas, apples, oranges, and berries.
- Seeds such as flaxseed, pumpkin and hemp
- Whole grains such as brown rice and oats
- Nuts such as almonds and cashews
- Healthy oils such as avocado, olive, and salmon
- Herbs and spices such as cumin and black pepper
Difference between Child-Pugh score and MELD model of end stage liver disease
Both the scores are used to predict the outcomes of cirrhotic patients. However, the following are the differences between them.
| Elements | Child-Pugh score | MELD score |
|---|---|---|
| Sensitivity and specificity | Higher sensitivity and lower specificity in patients with acute-on-chronic liver failure, compared to MELD score and higher specificity in patients undergoing surgery. | Higher sensitivity and smaller negative likelihood ratio in patients admitted in ICU, compared to Child–Pugh score and lower specificity in patients undergoing surgery compared to Child–Pugh score. |
| Initially used for predicting | Operative risk in a patient undergoing portosystemic shunt surgery for variceal bleeding | Patient’s survival undergoing transjugular intrahepatic portosystemic shunts (TIPS) |
| Primary version includes | Ascites*, nutritional status, total bilirubin, hepatic encephalopathy* and albumin | Causes of liver cirrhosis |
| Current version includes | Removal of nutritional status and addition of prothrombin time or international normalised ratio (INR), widely used to assess liver dysfunction severity | Total bilirubin, creatinine, and INR to rank the priority of liver transplantation candidates |
Share on
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868