Chronic Kidney Disease - Symptoms, Stages, Causes, Complications, Prevention
PACE Hospitals
Chronic Kidney Disease definition / meaning
Chronic Kidney Disease (CKD) / Chronic renal failure is a long-term (chronic) condition comprised of progressive and irreversible deterioration of renal capacity due to slow destruction of renal parenchyma (the kidney), the kidneys gradually lose their ability to filter blood. This can lead to a buildup of waste products and fluids in the body, which can cause a variety of health problems, eventually leading to death when enough nephrons (the functional unit of the kidney) have been damaged.
The most common causes of CKD are diabetes and high blood pressure. CKD is often asymptomatic in the early stages. Acidosis (condition of increased acid in the body fluids) is the major problem in chronic kidney disease, with the development of biochemical azotaemia (build-up of nitrogenous products in the blood) and clinical uraemia syndrome.
CKD full form in medical terms - Chronic Kidney Disease
Chronic kidney disease, another name for chronic renal failure. Although the medical term CKD/ chronic kidney disease/ chronic renal failure hadn’t been coined, throughout the older history, its symptoms such as pyuria (pus in the urine), pain and fever, had been edified in Greek and Roman antiquity. Only in the 18th century, after proteinuria (protein in urine – an abnormal condition) was discovered, the work on CKD accelerated, especially with Dr Bright, who in 1827 demonstrated the first, nearly complete clinical description of acute and chronic glomerulonephritis (inflammation of glomerulus) and the macroscopic differences seen in the kidneys.
Global Prevalence of Chronic Kidney Disease (CKD)
More than 10% of the world's population (>80 crores individuals, especially with older and diabetic populations and hypertension) in the world are suffering from the progressive condition of chronic kidney disease or CKD.
As CKD is emerging as one of the leading causes of mortality, with its increasing death rate in the last two decades, its heavy burden is mostly seen in low- and middle-income countries.
Prevalence of CKD in India
Chronic Kidney Disease (CKD) patients pose a significant public health problem due to its high morbidity, prevalence, and mortality.
- Hosting around 17% of the Earth’s population with a little over 3% of global land mass, India faces challenges in providing access to healthcare.
- While the International Society of Nephrology’s Kidney Disease Data Centre Study demonstrated a 17% prevalence of CKD among Indians, the majority of the patients approach the healthcare personnel when their estimated glomerular filtration rate (eGFR) is <15 ml/min per 1.73m2.
- High levels of prevalence are seen in parts of Andhra Pradesh, Goa, and Odisha.
Types of Chronic Kidney Disease (CKD)
Chronic kidney disease can arise from different underlying conditions that gradually damage kidney structure or normal function. Identifying the type of CKD based on its cause helps doctors plan appropriate treatment plan, slow progression, and reduce complications. The main types of CKD are outlined below:
- Diabetic Kidney Disease (Diabetic Nephropathy)
- Hypertensive Kidney Disease
- Glomerular Diseases
- Polycystic Kidney Disease (PKD)
- Chronic Tubulointerstitial Kidney Disease
- Obstructive Uropathy–Related CKD
- Recurrent or Chronic Kidney Infections
Diabetic Kidney Disease (Diabetic Nephropathy)
This is the most common cause of chronic kidney disease worldwide. Long-standing diabetes condition damages the small blood vessels in the kidneys, reducing their ability to filter waste effectively. Early detection and strict blood sugar control can slow disease progression.
Hypertensive Kidney Disease
Chronic high blood pressure can damage kidney blood vessels over time, leading to progressive loss of kidney function. Poorly controlled hypertension accelerates kidney damage and increases the risk of heart disease.
Glomerular Diseases
These conditions affect the glomeruli, the tiny filtering units of the kidney. They may be caused by immune disorders, infections, or systemic diseases. Glomerular diseases can lead to protein loss in urine and gradual
kidney failure if untreated.
Polycystic Kidney Disease (PKD)
PKD is a genetic condition in which multiple fluid-filled cysts develop in the kidneys. Over time, these cysts enlarge and interfere with normal kidney function, often leading to chronic kidney disease.
Chronic Tubulointerstitial Kidney Disease
This form of CKD affects the kidney tubules and surrounding tissues. It may result from long-term medication use, recurrent infections, toxins, or inherited disorders. Kidney damage usually develops slowly and may be difficult to detect early.
Obstructive Uropathy–Related CKD
Long-standing blockage in urine flow due to kidney stones, prostate enlargement, tumors, or structural abnormalities can cause back pressure on the kidneys and lead to chronic damage.
Recurrent or Chronic Kidney Infections
Repeated kidney infections (chronic pyelonephritis) can cause scarring of kidney tissue, gradually reducing kidney function over time.
Chronic Kidney Disease - CKD Symptoms
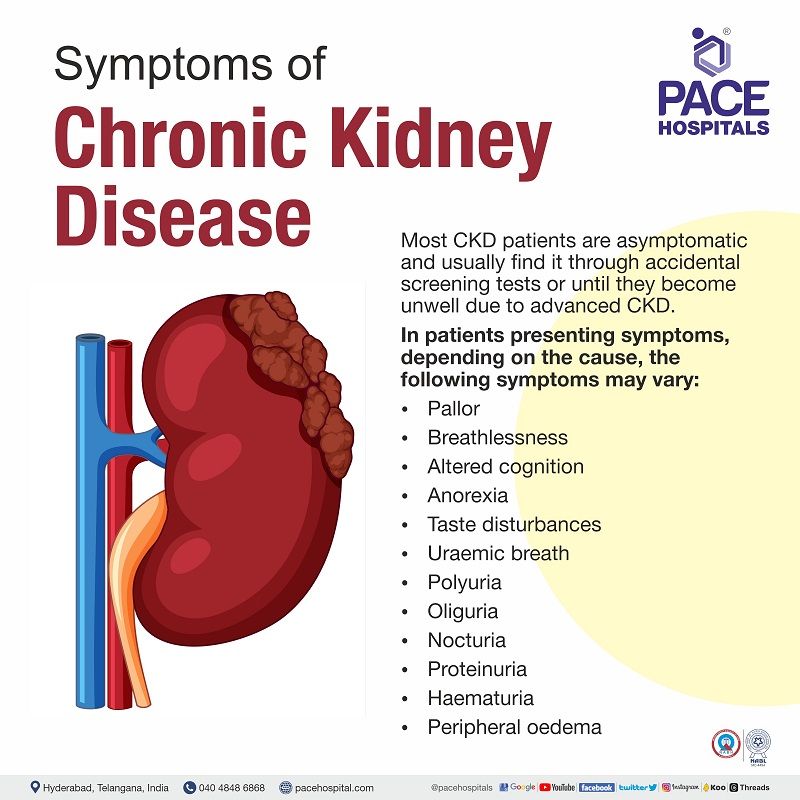
Many Chronic Kidney Disease (CKD) patients are asymptomatic and usually find it through chance findings from regular screening tests, usually through a routine medical examination or until they become unwell due to advanced CKD.
However, depending on the cause, in a few CKD patients, the symptoms are seen due to impaired kidney function. As CKD progresses, kidney function becomes less effective and uraemic toxins accumulate in the body.
These uraemic toxins not only help in the progression but also influence either directly or indirectly influence biochemical and physiological effects in CKD patients, contributing to immune dysfunction, vascular disease, platelet dysfunction and increased bleeding risk, dysbiosis in the gut (imbalance” in the gut microbes), altered drug metabolism. A few of the chronic renal failure symptoms can be seen below:
- Pallor (an unhealthy pale appearance) is usually due to anaemia from CKD.
- Shortness of breath is due to fluid overload, anaemia, cardiomyopathy etc.
- Itching is usually due to uremic toxins and the deregulation of the immune response.
- Cramps are typically worse at night due to neuronal irritation caused by biochemical abnormalities in CKD patients.
- Cognitive changes are seen in CKD patients, and skills decline at different rates. Language and attention may be particularly affected.
- Gastrointestinal symptoms such as anorexia (an eating disorder of obsessing overweight and intake), vomiting, and taste disturbance may occur in advanced CKD patients.
- The caretakers may notice uraemic breath in advanced CKD patients due to the breakdown of urea by saliva.
- Change in urine output, such as polyuria (more urination) due to impaired tubular concentration, oliguria (small amounts of urine), nocturia (urine during the night), and proteinuria (protein in urine).
- Haematuria (blood in urine)
- Peripheral oedema (swelling in your lower legs or hands) due to renal sodium retention.
Causes of CKD - Chronic Kidney Disease
The pathophysiology of CKD or chronic renal failure (CRF) could potentially include almost all chronic nephropathies. The diseases leading to CRF can generally be classified into two major groups: those causing glomerular pathology and those causing tubulointerstitial pathology.
Diseases causing glomerular pathology
Several glomerular diseases associated with CKD patients originate from immune system disturbances. Glomerular destruction changes in the filtration process, leading to nephrotic syndrome. Examples of glomerular diseases are chronic glomerulonephritis (glomerulus inflammation), membranoproliferative glomerulonephritis, lipoid nephrosis, systemic lupus erythematosus, etc.
Diseases causing tubulointerstitial pathology
Tubulointerstitial damage alters the reabsorption and secretion of important constituents, which leads to large volumes of diluted urination. A few of the tubulointerstitial conditions are nephrosclerosis, chronic pyelonephritis, chronic renal infection, drug toxicity, and chronic obstruction such as stones, blood clots, tumours, enlarged prostate etc.
Major causes of CKD - Chronic Kidney Disease
Nearly 45% of incident kidney failure is attributed to diabetes, and another 20% is attributed to chronic hypertension. The five major causes of CKD accounting for >90% of the burden are listed below:
- Diabetic nephropathy
- Glomerulonephritis
- Hypertension-associated CKD such as:
- Vascular and ischemic kidney disease
- Primary glomerular disease with associated hypertension
- Autosomal dominant polycystic kidney disease
- Cystic and tubulointerstitial nephropathy
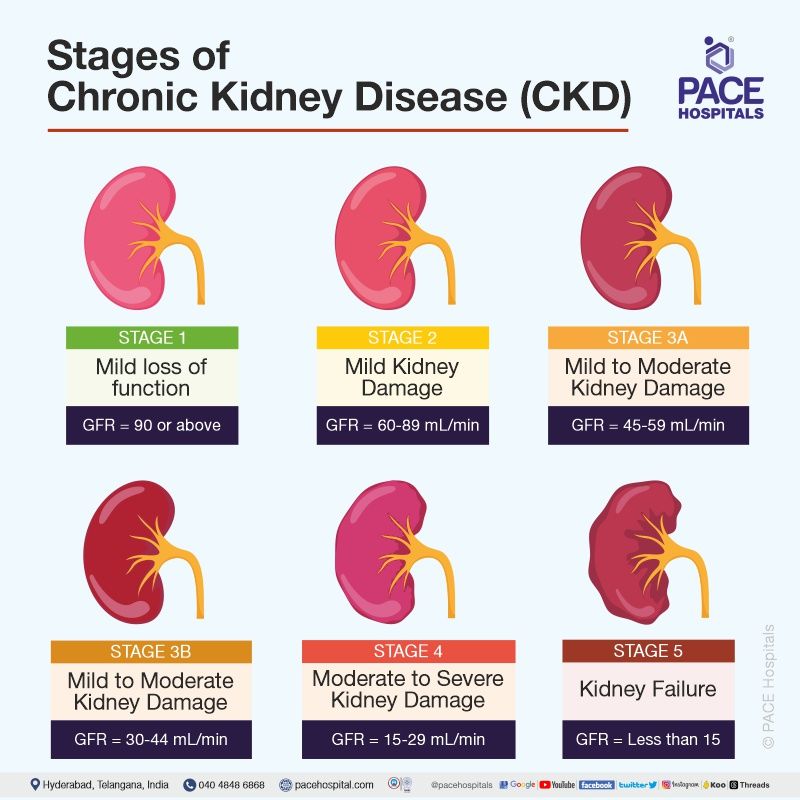
Chronic Kidney Disease - CKD stages
There are five (5) stages in the kidney disease. Stage of kidney disease is determined by the glomerular filtration rate (GFR) and the presence of kidney disease. Glomerular filtration rate is the measure of kidney function. As Chronic kidney disease progresses GFR decreases. Treatment of chronic kidney disease patients is based on stage of the disease.
| Stage | Description | Glomerular filtration rate (GFR) |
|---|---|---|
| 1 | Kidney damage (e.g., protein in urine) with normal GFR | 90 or above |
| 2 | Kidney damage with mild decrease in GFR | 60 to 89 |
| 3A | Moderate decrease in GFR | 45 to 59 |
| 3B | Moderate decrease in GFR | 30 to 44 |
| 4 | Severe reduction in GFR | 15 to 29 |
| 5 | Kidney failure | Less than 15 |
Risk Factors for CKD - Chronic Kidney Disease
There has been significant recent progress in the identification of risk factors that increase the risk for chronic kidney disease, even in individuals with normal glomerular filtration rates.
Adults with such risk factors must get screened at least every two years for albuminuria (increased albumin in the urine) and blood pressure abnormalities to arrest CKD development. The various risk factors which can influence contracting CKD include:
Chronic Nonrenal (Systemic) Disease
- Diabetes, hypertension, and metabolic syndrome – Through obesity, dyslipidaemia, insulin resistance, and oxidative stress, the pathogenesis of CKD is seen with diabetes and metabolic syndrome.
- Autoinflammatory disease - CKD could occur due to the effector responses which target the kidneys.
- Infections (e.g., HIV, HBV, HCV) – Apart from direct infection of renal parenchyma, microbes can induce CDK through 3 paths:
- Kidney complications due to liver disease.
- Drug-induced CKD.
- Glomerular immune complex deposition.
- Nephrotoxic exposure (including many antineoplastic therapies)- Various proponents of chemotherapies cause nephrotoxicity, which can induce CKD with long-term use.
Demographical and genetical factors
- Age and gender – A 2022 study demonstrated that although female CKD patients are more prevalent, the majority of male CKD patients receive kidney replacement therapy as the mean glomerular filtration rate in women was slower than in men among the elderly and the middle-aged population. Usually, CKD patients are the elderly.
- Family history - Genetic research demonstrated that predisposition to common complex diseases due to DNA sequence variants at several genetic loci are associated with CKD.
Childhood and Adolescent States and Diseases
- Premature birth - Due to decreased nephrons and post-natal exposure to nephrotoxins, premature infants are at a higher risk of chronic kidney disease.
- Treated childhood cancer - Due to unknown reasons in certain cases, adult survivors of childhood cancer could have a higher risk of CKD.
- Lifestyle factors such as smoking, alcoholism, and low physical activity could increase various proponents, which could increase BMI, hypertension, and metabolic diseases, which can increase the chances of CKD.
Complications of CKD - Chronic Kidney Disease
The complications of chronic renal failure could display through various clinical manifestations due to uraemic syndrome. The complications of chronic kidney disease are divided into primary (renal) uraemic manifestations and secondary (systemic or extra-renal) uraemic manifestations based upon the locality.
Primary uraemic (renal) manifestations develop slowly, deteriorating the renal function and resulting in:
- Metabolic acidosis - Renal dysfunction causes acid-base imbalance resulting in metabolic acidosis, causing hyperkalaemia (increased potassium in the blood) and hypercalcaemia (increased calcium in the blood).
- Hyperkalaemia - Excessive accumulation of potassium in the blood since potassium excretion is hampered, causing cardiac arrhythmias, weakness, nausea, etc.
- Sodium and water imbalance - Due to renal dysfunction, sodium and water cannot pass sufficiently into Bowman’s capsule leading to their retention. The main symptoms are hypervolaemia and circulatory overload with congestive heart failure.
- Hyperuricaemia - Excess levels of uric acid in the blood lead to its progressive deposition in joints and soft tissues resulting in gout disease.
- Azotaemia - Protein metabolism results in the production of waste products (urea, creatinine, phenols and guanidines), but since the kidney is redundant, they are circulated in the body.
Secondary uraemic (extra-renal) manifestations usually develop due to the fluid-electrolyte and acid-base imbalances resulting in:
- Anaemia - Decreased production of erythropoietin (a hormone for blood) causes a decline in erythropoiesis (red blood cell production), resulting in anaemia.
- Nephrogenic fibrosing dermopathy - A very rare condition of progressive integumentary induration (skin hardening), especially on the arms and legs.
- Congestive heart failure - Since fluid retention causes hypervolaemia (increased fluid in the body) and therefore increased workload on the heart, it eventually leads to congestive heart failure.
- Pulmonary congestion (condition of fluid in the lungs) - due to the back pressure caused by hypervolaemia and heart failure, pulmonary congestion is caused.
- Mucosal ulcerations - Azotaemia is directly involved in mucosal ulcerations in the lining of the stomach and intestines. The subsequent bleeding can aggravate anaemia.
- Renal osteodystrophy - In extreme renal dysfunction, the drastic changes in minerals and hormones cause the weakening of bone and are in your blood. The main signs are bone pain and fractures.
Chronic Kidney Disease - CKD Diagnosis
Chronic kidney disease (CKD) is diagnosed with a combination of blood tests, urine tests, and imaging tests, including:
- Physical examination and history taking
- Kidney assessment tests (both serum and urine tests)
- Imaging tests
- Chronic renal failure ultrasound (Ultrasonography)
- Renal doppler in chronic kidney disease (Doppler ultrasonography)
- Intravenous urography (IVU)
- Computed tomography (CT)
- Magnetic resonance imaging (MRI)
- Magnetic resonance angiography (MRA)
- Nuclear medicine investigations
The stage of CKD is determined by the GFR. The GFR is divided into six stages, with stage 1 being the least severe and stage 5 being the most severe.
CKD - Chronic Kidney Disease Treatment
The goal of CKD treatment is to slow the progression of the disease and maintain a good quality of life. With proper care, many people with CKD can live long and healthy lives. The treatment of CKD can be summarised as:
- Reverse or arrest the process causing the renal damage.
- Prevention of conditions that might worsen renal failure.
- Treatment of CKD symptoms and its secondary complications.
- Chronic kidney disease dialysis and transplantation.
Why Choose PACE Hospitals?
Expert Super Specialist Doctors
Advanced Diagnostics & Treatment
Affordable & Transparent Care
24x7 Emergency & ICU Support
Prevention of CKD - Chronic Kidney Disease
Avoiding exposure to various proponents which cause disease is necessary as prevention is more effective than cure. In this particular disease - Chronic Kidney Disease (CKD), the treatment plan also consists of various dietary and lifestyle adaptations that diametrically help in reducing the ailment.
- CKD diet: The dietary factors which can reduce the risk of CKD are dairy products, fibre, folate, cereal fibre, coffee, legumes, magnesium, nitrate, plant protein, omega-3, nuts, legumes, docosahexaenoic acid (DHA), eicosapentaenoic acid (EPA), vitamin B12, vitamin C, vitamin D, vitamin E, and zinc. Vegetable intake is associated with greater levels of potassium, resulting in lowering chances of CKD.
- Physical exercise: Met analysis of 9 studies demonstrated the lowering of odds of CKD contraction with higher physical exercise when compared with those who were less physically active.
- Smoking: When compared with those who haven’t smoked, former and current smokers face an increased risk of incident CKD. Tobacco smoking leads to insulin resistance and, ultimately, CKD. Avoidance of smoke can prevent kidney disease as well as cardiovascular disease.
AKI vs CKD | Acute Kidney Failure vs Chronic Kidney Disease
While both AKI and CKD depict kidney diseases, the difference lies in the severity of the conditions. AKI, previously called as acute renal failure (ARF) or acute kidney failure and by 2021, KDIGO redefined it. (Kidney Disease: Improving Global Outcomes).
The sudden reduction in kidney function - acute kidney injury (AKI) is a reversible condition. Chronic Kidney Disease (CKD), on the other hand, is progressive in nature with irreversible deterioration of renal function due to slow destruction of renal parenchyma. The other differences include:
| Characteristics | Acute kidney injury (AKI) | Chronic kidney disease (CKD) |
|---|---|---|
| Onset | Sudden onset | Insidious onset |
| Reversibility | Reversible | Irreversible |
| Causes | Could be prerenal, renal and post-renal causes | Chronic nephropathies can eventually lead to CKD |
| Symptoms | Low or no urine volume, haematuria, thirst, dehydration, flank pain etc | Patients are usually asymptomatic till advanced stage |
CKD vs ESRD | Chronic Kidney Disease vs End-Stage Renal Disease
Both End-Stage Renal Disease (ESRD) and Chronic Kidney Disease (CKD) depict serious kidney diseases. Depending upon the estimated glomerular filtration rate (eGFR), CKD can be divided into five stages. ESRD is the last stage of CKD. The other differences include:
| Characteristics | Chronic kidney disease (CKD) | End-stage renal disease (ESRD) |
|---|---|---|
| Defined by | Glomerular filtration rate less than 60 mL/min/1.73m2 | Glomerular filtration rate less than 15 mL/min/1.73m2 |
| Progresses to | End-stage renal failure (ESRF) | Death |
| Symptoms | Usually, CKD patients are asymptomatic until they reach advanced stage | High BP, unresponsive to medication, anaemia, mineral and bone disorders, etc |
| Causes | Diabetes, metabolic disorders etc | Uncontrolled CKD |
Frequently Asked Questions (FAQs) on Chronic Kidney Disease (CKD)
Share on
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868