Pharyngeal cancer - Causes, Symptoms, Stages, Prognosis, Risk Factors
Pace Hospitals
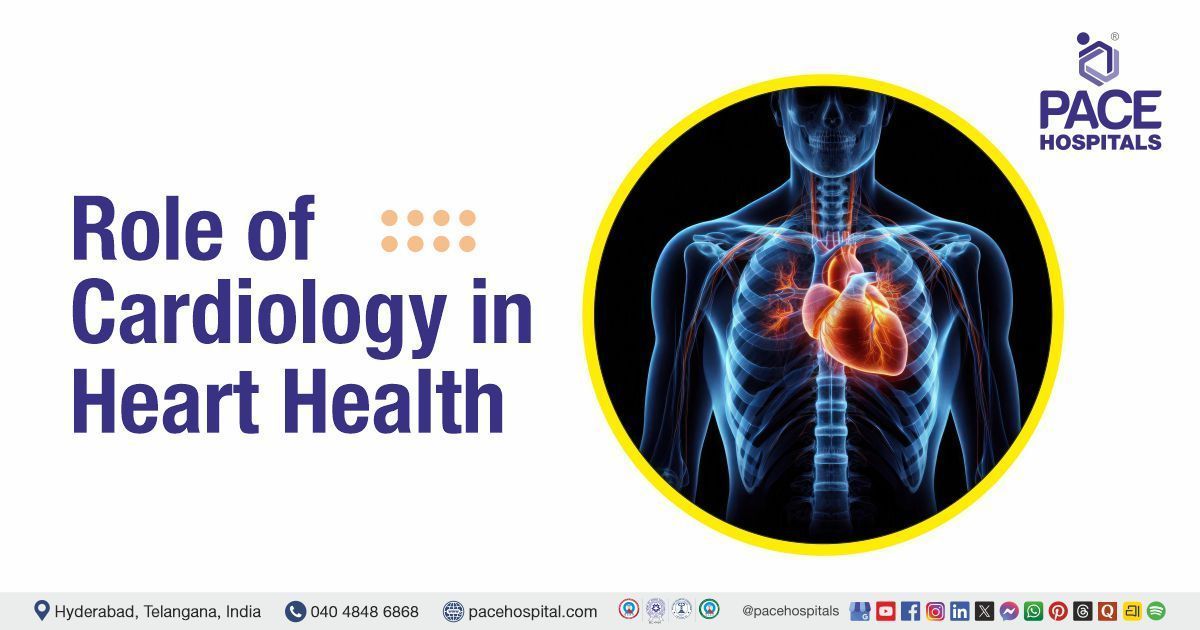
Pharyngeal cancer definition
When healthy cells multiply out of control, forming a tumour (a mass of cells) which could be cancerous or benign. If cancer begins in the pharyngeal areas, it is called pharyngeal cancer.
The oropharynx, oral cavity and other parts of the head and neck provide the ability to chew, swallow, breathe, and talk. The pharynx begins after the oral cavity. It includes the following:
- Tonsils
- The base of the tongue
- Soft palate
- Part of the throat behind the mouth

Types of pharyngeal cancers
The site of cancer origin distinguishes the basis of the types of pharyngeal cancer. The most common pharyngeal cancer sites are:
- The nasopharynx (the upper throat situated on the back of the nose).
- The oropharynx, which includes:
- The middle throat behind the mouth.
- The back part of the tongue (last 1/3rd of the tongue)
- The soft palate (the back of the roof of the mouth), including the uvula.
- The back and side walls of the throat.
- The tonsils.
- The hypopharynx (the lower bottom part of the throat).
Posterior pharyngeal wall cancers are one of the rare hypopharyngeal cancers, accounting for around 7%. Silent during the early stages, the posterior pharyngeal wall cancers majorly are presented in their advanced stage. Even though the cervical vertebral bodies are close to the Posterior pharyngeal wall cancers, direct invasion of the cervical vertebrae is rare.
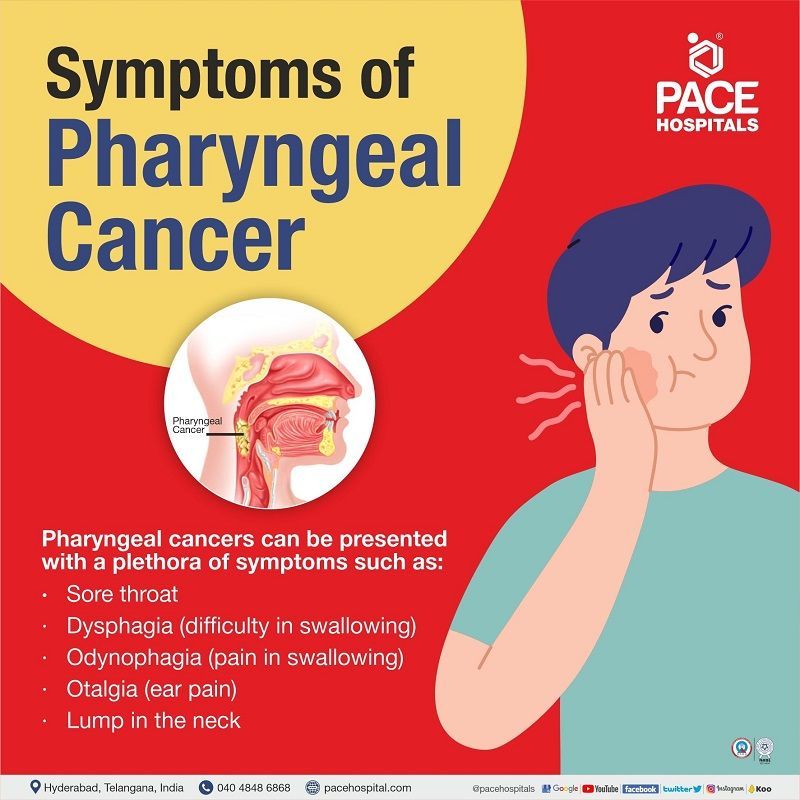
Pharyngeal cancer symptoms
Pharyngeal cancers can be presented with a plethora of symptoms which vary by the tumour’s location, such as high-pitched sounds during breathing or hoarseness in laryngopharyngeal cancer. Despite the location, a few of the most common symptoms include:
- Sore throat
- Dysphagia (difficulty in swallowing)
- Odynophagia (pain in swallowing)
- Dysarthria (slowed/slurred speech due to weakness in the muscles creating speech)
- Lump in the neck
- Otalgia (ear pain)
- Voice changes (hoarseness)
- Unexplained weight loss
- Hematemesis (blood vomiting)
- Ulcer in the oropharyngeal area
The symptoms could also present a red or white patch on the
- Base or posterior one-third of the tongue
- Posterior and lateral pharyngeal walls
- Soft palate
- Tonsils
Chronic pharyngitis cancer: Throat cancer can cause chronic painful throats in rare cases, which begins in the pharynx or larynx (voice box). Shortness of breath, lumps in the neck, or bleeding in your nose or mouth may occur as a result of the throat pain. Posterior pharyngeal wall cancer symptoms are also the same as the above explained.
Pharyngeal pouch cancer: The pharyngeal pouch cancer symptoms could range from weeks to years, presenting weight loss, regurgitation of undigested food, fetor ex ore (strong evil-smelling odour), borborygmi in the cervical region (borborygmus is the rumbling or gurgling noise due to fluid and gas movement in the intestines.), coughing.
Nevertheless, at times the patients remain asymptotic, and the discovery of pharyngeal cancer is not made until it reaches an advanced stage.
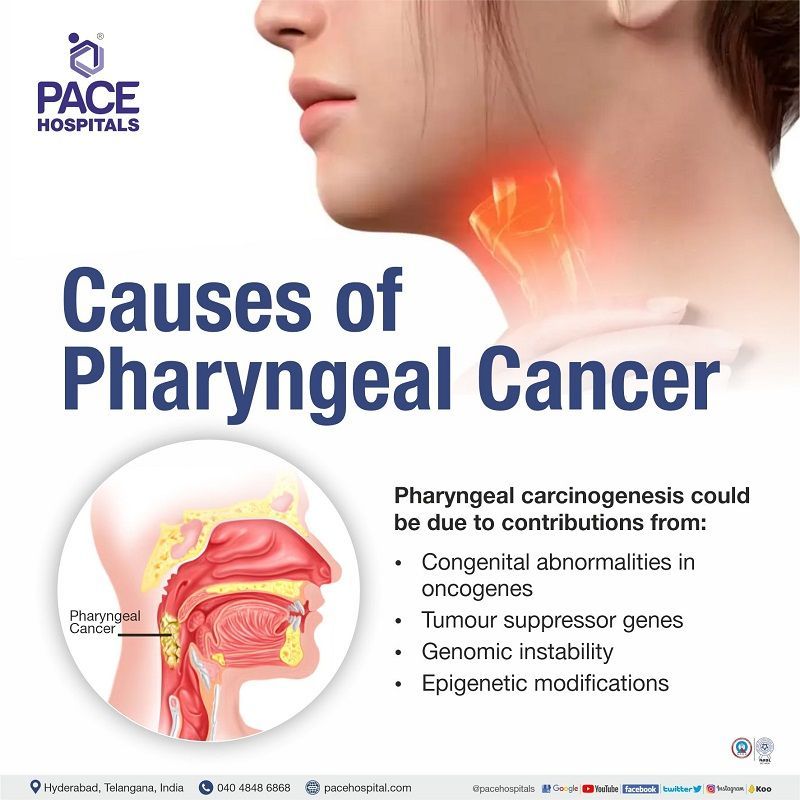
Pharyngeal cancer causes
Pharyngeal carcinogenesis, like other cancers, progresses from dysplasia to invasive phenotypes. Genetic and proteomic approaches have revealed molecular pathology such as congenital abnormalities in
- Oncogenes
- Tumour suppressor genes
- Genomic instability
- Epigenetic modifications.
Various risk factors could play a key role in enhancing the aforementioned genetic abnormalities.
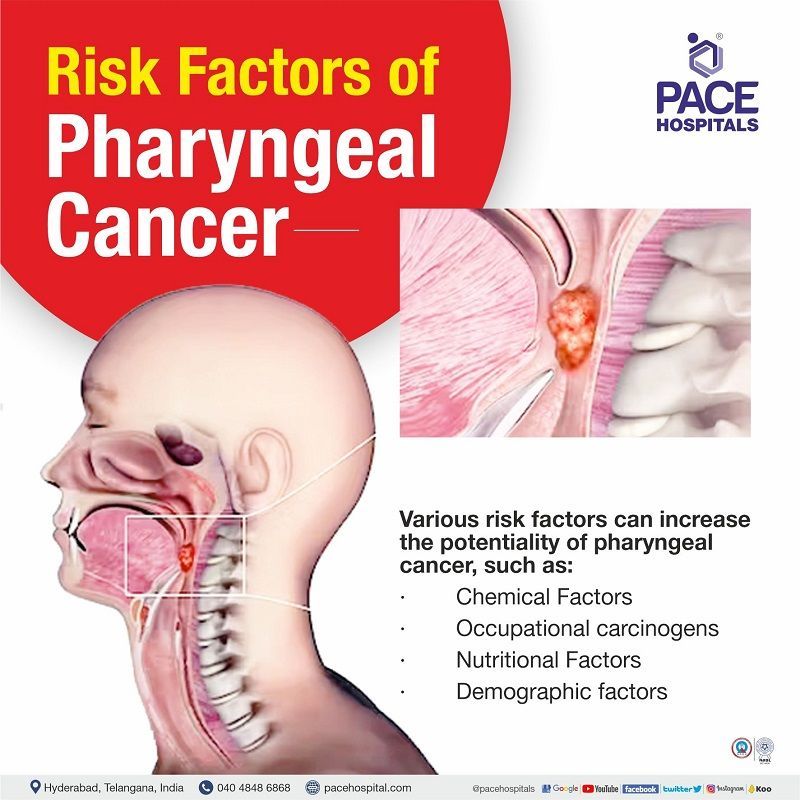
Pharyngeal cancer risk factors
Various risk factors can increase the potentiality of pharyngeal cancer, such as:
- Chemical Factors
- Occupational carcinogens
- Nutritional Factors
Chemical Factors
- Tobacco - There are ample amounts of evidence demonstrating that the consumption of tobacco in various forms, including (smoking, chewing, and in betel quid) could have a carcinogenic impact on the pharyngeal cavity, with smoking being the most standard form of tobacco use (cigarettes, cigars, pipe and bidi, hookah or chillum). In some parts of India (Mizoram and other northeast regions.), tobacco smoke is dissolved in water ("smoke on the water"), which is another peculiar form of tobacco use.
- Alcohol - Multiple studies have linked alcoholism to oral cancers and pharyngeal cancers, and it is exceptionally high in people indulging in alcoholism and tobacco use. Individuals consuming more than 170g of whiskey/day demonstrate ten times increased risk of oral cancer.
- Marijuana - studies showed the increased average risk for patients using marijuana.
Occupational carcinogens
- Formaldehyde - Hypopharyngeal and nasopharyngeal cancers can be increased with repeated exposure to formaldehyde.
- Asbestos –Studies demonstrated an increased risk for oral and pharyngeal cancers, including pharynx and hypopharynx.
- Wood particles - A reported a 5-fold and 4-fold risk for oral cavity and oropharyngeal cancer was seen among subjects exposed to wood particles.
- Metal particles-A 2006 study evaluated 20 occupational substances, including metal dust and demonstrated an increased associated risk with nasopharyngeal cancer.
- Coal particles- Association of occupational exposure to coal dust is seen with the development of hypopharyngeal cancer but not for other anatomical cancer sites.
- Smoke and fumes from different sources- An increased risk of oral and pharyngeal cancer is seen after >8 years of occupational exposure to welding fumes. Increased risk of nasopharyngeal cancer is seen with exposure to fumes from different sources (cooking, engines, wood, etc.), proportional to intensity.
Nutritional Factors
- Dietary deficits may potentially cause pharyngeal cancer. A reduced risk can be seen with a diet rich in fruits and vegetables.
Pharyngeal cancer diagnosis
While there are various diagnostic tests to identify confirm the ailment, not every individual necessarily needs to undergo every test. The oncologist and the healthcare team discuss within themselves before prescribing any of the tests outlined here.
- Endoscopy
- Laryngoscopy to examine the larynx,
- Pharynxgoscopy to investigate the pharynx,
- Nasopharyngoscopy to check the nasopharynx and other connecting cavities.
- Radiography: It is usually done to assess the bony invasion dental assessment.
- Ultrasonography: Ultrasonography is done during needle biopsy (both with or without needle biopsy)
- Magnetic Resonance Imaging (MRI): It gives perfect visualisation of the cancer
- Computed Tomography (CT): The size of the tumour can be estimated with a CT scan
- Positron Emission Tomography (PET): PET combined with a CT scan can detectthe recurrence of the primary tumours.
- Biopsy: A biopsy can collect a sample of the tissue for further examination.
Pharyngeal cancer treatment
The primary treatment options for oral or oropharyngeal cancer are surgery, radiation therapy, medication-based, and comprehensive dental treatment.
Surgery
- Maxillectomy hard palate (roof of the mouth) removal.
- Neck dissection (done to prevent the spread of cancer to neck lymph nodes)
- Laryngectomy (removal of the larynx - voice box)
- Transoral robotic surgery (TORS) and transoral laser microsurgery (TLM): both are minimally invasive surgeries
Radiation therapy
- High energy X-rays or other types of radiation are utilised to kill cancer cells and their growth.
Chemotherapy
- Medicines are given along with radiation therapy to kill growing cancer cells. Targeted therapy and immunotherapy are other kinds of therapy given to treat cancer.
Frequently Asked Questions - FAQs
Share on
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868