Sleeve Gastrectomy Surgery - Procedure & Cost
PACE Hospitals is recognized as the best hospital for sleeve gastrectomy in Hyderabad, India, offering advanced laparoscopic vertical sleeve gastrectomy for safe surgery and faster recovery. With expert bariatric surgeons and modern technology, we manage obesity and related conditions effectively. We also provide clear guidance on sleeve gastrectomy cost to support informed decision-making.
Book an Appointment for Sleeve Gastrectomy
Sleeve Gastrectomy Surgery Appointment
Why Choose PACE Hospitals for Sleeve Gastrectomy?
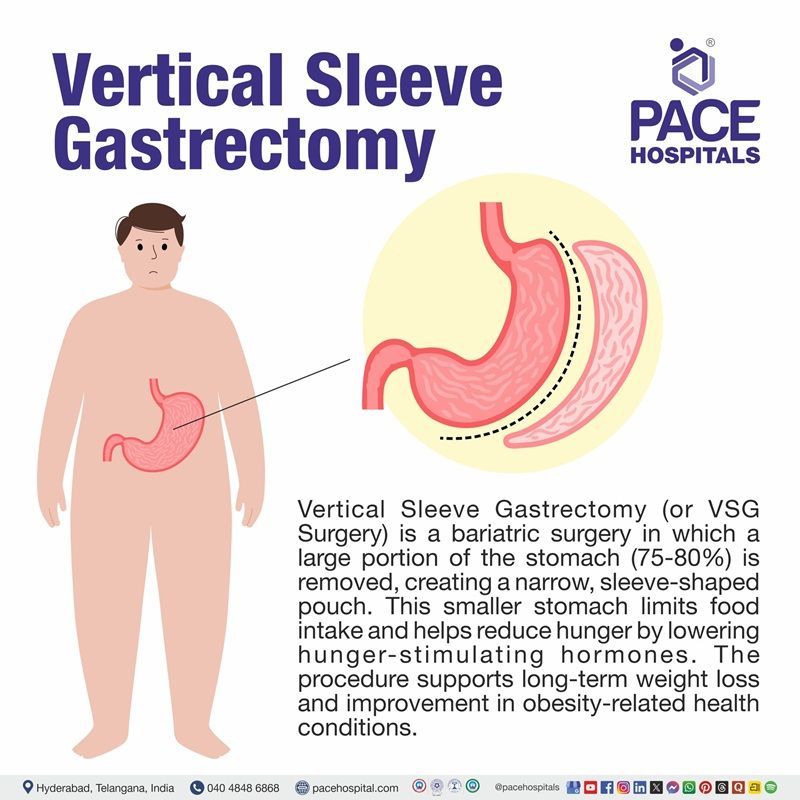
What is Sleeve Gastrectomy?
Sleeve gastrectomy (also called as vertical sleeve gastrectomy (VSG)) is a type of restrictive bariatric surgery performed on morbidly obese individuals to reduce the food intake to achieve the targeted weight loss. It could also be called “resective” or “reductive” surgery, as a large portion of the stomach is removed, facilitating gastric emptying.
The introduction of sleeve gastrectomy has resulted in a revolution with a significant decline in the number of gastric bypasses and the fall of the adjustable gastric banding being performed worldwide. Sleeve gastrectomy's low morbidity and technical simplicity resonate with patients and bariatric surgeons.
Doug Hess performed the first sleeve gastrectomy (open) in 1988 as part of the duodenal switch procedure (another type of bariatric surgery). Currently, sleeve gastrostomies are done laparoscopically.
Why is it called Sleeve Gastrectomy?
This surgical procedure produces weight loss by restricting food intake by removing at least 75% of the stomach. Once the surgery is over, the stomach takes the shape of a tube or "sleeve" holding much less food, hence the sleeve gastrectomy.
Sleeve Gastrectomy Indications
Gastric sleeve surgery is advised for obese people (with a body mass index (BMI) over 40) who have tried other weight loss methods but with no long-term success.
In few obese people, even with 35-40 BMI, this procedure is suggested but only if they have other pressing comorbidities such as:
- Sleep apnea
- High blood pressure
- Heart disease
- Type 2 diabetes
Sleeve Gastrectomy Contraindications
Some consider severe gastroesophageal reflux disease (GERD) a relative contraindication to sleeve gastrectomy, as reflux may worsen temporarily after surgery. GERD is a gastrointestinal disease characterized by the repeated flowing back of stomach acid into the oesophagus, which can irritate the oesophageal lining. The research found increased GERD symptoms from 12.1% preoperatively to 47% after one year post-operation.
The other contraindications for vertical sleeve gastrectomy procedures are as follows.
- Barrett’s oesophagus - damaged oesophagus (tube connecting mouth to the stomach) with thickened and reddened lining due to acid reflux.
- Hiatal hernias - The stomach is pushed up through the diaphragm muscle into the chest cavity via oesophageal hiatus (an opening where the oesophagus travels to the stomach)
- BMI > 60
Many surgeons (especially researchers) consider nicotine a contraindication for surgery. These surgeons recommend stopping smoking three months before the surgery to allow lung recovery and improved tissue perfusion. There are various bariatric programs and centres that include routine nicotine testing to ensure patients are free of nicotine before surgery to decrease complications.
Considerations of the Surgeon Before the Sleeve Gastrectomy Procedure
The surgeons undergo rigorous study and training, honed with years of experience, to pay keen attention even to minute details in the surgical technique of laparoscopic sleeve gastrectomy procedure as it is fundamental to avoid complications both in the short and long term.
The surgeons take special care in treating patients with pre-existing mental health conditions and their medication, as some medicines may be associated with increased appetite and thirst.
The other patients who need special support are:
- Pregnant and/or nursing women
- Women suffering from menorrhagia (iron deficiency anaemia)
- Patients on proton pump inhibitors
- Patients with B12 deficiency
- Patients who have had duodenal switch surgery
- Patients with co-existing malabsorptive conditions, such as coeliac disease, tropical sprue, inflammatory bowel disease
- Patients with renal impairment or with a single kidney, kidney stones
- Patients with high cardiovascular risk
Pre-operative Weight Loss and its Principle
Apart from other evaluatory pathways, pre-operative weight loss has been used as a screening tool for predicting success in surgical candidates. It is accepted that patients who weigh less have decreased risk with surgery and less weight-related comorbidity.
- Thinner patients generally require less rigorous pre-operative clearance than their heavier counterparts due to a lower burden of obesity-related disease.
- It is technically easier to operate on someone thinner due to improved exposure and accessibility.
- Pre-operative programs to decrease BMI would theoretically reduce perioperative and postoperative complications such as bleeding, wound infection, etc.
- In addition, shorter operative times and hospital stays could occur.
- In addition to the hypothetical risk improvement with pre-operative weight loss, many medical providers theorized that patients who demonstrate pre-operative weight loss are more severe and motivated about adhering to postoperative diet and exercise recommendations.
Steps for pre-operative weight loss
Most pre-operative weight loss programs include several meetings with nutritionists and physicians and psychiatric assessments and weigh-ins at these appointments.
In these and other meetings, the bond between the patient and healthcare providers strengthens, which is necessary for a low attrition rate during the postoperative phase.
If the patients cannot show adequate weight loss or miss appointments, they may be forced to start over or, in extreme cases, are even refused surgery.
Patient Selection Criteria
Overall, the surgeons opt for sleeve gastrectomy patients with the following traits. The counselling and education during the entirety of the pre-operative journey are designed to prepare the patients and cultivate the following traits in them.
- Well-informed, motivated individuals
- Acceptable operative risks
- Able and willing to comply with long-term follow-up
- Psychological stability
- Free from drug and alcohol abuse
- Demonstrated previous weight loss attempts
- A clear and realistic understanding of the lifestyle changes needs lifelong before and after surgery.
Sleeve Gastrectomy Procedure and Preparation
The preparation for surgery may start months before the actual procedure. A preoperational weight loss procedure plan is presented to the patients and is expected to stick with it. Apart from various other advantages, the preoperational weight loss procedure plan provides discipline to the patient, which helps restrict food after surgery.
The doctor explains to the patient that although laparoscopic sleeve gastrectomy procedure steps is an effective bariatric surgery, it may not work over the long term if the patient fails to change their habits and lifestyle.
Pre-operative evaluations
Pre-operative evaluations are necessarily done once the patient demonstrates substantial pre-operative weight loss. These evaluations include:
- Allergy evaluation
- Cardiac evaluation
- Nutritional evaluation
- Anaesthetic evaluation
- Sleep apnea evaluation
- Psychological evaluation
- Obesity Hypoventilation evaluation
- Upper gastrointestinal anatomy evaluation
- Pulmonary evaluation is usually for pulmonary embolism and venous thromboembolism
Informed consent
After undergoing all the aforementioned evaluations, the new information about the patient's overall candidacy for surgery is revalued, considering the result of pre-operative weight loss. This new information may change the benefit-risk equation discussed at the patient’s initial evaluation.
If the patient is deemed for bariatric surgery, the next question is about the type of surgery. Once laparoscopic sleeve gastrectomy surgery is confirmed, the patient is provided with all the information about the surgery required to make an informed decision.
The language associated with consent is in simple terms. The consent process, theoretically and ideally, should be a focused discussion reinforcing the personalized risks and benefits to the specific patient, which usually varies from case to case. The patient is provided with ample opportunities to ask any questions.
Ultimately, the patient and the caretakers should fully understand the therapy and the risks associated with the treatment.
Commencement of surgery is done only after the informed consent form is signed.
During the Sleeve Gastrectomy Surgery
Patients will be placed in supine, legs spread (French position), in a steep Fowler (reverse Trendelenburg) position. The table is slightly tilted right side down for adequate visualization of the gastroesophageal junction. This requires the patient to be secured to the table.
Anti-embolic stockings and intermittent compression devices may be provided to necessary patients to prevent venous thromboembolism.
Electrocautery /ultrasonic scalpel
- The procedure is performed laparoscopically, typically with five to six ports.
- The greater omentum is divided from, the greater curvature of the stomach using an electrocautery or ultrasonic scalpel.
- This is carried superiorly to the left diaphragmatic crus, freed from the stomach and oesophagus.
- If a hiatal hernia is present, the oesophagus is dissected circumferentially to ensure adequate intra-abdominal length.
- The hernia is repaired by closing the crura with nonabsorbable sutures.
Stapling up the stomach
- An endoscope, bougie, or other sizing device is then placed into the stomach from the mouth by the anaesthesiologist or an assistant.
- Sizing devices for sleeve gastrectomy range from 32 F (10.6 mm) or higher, depending on surgeon preference.
- A surgical stapler divides the stomach at a distance up to 6 cm from the pylorus, serially stapling up the gut and hugging the sizer with the stapler until the left crus is reached.
- The freed portion of the stomach is removed from the operative field and sent for pathologic analysis.
- The sleeve staple line can be reinforced using manufactured buttress material, additional sutures, or omentum.
- Most surgeons perform a leak test by clamping the distal end of the stomach and insufflating the lumen with air or methylene blue.
After the Vertical Sleeve Gastrectomy Procedure
- After having a laparoscopic vertical sleeve gastrectomy surgery, the patient needs to stay in the hospital for one or two days.
- The patients will be taken into a recovery room or post-anaesthesia unit once their vital signs (heart rate, respiration rate, and blood pressure) are stabilized.
- Appropriate hydration and pain and nausea control are initiated.
- During the in-hospital stay, patients are observed for signs of leak or bleeding, such as tachycardia (increased heart rate), tachypnoea (increased respiration), or fever.
- Anti-embolic stockings and intermittent sequential compression devices are removed as soon as the patient is ready to walk.
- The next day, an upper gastrointestinal contrast X-ray is done to identify any possible leaks.
- If the study is negative for leaks, a liquid diet is started, and patients are encouraged to ambulate.
- Respiratory therapy is initiated, and previous home medication is restarted.
- Patients are usually discharged home on the first or second postoperative day with liquid pain medications for a few days and a proton pump inhibitor for 6-8 weeks.
Vertical Sleeve Gastrectomy Recovery Time
At least 2-3 weeks is necessary for recovery after sleeve gastrectomy as the body takes its sweet time to heal that, too, with a very restricted diet during this time.
Follow-up for sleeve gastrectomy
Within the bariatric surgical service, there is usually an initial follow-up at six to eight weeks postoperatively, every three months for the first year, and then every six months in the second year as a minimum.
- Patients may have additional appointments with the dietician, which may be face-to-face or by telephone.
- Continuity of care with ongoing support following bariatric surgery is essential for the achievement of long-term weight loss and metabolic goals.
Questions that the patients can ask the healthcare team about sleeve gastrectomy?
- Can I have an online consultation for follow-up, or should I be present there?
- Now that I am eating less compared to earlier, won't I feel weak and tired?
- When can I start riding my bike or driving my car after surgery?
- How much time does it take to fully heal the surgical cuts?
- How many months will the follow-up is going to be? How many times should I come for a follow-up?
- How can I manage pain after surgery?
- When can I start exercising again?
- How do I care for my incisions?
- What should my diet plan be?
- When can I return to work?
Vertical Sleeve Gastrectomy Complications
The main postoperative vertical sleeve gastrectomy side effects are leak, bleeding, stricture, abscess, wound infection, splenic injury, trocar site hernia, and delayed gastric emptying. The complications are divided into early and late, depending on their onset.
Early complications
Leak: A constructed sleeve gastrectomy results in high intra-gastric pressure compared to a normal stomach. This high intra-gastric pressure is why sleeve gastrectomy has a higher leak rate, and sleeve leaks tend to be more prolonged than anastomotic techniques like gastric bypass.
Most leaks occur ''early'' during the first seven postoperative days and can be either confined or disseminated. These typically occur along the upper third of the staple line. Some leaks occur later or are initially undetected; therefore, the surgeons may prescribe a repeat upper gastrointestinal imaging (UGI) X-ray exam or computed tomography (CT) scan should be considered in cases of unexplained sepsis.
Haemorrhage: The long staple line is susceptible to haemorrhage (internal bleeding) and hematoma (swelling of clotted blood) formation. CT scans can help detect complications. Bleeding may also be seen at a trocar site or secondary to organ injury adjacent to the liver or spleen.
Stenosis: The gastric sleeve can develop stenosis (narrowing of the diameter of the stomach), usually occurring at the incisura angularis, related to oversewing. Stenosis is not ideal due to increased fundal pressure and gastroesophageal reflux. The surgeon may prescribe a UGI to identify stenosis.
Abscess: An abscess (a painful collection of pus, usually by an infection) is typically the result of a postoperative leak and is often located near the angle of His. Abscesses appear as fluid collections, often with rim enhancement, internal gas, and surrounding inflammatory change. Any collection outside of the staple line is highly concerning for abscess.
Wound complications: The surgeons may prescribe a CT scan to identify any wound complications. The CT scan could demonstrate the following:
- Fat stranding (accumulation of fat) and air in the subcutaneous tissues are expected postoperatively.
- Larger fluid collections/abscesses and trocar site hernias demonstrate wound complications.
Acute pancreatitis: Acute pancreatitis is another early complication that can arise following bariatric surgery. According to a study, the incidence of acute pancreatitis was 1.04% among all patients who underwent bariatric surgeries at their medical institution.
- The surgeon may prescribe CT for the diagnosis. Fluid replacement, optimization of electrolyte balance, antibiotics administration, and proper nutrition are essential points of initial management of acute pancreatitis.
Postoperative venous thromboembolism (VTE): A life-threatening complication causing premature death, the incidence of VTE post-bariatric surgery is 0.06-2.20%.
- A 2020 study showed that longer operational time, transfusions, and a history of deep vein thrombosis (DVT) increase the chances of DVT or pulmonary embolism (PE).
- In all individuals suspected of developing DVT or PE, the surgeon prescribes a D-dimer test, ultrasonography (for DVT), CT angiography (for PE) and anticoagulation therapy.
Late complications
Gastroesophageal reflux disease (GERD): The development or worsening of GERD has been linked to laparoscopic sleeve gastrectomy. According to a 2018 study, 47.06% of sleeve gastrectomy patients experienced new-onset heartburn (a frequent symptom of GERD), followed by dysphagia and regurgitation. GERD following sleeve gastrectomy could be due to increased intragastric pressure by
- lowered oesophageal sphincter tension,
- blunting of the angle of His,
- slowed gastric emptying, and
- decreased gastric volume and compliance.
Nutritional deficiency: A post-sleeve gastrectomy complication, a 2010 study showed the following nutritional deficiencies
- Zinc -34%
- Vitamin D3 - 32%
- Iron-18%
- vitamin B12-18% and
- Folic acid -18% deficiencies.
Gastric dilation: Gastric capacity can increase 2-3 years after sleeve gastrectomy and cause weight to regain. The surgeon may prescribe a follow-up UGI in these cases. Repeat sleeve gastrectomy is the treatment for patients who suffer from gastric dilation.
Overall, sleeve gastrectomy has been demonstrated to be a safe, reproducible, and effective operation on its own to treat morbid obesity with a rate of success that is at least as good as the Roux-en-Y gastric bypass.
Outcomes
Sleeve gastrectomy is the most frequent bariatric surgery done worldwide due to its effectiveness in treating obesity and related comorbidities. The weight loss and other outcomes of sleeve gastrectomy are given below:
- Weight loss: The excess weight loss percentage changes with the follow-up length. A 2012 study indicated that the average weight loss percentage was around 60% one year after surgery and 65% two years later. The 3rd year weight loss varied from 46-84.5%
- Type 2 Diabetes Mellitus (T2DM): T2DM is significantly improved after a sleeve gastrectomy. At year one, the complete remission rate is 78.3%, and at three years, the rate is 76.2%. The remission rate at five years varied from 60.8-71.4%.
- Hypertension: Improvements in hypertension are seen in both long and short terms. Hypertension is resolved in 87% and improved by 100% in the 1st year. Patients using more than two antihypertensive medications decreased from 49% to 22% in 12 months.
- Hyperlipidaemia: One year after sleeve gastrectomy, 45% and 86% of individuals achieved hypercholesterolemia remission and hypertriglyceridemia remission. 43.7% of patients even discontinued treatment.
- Obstructive sleep apnoea (OSA): Sleeve gastrectomy resolved sleep apnoea in 72% and improved in 51% of individuals after 24.7 months. Another study found that the apnoea hypopnea index dropped from 45.8 to 11.3 events/hour 10 months after surgery.
- Asthma: Asthma risk factors include obesity. Weight loss following surgery significantly reduces asthma symptoms. Improved small airway function, airway hyperresponsiveness, asthma management, and quality of life were all outcomes after the sleeve gastrectomy.
- Mental health: Depression has a significant association with obesity. A year after the surgery, patients demonstrated encouraging improvements in areas including depressed symptoms, self-esteem, eating behaviour, cognitive constraint and better eating habits.
- Quality of life (QoL): Obesity has a detrimental influence on the quality of life. Significant improvements in physical, psychological, and sexual quality of life have been observed following a sleeve gastrectomy. QoL and overall well-being increased dramatically in 1 to 2 years and have been sustained in the long term.
Sleeve Gastrectomy Cost in Hyderabad, India
The cost of Vertical Sleeve Gastrectomy (VSG) in Hyderabad generally ranges from ₹1,40,000 to ₹2,80,000 (approx. US $1,680 – US $3,360).
The exact cost varies depending on BMI, associated metabolic conditions (diabetes, sleep apnea, PCOS, fatty liver), preoperative tests, anesthesia, surgeon expertise, hospital stay, and postoperative requirements — including cashless insurance, TPA corporate tie-ups, and medical insurance documentation support wherever applicable.
Cost Breakdown According to Type of Vertical Sleeve Gastrectomy
- Bariatric Surgeon Consultation – ₹800 – ₹2,500 (US $10 – US $30)
- Preoperative Evaluation (CBC, LFT, RFT, Thyroid, ECG, Echo, CXR) – ₹3,500 – ₹7,500 (US $42 – US $90)
- Upper GI Endoscopy (If Advised) – ₹2,000 – ₹4,500 (US $24 – US $54)
- Anesthesia Assessment – ₹1,000 – ₹2,500 (US $12 – US $30)
- Vertical Sleeve Gastrectomy Surgery Costs
- Standard Laparoscopic VSG – ₹1,40,000 – ₹2,50,000 (US $1,680 – US $3,000)
- High-BMI / Complex VSG – ₹1,80,000 – ₹2,80,000 (US $2,160 – US $3,360)
- Additional Cost Components
- Hospital Stay (2–3 days) – ₹15,000 – ₹40,000 (US $180 – US $480)
- Postoperative Medications & Supplements – ₹4,000 – ₹10,000 (US $48 – US $120)
- Dietitian & Lifestyle Counseling – ₹1,500 – ₹4,000 (US $18 – US $48)
- Follow-up Blood Tests (Vitamin Levels & Metabolic Panel) – ₹1,500 – ₹5,000 (US $18 – US $60)
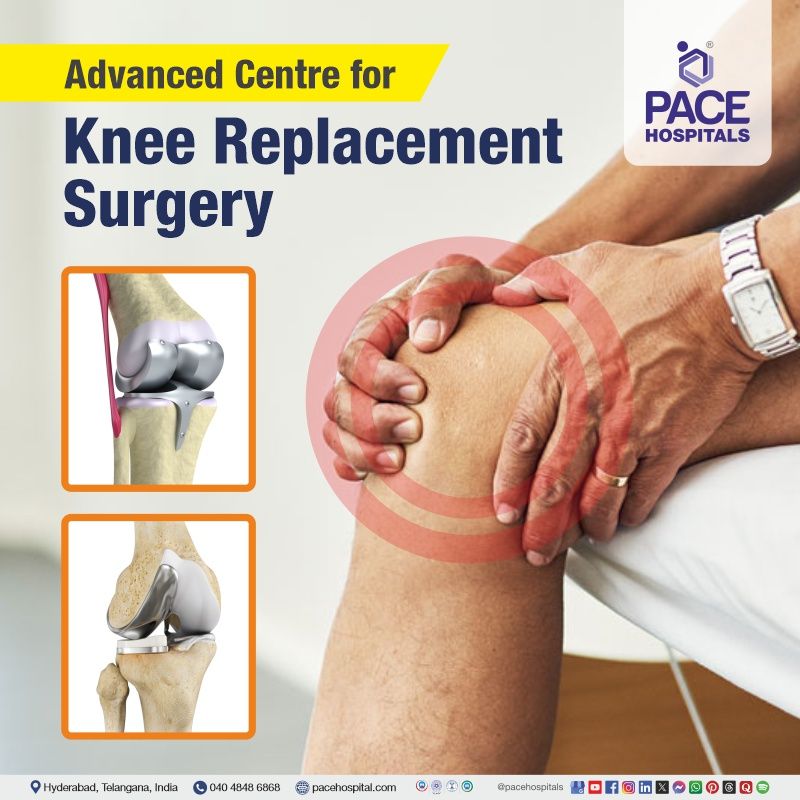
Frequently Asked Questions (FAQs) on Knee Replacement Surgery
What is the success rate of vertical sleeve gastrectomy?
The success rate of the vertical sleeve gastrectomy procedure, could range from 80% to 90%. This remarkable success rate is one of the primary factors that contributes to its widespread acceptance. People who have this weight reduction surgery often lose between 60% and 70% of their extra weight during the first year after the surgery.
Which Is the best hospital for Sleeve Gastrectomy in Hyderabad, India?
PACE Hospitals, Hyderabad, is one of the most trusted centers for Vertical Sleeve Gastrectomy and advanced bariatric surgery.
Our team manages:
- Severe obesity
- Type 2 diabetes
- PCOS-related weight gain
- Fatty liver (NAFLD/MASLD)
- Sleep apnea
- High cholesterol and hypertension
- Obesity-related joint problems
- Failed weight-loss attempts
We are offering laparoscopic sleeve gastrectomy option to our patients and guided by experienced bariatric surgeons, ICU support, structured nutrition plans, and long-term lifestyle guidance, PACE Hospitals ensures safe, effective, and patient-focused bariatric care — supported by cashless insurance, TPA tie-ups, and complete documentation assistance.
Is vertical sleeve gastrectomy safe?
Yes, vertical sleeve gastrectomy is safe. A 2022 study demonstrated that laparoscopic sleeve gastrectomy is one of the safe and effective ways to lose weight in mildly obese individuals. Compared with the high body mass index (BMI) group, patients with low BMI had significantly lower rates of obesity associated medical problems (OAMP), after the procedures.
Can a patient enjoy food again after gastric sleeve surgery?
Absolutely. The gastric sleeve surgery is a type of bariatric procedure which is performed on the patient’s stomach. The procedure ensures that none of the taste buds are harmed or damaged. In fact, it doesn’t have to do anything with tongue. So, the patient can heartly enjoy food again after gastric sleeve.
On the other had apart from weight loss and with proper food discipline, the rates of depression also fade which helps the patient to enjoy his/her life to the fullest.
Can sleeve gastrectomy cure diabetes?
Sleeve gastrectomy can pave a better pathway for improvement in type 2 diabetes, and many patients experience remission after surgery. The smaller stomach helps to reduce food intake, but the metabolic benefits go beyond restriction. By removing the upper portion of the stomach it helps to lowers ghrelin and influences other associated hormones involved in blood sugar regulation. Insulin sensitivity often improves within weeks, even before major weight loss occurs. While some individuals maintain long-term remission, others may see diabetes return if weight increases or if the disease was long-standing before surgery. The procedure is effective, but it is not considered a guaranteed cure for everyone.
How much does Vertical Sleeve Gastrectomy cost in PACE Hospitals, Hyderabad?
At PACE Hospitals, Hyderabad, the cost of Vertical Sleeve Gastrectomy typically ranges from ₹1,35,000 to ₹2,60,000 and above (approx. US $1,620 – US $3,120), making it a competitive and specialized option for weight-loss surgery. However, the final cost depends on:
- Patient’s BMI and overall health
- Requirement for endoscopy or advanced imaging
- Duration of hospital stay
- Presence of diabetes, PCOS, hypertension, or sleep apnea
- Postoperative supplements and follow-up needs
- Nutritional counseling and long-term monitoring
Patients undergoing uncomplicated laparoscopic sleeve gastrectomy are at the lower range, while complex or cases with major comorbidities may fall toward the higher range.
After evaluation, nutritional screening, and diagnostic tests, our bariatric team provides a personalized treatment plan and a clear cost estimate based on individual.
What happens first week after gastric sleeve?
During the first week, after the gastric sleeve surgery, the patient can feel nauseous and even vomiting. It is the body being adjusted to the new change in the gut. Maintaining the fluid intake by drinking water in short, frequent sips is one way to reduce the severity of these adverse effects. It is advised that one consume between 1.5 and 2 litres of water on a daily basis.
Is vertical sleeve the same as gastric sleeve?
Yes. Vertical sleeve is same as gastric sleeve.
Vertical sleeve is a short term for vertical sleeve gastrectomy, often known as the sleeve gastrectomy or gastric sleeve surgery. In this procedure, the size of the stomach is surgically reduced to limit the amount of food the patients eat. The minimally invasive operation (laparoscopic) involves removing a section of the stomach, resulting in the reduction of stomach the size and shape of a banana.
This ensures faster satiety even with smaller amounts of food.
Will gastric sleeve change a persons’ life?
Yes. Gastric sleeve surgery or for any bariatric surgery for that matter, provides the patient the means to be happy and healthy. With one single surgery, weight loss and other obesity associated medical problems are mightily improved giving the patient a second chance at living healthy + With proper food discipline and lifestyle management, gastric sleeve can surely change your life. The following are improved with gastric sleeve surgery:
- Asthma
- Hypertension
- Mental health
- Hyperlipidaemia
- Male sex hormones
- Quality of life (QoL)
- Excesses weight loss (EWL)
- Polycystic ovarian syndrome
- Obstructive sleep apnea (OSA)
- Type 2 Diabetes Mellitus (T2DM)
- Non-alcoholic fatty liver disease (NAFLD)
Does everyone gain weight after gastric sleeve?
Well, not everyone may gain weight after gastric sleeve although it is not an unusual sight. Gastric sleeve surgery provides a means to promote weight loss through restriction in food intake. Despite this procedure, if the patients inculcate little to no change in their eating habits, then they may experience weight gain even after surgery.
It is usually for this very specific reason; the patient is put on a preoperative weight loss programme so that the binge eating and or other chaotic eating behaviours are curbed.
Why does gastric sleeve fail?
Yes. Gastric sleeve surgeries do fail but only in 10-20% of the cases. Similar to various other bariatric surgery procedures, sleeve gastrectomy failure is also likely to be multifactorial and related to a combination of technical, physiological, and psychological parameters, such as gradual sleeve dilation, hormonal adaptation, and relapse of inappropriate eating behaviours etc.
There is a dearth of research literature on the long-term outcomes of vertical sleeve gastrectomy.
Does a patient feel less hungry after gastric sleeve?
Yes. The patients who underwent gastric sleeve are less hungry than before surgery. In sleeve gastrectomy, the roughly bean shaped stomach is excised and stapled to the form a vertical tube (more like a banana). This ensures faster filling of stomach with food achieving satiety soon.
A 2015 study demonstrated that the profound changes in gastrointestinal anatomy and physiology brought by sleeve gastrectomy procedure is the key factor in contributing hunger reduction by faster satiation. Accelerated gastric emptying is one among the various physiological changes through which weight loss and glucose metabolism is improved after surgery.
When can a person start exercising after gastric sleeve?
It is generally recommended that patients to wait at least 2 - 4 weeks before starting any exercise after gastric sleeve surgery.
It's important to listen to the body and not push individual too hard too soon. The surgeon will be able to give the patients specific instructions based on their individual recovery. It's important to start with light walking and gradually increase the intensity and duration of the exercise routine. It's also important to stay hydrated and pay attention to any signs of pain or discomfort.
How much of the stomach is removed in sleeve gastrectomy?
The final size of the stomach sleeve depends on bougie size used during surgery, which surgeons adjust based on patient anatomy.
A 2021 article explains that after sleeve gastrectomy, “70–80% of the outer stomach is removed,” leaving a “narrow gastric tube.
In this procedure, a large portion of the stomach is removed, remaining section forms a narrow, tube-shaped stomach or “sleeve.” This smaller stomach reduces the amount of food that can be eaten at one time and lowers hunger by decreasing the production of appetite-stimulating hormones such as ghrelin. The normal digestive pathway is maintained, but the reduced stomach size helps achieve significant and sustained weight loss when combined with dietary and lifestyle changes.
What is the difference between gastric bypass and sleeve gastrectomy?
The two surgical procedures help with weight loss although in different ways and approach. Sleeve gastrectomy is performed by removing the curved outer portion of the stomach, leaving a narrow tube that holds less food and reduces appetite. While, gastric bypass creates a small pouch at the top of the stomach and connects it directly to a lower segment of the small intestine. This not only limits how much food can be eaten but also reduces calorie absorption. Because of this intestinal rerouting, gastric bypass has a stronger effect on blood sugar control, while sleeve gastrectomy is simpler and avoids altering the intestinal pathway.
Does sleeve gastrectomy cause iron deficiency?
Iron deficiency can occur after sleeve gastrectomy, although it is less common than after gastric bypass. The procedure does not reroute the intestine, but it decreases stomach size and removes the portion that produces acid needed for optimal iron absorption. Lower acid levels can make it harder to absorb iron from food, especially from plant sources. Reduced food intake after surgery may also contribute to lower iron intake. Some individuals develop iron deficiency months or years after the procedure, which is why routine blood tests and appropriate supplementation are often recommended to maintain healthy levels.
Why choose PACE Hospitals?
- A Multi-Super Speciality Hospital.
- NABH, NABL, NBE & NABH - Nursing Excellence accreditation.
- State-of-the-art Liver and Kidney transplant centre.
- Empanelled with all TPAs for smooth cashless benefits.
- Centralized HIMS (Hospital Information System).
- Computerized health records available via website.
- Minimum waiting time for Inpatient and Outpatient.
- Round-the-clock guidance from highly qualified super specialist doctors, surgeons and physicians.
- Standardization of ethical medical care.
- 24X7 Outpatient & Inpatient Pharmacy Services.
- State-of-the-art operation theaters.
- Intensive Care Units (Surgical and Medical) with ISO-9001 accreditation.