Polycystic kidney disease - Symptoms, Causes, Types, Treatment
Pace Hospitals
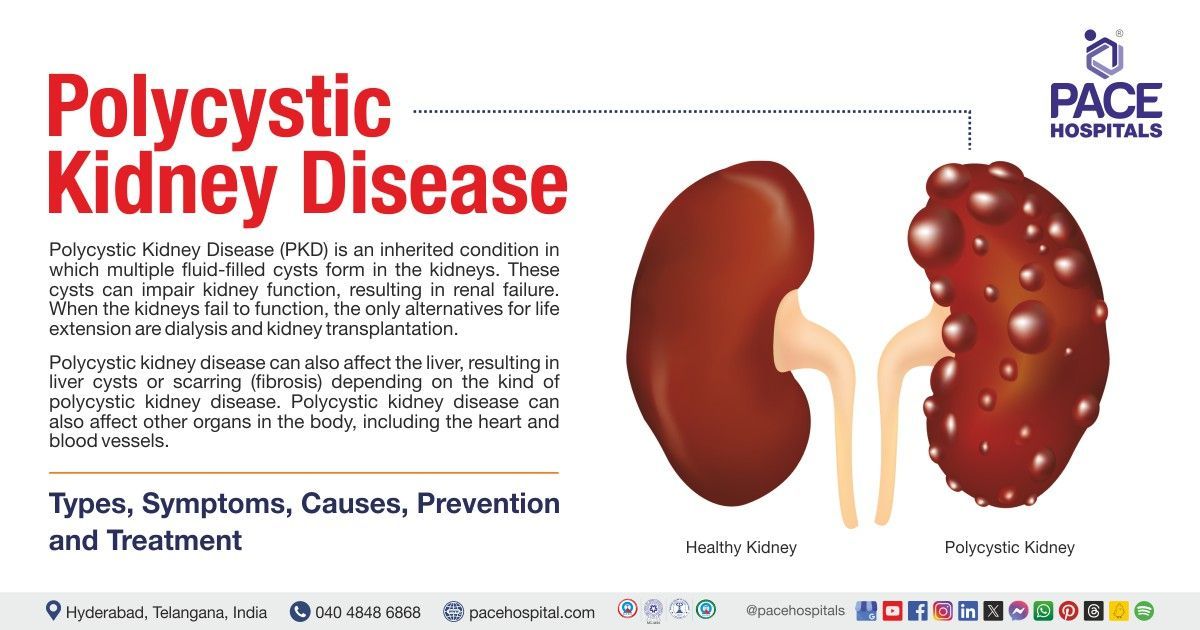
Polycystic kidney disease (PKD) is a potentially lethal hereditary condition that is characterized by the development of fluid-filled cysts, in the kidneys.
The initial symptom of polycystic kidney disease in people may be elevated blood pressure. This can happen even before kidney cysts are apparent. Flank pain on the sides of the lower back could be one of the additional early signs. The cysts that are formed in the kidneys may have the potential to increase its size and cause subsequent scarring. A genetic mutation, typically inherited from one's parents, is the cause of this illness.
Although this disease commonly manifests in young adults, polycystic kidney disease typically advances gradually and varies throughout individuals. If treatment is not received, it could alter the normal kidney function and eventually lead to kidney failure. In addition, polycystic kidney disease may result in additional complications like hypertension, hepatic cysts, and issues with the blood arteries in the brain and heart.
It is said that approximately 50% of PKD patients will eventually experience renal failure and require kidney dialysis or a transplant. However, it may take years, sometimes decades, for kidney damage to worsen to that extent in some people.
Polycystic kidney disease definition
Polycystic kidney disease (PKD) is defined as a genetic condition that is marked by the development of many fluid-filled kidney cysts, which can cause kidney enlargement and decreased kidney function. Kidney failure may occur by progressive PKD that may need dialysis or kidney transplantation as a form of treatment.
Polycystic kidney disease meaning
Despite the fact that polycystic kidney disease has always existed in humans, it was first identified in the eighteenth century. Following the illness of Stephen Bathory, the king of Poland, the most thorough observations on PKD have been written.
After going on a hunting trip, he experienced tiredness, chest pain, and unconsciousness where he passed away in 9 days, at the age of 53, in 1586. During the mummification process, surgeon Mr Jan Zigulitz distinguished the presence of cysts in his kidney resembles the size of kidneys in a bull, possessing an uneven and bumpy surface.
347 years later, a panel of doctors and historians in Krakow concluded that PKD and uremia were most likely the cause of King's death based on the information that was available.
Regretfully, doctors were not interested in PKD until the 18th century. Matthew Baillie referred to these kidney vesicular cysts as "false hydatids of kidney" in the late 18th century after observing that they differed from hydatid cysts (a slowly forming, fluid-filled sac with the potential to grow quite enormous).
The phrase "polycystic kidney" was first used by Mr Flix Lejars in 1888, and he emphasized that these cysts were bilateral and produced symptoms that could be identified clinically. By the end of the 1800s, the disease's core clinical manifestations and genetic foundation were more clearly understood.
Polycystic kidney disease types
There are two primary types of polycystic kidney disease they are:
- Autosomal recessive polycystic kidney disease (ARPKD), which may be diagnosed during pregnancy or soon after birth.
- Autosomal dominant polycystic kidney disease (ADPKD), which is typically diagnosed in adulthood.
Prevalence of polycystic kidney disease
Prevalence of Autosomal recessive polycystic kidney disease (ARPKD)
Autosomal recessive polycystic kidney disease is one of the most frequent causes of heritable infantile cystic renal disease. Despite this, just 1 in 20,000 to 40,000 live newborns have it. This indicates a carrier frequency of roughly 1 in 70 in non-isolated populations.
Prevalence of Autosomal dominant polycystic kidney disease (ADPKD)
The prevalence rate of diagnosed cases of ADPKD, a disorder that affects people of all ethnic backgrounds globally, ranges from 1:400 to 1:1,000.
Since up to 75% of affected patients acquire end-stage kidney disease by the time they turn 70 years old, accounting for up to 10% of all ESKD patients, ADPKD is not regarded as a benign ailment.
Prevalence of polycystic kidney disease in India
The frequency of autosomal dominant experiences polycystic kidney disease equally, which affects roughly 1 in 1,000 people. It also affects men and women equally. Polycystic kidney disease affects about 5% of all patients with chronic kidney disease who need dialysis or a kidney transplant.
Polycystic kidney disease symptoms
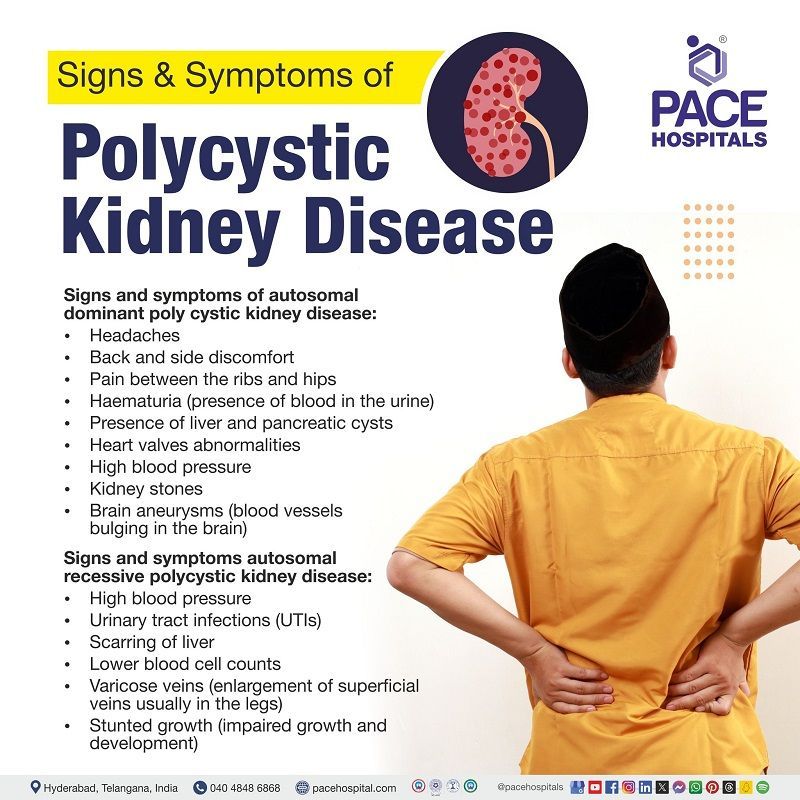
Signs and symptoms of autosomal dominant polycystic kidney disease
Autosomal dominant poly cystic kidney disease frequently doesn't show any symptoms or indications until cysts are half an inch or bigger.
This condition may show signs and symptoms such as:
- Headaches
- Back and side discomfort
- Pain between the ribs and hips
- Hematuria (presence of blood in the urine)
- Presence of liver and pancreatic cysts
- Heart valves abnormalities
- High blood pressure
- Kidney stones
- Brain aneurysms (blood vessels bulging in the brain)
The discomfort may be minor or severe, transient or persistent.
Signs and symptoms autosomal recessive polycystic kidney disease
Autosomal recessive polycystic kidney disease’s symptoms frequently arise in the first few months of childhood and while in the womb. Early symptoms of autosomal recessive polycystic kidney disease in pregnancy can have major health consequences. As a result, a woman who is at risk of spreading polycystic kidney disease to her children should seek prenatal care as soon as she becomes pregnant.
Signs and symptoms of autosomal recessive polycystic kidney disease may include:
- High blood pressure
- Urinary tract infections (UTIs)
- Scarring of liver
- Lower blood cell counts
- Varicose veins (enlargement of superficial veins, usually in the legs)
- Stunted growth (impaired growth and development)
Polycystic kidney disease causes
Causes of autosomal recessive polycystic kidney disease
The phenotypic manifestation of autosomal recessive polycystic kidney disease varies significantly. About 90% of ARPKD cases occur due to the mutation of PKHD1 gene on chromosome 6p12.
The regular function of tubular epithelium is dependent on the critical quantity of full-length protein released by this gene.
DAZ-interacting zinc finger protein 1-like (DZIP1L) has been connected to a few cases of ARPKD more recently, however it is extremely rare.
TSC1 and TSC2 mutations are seen in patients with tuberous sclerosis. Like PKD1, these genes are located on chromosome 16. Patients with tuberous sclerosis frequently present similarly to ARPKD and have an early onset of PKD.
Causes of autosomal dominant polycystic kidney disease
Two genes have been identified that are involved in mutations that cause ADPKD. Fifteen percent of ADPKD instances are caused by mutations in PKD2 gene on chromosome 4q21, while eighty-five percent are caused by mutations in PKD1 gene on chromosome 16p13.3.
In people with more variable polycystic liver disease, it is demonstrated that 1% people may diagnose with ADPKD due to mutations in GANAB gene.
Similar symptoms are expressed by mutations in the PKD1 and PKD2 genes. About half of people with PKD1 require renal replacement therapy by the time they are 60 years old. PKD2 mutations are more common in older people and are associated with a milder form of the disease than PKD1 mutations, with fewer renal cysts, late-onset hypertension, and less end-stage kidney disease (ESKD).
Polycystic kidney disease risk factors
- Family history: Polycystic kidney disease is a familial disease. It is a genetic condition that is inherited and is transferred from parents to offspring. The building blocks of heredity are genes. Each parent contributes a set of genes to the child at conception.
- Gender: The development of autosomal-dominant polycystic kidney disease (ADPKD) may be influenced by a person's gender. End-stage renal disease (ESRD) and renal function loss are more common in males with ADPKD than in women.
- Long-term dialysis:
It is asserted that a type of polycystic kidney disease called acquired cystic kidney disease (ACKD) has been linked to long-term dialysis (PKD)
Polycystic kidney disease complications
Complications associated with autosomal recessive polycystic kidney disease may include:
- Azotemia (presence of high creatinine and waste products in the blood)
- Cholangitis (inflammation in the bile duct system)
- Congenital hepatic fibrosis (a rare genetic condition that impacts the kidneys and liver prior to birth)
- Gastrointestinal bleeding
- Hypertension (high blood pressure)
- Increased risk for ascending cholangitis
- Large bilateral flank masses
- Liver failure and cirrhosis
- Poor absorption of fat-soluble vitamins
- Poor growth, feeding, and nutrition
- Progressive portal hypertension (increased blood pressure in the portal vein)
- Progressive kidney failure
- Renal osteopathy (a chronic renal disease consequence that affects bones)
- Respiratory distress brought on by pulmonary hypoplasia and constricted diaphragmatic movement as a result of the kidneys' immense enlargement
- Splenomegaly (enlargement of spleen) may present in about 60% of patients
- Thrombocytopenia (low platelet count)
Complications that arise due to autosomal dominant polycystic kidney disease may include:
The most typical ADPKD complication is end-stage kidney disease, which necessitates dialysis or renal transplantation.
The most hazardous extra renal consequence of ADPKD is a ruptured cerebral aneurysm, which is four times more common in ADPKD patients than in the normal population.
Another recognized negative consequence of ADPKD is hepatic cysts, which are more common as people age. The frequency rises with age, with a 10%–20% prevalence up to the age of 30 and up to 50%–70% in people over 60.
Other complications that are frequently linked to ADPKD include:
- Abdominal wall or inguinal hernias
- Nephrolithiasis (kidney stones)
- Diverticular disease (medical condition that affects large intestine)
Polycystic kidney disease prevention
There is currently no known method for polycystic kidney disease prevention. On the other hand, kidney damage and other polycystic kidney disease issues brought on by high blood pressure might be slowed down by managing blood pressure at 120/80mmhg.
However, some preventive strategies are available to help manage symptoms, prevent or delay kidney function loss in patients with polycystic kidney disease, and help decrease the growth of cysts. They consist of:
- A healthy way of living that includes smoking cessation, exercising, controlling weight, and consuming less salt
- Consuming a large amount of plain water all day long
- Limiting the amount of caffeine in all drinks
- Consuming a lot of liquids as soon as blood in the urine is noticed
- Cautious blood pressure monitoring
Polycystic kidney disease diagnosis
Diagnosis of Autosomal dominant polycystic kidney disease
The most common methods used to detect autosomal dominant polycystic kidney disease include kidney ultrasonography, CT scans, and MRIs. As people become older, the cysts get bigger and more numerous. Therefore, the presence of even two kidney cysts in a 30-year-old patient with a family history of the condition is very suggestive. Once symptoms appear, a genetic test to identify mutations is typically conclusive but not always required.
Diagnosis of Autosomal recessive polycystic kidney disease
Since this is a condition that can be detected during pregnancy in mother’s womb, an ultrasound of the developing foetus may reveal enlarged kidneys. Since the condition leaves the liver scarred, liver imaging is also advised.
Polycystic kidney disease treatment
As the mutations causing polycystic kidney disease can no longer be corrected, this disease has no known treatment. The goals of treatment are to relieve symptoms and counter the complications. Medications may be used to treat urinary tract infections and to regulate hypertension. It is possible to enhance growth with growth hormone. When renal failure sets in, dialysis and transplantation become necessary. Pain may be managed using non-steroidal anti-inflammatory drugs (NSAIDS).
Difference between medullary cystic kidney disease (MCKD) and polycystic kidney disease (PKD)
Since urethral strictures and benign prostatic hyperplasia symptoms resembles closely, it is important to understand the basic differences between these two conditions:
| Aspect | Medullary cystic kidney disease | Polycystic kidney disease |
|---|---|---|
| Age of onset | Usually, adult onset | Variable, but typically manifests in adulthood |
| Cyst formation | Tubular dilation in the medullary region | Clusters of noncancerous cysts throughout kidneys |
| Genetic Inheritance | Not typically inherited | Inherited (autosomal dominant or recessive) |
| Symptoms | Dull back or side pain - Fever - Upper stomach pain | - High blood pressure - Back or side pain - Blood in urine - Abdominal fullness |
| Complications | Less severe | Can cause kidney enlargement and loss of kidney function |
| Prevalence | Less common | One of the most frequent genetic diseases. |
Frequently Asked Questions (FAQs) on Polycystic kidney disease
What is polycystic kidney disease life expectancy?
The life expectancy of persons with polycystic kidney disease (PKD) varies greatly, ranging from 53 to 70 years, depending on the disease subtype.
Can someone live a normal life with polycystic kidney disease?
Yes. This condition allows individuals to live a normal, active life. Kidney failure usually does not create any symptoms until it is advanced. Dialysis and transplantation should allow someone to continue working and doing most of the activities they wish to do.
What are the stages of polycystic kidney disease?
ADPKD is staged in the same way as chronic kidney disease (CKD), using the estimated glomerular filtration rate (GFR), as follows:
- Stage 1: Glomerular filtration rate (GFR): 90 mL/min
- Stage 2: Glomerular filtration rate (GFR): 60-90 mL/min
- Stage 3: Glomerular filtration rate (GFR): 30-60 mL/min
- Stage 4: Glomerular filtration rate (GFR): 15–29 mL/min
- Stage 5: Glomerular filtration rate (GFR): <15 mL/min
Can women with polycystic kidney disease have kids?
Yes, women with polycystic kidney disease (PKD) can have healthy kids as long as their kidney function and blood pressure are normal.
How much water should a PKD patient drink?
It is important to consume enough of water. People with polycystic kidney should consume at least 3 litters of water every day to lower their risk of kidney stones. Furthermore, consuming plenty of water may help to limit cyst formation.
What is bilateral polycystic kidney disease?
Bilateral polycystic kidney disease (BPKD) is a hereditary condition characterized by the formation of numerous cysts in both kidneys, resulting in organ enlargement and ultimately function loss.
What is polycystic kidney disease pathophysiology?
Mutations in polycystin 1 and polycystin 2 proteins can affect the function of renal cilia, which allow tubular cells to perceive flow rates. A prominent concept suggests that flow rate influences tubular cell proliferation and differentiation, and thus ciliary failure may result in cyst transformation.
Can polycystic kidneys be removed?
Polycystic kidneys should not be removed routinely prior to transplantation since nephrectomy (kidney removal) in ADPKD patients is associated with considerable morbidity and death.
What age does polycystic kidney start?
Polycystic kidney disease (PKD) symptoms typically appear between the ages of 30 and 40, but this can begin, even in childhood in case of an autosomal recessive poly cystic kidney disease. The condition is inherited as a dominant trait, thus children born to parents who carry the gene have a 50/50 chance of getting it.
Do polycystic kidney disease cause pain?
Yes, polycystic kidney disease (PKD) can induce pain, which occurs in around 60% of people with autosomal dominant PKD (ADPKD). The discomfort can be dull and continuous, or it can be temporary. It frequently arises in the side or back and can be felt as pressure on other organs or stretching of the cyst wall.
What causes death in polycystic kidney disease patients?
If polycystic kidney disease affects the brain, it might result in an aneurysm. An aneurysm is a bulging blood vessel that can rupture, causing a stroke or possibly death. If polycystic kidney disease affects the heart, the valves may become floppy, causing heart murmurs in some people.
Can polycystic kidneys burst?
Yes, there had been cases reported that the cysts in polycystic kidney disease (PKD) can burst, however this is uncommon, particularly in the presence of trauma. Rupture of an infected cyst might result in an abscess, sepsis, or death.
Share on
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868