Liver transplantation breathes new life in patient with decompensated liver failure and CKD | Case study
Pace Hospitals
PACE Hospitals' Liver transplant team successfully performed a living donor liver transplantation (LDLT) for a 49-year-old male with decompensated liver cirrhosis and pneumonia.
Chief Complaints
A 49-year-old male patient with a
BMI of 30 and a medical history of ascites, chronic kidney disease, and pneumonia, presented to
PACE Hospitals, Hitech City, Hyderabad for further management.
Medical History
Delving deeper, it was understood that the patient was a known case of decompensated chronic liver disease, ascites with hepatorenal syndrome and chronic kidney disease.
Diagnosis
Upon being admitted to PACE Hospitals and undergoing necessary investigations (blood tests, liver function tests and imaging tests such as liver Doppler), to evaluate the patient’s profile, he was found to be diagnosed with:
Decompensated chronic liver failure with chronic kidney disease and pneumonia with diabetes mellitus. The Model for End-Stage Liver Disease (MELD) Na score is 28.
To confirm any diagnostic discrepancy in view with pneumonia, the patient was also subjected to a COVID-19 test (SARC 2 COVID-19 RTPCR test) which turned out to be negative.
His anaemic profile can be traced to chronic inflammation of the liver, which may cause normocytic normochromic anaemia. Also, due to hepatorenal syndrome, there is a reduction of erythropoietin (an enzyme necessary for the bone marrow to produce red blood cells) causing anaemia.
A person with advanced liver disease may develop a serious illness known as hepatorenal syndrome (HRS), which is caused by damaged kidneys. Patients with this illness typically exhibit decreased urination as they develop oliguria (low urine output), along with liver failure signs and symptoms.
A condition known as ascites causes fluid to build up in abdominal spaces. Ascites may be painful if it is severe. Liver cirrhosis is the most common cause of ascites.
Following the results, he was advised to undergo Decompensated
Chronic
Liver Failure Treatment in Hyderabad, India, under the expert care of the Liver Transplant Department for specialized management and intervention.
Treatment
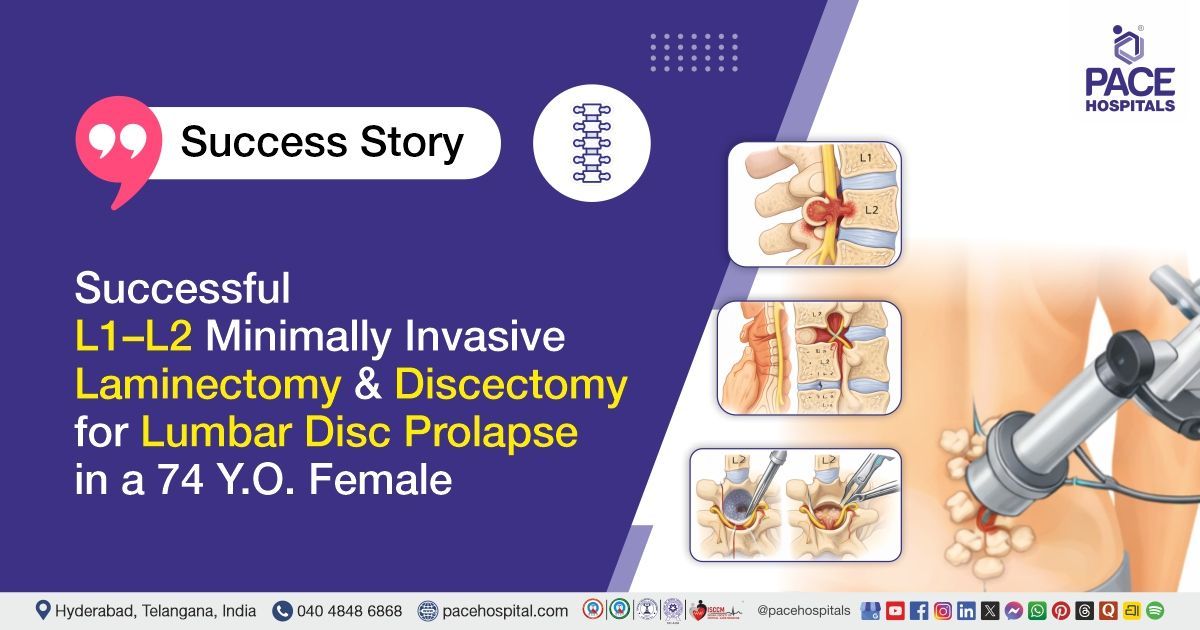
As the patient’s blood urea and protein excretion in urine are elevated due to chronic kidney disease (CKD), consultation with nephrologist, Dr. A Kishore Kumar’s opinion is considered and obtained clearance to perform transplantation surgery. Upon considering the patient’s disease condition, and opinion from the liver transplantation team, Dr. CH. Madhusudhan, Dr. Suresh Kumar S, asserted that a liver transplant was the only way to salvage the patient.
Following the confirmed diagnosis, the patient was scheduled for a Living Donor Liver Transplant in Hyderabad at PACE Hospitals, under the expert supervision of Liver transplant surgeon Dr. CH Madhusudhan.
Promptly, the patient was put on multiple lifesaving supports, efforts were made to obtain a liver from donors. The son of the patient came forward to donate his liver to save the patient.
With necessary investigations done & clearances obtained, the patient underwent living donor liver transplantation (LDLT), receiving the right lobe modified liver graft. The procedure was supervised by the liver transplant surgeon Dr. CH Madhusudhan, and it was accomplished devoid of any complications.
Aftermath
Concerning the hepatic profile and the transplanted graft, the post-operative period was uneventful. Although bilateral pleural effusion was developed during the post-operative period, it is a complication which was anticipated in patients with MELD scores > 20. Nevertheless, through an intercostal drainage (ICD) tube, the pleural effusion was drained, thus neutralising the complication. His abdominal drain output demonstrated a decreasing trend.
The necessary medicines, immunosuppressives, antibiotics, proton pump inhibitors, multivitamins, antiemetics, analgesics, antipyretics & other supportive care were given to treat the conditions of transplant, especially any rejection.
Regular tests were done to understand the overall health of the patient. It was revealed that the patient depicted a worsening renal function, due to which renal-sparing immunosuppressants were given to address the issue.
In the initial days after the surgery, it was revealed that the patient demonstrated an increase in the liver enzymes, depicting a degradation in liver function. To counter the same, a pulse dose of steroids was given which resolved the issues with liver enzymes and the doses of immunosuppressants were adjusted regularly as evidenced by the liver function reports.
The pulse corticosteroid therapy involves the administration of corticosteroids in "suprapharmacological" doses through the intravenous route. The pharmacological effects of a single pulse dose could extend for at least two days.
The patient and his attendees were counselled regularly regarding the prognosis of the transplantation and the graft, along with the risks that may come with it. Once the patient achieved hemodynamic stabilisation, he was discharged with the necessary medications, advised to schedule a follow-up appointment with the Liver Transplant Surgeons in Hyderabad at PACE Hospitals to assess his post-operative condition and ensure continued recovery.
The
liver transplant doctor/specialist concurred that it would be beneficial to regularly monitor the patient's liver function tests, including serum bilirubin, ALT, AST, and INR levels, on an outpatient basis. Additionally, regular assessment of the patient's renal function, including creatinine levels and glomerular filtration rate (GFR), is essential due to his underlying chronic kidney disease. If there is any significant deterioration in liver or kidney function, further investigations such as a liver biopsy or renal biopsy may be required to assess graft function and identify any complications.
Conclusion
This case highlights the successful application of Living Donor Liver Transplantation in managing decompensated liver cirrhosis in a patient with underlying chronic kidney disease, demonstrating the advanced capabilities of PACE Hospitals in providing comprehensive care for complex hepatological conditions.
Pleural Effusion: An Unforeseen Consequence of Liver Transplantation
Pleural effusion is an accumulation of fluid between the layers of tissue lining the chest cavity and lungs. It is the most common postoperative pulmonary complication after liver transplantation (LT).
Bilateral pleural effusion is a commonly reported incident among the cases of post procedural liver transplant patients (mostly described as between 35-70%) most likely seen in the patients with higher MELD scores which are much sicker. Nevertheless, it must be understood that not every pleural effusion case needs a chest drain. It is only seen in 22 to 52% of procedural liver transplant patients. However, the advantages of the procedure have to be compared with the potential risks of placing a chest drain. The others can be treated with improved oxygenation and pneumonia prophylaxis.
According to current guidelines, non-urgent chest drain insertion can be avoided if the international normalization ratio (INR) is >1.5, even though the majority of recent studies in general populations do not advise improving coagulation before pleural drainage placement. When interventions are necessary, individuals who are more likely to bleed are also often given costly fresh frozen plasma and platelet concentrates in hospitals.
Share on
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868