Best COPD Treatment in Hyderabad, India
PACE Hospitals, is renowned for its excellence in Chronic Obstructive Pulmonary Disease treatment in Hyderabad, India; delivering compassionate care and optimal outcomes. Our expert team of pulmonologists, respiratory therapists and healthcare professionals are dedicated to diagnosing and managing COPD effectively with advanced medical technology, we tailor personalized treatment plans for patients of all ages, focusing on improving quality of life and slowing disease progression.
Request an Appointment for COPD Treatment
COPD Treatment - appointment
Why choose us

8200+ Patients treated with COPD
Team of the Best Pulmonologist in Hyderabad
Precision Treatment with 99.9% success rate
All insurance accepted with No-cost EMI option
PACE Hospitals is recognized as one of the best hospitals for COPD treatment in Hyderabad, India; the hospital's pulmonology department is staffed with highly skilled and experienced pulmonologists, respiratory therapists who specialize in the diagnosis and management of COPD and other respiratory conditions. We offer a comprehensive range of diagnostic and therapeutic services for COPD, including spirometry, chest X-rays, CT scans, bronchoscopy, and pulmonary function tests. The hospital's state-of-the-art facilities and advanced medical technology enable accurate diagnosis and effective treatment of COPD, ensuring the best possible outcomes for patients.
Our treatment approach for COPD is multidisciplinary, involving a team of healthcare professionals, including pulmonologists, respiratory therapists, physiotherapists, and nutritionists. This collaborative approach ensures that patients receive personalized and comprehensive care that addresses their specific needs and medical history. We also offer various non-pharmacological therapies for COPD, such as pulmonary rehabilitation, smoking cessation programs, and oxygen therapy. These therapies are designed to improve lung function, reduce symptoms, and enhance the overall quality of life for patients with Chronic Obstructive Pulmonary Disease. Patients can feel confident in the hospital's ability to provide them with the highest level of care and support throughout their treatment journey.
With 24/7 emergency care, personalized disease management plans, and patient education on lifestyle modifications, PACE Hospitals is one of the top-rated COPD hospital in Hyderabad, combining clinical expertise with compassionate care.
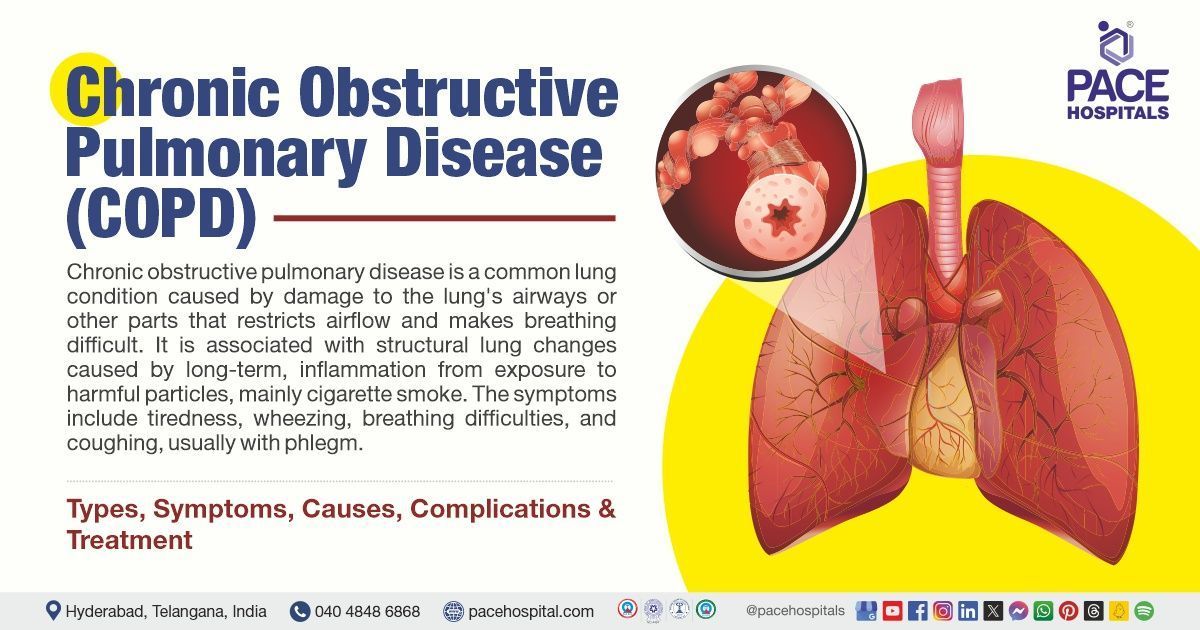
Patients who are present with any of the hallmark symptoms, such as dyspnoea, increased sputum production and cough, and particularly those who have a history of smoking are clinically suspected of having chronic obstructive pulmonary disease (COPD). The World Health Organization (WHO) and the National Heart, Lung, and Blood Institute (NHLBI) initiated the Global Initiative for Chronic Obstructive Lung Disease (GOLD) program. The program's ability to provide complete and up-to-date reports on COPD diagnosis and treatment guidelines are widely recognized.
COPD diagnosis
Diagnosis of COPD may depend on various factors such as medical history, family history, and physical examination, which help the pulmonologist to conclude the diagnosis because a complete medical history and complete examination are necessary when a new patient has COPD, whether confirmed or suspected. The pulmonologist takes into consideration the following steps before selecting the appropriate tests for the diagnosis of COPD:
- Patient’s medical history
- COPD family history
- Physical examination of the COPD patient
Patient’s medical history
- For individuals with suspected chronic obstructive pulmonary disease (COPD), a complete medical history of tobacco smoking is an essential part of the clinical history.
- Pack years, calculated by multiplying the daily pack count by the total number of years smoked, which is the most accurate way to measure cigarette smoking.
- A complete occupational history is essential when occupational exposure is considered as a possibility. This includes a list of professions, a description of work-related tasks, used personal protective equipment (PPE), especially breathing equipments, and the duration and intensity of exposures.
- Material safety data sheets at work sites can help determine the relative hazards of occupational lung disease
COPD family history
- Family history is also significant in the process of screening (checking) for chronic obstructive pulmonary disease (COPD).
- A chromosome 14 genetic abnormality called alpha1-antitrypsin deficiency causes early liver and lung diseases. Alpha1-antitrypsin deficiency causes more significant tissue damage from neutrophil elastase, which leads to early-onset COPD in patients.
Physical examination of COPD patient
- Many patients have normal examination results, indicating that physical examination results are not sensitive to the early diagnosis of COPD.
- Lung hyperinflation is characterized by an enlarged anteroposterior chest width, hyper resonance on percussion, and reduced breath sounds in patients with abnormal findings.
- Chronic lung injury can raise the pressure on the right side of the heart, which can result in cor pulmonale (right-sided heart failure).
- Upon physical examination, hepatomegaly, peripheral edema, jugular venous distension, and an increased second heart sound are the indications of cor pulmonale.
✅COPD diagnostic tests
Based on the above information, a pulmonologist advises the single or combination of the following diagnostic tests to detect COPD:
- COPD blood tests
- Complete blood count
- Alpha-1 antitrypsin test
- Electrocardiogram
- Echocardiogram
- Lung function tests
- Spirometry
- Peak expiratory flow (PEF) test
- Fractional exhaled nitric oxide (FeNO) test
- Arterial blood gas test
- Lung imaging tests
- Chest X-ray
- Chest computed tomography (CT) scan
- A calculation of the patient’s body mass index (BMI)
- Pulse oximetry
- Sputum analysis
- A 6-minute walk test
COPD blood tests
- Complete blood count: It can identify other health conditions, such as anaemia (low iron) or erythrocytosis (high red blood cell concentration), that may cause symptoms similar to those of COPD.
- Alpha-1 antitrypsin test: A blood test may also be performed to determine whether patients have an alpha-1 antitrypsin deficiency. This rare genetic condition raises the risk of COPD.
Electrocardiogram
- An electrocardiogram or ECG records the electrical activity of the heart.
- Electrocardiography needs to be performed to assess pulmonary circulation pressures in individuals presenting with cor pulmonale symptoms.
Echocardiogram
An ultrasound scan of the heart is known as an echocardiogram, which is performed to assess pulmonary circulation pressures in individuals presenting cor pulmonale symptoms.
Lung function tests
- Pulmonary function tests also known as lung function tests, are crucial for the diagnosis, staging, and treatment of COPD.
- Spirometry: A type of lung function test called spirometry which measures how much air patients exhale and how fast they exhale, and is the primary test for COPD.
- Peak expiratory flow (PEF) test: This test determines how quickly one can expel air while exerting the maximum effort. This test can be performed using a tiny handheld instrument or during spirometry.
- Fractional exhaled nitric oxide (FeNO) test: The amount of nitric oxide in one's breath is determined by fractional exhaled nitric oxide (FeNO) testing. Breathing difficulties may be caused by inflammation of the lungs' airways, which is indicated by high nitric oxide levels.
- Arterial blood gas test: An arterial blood gas test measures the amount of oxygen and carbon dioxide levels in the patient's blood.
Lung imaging tests
- Chest X-ray: It is a painless and fast imaging test that examines the structures in and around the chest. The test can identify other conditions that may interact with COPD, but it is not effective in diagnosing COPD.
- Chest computed tomography (CT) scan: A computed tomography (CT) scan of the chest is a non-invasive imaging procedure that produces several detailed images, or slices of the lungs and the interior of the chest. Computers can combine these images to create three-dimensional (3D) models that depict the size, shape, and placement of the lungs and other chest structures. The cause of lung related symptoms, such as chest discomfort or shortness of breath, may be determined with the use of a chest CT scan.
A calculation of the patient's body mass index (BMI)
- Chronic weight loss is associated with COPD and is an independent predictor of mortality. Therefore, measuring and monitoring BMI in all COPD patients is essential.
Pulse oximetry
- To assess for hypoxemia (low oxygen levels) and the need for supplemental oxygen, pulse oximetry needs to be done at rest, during exercise, and while at sleep.
Sputum analysis
- A sample of phlegm (mucus) may be tested to look for signs of a chest infection.
A 6-minute walk test
- A 6-minute walk test is frequently used to evaluate a patient's submaximal functional ability. This test is conducted on an even straight surface indoors. Typically, the corridor is 100 feet long, and the test measures how far the patient walks in six minutes.
✅Considerations of a pulmonologist for treating COPD
While treating patients with chronic obstructive pulmonary disease (COPD), the pulmonologists may consider the following criteria for better outcome of the patients:
- To minimize the number of inhalations and the environmental impact of using multiple inhalers, combination inhalers may be considered. Patients who experience worsening symptoms after changing inhalers need to be changed to the alternatives provided.
- Patients with a persistent cough that produces sputum need to be considered for mucolytic drug therapy; treatment is appropriate only if symptoms improve (e.g., coughing frequency and sputum production decrease).
- Only patients with confirmed hypoxemia (SaO2 <92%, PaO2 <7.3 kPa) are candidates for oxygen therapy.
- Long-term inhaled corticosteroids (ICS) medication for COPD patients may only be considered in combination with long-acting beta2-agonists (LABAs) if the patient has a history of exacerbations despite receiving appropriate long-acting bronchodilator treatment.
- When a patient has stable COPD but is still unable to exercise despite receiving effective pharmacologic treatment, or if they are a symptomatic patient with a projected FEV1 of less than 50%, the doctor may consider pulmonary rehabilitation (PR).
- Patients who have unstable angina, are unable to move, or recently had a myocardial infarction (MI) are not considered for pulmonary rehabilitation (PR).
- When treating COPD patients who produce a significant amount of sputum daily, have frequent (usually four or more) sputum-producing exacerbations, long-term exacerbations, or undergo hospitalization-causing exacerbations, physicians may consider prophylactic antibiotic use.
✅Goals for COPD patients
The main goals of therapy for chronic obstructive pulmonary disease (COPD) include:
- Reducing symptoms
- Lowering the frequency and intensity of exacerbations
- Enhancing exercise tolerance and general health
- Delaying the course of the illness
- Lowering mortality
COPD Treatment
Although there is no known cure for chronic obstructive pulmonary disease (COPD), medication can help manage the symptoms and decrease the disease's progression. However, the chance of complications and flare-ups decreases with the earlier initiation of treatment. Below are the available treatment options for COPD:
- Nonpharmacological management of COPD
- Pharmacological management of COPD
- Surgical management of COPD
Non-pharmacological management of COPD
- Cessation of smoking: The most effective way to stop COPD from getting worse is to quit smoking. Giving up smoking may help prevent additional harm to the lungs and airways, even though many of the already existing damage cannot be reversed.
- Diet: In individuals with COPD, the inadequate nutritional status associated with low body weight is linked to decreased diaphragmatic mass, reduced exercise capacity, and increased mortality rates. For COPD patients, nutritional support is essential for complete treatment.
- Pulmonary rehabilitation: Pulmonary rehabilitation is recommended at all stages of COPD. It is a thorough approach customized for each patient and may include therapies such as behavioral modifications, education, and exercise training. The goal is to enhance the psychological and physical well-being of the patient. Group sessions are typically held twice a week for a minimum of six weeks in pulmonary rehabilitation programs. Numerous healthcare professionals, such as physiotherapists, nurse specialists, and dietitians, conduct these classes.
- Physical activity: Engaging in physical activity may improve overall health and strengthen the muscles that support breathing.
- Air quality: Since poor air quality can significantly affect COPD symptoms and the likelihood of exacerbations, it is recommended that patients stay indoors during low air quality.
- Immunization: People who have COPD are more vulnerable to pneumococcal and influenza-related problems. Although there is currently little evidence, the polysaccharide pneumococcal vaccine may protect COPD patients from morbidity in rare cases. Encouraging persons with COPD to have the yearly influenza vaccination and pneumococcal polysaccharide vaccine which lowers hospital admission rates as well as the chance of influenza and pneumonia-related deaths.
Pharmacological management of COPD
COPD treatment medications include bronchodilators (beta2-agonists, antimuscarinics, methylxanthines), inhaled corticosteroids (ICS), glucocorticoids, phosphodiesterase-4 (PDE4) inhibitors, and antibiotics, expectorants, and oxygen therapy.
- Bronchodilators: This medication is used to open the airways. It is administered with a puffer. Smooth muscle in the airways undergoes relaxation by beta2-agonists. Short-acting beta-agonists (SABAs) and long-acting beta2-agonists (LABA) are frequently used in the treatment. By inhibiting the smooth muscle's M3 muscarinic receptors, antimuscarinics prevent bronchoconstriction. Methylxanthines cause mild bronchodilation by relaxing the smooth muscle in the airways.
- In mild and asymptomatic COPD: The pulmonologist may recommend a short-acting bronchodilator that patients take only when they experience symptoms if their COPD is moderate and don't have symptoms frequently. Bronchodilators work by relaxing the muscles adjacent to the airways to facilitate easier breathing. Short-acting bronchodilators last about four to six hours.
- Moderate or severe COPD: Long-acting bronchodilators last for at least 12 hours and may be necessary if a person's COPD is moderate or severe.
- Severe COPD: In cases of severe COPD or frequent flare-ups of symptoms, pulmonologists may prescribe a combination of bronchodilators and inhaled steroids which assist in lowering the swelling or inflammation in the airways that interferes with breathing.
- Inhaled corticosteroids (ICS): To reduce inflammation, inhaled corticosteroids are frequently used with long-acting beta2-agonists (LABAs) and long-acting antimuscarinic agents (LAMAs). It has been demonstrated that ICS and LABA together are more advantageous than either medication used separately. Patients and doctors need to be aware that the use of ICS increases the risk of pneumonia.
- Glucocorticoids: Long-term usage of glucocorticoids is not recommended due to their numerous side effects. Instead, these are appropriate to be saved for the treatment of acute exacerbations.
- Phosphodiesterase-4 (PDE4) inhibitors: Phosphodiesterase-4 inhibitors reduce inflammation by inhibiting intracellular cyclic AMP from breakdown.
- Antibiotics: If a bacterial infection is suspected in the patients, antibiotics need to be taken into consideration.
- Expectorants: These medications may help the patients cough up more easily by loosening mucus.
- Oxygen therapy: If individuals have low blood oxygen levels and severe COPD. They can breathe more comfortably with oxygen therapy. Patients may require more oxygen more often or only sometimes. Patients with COPD who are significantly hypoxic (low oxygen levels) at rest benefit from increased survival and improved quality of life if supplemental oxygen treatment is used for at least 15 hours per day. For patients with stable COPD and mild or absent hypoxemia at rest, oxygen lacks any significant benefits, nevertheless. Patients should not be provided oxygen if they smoke continuously because of the risk of possibly fatal upper airway and facial burns.
Surgical management of COPD
When medical therapy alone fails to control symptoms in severe situations, surgical intervention is needed and may even enhance the quality of life. Surgical intervention that includes lung volume reduction surgery, lung transplantation, or bullectomy may be necessary in such cases.
- Bullectomy: A surgery performed to remove an air pocket from one lung that improves lung function providing more comfortable breathing.
- Lung volume reduction surgery: A surgery to remove a severely damaged lung section to improve the function of the healthy lung tissue and improve breathing.
- Lung transplantation: It is the process of extracting a diseased lung and replacing it with a donor's healthy lung.
✅COPD prognosis
- The prognosis for COPD varies according to adherence to therapy, which includes giving up smoking and avoiding other harmful gases. The prognosis is usually worse for patients with other comorbidities (pulmonary hypertension, cardiovascular disease, lung cancer, etc.). Dyspnoea and breathing restriction typically worsen over time.0000
- An approach for determining the risk of mortality in COPD patients is the BODE (Body-mass index (BMI), airflow obstruction, dyspnea, and exercise capacity) index.
Frequently Asked Questions (FAQs) on COPD Treatment
Can COPD be cured?
While there is no known cure for COPD, symptoms may improve if a person stops smoking, protects themselves from air pollution, and receives vaccinations to fight against illnesses. Medication, oxygen, and pulmonary rehabilitation are further treatment options.
Is COPD cancer?
Cigarette smoking causes both lung cancer and COPD, and there is increasing evidence that the two illnesses have more in common besides a common etiology. COPD is an independent risk factor for lung carcinoma, mainly for squamous cell carcinoma.
Can second hand smoke cause COPD?
During childhood and adolescence, smoking and exposure to second hand smoke (inhaled accidentally) may inhibit the growth and development of the lungs. This may raise the chance that an adult may develop chronic obstructive pulmonary disease (COPD).
Is COPD reversible?
It is not possible to reverse chronic obstructive pulmonary disease (COPD), although it can be controlled and treated to lessen symptoms and decrease the disease's progression. Moreover, damaged lung tissue does not heal on its own.
What is the emergency treatment for COPD?
Immediate intubation and oxygenation is the appropriate way of action. There is no concern about oxygen supplementation causing clinical deterioration; instead, giving the patient enough oxygen to maintain a near-normal saturation (above 90%). Intubation is probably necessary regardless of the patient's health if it is dangerous.
What are some symptoms of COPD?
Shortness of breath, a long term cough with phlegm that does not go away, fatigue (feeling of tiredness), repeated chest infections, chest heaviness or tightness, and persistent wheezing or whistling are common symptoms of COPD.
Can COPD symptoms come and go?
Yes, symptoms of chronic obstructive pulmonary disease (COPD) may come and go and can change in intensity throughout the day, week, and year. Symptoms may become unexpectedly severe during a flare-up, also known as an exacerbation, which may last for a few days or even weeks.
What causes COPD?
The most common cause of chronic obstructive pulmonary disease (COPD) is cigarette smoking. The lungs and airways are damaged by prolonged smoking or by breathing in tobacco smoke or airborne pollutants. In some cases, genetics may also cause COPD.
What is the difference between asthma and COPD?
Both conditions cause a cough, but people with asthma frequently experience a dry cough that is worse at night and is commonly associated with allergens. On the other hand, years of smoking are usually the cause of COPD.
What is bullae in COPD?
Large, air-filled spaces called bullae are found in lung tissue and are frequently linked to chronic obstructive pulmonary disease (COPD). Although bullae are often bigger than blebs, there is no particular limit to their size.
What is salt therapy for COPD?
One well-known alternative treatment option for respiratory chronic disorders is salt therapy or halotherapy, which is used to prevent infections in the lungs. According to some research, halotherapy sessions are particularly beneficial for individuals suffering from COPD. With the advancement of technology, treating this condition with tiny inhalers filled with salt is now possible.
Is COPD painful?
With chronic obstructive pulmonary disease (COPD), long term pain is common. It is associated with reduced physical activity, sadness, and increased dyspnoea (shortness of breath).
Is COPD worse at night or morning?
Morning symptoms often characterize chronic obstructive pulmonary disease (COPD). A significant number of individuals with COPD consider the morning as the most challenging time of day due to increased symptoms and restricted physical activity.
Is climbing stairs good for patients with COPD?
Patients with severe COPD noticed a similar decrease in PaO2 when walking or climbing stairs. Compared to walking, stair climbing caused more noticeable hyperinflation of the lungs, increased blood lactate levels, and more dyspnoea.