Best Neurology Hospital in Hyderabad for all Neurological Conditions
PACE Hospitals is one of the Best Neurology Hospital in Hyderabad, India, providing holistic and patient centric neurology treatment. The team of experienced and skilled neurology doctors, neurosurgeons have vast expertise in managing all kind of critical neurological conditions, including:
- Epilepsy
- Alzheimer's disease
- Parkinson disease
- Stroke
- Brain tumor
- Brain cancer
- Movement disorders
- Ataxia
- Headache
- Multiple sclerosis
- Neurobehavioral and Neuromuscular disorders
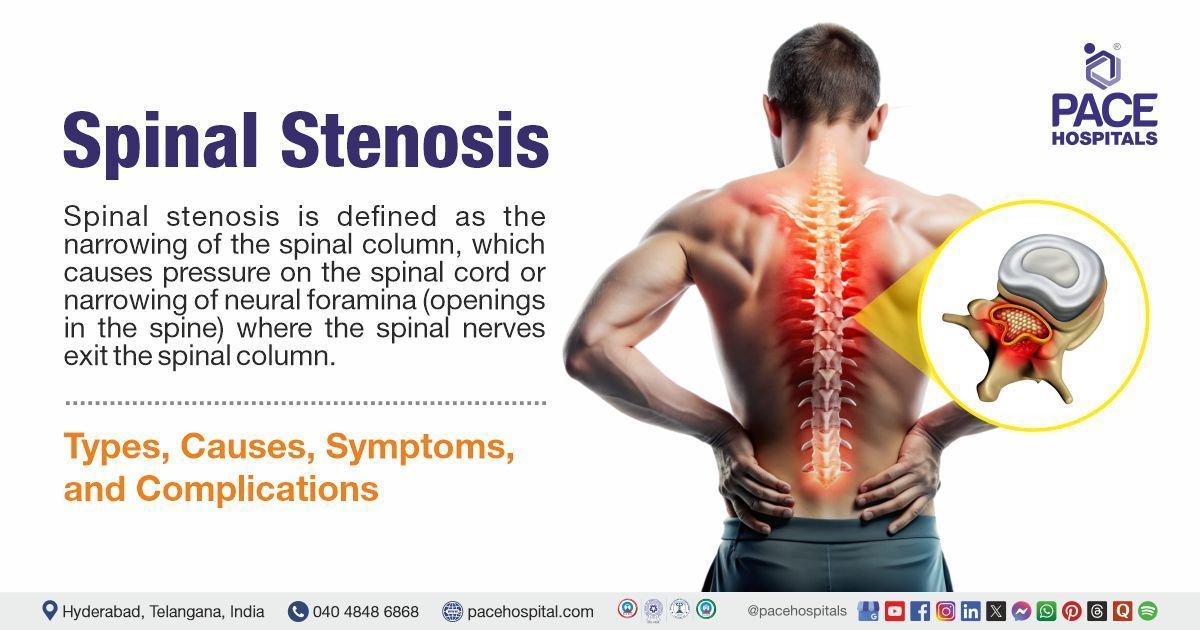
- Spinal cord disorder etc
Why to choose us?
Comprehensive Neurology Treatment
Providing treatment to a wide range of neurological disorders, including brain cancer, stroke, spinal disorder, neuropathy and neuromuscular abnormalities.
Advanced State-of-the-art Facility
Equipped with advanced and latest diagnostic equipment, robotic and minimally invasive surgical facilities for critical neurological disorders treatment.
Skilled & Experienced Neurology Doctors
Team of experienced neurologists, brain specialist doctor & neurosurgeons with vast experience in laser, minimally invasive and laparoscopic surgeries for brain & spinal cord disorders.
Advanced Centre for Neurology Treatment in Hyderabad, Telangana

The neurology department at PACE Hospitals is one of the top neuro centers in Hyderabad. It is staffed with a team of highly skilled, experienced, and renowned neurology doctors, neurosurgeons, and an interdisciplinary team of adult and paediatric neuro specialists who are experts in diagnosing and managing critical conditions related to the brain, spinal cord, and nerves. They are well-versed in the latest treatment modalities and provide holistic and precise neurological condition treatment with a high success rate.
The department of neurology is equipped with state-of-the-art and cutting-edge facilities that offer a wide array of comprehensive care, including advanced imaging systems, endoscopic equipment, minimally invasive surgeries, intensive care units, and a neurocritical care unit to manage a broad spectrum of neurological conditions, ensuring the highest degree of patient care environment.
3,28,338
99,825
684
2011
Best Neurology Doctor in Hyderabad | Top Neuro Specialist
Team of the best neurologists in Hyderabad, India, having extensive expertise in specialized care for stroke, scissors, epilepsy, headache, head and spinal injuries, movement disorders, multiple sclerosis and sleep disorders, are committed to delivering patient-centric, evidence-based and compassionate treatment care to the patients. The specialized team of brain specialist doctors, spine specialists, nerve doctors and neurosurgeons are highly skilled and apt with the latest and advanced treatment modalities to cater for the utmost treatment care with precision, minimal complications and a high success rate.
Dr. Sandhya Manorenj
MBBS, DNB (General Medicine), DNB (Neurology), FNR, MRCP (UK), Neurology (SCE), FEBN, FRCP (London)
23+ years of Exp.
Senior Consultant Neurologist
Dr. U L Sandeep Varma
MBBS, MS (General Surgery), MCh (Neurosurgery), Fellowship in Minimal Invasive and Advanced Spine Surgery
8+ years of Exp.
Consultant Neurosurgeon, Brain & Spine Surgeon
Neurology Diseases and Conditions Explained by Drs
Need Help?
Struggling with the typical brain, spinal cord and nerves related issues or seeking treatment for critical neurological conditions like, epilepsy, alzheimer's disease, parkinson's disease, autism spectrum disorder, brain tumours, brain cancer, stroke, severe head injuries cerebral aneurysms, hydrocephalus, encephalitis, meningitis, spinal disc herniation, Spinal stenosis, peripheral neuropathy or neuromuscular disorders, we offer evidence-based solutions tailored to your needs. Our team of skilled and experienced neurologists and neurosurgeons provides comprehensive and compassionate care for adult and pediatric patients.
What we treat?
We specialize in treating various neurological disorders and conditions affecting the brain, spinal cord and nerves originating from it. From brain stroke, brain tumour, epilepsy, Alzheimer's disease, cluster headache, and migraine to all kinds of neuropathy, spinal disorder, neuromuscular abnormalities and brain cancer, our team of neuro specialist & neurosurgeons is committed to cater patient centric comprehensive solutions for all your neuro health.

Patient Testimonials
A Bangladeshi patient with severe headaches and vision loss for two years was successfully treated with Brain Tumour Surgery.
Successful Minimally Invasive Lumbar discectomy done for L4 and L5 Intervertebral Disc Disorder (Prolapsed Disc) with Radiculopathy and Symptoms of Parkinson's Disease.
Diagnostic Tests and Procedures Performed
We provide comprehensive diagnostic tests. Our advanced and latest screening approach examines any impairment in the brain, spinal cord, abnormalities of neuromuscular functions and severe cases of neuropathy with precision. This results in early detection and precise evaluation, enabling our neurologist and neurosurgeon to make an informed decision about proceeding with the appropriate treatment modalities and surgical procedures.

1. Magnetic Resonance Imaging (MRI): Magnetic resonance imaging (MRI), with the help of computer-generated radio waves and a strong magnetic field, creates precise images of body tissues. Using various sequences of magnetic pulses, the MRI can measure blood flow, display anatomical pictures of the brain or spinal cord, or locate iron (mineral) depositions. MRI is indicated to diagnose stroke, inflammation, brain and spinal cord tumours, traumatic brain injury infection, improperly formed brain regions, vascular irregularities, multiple sclerosis, epilepsy-related brain damage and various neurodegenerative disorders. The radiologist inserts a contrast dye that may be injected into a vein to make certain tissues or organs more visible.
The real-time pictures of blood flow to specific brain regions can be done with functional MRI (fMRI) with the help of blood magnetic properties. Prior to epilepsy surgery, this imaging procedure may be utilised to identify the brain regions responsible for language, motor function, or sensation.
2. Computed Tomography (CT Scan): Computed tomography (CT), with the help of X-rays, provides two-dimensional pictures of organs, bones, and tissues. A CT scan can diagnose the patient’s condition by displaying the damaged area of the brain. CT scans can be used to detect brain haemorrhage. An interventional radiologist will inject a contrast dye into the bloodstream to highlight the various brain tissues. Herniated discs, spine fractures, and spinal stenosis (spinal canal narrowing) can be diagnosed and can all be seen on a CT scan of the spine.
4. Electromyography (EMG):
Electromyography (EMG) measures a muscle's reaction or electrical activity when a nerve stimulates a muscle. The test is used to identify abnormalities of neuromuscular functions. This procedure is done by inserting one or more tiny needles, commonly known as electrodes, which are introduced through the skin and into the muscle during the test. An oscilloscope, a monitor that shows electrical activity as waves, displays the electrical activity detected by the electrodes. In order to hear the activity, an audio amplifier is employed. The muscle's electrical activity during the rest and contraction (light and strong) are measured by EMG. At rest, muscle tissue doesn't typically create any electrical signals.
5. Electroencephalogram (EEG): Electroencephalogram (EEG) test is a non-invasive procedure used to estimate the electrical activity of a patient's brain, with the help of small metal discs or electrodes placed on the patient's scalp, which is further observed by the neurophysiologist to analyse the patient's brain functions. It helps diagnose and monitor several conditions affecting the brain, such as epilepsy, memory loss, Alzheimer's disease, encephalitis, narcolepsy, stroke, the presence of internal bleeding, brain tumours, etc. Routine EEG, Prolonged EEG, Ambulatory EEG, Video EEG, Sleep EEG, and Invasive EEG are the types of EEG tests.
6. Nerve Conduction Velocity: Nerve conduction velocity measures an electrical impulse's speed across the nerve, which detects nerve injury. This test includes the attachment of two electrode patches to the skin over the nerve. The nerve will be stimulated by passing a mild electrode impulse to one electrode, and the other electrode records the resulting electrical activity. The same procedure will be repeated for every nerve being tested. The speed is calculated by measuring the electrode's distance and the time it takes for electrical impulses to travel between electrodes.
This test is indicated to diagnose Charcot-Marie-Tooth disease, Guillain-Barré syndrome, Herniated disk disease, Carpal tunnel syndrome, Chronic inflammatory polyneuropathy and neuropathy, and Sciatic nerve problems.
7. Cerebral Angiography: Cerebral angiography is a diagnostic procedure used to detect cerebral aneurysms or any other blood vessel abnormalities in the head and neck with the help of X-ray imaging. A vascular surgeon performs this procedure by injecting a dye into the patient's arteries/veins to detect any blockage or narrowing. The X-ray creates an image known as a cerebral angiogram, which a vascular surgeon can use to identify blockages or other anomalies in the brain, head and neck that include arteriosclerosis, brain tumours, arteriovenous malformation, aneurysm, tears in the lining of an artery, blood clots and blood vessels inflammation. It can also identify the location and size of an aneurysm or vascular malformation. Angiograms are helpful, especially in strokes.
8. Electronystagmography (ENG): A group of tests to identify involuntary eye movement, dizziness, and balance disorders. It is usually done in patients suffering from vertigo, multiple sclerosis, spinal cord injury, and acoustic neuroma.
Calibration test, gaze nystagmus test, pendulum-tracking test, optokinetic test, positional test, and water caloric test are the types of ENG tests. This test is carried out by placing the electrodes above and below the eye to record electrical activity. ENG can identify nystagmus (involuntary fast eye movement) by measuring the electrical field changes within the eye in response to various stimuli. If stimulation does not cause nystagmus, there may be a problem with the ear, the nerves that supply the ear, or certain brain regions.
9. Sensory Evoked Potentials: Sensory evoked potentials measure the brain’s electrical activity in response to stimulation by touch, sound, or sight. Signals move through the nerves to the brain when the brain is stimulated by sound, touch or sight. These signals are further detected by the electrodes and displayed for neurological interpretation.
Visual evoked response (VER), Brainstem auditory evoked response (BAER) and Somatosensory evoked response (SSER) are the tests used to measure response to visual, auditory, and electrical stimuli. VER test is used to diagnose optic nerve problems that affect sight. BAER test is used to detect hearing ability in addition to diagnosing potential brainstem tumours or multiple sclerosis. SSER test is used to diagnose problems related to the spinal cord that cause leg and arm numbness.
10. Polysomnogram: This diagnostic procedure calculates the activity of the brain and body during sleep by recording the brain waves, eye movement, sleep/wake cycles, breathing, blood pressure, leg and skeletal muscle activity, and heart rate. A polysomnogram is the gold standard for diagnosing obstructive sleep apnoea (OSA), central sleep apnoea, and sleep-related hypoventilation/hypoxia. In addition, it can be used to test for narcolepsy, periodic limb movement disorder, rapid eye movement sleep behaviour disorder, and nocturnal seizures.
A polysomnogram (PSG) is a procedure that assesses underlying causes of sleep problems by using an electroencephalogram, electrocardiogram, electrooculogram, electromyogram, pulse oximetry, airflow, and respiratory effort.
11. Thermography (Digital Infrared Thermal Imaging): This non-invasive diagnostic procedure uses an infrared camera to capture heat map images of the target surface, which aids in the detection of cancer. The heatmap infrared sensing devices measure the slight temperature changes and abnormalities between the two sides of the system or within a specific organ, thus evaluating the complex regional and certain peripheral nerve disorders apart from nerve root compression.
12. Genetic Testing: It is done to comprehend the family history of neurological disease in patients. Prenatal genetic testing (done in utero) can identify congenital abnormalities and neurological disorders. Genetic counselling can help understand its necessity and the meaning of its results. An individual's blood, skin, hair, or other body tissue may be subjected to genetic testing to examine the DNA, chromosomes, or proteins for mutation or any change that is linked to a genetic disorder. A gene's function may be altered due to a mutation, which may impact a gene's entire structure or only a portion of it. Newborn screening, Carrier testing, Prenatal diagnostic testing, Predictive or predisposition genetic testing and Forensic testing are the types of genetic testing.
13. Lumbar Puncture (Spinal Tap): A lumbar puncture is a diagnostic and treatment procedure used to diagnose various disorders by collecting a small amount of Cerebrospinal fluid (CSF) for testing in patients with overproduction or decreased absorption of CSF. A neurosurgeon will carry out this procedure by inserting a hollow needle into the subarachnoid area (space surrounding the spinal column) in the lower back.
The fluid is tested for the presence of proteins, red and white blood cells, glucose, bacteria, viruses, and abnormal cells. Lumbar puncture is used to diagnose Meningitis, Brian and spinal cord cancers, Encephalitis, Subarachnoid space bleeding, Reye syndrome, Myelitis, Neurosyphilis, Guillain-Barré syndrome, Demyelinating diseases, Headaches of unknown cause, Pseudotumor cerebri and Normal pressure hydrocephalus.
14. Dopamine Transporter Imaging with Single Photon Emission Computed Tomography (DaT-SPECT): It can help detect various conditions, especially Parkinson's disease. This imaging technique can help differentiate between the neurodegenerative symptoms of Parkinson's disorders and a dopaminergic deficit from other causes of Parkinsonism, such as drug-induced Parkinsonism, etc.
Neurological Procedures Performed:
1. Craniotomy: A craniotomy is a surgical procedure that includes removing a portion of the skull bone to expose the brain. This procedure involves specialised tools to temporarily remove the bone flap, a part of the skull bone that will be replaced following the brain surgery. Some craniotomy procedures will be performed with the guidance of magnetic resonance imaging [MRI] or computerised tomography [CT] scans for the identification of the precise location of the brain to be treated.
Extended Bifrontal Craniotomy, Minimally Invasive Supra-Orbital “Eyebrow” Craniotomy, Retro-Sigmoid “Keyhole” Craniotomy, Orbitozygomatic Craniotomy, and Translabyrinthine Craniotomy are the types of Craniotomies. This procedure is indicated to repair skull fractures, drain a brain abscess, clip or repair an aneurysm, diagnose, remove, or treat brain tumours, remove an arteriovenous malformation, remove blood or blood clots from a leaking blood vessel, repair a tear in the membrane lining the brain, and epilepsy.
2. Decompressive Craniectomy: Decompressive craniectomy is the temporary removal of a skull portion for the relief of high intracranial pressure. High intracranial pressure within the fixed-volume skull, resulting from cerebral oedema, intracranial haemorrhage, or a space-occupying hematoma, can quickly lead to secondary brain damage, herniation, permanent neurological damage, or death.
Decompressive craniectomy is usually done by removing the fronto-temporal-occipital bone, but in some cases, bi-lateral removal is also done. Decompressive craniectomy effectively increases the brain volume which can be occupied under the scalp and may minimise the ischemic damage by allowing increased cerebral blood flow and tissue oxygenation.
3. Stereotactic Radiosurgery: Stereotactic radiosurgery is used to treat cancer, epilepsy, trigeminal neuralgia, and arteriovenous malformations. It performed carefully bypassing beams of X-rays at the abnormal tissues without making an incision. These X-ray beams alter or destroy the DNA of abnormal cells, thereby preventing their growth and reproduction, resulting in the inactivation and shrinking of abnormal tissue. Fatigue, headache, skin irritation, loss of hair at the treatment site, vomiting, nausea, diarrhoea, seizure, and numbness are the common short-term side effects of Stereotactic radiosurgery.
4. Epilepsy surgery: Epilepsy surgery is a surgical procedure that eliminates the part of the brain that causes seizures; thereby, it inhibits further seizure activities or reduces its severity. Epilepsy surgery is indicated in patients with refractory seizure disorders after receiving two antiepileptic medications (drug-resistant seizure disorder) in a sufficient dosage for a year . Superficial hemosiderosis, Sinus thrombosis, progressive hydrocephalus, memory decline, disconnection syndrome, cough, hoarseness of voice, hemiparesis and dysphagia are some of the major complications of epilepsy surgery.
5. Deep Brain Stimulation (DBS): Deep Brain Stimulation (DBS) is a neurosurgical procedure that is indicated to treat movement disorders associated with Essential tremor, dystonia, Parkinson's disease (PD), and other neurological conditions using implanted electrodes and electrical stimulation. DBS is often referred to as a brain pacemaker or neuromodulation. A neurosurgeon will insert a device beneath the patient’s skin during deep brain stimulation (DBS). Specific areas of the brain get electrical impulses from the device that block the abnormal signals that underlie several neurological conditions.
6. Transcranial Magnetic Stimulation (TMS): Transcranial magnetic stimulation (TMS) is a non-invasive procedure and a type of Brain stimulation therapy that stimulates nerve cells using electromagnetic pulses, which may reduce the symptoms of neurological or mental health conditions.
Repetitive transcranial magnetic stimulation and deep transcranial magnetic stimulation are the two subtypes of TMS therapy. Patients with certain diseases, such as depression, anxiety, post-traumatic stress disorder (PTSD), stroke recovery, and Parkinson's disease, are indicated for TMS. Some adverse effects of this surgical procedure include headaches, discomfort, light-headedness, and tingling.
8. Brain Tumor Surgery: Brain Tumour surgery is a common surgical approach in people with brain tumours, including Pineal region tumours, Pituitary tumours, Rathke's cleft cysts, Skull base tumours and Ventricular tumours. The several methods of brain tumour surgery include craniotomies, MRI-guided laser ablation, and endoscopic brain tumour surgery (neuroendoscopy).
9. Shunt Placement: Shunt placement is a surgical procedure of placing a hollow tube in the patient’s brain (or occasionally in the spine). It is used to relieve hydrocephalus symptoms like gait problems, mild dementia, and lack of bladder control by relieving pressure on the brain. The ventricles (spaces in the brain) often contain the ideal volume of fluid. Hydrocephalus, a chronic neurological condition caused by abnormal cerebrospinal fluid (CSF) accumulation within the ventricles of the brain, creating pressure on the brain. The shunt removes extra fluid that could be compressing the brain and routes it to another part of the body where it can be reabsorbed.
10. Spinal Cord Stimulation: This procedure is carried out by inserting a spinal cord stimulator device that emits low levels of electricity into the spinal cord to reduce pain. This procedure is frequently used when nonsurgical pain management alternatives are ineffective. Spinal cord stimulators consist of thin electrodes and a battery pack (generator). The generator is positioned beneath the skin, typically close to the abdomen or buttocks, and the electrodes are positioned in the epidural space (space between the spinal cord and the vertebrae). These spinal cord stimulator aids in reducing pain by sending electrical impulses with the help of a remote operated by the patient.
11. Craniosynostosis Correction: A congenital abnormality of the infant skull is known as craniosynostosis. It happens when the cranial sutures, which are the fibrous joints connecting the skull's bones, close prematurely. This results in the development of an abnormal shape of the baby's skull. This procedure is carried out by making an incision on the baby's scalp, removing the affected bone, and reshaping and replacing the bone for an improved head shape, thereby increasing space for the developing brain . This procedure can be carried out through endoscopic or open surgery, which yields good cosmetic results with low complications.
12. Laminectomy: It is a surgical procedure where the spinal bone (lamina) is completely or partially removed, resulting in reducing the pressure that may be placed on the spinal cord or the nerve roots as a result of an accident, a herniated disk, a stenosis (narrowing) of the canal, or tumours. Laminectomy is indicated in patients if other medical therapies are not effective. Infection, blood clots in the legs or lungs, bleeding and spinal cord injury are the complications associated with the procedure.
13. Discectomy: It is a surgical procedure used to remove the damaged portion of a disk in the spine that has its soft centre protruding through the tough outer layer. A herniated disk may compress the nearby nerves, resulting in pain radiating down the arms or legs. Discectomy is preferred if the nerve pain causes trouble in standing or walking, failure of other standard treatment for 6 to 12 weeks, such as physical therapy or steroid injections, and difficulty managing the pain in buttocks, arms, legs or chest. Infection, bleeding, leaking spinal fluid, and injury to adjacent spine blood vessels and nerves are the risks associated with this procedure.
14. Transluminal Angioplasty:
Extracerebral arterial stenosis (narrowing of the artery) can be treated with percutaneous transluminal angioplasty (PCTA). It is also indicated for the treatment of extracranial stenosis secondary to atherosclerosis, fibromuscular dysplasia, and vasculitis. In selected cases, percutaneous transluminal angioplasty could also be indicated in symptomatic intracranial stenosis as it produced excellent symptom reduction without any evidence of early restenosis.
15. Neuroplasty: Epidural adhesion is an inflammatory reaction created by a scar due to trauma in the epidural space. It is one of the prime causes of back pain, and various novel treatment approaches have been developed. Neuroplasty is one such treatment modality with the principle of removing the adhesion cause and reducing the inflammation, as it was understood that adhesion and inflammation of the epidural space stimulate the nerve roots, which cause the pain.
16. Expansile Duraplasty:
Chiari malformation type I is characterised by a downward displacement of the cerebellar tonsils through the foramen magnum, leading to disruption of normal cerebrospinal fluid flow in the posterior fossa and compression of the medulla/ upper cervical cord. This condition is mostly treated with suboccipital craniectomy, C1laminectomy, and expansile duraplasty. Expansile duraplasty is often performed to achieve a watertight closure in the posterior fossa while also increasing the space available for the hindbrain. Various dural grafts, including autologous, allograft, xenograft, and synthetic products, can be used.

Stroke Prevention Health Checkup Package
Rs. 2,999
- Lipid Profile
- Blood Pressure Monitoring
- HbA1c (Glycosylated Hemoglobin)
- Carotid Doppler Test
- Consultation with Neurologist
Health and Diseases Information
Why choose PACE Hospitals?
- A Multi-Super Speciality Hospital.
- NABH, NABL, NBE & NABH - Nursing Excellence accreditation.
- State-of-the-art Liver and Kidney transplant centre.
- Empanelled with all TPA’s for smooth cashless benefits.
- Centralized HIMS (Hospital Information System).
- Computerized health records available via website.
- Minimum waiting time for Inpatient and Outpatient.
- Round-the-clock guidance from highly qualified neurologists and neurosurgeons.
- Standardization of ethical medical care.
- 24X7 Outpatient & Inpatient Pharmacy Services.
- State-of-the-art operation theaters.
- Intensive Care Units (Surgical and Medical) with ISO-9001 accreditation.