Brain Tumor - Symptoms, Causes, Complications, Prevention and Treatment
Pace Hospitals
Brain tumor definition
Any abnormal cell growth is called a tumor. If the tumor formation is seen in the brain, it is called a brain tumor. There are chances of a tumor turning into cancer (malignant tumors). Some tumors remain non-cancerous (non-malignant or benign).
The brain and spinal cord comprise the central nervous system (CNS), which plays an important role in maintaining bodily functions, such as movements, sensations, awareness, thoughts, memory, speech, and linguistics. The development of a tumor in the brain could not only induce the ill effects of cancer but also disturb the abilities of the brain, which can trickle down to inadequate performance of bodily functions. A neuro-oncologist can manage brain tumors.
Brain tumor meaning
- The word “brain” is a derivation from Old English “braegen," which originated from the Proto-Germanic source “bragnan” (source also of Middle Low German bregen, Old Frisian, and Dutch brein). All the derivations describe it as a “soft, greyish mass which fills the cranium of any vertebrate."
- The word “tumor” has the Latin “tumere” which says anything about swelling or becoming large. “Tumere," in turn, has been borrowed from the Proto-Indo-European root "teue," which has been incorporated in various words that have underlying themes of swelling or bigger than the rest, etc.
Global incidence rate of brain tumors
As such, the term “brain tumours" comprises not only the various types of cancers that differ with the site of origin but also various types of cancers of the brain; it is difficult to list all brain cancers. Currently, according to the 2020 Globocan data, the death of patients suffering from brain and central nervous system cancer ranked 12th on the list of all cancer deaths worldwide.
A 2008 study mentioned that the annual global age-standardized incidence of primary malignant brain tumors could be estimated around:
- ~3.7 per 1,00,000 for males and
- 2.6 per 1,00,000 for females.
Higher rates of primary malignant brain tumors could be seen within developed countries (males, 5.8 and females, 4.1 per 1,00,000) when compared with underdeveloped countries (males, 3.0 and females, 2.1 per 1,00,000). Also, higher rates of primary malignant brain tumors are seen in males, while females develop higher rates of non-malignant tumors, usually meningiomas.
Understanding the global emphasis of brain tumor from its ever-increasing prevalence and incidence, World Brain Tumor Day has been observed every year on the 8th of June with the intent of increasing public awareness about brain tumors.
Brain tumor incidence in India
While the Indian incidence of central nervous system (CNS) tumors could range from 5-10 patients per 1,00,000 population, the prevalence of brain tumors in the general population has been increasing, accounting for about 2% of malignancies (cancers).
Few Indian studies and registries on brain tumors from Tata Memorial Hospital (TMH), National Institute of Mental Health and Neurosciences (NIMHANS), and All India Institute of Medical Sciences (AIIMS) demonstrated that between 2010-2014, a total of 4295 cases were recorded, in which 1847 (43%) were female and 2448 (57%) were male patients.
A 2020 study from Gujarat Cancer and Research Institute, Ahmedabad, involving 242 Indian children (pediatric patients) demonstrated that boys were more likely to contract with brain tumors when compared to that of girls, with the cerebellum being the most common site of tumor development, followed by the brain’s hemispheres.
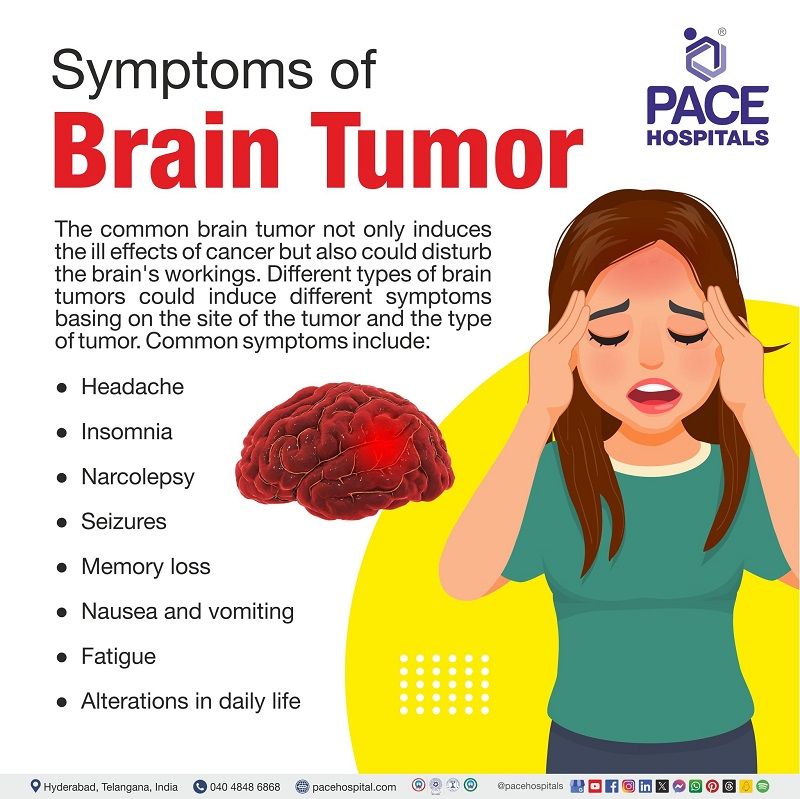
Brain tumor symptoms
As explained earlier, the common brain tumor not only induces the ill effects of cancer but also could disturb the brain's workings, which trickles down into inadequate bodily functions. Nevertheless, it must be understood that different types of brain tumors could induce different symptoms basing on the site and the type of tumor.
Regardless of the type, the common symptoms of brain tumor include:
- Headaches: One of the common signs of brain tumor, severe headaches worsen in the early morning or with activity.
- Sleeping issue: Sleep problems such as insomnia, restless legs syndrome, narcolepsy, and sleep apnea.
- Seizures: Seizures are a medical condition that can occur due to uncontrolled electrical activity in the brain. Patients suffering from brain tumours may experience various types of seizures depending upon the type of tumour and the site of its occurrence. The different types of seizures could include:
- Myoclonic
- Single or multiple muscle jerks, twitches, and spasms
- Tonic-Clonic (Grand Mal)
- Loss of body tone and consciousness, followed by muscle contractions.
- Uncontrolled body functions, such as uncontrolled bladder function
- Development of a 30-second period of no respiration resulting in the blue, purple, white, or green shading of skin colour.
- Sensory
- The patients may experience changes in sensation such as in smell, vision, and/or hearing etc. These may occur in patients without losing consciousness.
- Complex partial
- Loss of situational awareness or a partial/total loss of consciousness. At times, it is associated with muscle twitching and repetitive and unintentional movements.
- Memory loss: In some cases, brain tumour causes memory loss along with changes in personality.
- Nausea: it is usually accompanied by vomiting.
- Fatigue: Muscle fatigue – The patients may not be able to exert their maximal force in response to contractile activity.
- Drowsiness: Can be associated with insomnia or even with healthy sleep.
- Alterations in daily life: In general, and daily activities such as walking, etc., changes may be seen.
- The brain tumour position also influences the development of the symptoms. The various locations which help in the development of various symptoms include:
- Cerebellum: Imbalance and difficulty with fine motor skills
- Frontal lobe of the cerebrum: Loss of initiative, altered judgment, sluggishness, and muscle weakness or paralysis.
- Occipital or temporal lobe of the cerebrum: Partial/complete vision loss.
- The temporal and frontal lobe of the cerebrum: Altered speech, hearing, issues with memory, or emotions, such as aggressiveness, etc. Comprehension loss or linguistic retrieval difficulty (searching for words).
- The parietal or frontal lobe of the cerebrum: Altered tactile and pressure perception, weakness on one side of the body.
- Pineal gland: Inability to look upward.
- Pituitary gland: Issues in lactation (breast milk secretion) and oligomenorrhea (altered menstrual periods).
- Brain stem: Dysphagia (difficulty swallowing), facial numbness or weakness.
Early symptoms of brain tumor
One of the early symptoms of brain tumour in adults is headache.
The “classic” presentation of tumour headache refers to intense pain in the head upon waking up, with dullness, accompanied by feelings of nausea and vomiting. A study published in 1999 noted that several nonclassic findings such as:
- Morning headache occurred in only 31.8% of patients.
- Headache was daily seen in only 10.6% of patients.
- Pain was more likely intermittent (88.4%) than constant.
One of the early signs of brain tumour in babies is increased head circumference.
Widely regarded as the initial signs of a brain tumour in babies is an abnormal increase in head size. The doctors confirm macrocephaly (increased head circumference) by measuring the baby's head circumference with ratio to that of the body.
The common symptoms of brain tumour in children include:
- Recurrent (repeated) vomiting
- Persistent (very frequent) headaches
- Changes in behaviour
- Abnormal movements of the eye
- Problems with balance or coordination
- Double vision or blurred vision
Brain tumor types
Brain tumour classification can be divided into two types:
- Primary brain tumours
- Secondary brain tumours
Primary brain tumours – the tumour/cancer developed in brain. Secondary brain tumours occur when cancers from distant locations metastasize, reaching the cranial cavity.
Differentiated by their site of occurrence and their composition (kinds of cells they are made of), there are more than 120 types of brain tumours. Depending on their malignancy or non-malignancy, all types of brain tumours are divided into:
- Benign tumours, lesions, and cysts (usually do not develop into cancer)
- Graded brain tumours (has a 50% chance of cancer development)
- Brain cancers (typically malignant)
Benign Tumours, Lesions, and Cysts (Usually do not develop into cancer)
A few of the benign brain tumour types include:
- Meningioma
- Pituitary Adenoma
- Craniopharyngioma
- Schwannoma
- Nasopharyngeal Angiofibroma
- Choroid Plexus Tumour
- Dysembryoplastic Neuroepithelial Tumour
- Neurofibroma
- Hemangioblastoma
- Chondroma
- Giant Cell Tumour
- Osteoma
- Arachnoid Cyst
- Colloid Cyst
- Dermoid or Epidermoid Cyst
- Encephalocele
- Meningioma: The most common primary brain tumor (more than 30% of all brain tumors). These form in the meninges (outer tissue layers protecting the brain under the skull). Usually, it is seen more in women than in men. While 85% of meningiomas prove to be noncancerous, few can be persistent, which may not respond to treatment.
- Pituitary adenoma: Tumors that develop at a slow rate in the gland (usually the pituitary gland). About 10% of primary brain tumors are adenomas presenting with endocrinological and vision problems. Nevertheless, since adenomas are benign, they can be treated with surgery and/or medication.
- Craniopharyngioma: The tumours that grow adjacent to the pituitary gland, which appears as solid tumours or cysts and often compress nerves, blood vessels, or adjacent parts of the brain. They can cause endocrinological and vision concerns.
- Schwannoma: Benign, slow-growing tumours appearing on the nerve sheath (a covering around the nerve fibres). They develop in middle-aged adults, which can often cause hearing loss (acoustic neuromas).
- Nasopharyngeal angiofibroma: Develops in the skull base (at the nose) and is usually seen in adolescent boys. Being the most common benign nasopharynx tumour, it spreads around the nose, causing congestion and nosebleeds, among other things.
- Choroid plexus tumour: One of the rare tumours arising in the choroid plexus (where cerebrospinal fluid is produced). Despite being, 90% of these tumours are benign. They most frequently occur in children who are under the age of 2 causing e hydrocephalus (cerebrospinal fluid build-up). This results in increased pressure on the brain, leading to skull enlargement.
- Neurofibroma:
Benign, painless tumours that can grow not only in the brain but also in the nerves of the body and on the spinal cord.
- Dysembryoplastic neuroepithelial tumour: A neuronal-glial brain tumour (made of neurons and supporting cells), dysembryoplastic neuroepithelial tumour is a rare tumour originating in the brain and spinal cord in children and teens causing seizures.
- Hemangioblastoma: These benign tumours of the cerebral blood vessels, which can usually be removed through surgery. Rarely, they appear in multiple sites as a symptom of Von Hippel-Lindau (hereditary disease).
- Chondroma: Very rare benign tumours formed in cartilage found in the base of the skull base and the paranasal sinuses. They usually originate within 10–30 years of age. Slow growth eventually causes either bone fracture or increased bone growth, pressuring the brain.
- Giant cell tumour:
Usually affecting the bones of the limbs, these rare tumours can also be found within the skull. Most giant cell tumours are benign, occurring between 20–40 years of age.
- Osteoma: Slow-growing benign tumours seen on the facial bones and skull base, usually without any symptoms. Nevertheless, breathing, vision, or hearing loss can be seen with large osteomas growing in certain areas of the brain.
- Arachnoid cyst: Common benign cysts that develop at birth in the meninges (membranes surrounding the brain filled with cerebrospinal fluid). They cause no symptoms and usually are left untreated.
- Colloid cyst: A benign mass appearing in the third ventricle of the brain, which blocks the cerebrospinal fluid pathways, resulting in hydrocephalus and headaches. With surgery, these can be removed, especially in the case of extreme hydrocephalus.
- Dermoid or epidermoid cyst: Slow-growing lesions originate from leftover skin tissue from embryonic development, which can be treated with surgery.
- Encephalocele: A birth defect in which a sac-like protrusion is seen in the meninges. This rare birth defect is seen due to the failure of partial closure of the neural tube during the embronic stage. The neural tube is seen in the spinal cord and in the brain. Encephaloceles could be seen either in the skull base, or at the top or between the forehead and nose or at the back of the skull. These encephaloceles can cause deformities in the face and cranium that are repaired with surgery.
Graded Brain Tumours (has a 50% chance of cancer development)
- Glioma
- Ependymal Tumours
- Hemangiopericytoma
- Germ Cell Tumours
- Pineal Tumours
- Glioma: A common brain tumour that can also be found in the spinal cord at times; these gliomas originate from the glial cells. Comprising about 33% of all brain tumours, there are several types of glioma tumours, such as:
- Astrocytomas: Usually seen in young adults or children and can be surgically removed.
- Oligodendrogliomas: An aggressive brain tumour
- Ependymal Tumours: Rare tumours that arise from the walls of the central canal of the spinal cord or from the ventricles. The various types of ependymal tumours include:
- Subependymoma: Benign tumours growing from the ventricular wall into the spinal fluid spaces in the brain, blocking the flow of spinal fluid flow.
- Myxopapillary ependymoma: Slow-growing benign tumours from the ependyma of the filum terminale, occurring between 30–50 years of age.
- Ependymoma: Similar to gliomas, these ependymomas possess specific genetic mutations. Depending on the origin site, their behaviour differs.
- Hemangiopericytoma: Rare skull base tumours involving blood vessels that could be either benign or malignant. In the head region, they are usually seen around the paranasal sinuses and the nasal cavity.
- Germ Cell Tumours: When germ cells get transported (accidentally) into the brain during fetal development, it results in benign or malignant germ cell tumours. Germ cells usually develop into eggs (in the female) or sperm (in the male).
- Pineal Tumours: Developed in the pineal gland region, pineal tumours can cause hydrocephalus through the blockage of cerebrospinal fluid pathways. Usually, a lumbar puncture or, in some cases, a simple blood test is done to find markers necessary for the pineal tumour diagnosis. In other cases, surgery for biopsy is recommended.
Brain Cancers (Typically malignant)
- Chordoma
- Chondrosarcoma
- Medulloblastoma
- Olfactory Neuroblastoma
- Lymphoma
- Gliosarcoma
- Rhabdomyosarcoma
- Paranasal Sinus Cancer
- Atypical Teratoid/Rhabdoid Tumor (AT/RT)
- Chordomas: A rare type of bone cancer (<1%) seen in the skull base or the lower back. It can pressure the nearby nerve tissue with its invasion. Despite displaying benign tendencies with its slow growth, its refractory inclination is as lethal as a malignant as it keeps coming back to spread to other areas.
- Chondrosarcoma: A malignant bone cancer that develops between 50-70 years of age, affecting the cartilage. This aggressive cancer could develop in the thighbone, arm, pelvis, etc, spreading to the head and spine. It could also develop directly in the face bones or skull base.
- Medulloblastoma: One of the most common malignant brain tumors in pediatric patients (5-9 years), medulloblastoma arises in the cerebellum. It is of various types with varying aggressivity.
- Olfactory Neuroblastoma: A rare malignancy associated with nose bleeds and difficulty breathing from the nose, olfactory neuroblastoma develops in the nose in the olfactory nerve (nerve transmitting olfactory impulses (smell) to the brain. Gradually, patients lose their sense of smell.
- Lymphoma: A type of tumor that forms in the lymphatic system (part of the body's immune system). Lymphomas can either spread from other body parts to the brain or form in the brain (primary central nervous system lymphomas) directly. Usually primary CNS lymphomas are often treated with chemotherapy and radiation.
- Gliosarcoma: Rare type of glioma combined with other supportive tissues. These can be aggressive and spread to other areas apart from being resistant to therapy.
- Rhabdomyosarcoma: A rare soft tissue cancer occurring not only in the head but also in many parts of the body (in muscles). Children have more of an affinity to develop rhabdomyosarcomas, which starts with complaints of the eyes or face.
- Paranasal Sinus Cancer: Formed in the cells lining the hollow spaces of the bones around the nose (maxillary sinuses (in the cheekbones under the eyes) and the ethmoid sinuses (beside the upper nose)).
- Atypical Teratoid/Rhabdoid Tumor (AT/RT): An embryonal tumor that typically affects children lesser than seven years of age. It is an aggressive cancer with low survival rates despite providing therapy.
Brain tumor risk factors
There are various risk factors that increase the propensity of developing a brain tumour. Despite the existence of one or various risk factors, brain tumour development may not be seen. There have been cases in which the development of brain tumours is seen even in patients without any risk factors and, similarly, cases with various risk factors with no development of brain tumours. The common risk factors that could increase a person’s risk of developing a brain tumour include:
- Age
- Gender
- Occupational exposures hazards
- Genetic history
- Infections and allergens
- Exposure to electromagnetic fields
- Exposure to ionizing radiation
- Head injury and seizures
- N-nitroso compounds
- Age: Although anyone at any age can develop a brain tumour, the propensity of brain tumours is higher among children and elderly older adults.
- Gender: The masculine gender (males) rather than the feminine (females) gender is likely to develop a brain tumour. Nevertheless, the type and location of the cancer origin can also contribute to the disparity. E.g., Meningioma is more common in women.
- Occupational exposure hazards: It is common to find hazards and brain tumour risk factors in the workplace, and implementation of risk reduction strategies was the prime strategy to mitigate the risks. Some of the chemicals that increase the risk of brain tumours with prolonged exposure include pesticides, oil products, solvents, vinyl chloride, rubber, etc. Scientific evidence supports these possible risks, which are yet to be reinforced.
- Genetic history: Hereditary genetic factors can influence the development of brain tumours. They include:
- Li-Fraumeni syndrome (a genetic disorder of increasing cancer risk)
- Neurofibromatosis (genetic condition of increasing cancer risk in brain and spinal cord)
- Nevoid basal cell carcinoma syndrome (a congenital multisystemic disease)
- Tuberous sclerosis (a genetic condition which causes the development of benign tumours)
- Turcot syndrome (a rare genetic disorder causing small growths in the intestines, brain, or spinal)
- von Hippel-Lindau disease (a genetic condition causing benign tumour development)
- Infections and allergens: There could be various infections that increase the risk of infection, such as:
- Epstein-Barr virus (increases the risk of central nervous system cancer and lymphoma).
- Cytomegalovirus (its presence is seen in brain tumour tissue).
- Allergens (anything that causes allergies) Studies demonstrated that patients displaying a history of skin allergies have a lower glioma risk.
- Electromagnetic fields: Despite a correlation, a proper causality hasn’t been established stating the role of electromagnetic fields in brain tumours. Exposure to electromagnetic energy can be experienced from power lines or increased cell phone use.
- Ionizing radiation: Any diagnosis or treatment containing exposure to the brain or head with ionizing radiation could trigger a brain tumour. Common ionizing radiation includes X-rays, CT scans, PET scans, etc.
- Head injury and seizures: A link has been established between head trauma and meningioma; however, studies are yet to discover the connection between head trauma and glioma. Similarly, there have been cases of seizures presenting with a history of brain tumours, but studies are underway to discover vice versa.
- N-nitroso compounds: When animals eat nitrite and nitrate-containing foods, they generate N-nitroso compounds in their meat, which can't be removed even by processing. N-nitroso compounds can increase the risk of both childhood and adult brain tumours. In some cases, certain diets can induce the production of N-nitroso compounds endogenously. It can also be found in cured meats, cigarette smoke, and cosmetics.
Brain tumor causes
Brain cancer (in fact, any cancer for that matter) is characterized by uncontrolled proliferation and abnormal cell growth, leading to the formation of cellular lumps called tumours which may be benign (non-spreadable tumours, confined to a specific area) or malignant tumours (metastasized tumours, spreadable to different parts of the body through blood or lymph), generated through angiogenesis (formation of new blood vessels) and further metastasize to other body tissues/organs.
Despite the differentiation between the various types of brain tumours, the possible causes of brain tumour always involve mutations in various genes. The uncontrolled proliferation of the cells is an abnormality and develops as a result of mutations in different genes, mainly proto-oncogenes, tumour suppressor genes and DNA repair genes which are mainly responsible for regulating the process of cellular division.
Causes of brain tumor in adults
One of the most common primary brain tumour in adults is glioblastoma multiforme.
- Its heterogeneity of tumour morphology and behaviour (indicated by the term “multiforme”) makes conclusions about its origin extremely difficult.
- Glioblastomas are often divided into two subtypes: progressive, which arises from lower-grade astrocytic tumours, and de novo, which does not.
- The glioblastoma formation is always complex and almost always involves mutation or overexpression of multiple genes.
- Cytogenetically, glioblastomas exhibit
- losses of portions of chromosomes and
- amplification or gain of material on chromosomes.
- Some of the relevant genes which involve in the development of glioblastoma include:
- Growth factor receptors (e.g. EGFR)
- Components of the cell cycle machinery (Rb, CDK4, and the CDK inhibitor p16)
- Regulators of apoptosis (p53, mdm2, ARF, and PTEN).
Causes of brain tumor in child
Central nervous system (CNS) tumors are the most common solid tumor in paediatrics and represent the largest cause of childhood cancer-related mortality.
- Low grade gliomas are the most common paediatric CNS tumour, comprising 30-40% of all CNS tumours.
- Brain tumour is caused by genetic alterations in paediatric low-grade gliomas involve the RAS-MAPK pathway, with the majority involving the BRAF oncogene.
- MAPK pathway activation in low grade gliomas has mediated oncogene-induced senescence (death), which may be one causal explanation for the relatively benign nature of these tumours.
Complications of brain tumor
Many patients with brain tumors develop long-term sequelae with an impact on survival or quality of life. The most common complications include:
- Epilepsy
- Vascular complications
- Cognitive impairment
- Vasogenic edema
- Endocrine
- Fertility
- Infectious complications
- Tumor-Related Epilepsy: Brain tumor epilepsy (seizures) are common among patients with brain tumors, with an overall incidence ranging from 35-70%. Multiple studies confirmed higher epilepsy prevalence in low-grade glioma patients with isocitrate dehydrogenase (IDH) mutations, confirming that molecular characteristics of tumors play a role in the development of epilepsy. Due to the high percentage of epilepsy, prophylactic antiepileptic drugs (drugs given to avoid epilepsy) are usually given to brain cancer patients.
- Vascular Complications: Glioma patients carry one of the highest risks of venous thromboembolism (VTE) among cancer patients, with rates up to 25–39%. A retrospective study showed that thromboembolic complications in brain tumor patients are responsible for 22% of readmission within 30 days of surgery. VTE can prove difficult to treat and is associated with worse survival, especially with comorbid intracranial conditions such as stroke (blockage of blood supply to the brain or bursting of blood vessels in the brain) or tumors susceptible to hemorrhage. In glioma patients, the risk of spontaneous intratumoral hemorrhage is reported between 2-8%. The neuro-oncologist may prescribe anticoagulation therapy. Its safety profile is well documented for both primary central nervous system tumors as well as metastases. Nevertheless, the neuro-oncologist takes extreme care to closely monitor it as it has greater chances of adversarial impact.
- Cognitive and Behavioral Complications: Patients with brain tumors are prone to cognitive impairment, which occurs either due to the cancer or its treatment. However, strong evidence suggests that even prior to treatment, a significant proportion of patients with non-CNS malignancies experience cognitive impairment prior to treatment (up to 30%), with higher prevalence during and after brain tumor treatment reaching up to 75% of patients. Chemotherapy plays a key role in cognitive impairment, and numerous studies have reported alterations in brain structure and function following chemotherapy. In such cases, the neuro oncologist prefers stereotactic radiosurgery to the surgical cavity post-resection for brain metastases as it appears safe with no significant cognitive decline or impairment in quality of life parameters. The management of cognitive impairment in cancer patients remains challenging. Psychostimulants have been studied with variable results. Other non-pharmacological treatments, such as cognitive behavioral therapy (CBT) and cognitive rehabilitation, may be helpful in selected patients.
- Vasogenic Edema: Also called brain edema or cerebral edema, vasogenic edema brain tumor is an extracellular fluid accumulation resulting from a disrupted blood-brain barrier (BBB). Management of vasogenic edema remains challenging for both primary central nervous system (CNS) malignancies as well as metastases. Its pathophysiology remains complex, with increased blood–brain barrier permeability being a key factor.
- Endocrine Complications: Endocrinopathies are not uncommon in brain tumor patients, with an incidence that may exceed 30% if the radiation field involves the hypothalamus and pituitary gland. Dysfunction typically starts within a few years of radiation and is radiation dose-dependent, manifesting as decreased production of growth hormones, thyroid stimulating hormones, adrenocorticotropic hormones, and gonadotropins.
- Fertility Complications: Patients with brain tumors are at risk of infertility due to either a direct tumor effect or it could arise as a side effect from chemo and/or radiation therapy; unfortunately, the magnitude of this risk is poorly studied in the brain tumor patient population. The neuro oncologist and the healthcare team would counsil and discus the risk of infertility risk with all patients of reproductive age prior to treatment.
- Infectious Complications: Infections are not uncommon in brain tumor patients. In the absence of supportive clinical findings, the treatment approach chosen by the neurooncologist is mostly guided by imaging findings, especially with recent advances in MR scans. Pneumocystis pneumonia is another neuro-oncological complication which is associated with the use of corticosteroids. Other very rare infections related to immunosuppression may be seen such as herpes reactivation, CMV-related infections, and Aspergillosis.
Difference between Brain tumor and Brain cancer
Not all brain tumours are cancerous, but all brain cancers are considered tumours. Below are the key differences between brain tumours and brain cancer.
| Parameters | Brain tumor | Brain cancer |
|---|---|---|
| Definition | A growth of abnormal cells in the areas of the brain that can be cancerous (malignant) or noncancerous (benign) | A malignant cell growth in the brain which can be primary or secondary. |
| Symptoms | Seizures, headaches, numbness or paralysis in one part or one side of the body, weakness, difficulty speaking, thinking, or finding words, loss of balance, dizziness or unsteadiness, confusion, hearing loss, memory loss, changes in the vision | Persistent headaches, seizures, persistent vomiting, nausea, and drowsiness, behavioural or mental changes, gradual weakness or paralysis on one side of the body, speech problems, and vision problems |
| Growth | Benign brain tumors typically grow slowly, have different borders, and rarely spread. | Typically, they grow rapidly and invade surrounding healthy brain structures. |
| Examples | Meningioma, vestibular schwannoma, and pituitary adenoma. | Neuroblastoma, olfactory, chondrosarcoma, and medulloblastoma |
Difference between Brain stroke and Brain tumor
Brain stroke vs Brain tumor
Brain tumours are the result of abnormal cell growth in the brain which progress gradually with time, whereas stroke is caused by the blockage of the blood supply to the brain. Below are some of the parameters that distinguish brain stroke and brain tumour.
| Parameters | Brain stroke | Brain tumor |
|---|---|---|
| Definition | Brain stroke is a medical emergency condition and occurs when the blood flow is restricted (to the part of the brain or when the brain blood vessel bursts. | A growth of abnormal cells in the areas of the brain that can be cancerous (malignant) or noncancerous (benign) |
| Symptoms | Sudden difficulty in speaking, sudden weakness or paralysis on one side of the body, sudden confusion and difficulty in understanding speech, loss of balance and coordination, dizziness, sudden loss of sensation, abnormal sensations on one side of the body | Seizures, headaches, numbness or paralysis in one part or one side of the body, weakness, difficulty speaking, thinking, or finding words, loss of balance, dizziness or unsteadiness, confusion, hearing loss, memory loss, changes in the vision |
| Onset | Sudden onset and symptoms develop rapidly. | Benign brain tumors typically grow slowly, have different borders, and rarely spread. |
| Recovery | Some people may recover fully, but others may have long-term or lifelong disabilities. | Recovery time depends on many factors, such as size, location of the tumor, age, general health, and complications. |
Brain tumor prevention
As such, the development of brain tumours includes mutation, and it is not possible to control mutations; there are certain initiatives that can be implemented to reduce the rate of mutations and tumorigenesis, thus reducing the rate of brain tumours. The brain tumour prevention tips include:
- Smoking cessation
- Decreasing alcohol consumption
- Ceasing areca nut consumption
- Smoking Cessation: While it takes over ten attempts to discontinue smoking for an average smoker, smoking cessation can be easily achieved if counselling and pharmacotherapy are accompanied by it. With smoking cessation aid prescribed by the neuro-oncologist, the maintained abstinence remains low (18–30%). Research demonstrated that glucagon-like peptide (GLP)-1 agonists can also be prescribed for the reduction of targeting cravings and tobacco addiction.
- Reducing Alcohol Consumption: An intake of 30 and 20 g of alcohol for men and women, respectively, is the maximum daily consumption recommended by the World Health Organization (WHO). Similar to tobacco cessation, pharmacotherapy combined with cognitive behavioural therapy or any other form of evidence-based counselling (EBC) can help in treating alcohol addiction than relying on pharmacotherapy alone. It must be understood that severe alcohol withdrawal may be seen in patients undergoing therapy for alcohol addiction. In such cases, inpatient admission is necessary to treat the risk of seizure and delirium.
- Ceasing Areca Nut Consumption: Various studies from India, Taiwan, and China demonstrated that roughly half of oral cancer cases can be controlled by ceasing areca nut consumption. In brain tumour patients with the habit of areca nut consumption, the neuro-oncologist may conduct awareness programs aimed at areca nut carcinogenicity, which can help promote cessation.
Apart from avoiding the above-mentioned initiatives, other aspects, such as promoting a healthy lifestyle and consuming healthy brain tumour prevention diet (high in fruits and vegetables), can also reduce the risk of any cancers, especially Head and neck squamous cell carcinoma (HNSCC).
Brain tumor screening
Understanding that regular clinical examination is not a reliable tool to screen brain tumours, as neurologic abnormalities are usually seen in the late stages of the neoplastic disease, which are often subtle, the neuro-oncologist may prescribe computed tomography (CT) scan in suspected patients.
Nevertheless, it must be understood that despite being a less expensive test than other examinations apart from being broadly available, the CT scan has a significantly low sensitivity and a non-negligible radiation exposure burden.
Magnetic resonance imaging (MRI), a more sensitive and widely available imaging option, will predictably remain the best weapon for finding the early signs of brain tumor and thus its detection.
- A 2009 meta-analysis regarding incidental findings in 19,559 asymptomatic individuals who underwent brain MRI in 16 different studies demonstrated an overall prevalence of 2.7% of patients with a brain tumor.
- Understanding the low prevalence, the consequence of oversensitive MRI scans cannot be ignored.
- MRI may, at times, display incidental foci, but additional investigation may disprove any underlying pathology.
- Nevertheless, it is better to opt for an oversensitive MRI rather than a low-sensitive CT scan as it is optimistic about living with a brain tumour-free life rather than an undiagnosed brain tumor for the rest of the life, which may present symptoms only at the advanced stages.
Brain tumor diagnosis
The various diagnostic modalities which confirm brain tumor include:
- Magnetic resonance imaging (MRI)
- Tissue sampling/biopsy/surgical removal of a tumor
- CT scan
- Positron emission tomography (PET) or PET-CT scan
- Cerebral arteriogram, also called a cerebral angiogram
- Lumbar puncture or spinal tap
- Myelogram
- Biomarker testing of the tumor
- Neurological, vision, and hearing tests
- Neurocognitive assessment
- Electroencephalography (EEG)
- Evoked potentials
Brain tumor treatment
The various treatment modalities which could include in managing brain tumour include:
Surgery
- Radiation therapy (radiation therapy for brain tumour)
- Chemotherapy
- Targeted therapy
- Alternating electric field therapy (tumour treating fields)
Frequently Asked Questions (FAQs) on Brain Tumor
What is brain tumor?
Any abnormal cell growth is called a tumor. If the tumor formation is seen in the brain, it is called a brain tumor. There are chances of a tumor turning into cancer (malignant tumors). Some tumors remain non-cancerous (non-malignant or benign). Brain tumor development could also cause inadequate performance of bodily functions.
How do I know if I have a brain tumor?
Brain tumors seldom display symptoms during the early stages of development. The symptoms of a brain tumor can vary depending on the location and size of the tumor. In few cases, the patients may notice brain cancer symptoms such as persistent headaches, seizures, changes in vision or hearing, difficulty with balance or coordination, cognitive changes, mood or personality changes, and nausea or vomiting.
How brain tumor occurs?
Brain tumour occurs by uncontrolled proliferation of cells supported by angiogenesis (formation of new blood vessels). The basic mechanism of brain tumor include mutations in various genes, mainly proto-oncogenes, tumor suppressor genes and DNA repair genes which are mainly responsible for regulating the process of cellular division.
How to prevent brain tumor?
Its hard to stop mutations nevertheless the incidence of tumours can be reduced by reducing the rate of mutations by following factors such as reducing the exposure to electromagnetic fields and ionizing radiation, avoiding foods containing, N-nitroso compounds and treating head injury and seizures etc.
Does brain tumor affect memory?
Yes. Brain tumor can affect memory. Patients with gliomas often experience subjective and objective limitations in cognitive functioning. In various types of brain tumour patients, the percentage of patients with cognitive impairments preceding surgery varied from 30-91%, with memory and executive functioning as the most frequently affected domains.
How to detect brain tumor at home?
Detecting a brain tumor at home is not possible without medical equipment and expertise. Brain tumors require specialized imaging techniques, such as MRI or CT scans, to accurately diagnose them. In case of any suspicion about the development of a brain tumor, it is important to consult a healthcare professional who can perform the necessary tests and provide appropriate medical care. Early brain tumor detection and treatment are crucial for better outcomes.
How long before brain tumor symptoms show?
The duration before brain tumor symptoms show can vary depending on various factors. According to a Thai study published in 2010, the average duration of symptoms in patients with brain tumors could be 471 days. However, certain factors such as age, type of tumor, and specific symptoms can influence the duration of symptoms. In some cases, brain tumor warning signs may appear within a month or less, which may suggest a malignant brain tumor. It is important to note that these findings of signs and symptoms of brain tumor are based on retrospective analysis and individual cases may vary.
Can stress cause brain tumors?
While currently there is not sufficient evidence to suggest the direct causes of brain tumors with exposure to stress, it must be understood that stress could influence the growth and progression of tumors. Stress can lead to inflammation and immune system dysregulation, which may create an environment conducive to tumor growth. Additionally, stress hormones like corticotropin-releasing hormone (CRH) can stimulate the release of mediators that disrupt the blood-brain barrier, potentially allowing tumor cells to enter the brain. Further research is needed to fully understand the relationship between stress and brain tumors.
What were your first signs of a brain tumor?
The first signs of a brain tumor can vary depending on factors such as the location, size, and rate of growth of the tumor. Common initial symptoms can include headaches, nausea and vomiting, changes in vision, seizures, motor system abnormalities, cranial nerve palsies, and behavioral changes. However, it's important for the patients to take note that these symptoms may not be specific to brain tumors and can be caused by other conditions as well.
How many brain tumors are benign?
The majority of brain tumors are benign. An American study published in 2017 concluded that the benign tumors account for the majority of primary neoplasms affecting the central nervous system. Meningiomas, schwannomas, and pituitary adenomas are some of the most common benign brain tumors. However, it's important to note that the classification of brain tumors as benign or malignant depends on their histology and behavior. A competent neuro oncologist can understand the subtle nuances in diagnosing a benign from a malignant brain tumor.
Is smelling smoke a sign of brain tumor?
Smelling smoke or any other components during their absence is called “phantosmia (phantom smell experiences)”. Phantosmia could be genetic or health-related incompetencies. Phantosmia is more seen with the female gender, patients with high vascular risks. In case of nervous system related aspects; phantosmia could arise due to head trauma, epilepsy, migraine, any form of cancer, hypothyroidism, and schizophrenia.
What food is good for brain tumor patients?
A 2013 study demonstrated that the risk of brain tumour is decreased when the subjects were consumed leafy green and yellow-orange vegetables but with noncured meat, the risk of gliomas was slightly increased. Similarly, higher risk with brain tumours (gliomas) was seen with grain, egg, and citrus fruit consumption and were also observed.
Can brain tumor be detected in blood test?
Usually blood tests alone may not directly diagnose brain tumours, but certain blood tests for biomarkers like GFAP, IL13Rα2, NLR, SII, and PIV can help determine tumour type, grade, and malignancy degree.
Do mobile phones cause brain tumours?
There has been ongoing debate about the use of cellular telephones increasing the risk of brain tumour development. A 2022 study comprising 14 years follow-up involving 7,76, 156 women demonstrated that there is no significant risk for brain tumours in mobile phone users when compared with those not using phones. For gliomas occurring in the temporal and parietal lobes, the parts of the brain most likely to be exposed to radio frequency electromagnetic fields from cellular telephones, relative risks were slightly below 1.0. The study concludes that cellular telephones under usual conditions does not increase brain tumour incidence.
Share on
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868