Spinal Stenosis - Types, Causes, Symptoms, Diagnosis, Treatment & Prevention
PACE Hospitals
Overview | Prevalence | Types | Causes | Symptoms | Risk Factors | Complications | Diagnosis | Treatment | Prevention | Foraminal stenosis vs Spinal stenosis | Spinal stenosis vs Herniated disc | FAQs | When to consult a Doctor
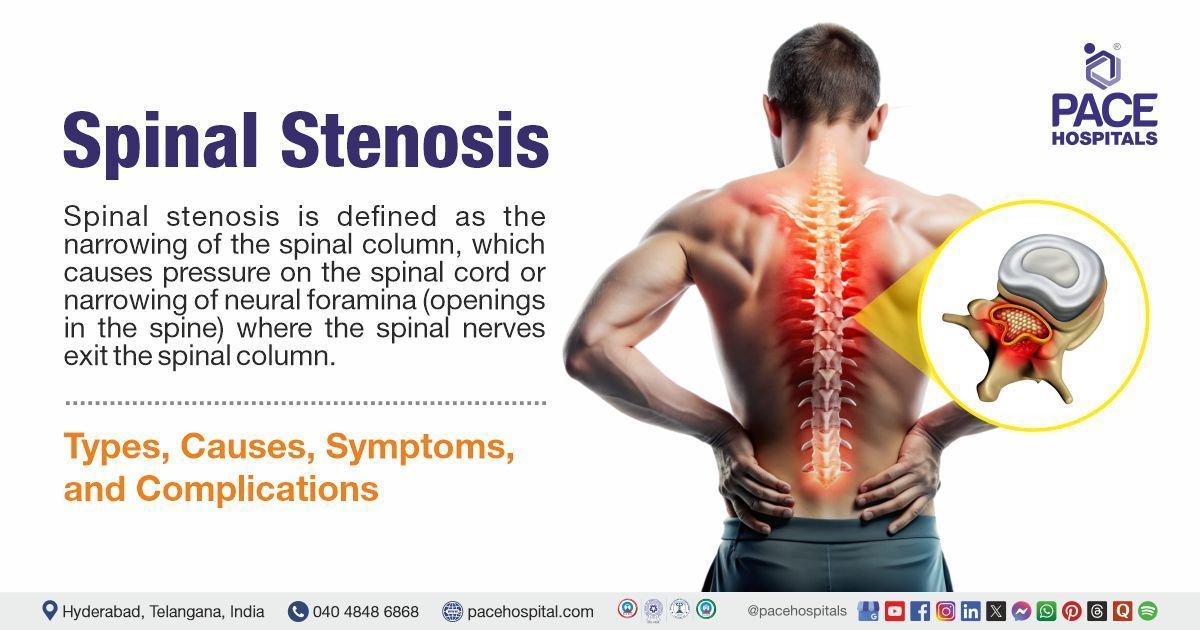
Spinal stenosis definition
Spinal stenosis is defined as the narrowing of the spinal column, which causes pressure on the spinal cord or the narrowing of neural foramina (openings in the spine) where the spinal nerves exit the spinal column. It is caused by congenital or acquired etiologies, whereas iatrogenic spinal stenosis is caused by laminectomy, fusion, and discectomy surgeries. On the basis of the affected spine level, each type of compression produces different symptoms that warrant a specific treatment strategy. Feeling numbness, cramping, or pain in the back, buttocks, thighs, or calves, or in the neck, shoulders or arms, and weakness in a part of a leg or arm are some of the symptoms of spinal stenosis. An orthopedist, neurologist, and neurosurgeon can treat spinal stenosis.
Spinal stenosis meaning
The term spinal stenosis is a combination of two words:
The term “spinal” is derived from the Late Latin “spinalis, " meaning “pertaining to a thorn or the spine”, and it is also derived from the Latin “spina," meaning “backbone”.
The term “stenosis” is extracted from the Greek word “stenosis" meaning “a narrowing”, and from “stenoun" meaning to “narrow”, and then from “stenos" meaning “narrow”.
Spinal Stenosis Prevalence
Spinal stenosis prevalence worldwide
Around 1020 lakhs of cases with spinal stenosis were reported every year, with the highest estimated in Europe, with 2.2 percent, and the lowest in Africa, with 0.94 percent. Many studies have shown that 1 in 1000 people over the age of 65 years and about 5 in 1000 people over the age of 50 years are more likely to develop spinal stenosis.
Types of Spinal Stenosis
Spinal stenosis can affect any part of the spine, but it more commonly affects the lower back and the neck. On the basis of the location of the narrowed portion of the spinal canal, spinal stenosis is classified into three types, and they are as follows:
- Cervical spinal stenosis (CSS): It is the narrowing of the spinal canal in the neck area. This narrowing of the spinal column compresses the nerves and spinal cord, causing neck pain, tingling, and numbness in the arms and legs. Osteoarthritis (a chronic disorder which causes damage to cartilage) bulging of slip disc, herniations, and spondylolisthesis (partial displacement of a bone in the lower back) can cause narrowing of the spinal canal. In some patients, the symptoms do not appear whereas in other individuals numbness or tingling in the arm and neck pain can occur.
- Thoracic spinal stenosis (TSS): It is a clinical condition characterized by a reduction in the volume of the thoracic spinal canal, leading to compression of the spinal cord and nerve roots. Ossification of the ligamentum flavum is the most common cause of thoracic spinal stenosis. Ossification of the ligamentum flavum usually occurs at the lower thoracic spine, especially at the T10-T12 levels, followed by the upper thoracic spine at the T1-T4 levels, due to increased biomechanical stress.
- Lumbar spinal stenosis (LSS): It is the narrowing of the spinal column in the lower back, This narrowing squeezes or compresses the nerves which travel from the lower back into the legs. The pain from this type of spinal stenosis is felt in the lower back and may travel down one or both legs. Patients may develop pain, pins-and-needle-like sensations, weakness, and reduced reflexes in their legs. The pain may be felt over the lower back, which worsens by straightening the back (as when walking or leaning back) and is relieved by leaning forward or sitting.
Spinal stenosis is mainly classified based on the cause as:
- Primary (Congenital) spinal stenosis: It is caused by congenital abnormalities or a disorder of postnatal development.
- Secondary (Acquired) spinal stenosis: This results from degenerative changes or as a result of local infection, trauma, or surgery.
Spinal stenosis is classified on the basis of affected anatomical structure as:
- Spinal canal stenosis (Central canal stenosis): It occurs due to reduced diameter in the anteroposterior, transversal, or combined dimensions which is secondary to loss of disc height with or without herniated disk (bulging of the intervertebral disc), and hypertrophy (increase in size of cells or tissues) of the facet joints and the ligamentum flavum.
- Lateral recess stenosis: In this stenosis decreased disc height, facet joint hypertrophy (with or without spondylolisthesis) and/or vertebral endplate osteophytosis occurs.
- Foraminal stenosis: It can be either anteroposterior which results from a combination of disc space narrowing and overgrowth of structures anterior to the facet joint capsule, and/or vertical, which results from posterolateral osteophytes from the vertebral endplates penetrating into the foramen. This penetration occurs along with a laterally bulging annulus fibrosus or herniated disc which compresses the nerve root against the superior pedicle.
Spinal Stenosis Causes
Different factors can cause narrowing of the spinal canal, leading to spinal stenosis. Generally, the vertebral canal provides enough space for the spinal cord, cauda equina, and the exiting nerves. But aging and age-related changes in the spine, injury, other diseases, or inherited conditions can cause narrowing of spaces.
Aging and Age-Related Changes in the Spine
Aging and age-related changes are the most common causes of spinal stenosis, which can occur over a period and slowly cause loss of the normal structure of the spine. With increasing age, the ligaments which keep the vertebrae of the spine in place thicken and calcify (harden due to deposits of calcium salts). Bones and joints also enlarge. When a bone surface starts to extend from the body, these projections are called osteophytes (bone spurs). For example:
- Discs are cushion-like pads that lie between the vertebrae and act like shock absorbers and spacers for the spine. As the disk ages, it dries out and cracks, causing bulging of the disc. A bulging disc can place pressure on the spinal cord or nerve root.
- Spondylolisthesis can occur when one of the vertebrae slips forward on another vertebra, which results in poor arrangement of the spinal column and can put pressure on the spinal cord or nerve roots.
Arthritis
It is a common cause of spinal stenosis. Osteoarthritis and rheumatoid arthritis are the two types of arthritis which affect the spine. They are described below:
- Osteoarthritis: It is a type of arthritis where the tissues in the joint break down over a period. It leads to disc degeneration and an enlargement of the bone that causes narrowing of the central and nerve root canals, causing spinal stenosis.
- Rheumatoid arthritis: It is a chronic (long-lasting) inflammatory disease, mostly affecting the joints. It is not a common cause, but damage from rheumatoid arthritis can cause significant problems with joints in the spine, leading to spinal stenosis.
Inherited conditions
Some people are born with inherited conditions which can cause spinal stenosis. These conditions usually cause the narrowing of the spinal canal, leading to spinal stenosis. A few examples of inherited conditions which cause spinal stenosis are listed below:
- Congenital stenosis occurs when an individual is born with a small and narrow spinal canal.
- Scoliosis is a curvature of the spine, which usually occurs in children and teens.
- Achondroplasia, which is an inherited condition, causes problems with the formation of bones in the spine and other bones of the body.
Other conditions
The following are some of the other conditions which can cause spinal stenosis:
- Tumors of the spine: These are abnormal growths of soft tissue which damage the spinal canal by causing inflammation or growth of tissue into the spinal canal. This causes narrowing of the space and bone changes, leading to spinal stenosis.
- Paget’s disease: It is a chronic disorder where the bones grow larger and become weaker than normal. With the progress of this disease, new bone forms at a faster rate, these new bones do not form correctly, leading to larger bones that are weaker and softer than normal bones. These new bone formation can cause problems with the structure of the bone, changing the spaces in the spinal canal, leading to spinal stenosis.
- Fractures due to trauma or other medical conditions: Fractures can cause misalignment of the spine and the spinal canal or cause fractures which produce fragments of bone that penetrate the spinal canal.
- Ossification of the posterior longitudinal ligament: It occurs when deposits of calcium form on the ligament, which runs up and down behind the spine and inside the spinal canal.
Spinal Stenosis Symptoms
Narrowing of spaces within the spine, most often in the lower back and neck area leads to the development of symptoms. This narrowing applies pressure on the spine, thereby causing symptoms. In the majority of patients, the symptoms develop and progress slowly over a period and in some cases, the symptoms may not show. Depending on the location of the narrowing in the spine, the symptoms may vary.
Spinal stenosis symptoms lower back
Signs of spinal stenosis in the lower back include:
- Pain in the lower back
- Burning pain which radiates down the buttocks and to the legs, this pain worsens with standing or walking and gets better with forward leaning.
- Numbness, tingling sensation, or cramping in the legs and feet, and this numbness may be more pronounced while walking or standing and gets better with leaning forward.
- Weakness in legs and feet.
Spinal stenosis symptoms neck
- Signs of spinal stenosis in the neck area includes:
- Neck pain
- Numbness or tingling sensation radiating down the arms into the hands
- Weakness in hand, arm, or fingers
Severe spinal stenosis symptoms include
- Problems in bowel functioning
- Problems with bladder functioning
- Problems in sexual functioning
Spinal Stenosis Risk Factors
A risk factor can be anything which can increase the likelihood of developing the disease. The following are some of the factors that can increase the risk of developing spinal stenosis:
- Individuals aged 60 years or older
- Individuals who are born with a narrower-than-average spinal canal
- Individuals who have experienced an injury to the spine
- Individuals with osteoarthritis and rheumatoid arthritis
- Individuals who have experienced swelling or inflammation of the spine
- Individuals who have tumors on the spine
- Individuals with Paget’s disease
- Individuals with neck or back injury
- Individuals with lower back pain history.
Spinal Stenosis Complications
There is always a risk of complications from an underlying condition. Complications of spinal stenosis result from the narrowing of the spine column. Pain that results from spinal stenosis is a serious complication that can affect the quality of life.
Lumbar spinal stenosis surgery complications
With every surgery, there is always a risk of complications. Lumbar decompression surgery has some risk of complications, and they are as follows:
- Infection: It is one of the most common complications of any surgery. It generally occurs at the site of incision, and it is more likely to develop in diabetic patients. Infections can be treated with antibiotics.
- Blood clots: After lumbar decompression therapy, particularly in the leg, there is a risk of blood clot formation called deep vein thrombosis (DVT). It causes pain and swelling in the leg and may lead to a serious problem called pulmonary embolism (blood clots breaks and blocks blood vessels of the heart.
- Dural tear: Dura is a watertight sac of tissue which covers the spinal cord and spinal nerves. During all the types of spinal surgery including lumbar decompression surgery there is an increased risk of tear of dura matter. This tear can lead to cerebrospinal fluid (CSF) leaking after the procedure if the tear is not repaired or treated.
- Leakage of cerebrospinal fluid: Accidental damage to the nerve lining during lumbar decompression therapy can lead to leakage of cerebrospinal fluid. Small leaks become apparent after the operation, causing headaches and the wound to leak.
- Nerve injury and paralysis: In some patients who have undergone lumbar decompression therapy, new numbness or weakness may develop in one or both legs. This complication may develop due to bleeding inside the spinal column or due to leaking of spinal fluid, or due to accidental damage to the blood vessels and nerves. Paralysis is a serious complication but occurs very rarely.
- Facial sores: During lumbar decompression surgery, the patient is positioned down faced. The patient is made to rest on the forehead and chin while the procedure is carried out, due to that some patients may develop red sores on their face or chin that last for several days.
- Death: Though it is rare, but risk of death always remains with surgeries, either during or after the procedure. Blood clot formation, heavy blood loss, and a bad reaction to anesthesia can be life-threatening and can lead to death.
Cervical spinal stenosis surgery complications
Posterior cervical decompression and fusion are the most commonly used surgical techniques in treating various cervical spine pathologies, including cervical spinal stenosis. There are various complications associated with posterior cervical decompression and fusion therapy; the following are some of the common complications:
- Acute blood loss anemia: Anemia is one of the common complications following spinal cord injury. During surgery, patients with cervical spinal stenosis may have sudden excessive blood loss that results in anemia.
- C5 palsy: It is a serious complication following cervical decompression therapy. During the surgery the C5 nerve root gets damaged resulting in weakness of the deltoid muscle, it can also involve biceps muscles causing decreased elbow flexion.
- Surgical site infection: It is one of the most notable complications following spine surgery which leads to longer hospital stays, poor patient outcomes, and high morbidity and mortality.
- Neurologic deficit: Neurologic deficit is rare, but a possible complication following anterior cervical decompression and fusion therapy. This deficit includes numbness, tingling, or burning sensation in the neck.
- Dural tears: These are the most commonly observed complications in spine surgery. The dura, which is a thin membrane covering the spinal cord, is damaged during cervical decompression.
Spinal Stenosis Diagnosis
Diagnosis of spinal stenosis involves a combination of medical history, physical examination and some diagnostic tests. The following are the steps involved in diagnosing spinal stenosis:
Initial evaluation
- Medical history and family history
- Physical examination
Diagnostic tests
- Imaging studies
- X-rays
- Magnetic resonance imaging (MRI)
- Computed tomography (CT) scan
- CT–Myelogram
- Electromyogram and Nerve Conduction Study
Spinal Stenosis Treatment
Spinal stenosis is a condition that is characterized by the compression of the nerve roots by a number of pathologic factors, potentially leading to symptoms such as pain, weakness, and numbness. The treatment approach for spinal stenosis is based on factors such as the severity of the symptoms. Treatment involves the following:
Nonsurgical treatment for spinal stenosis
- Physical therapy
- Brace technique
- Medications
- Non-steroidal anti-inflammatory drugs (NSAIDs)
- Corticosteroids
- Neuroleptics
- Complementary and alternative treatment
- Acupuncture
- Massaging the spine and muscles
- Chiropractic treatment and spinal manipulation
Surgical treatment for spinal stenosis
Surgery is recommended when spinal stenosis is not managed by non-pharmacological treatment and by pharmacological treatment. An orthopedist or a neurologist may recommend spinal stenosis surgery right away when numbness or weakness interferes with walking, impaired bowel or bladder function, and other neurologic movements.
The following are some of the surgical interventions involved in treating spinal stenosis:
- Laminectomy
- Spinal fusion
- Minimally invasive surgery
Why Choose PACE Hospitals?
Expert Super Specialist Doctors
Advanced Diagnostics & Treatment
Affordable & Transparent Care
24x7 Emergency & ICU Support
Spinal Stenosis Prevention
There is no guarantee that with lifestyle changes can stop spinal stenosis from developing. But by following these lifestyle modifications, there is a greater chance of preventing spinal stenosis and slowing its progression to further complications. Following are some of the measures to keep the spine healthy:
- Stay active: Regular exercise can strengthen the muscles which support the lower back and helps in keeping the spine flexible. Walking, swimming, and cycling are some of the aerobic exercises that are good for spine health.
- Maintaining healthy weight: Obesity or overweight puts extra pressure and stress on the spine, which can contribute to the development of spinal stenosis. Maintaining a healthy body weight can reduce the risk of spinal stenosis to a greater extent.
- Stretching the spine: Gently stretching the spine can keep the body flexible and provide a better range of motion. It can minimize symptoms such as stiffness and pain and slow down the progression.
- Maintaining good posture: A good posture plays an important role in spine health. Muscles of the abdomen, back, hips, and pelvic floor stabilizes the spine, helps in keeping it aligned and decreasing stress on bones and joints. With good posture, the spine will be neutral with support of the body distributed equally.
- Smoking: Smoking increases the risk of spinal stenosis by accelerating the degeneration of spinal discs. This degeneration causes bulging and narrowing of the spinal column and ultimately leads to spinal stenosis. Therefore, smoking cessation is an important measure to prevent spinal stenosis.
Difference between Foraminal stenosis and Spinal stenosis
Foraminal stenosis vs spinal stenosis
Foraminal stenosis is a specific type of stenosis that affects the foramina which are the small openings in the spine from where the nerve roots exit. Spinal stenosis is the narrowing of the spinal canal because of compression of nerve roots. The following are some of the parameters which differentiate between foraminal stenosis and spinal stenosis:
| Parameters | Foraminal stenosis | Spinal stenosis |
|---|---|---|
| Definition | It is a type of spinal Stenosis, where the openings between the bones in spine narrow. Like Spinal Stenosis, this can also cause the nerve roots passing through spinal cord to get pinched. | It is defined as the narrowing of spinal column or neural foramina due to the compression of nerve roots. |
| Causes | It is caused primarily by age, as well as age-related symptoms. It can be caused by a bulging or a herniated disk, which can press on the foramen and the nerve root, in the lower back. | Lower back pain, numbness, tingling, or cramping in the legs are some of the common symptoms. |
| Symptoms | Most of the individuals don’t experience any symptoms. They experience pain and discomfort if their nerves are moderately compressed. Local pain, numbness, weakness, and sensations of burning or tingling in the extremities affected are some of the symptoms. | Arthritis, Paget disease (A bone disorder that causes bones to become weak, enlarged, and deformed). defects in the spine from birth and past medical history of herniated or slipped disks are some of the common causes. |
| Treatment | Treatment includes physical therapy, medications to relieve pain and inflammation and surgical interventions such as foraminotomy or laminectomy | Treatment includes physical therapy, medications such as non-steroidal anti-inflammatory drugs, neuroleptics. |
Difference between Spinal stenosis and Herniated disc
Spinal stenosis vs herniated disc
Spinal stenosis is narrowing of the spinal canal because of compression of nerve roots. A herniated disc, also called a slip disc, is a condition which occurs when soft cushion of tissue between the bones in the spine bulges outwards. The Following are some of the key parameters that differentiate between spinal stenosis and herniated disc:
| Parameters | Spinal stenosis | Herniated disc |
|---|---|---|
| Definition | It is defined as the narrowing of spinal column or neural foramina due to the compression of nerve roots. | It is defined as a condition which occurs When soft cushion of tissue between the bones of spine bulges outwards. |
| Symptoms | Lower back pain, numbness, tingling, or cramping in the legs are some of the common symptoms. | Lower back pain, numbness or tingling in shoulders, back, arms, feet, neck pain, and muscle weakness are some of the common symptoms. |
| Causes | Arthritis, Paget disease (A bone disorder that causes bones to become weak, enlarged, and deformed). defects in the spine from birth and past medical history of herniated or slipped disks are some of the common causes. | A degenerative process in which, with increasing age, the nucleus becomes less hydrated and weakens is the most common cause of disc herniation. This process leads to progressive disc herniation. |
| Treatment | Treatment includes physical therapy, medications such as non-steroidal anti-inflammatory drugs, neuroleptics. | Nonsteroidal anti-inflammatory drugs and physical therapy are considered as first-line treatment. Surgical treatment for a herniated disc include laminectomies with discectomies depending on the cervical or lumbar area. |
Frequently Asked Questions (FAQs) on Spinal Stenosis
Is there a cure for spinal stenosis?
There is no cure for spinal stenosis, but the treatment can help in managing the symptoms and helps in preventing further progression. Treatment of spinal stenosis includes lifestyle modifications, medications to relieve the symptoms and some surgical interventions.
What happens if spinal stenosis is left untreated?
If left untreated, spinal stenos can lead to some serious complications such as loss of sensation in both legs, loss of bladder and bowel control, cauda equina syndrome (a rare condition where the nerves present at the bottom of the spinal cord are compressed), dural tear, surgical site infection, nerve injury, and paralysis.
Is spinal stenosis a permanent disability?
Spinal stenosis can lead to some serious conditions such as cervical myelopathy (a condition where the spinal cord in the neck gets compressed) or cauda equina syndrome (a condition where the bundles of nerves below the end of the spinal cord called cauda equina get damaged). Though rare, serious spinal conditions can lead to permanent damage or disability.
Can exercise help spinal stenosis?
Yes, regular exercise can strengthen the muscles which support the lower back and helps in keeping the spine flexible. Walking, swimming & cycling, which are some of the aerobic exercises, are good for spine health.
Will spinal stenosis heal on its own?
Spinal stenosis does not heal on its own. The symptoms worsen over time, and medical attention is essential to prevent further complications. Non-surgical treatment, which includes physical therapy, medications such as neuroleptics, and non-steroidal anti-inflammatory drugs can help manages spinal stenosis.
What are the surgical interventions involved in treatment for spinal stenosis?
Surgery is recommended when spinal stenosis cannot be managed with non-pharmacological treatment and by pharmacological treatment. Laminectomy and spinal fusion are the two major surgical interventions involved in treating spinal stenosis. In a laminectomy the surgeon removes part or all of the vertebral bone (lamina), whereas spinal fusion is a surgical procedure in which two or more bones are joined together.
Can massage therapy help spinal stenosis?
Massage therapy has many benefits in treating spinal stenosis. It helps in relaxing the muscles, which decreases tension and pain in the spine caused by muscle tightness. It can also improve blood flow throughout the body, allowing more oxygen and nutrients to reach the affected area and this improved circulation can reduce inflammation in the area around the spine.
Can MRI diagnose spinal stenosis?
Magnetic resonance imaging is the gold standard imaging technique used in the diagnosis of spinal stenosis. Diameter of the cervical spinal canal, distance between the posterior vertebral line and spinolaminar line, and ratio on lateral radiographs have been proposed as criteria for diagnosing cervical myelopathy or spinal canal stenosis Findings of MRI include central stenosis, with the thecal sac which measures less than 100 mm2 in area, hypertrophy of facet and ligament, removal of perineural fat and compression of lateral recess or foramen.
How to identify spinal stenosis in computed tomography?
Computed tomography (CT) scan is performed when other investigations such as X-ray are not conclusive. This is performed to assess the spine for a herniated disk, to assess the presence of tumors and other lesions, the extent of injuries, and to detect spina bifida (a type of congenital defect of the spine), and blood vessel malformations. It is also used to evaluate the effects and outcomes of surgical treatment for spinal stenosis.
Can acupuncture help spinal stenosis?
Acupuncture shows promising results in relieving the pain associated with nerve compression. This ancient method has a marked impact on the pain levels of patients suffering from back pain, particularly when it is caused by spinal stenosis.
What is the role of brace technique in treatment of spinal stenosis?
Orthopedic back braces, which are specially made for spinal stenosis, can provide essential support to the spine. They help in stabilizing the affected area and alleviates pressure on the spinal nerves. These braces can improve daily activities and can provide comfort.
What is the role of neuroleptics in treating spinal stenosis?
Neuroleptics stabilize the neurons within the spinal cord which are overactive, in order to relieve arm or leg pain associated with nerve compression. When taken orally, these agents alleviate discomfort caused by spinal stenosis.
When to consult a doctor for spinal stenosis?
Consult a doctor for spinal stenosis when back, neck, or leg pain, along with numbness or weakness, does not improve with rest or starts interfering with daily activities. The problem occurs when the spinal canal narrows and presses on nerves, and early treatment can help manage symptoms and prevent complications.
Key warning signs include:
- Ongoing back or neck pain
- Tingling or weakness in arms, legs, hands, or feet
- Pain that worsens when standing or walking
- Trouble with balance or coordination
- Loss of bladder or bowel control (serious cases)
If these symptoms persist, a spinal stenosis doctor can perform tests and recommend treatment. In urgent cases, such as sudden leg weakness, severe pain, or bladder/bowel issues, emergency care is essential. An orthopaedic spine specialist or neurologist can provide effective spinal stenosis treatment to relieve pressure, reduce pain, and improve mobility.
Share on
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868