Rheumatoid Arthritis Treatment in Hyderabad, India
PACE Hospitals is a trusted rheumatoid arthritis hospital in Hyderabad, offering specialized care for rheumatoid arthritis, psoriatic arthritis, osteoarthritis, and other inflammatory joint conditions. Our team of the best rheumatologists and orthopedic experts ensures early diagnosis and personalized treatment using advanced imaging and lab diagnostics.
We provide comprehensive rheumatoid arthritis treatment through medication, physiotherapy, lifestyle changes, and surgery when needed. Our goal is to relieve joint pain, reduce inflammation, and restore long-term mobility. With state-of-the-art facilities and a patient-first approach, PACE Hospitals is a leading choice for arthritis care in Hyderabad.
Book an appointment for
Rheumatoid Arthritis Treatment
Rheumatoid Arthritis Treatment Online Appointment
Thank you for contacting us. We will get back to you as soon as possible. Kindly save these contact details in your contacts to receive calls and messages:-
Appointment Desk: 04048486868
WhatsApp: 8977889778
Regards,
PACE Hospitals
HITEC City and Madeenaguda
Hyderabad, Telangana, India.
Oops, there was an error sending your message. Please try again later. Kindly save these contact details in your contacts to receive calls and messages:-
Appointment Desk: 04048486868
WhatsApp: 8977889778
Regards,
PACE Hospitals
HITEC City and Madeenaguda
Hyderabad, Telangana, India.
Why Choose PACE Hospitals for Rheumatoid Arthritis Treatment?
Comprehensive Arthritis Screening Panels: RA Factor, Anti-CCP, ESR, CRP, ANA, HLA-B27 to Accurately Identify Rheumatoid Arthritis
Board-Certified Experienced Orthopedic Doctors, Rheumatologists & Orthopaedic Surgeon in Hyderabad
Minimally Invasive Joint Preservation and Replacement Procedures | Integrated Physiotherapy & Rehabilitation Facilities
Affordable & Transparent Rheumatoid Arthritis Treatment with Insurance & Cashless Options
Rheumatoid Arthritis Diagnosis
Diagnosis of rheumatoid arthritis (RA) is challenging because its symptoms, like joint pain, stiffness, and swelling, are like those of other conditions. Since rheumatoid arthritis (RA) cannot be diagnosed with a single test, rheumatologists employ a combination of imaging tests, blood tests, physical examinations, and a detailed medical history. Early Rheumatoid arthritis (RA) can resemble other types of arthritis, making accurate diagnosis difficult. The rheumatologist considers the following before selecting the appropriate tests to diagnose rheumatoid arthritis.
- Medical history
- Physical examination
Medical history
When assessing a patient with suspected rheumatoid arthritis (RA), rheumatologists start by collecting a thorough clinical history, emphasizing key aspects that help in identifying the disease, including:
- The onset of symptoms and their progression over time.
- Assess the duration of symptoms to determine whether joint pain has persisted for more than six weeks.
- Patterns of joints affected
- Symmetry
- The number of joints affected
- Other associated symptoms
- Systemic symptoms include fever
- Symptoms that affect daily functioning
- Relieving and aggravating factors (The factors seem to lessen or worsen the symptoms)
- Extra-articular Manifestations (any symptoms outside the joints, such as skin changes or eye problems)
- Family and past medical history
Physical examination
- On physical examination, affected joints may be tender to pressure or movement, with or without visible swelling. Synovial thickening is often present and may feel boggy (soft and spongy) upon palpation.
- Joint redness and warmth are typically absent. In cases involving the wrist, signs and symptoms of carpal tunnel syndrome may be observed. When multiple joints are affected, reduced grip strength is commonly noted during physical testing.
- In advanced stages of chronic rheumatoid arthritis, classical physical findings may include ulnar deviation, subluxation of the metacarpophalangeal joints, swan-neck deformity, Boutonnière deformity, and tendon prominence (bowstringing) sign.
- As the disease progresses, patients may also experience a reduced range of motion in the shoulders, elbows, and knees. In the feet, common deformities include hallux valgus (a foot deformity where the hallux (big toe) deviates laterally) and various toe abnormalities.
- Rheumatoid nodules represent the most common manifestation of rheumatoid arthritis outside the joints. They typically develop at pressure points, such as the olecranon, but can also appear over joints in the hands and feet, the patella, and along the Achilles tendons.
Diagnostic Evaluation for Rheumatoid Arthritis
Based on the above information, a rheumatologist may advise the following diagnostic tests to diagnose rheumatoid arthritis:
- Laboratory tests
- Rheumatoid factor (RF)
- Complete blood count (CBC)
- Anti-cyclic citrullinated peptide antibody (anti-CCP).
- Erythrocyte sedimentation rate (often called the sed rate)
- C-reactive protein.
- Other blood tests
- Serum electrolytes
- Liver function tests
- Muscle and autoimmune markers
- Thyroid function tests
- Imaging tests
- X-rays (plain radiographs)
- Magnetic resonance imaging (MRI) and ultrasound
- Computed Tomography (CT) scan
- Positron emission tomography (PET) scan
- Bone scan
- Dual-energy X-ray absorptiometry (DEXA).
- Joint aspiration
- Nodule biopsy
Rheumatoid factor (RF): This blood test detects the rheumatoid factor (RF), an antibody commonly found in the blood of patients with rheumatoid arthritis. The immune system produces a unique protein called an antibody, which typically aids in the body's defense against intruders. Not all individuals with RA test positive for RF. Some individuals with RA test positive for RF and never get the disease, whereas others test positive but have another illness. However, physicians can identify rheumatoid arthritis using this test in combination with other test findings and assessments.
Complete blood count: This blood test evaluates different blood cell counts and can be used to identify anaemia, which is often associated with rheumatoid arthritis (RA).
Anti-cyclic citrullinated peptide antibody (anti-CCP): This blood test examines anti-CCP antibodies, which are frequently present in patients with rheumatoid arthritis. Anti-CCP antibodies may also appear before RA symptoms do, which aids in early identification. As with RF blood testing, the test results are helpful in verifying a diagnosis of rheumatoid arthritis.
Erythrocyte sedimentation rate (ESR): In rheumatoid arthritis, an elevated ESR suggests active inflammation and can help assess disease activity. It is also helpful in monitoring the effectiveness of treatment over time, as a decreasing ESR may indicate a positive response to therapy.
C-reactive protein (CRP): This is another popular test for inflammation that can be used to diagnose rheumatoid arthritis (RA) and monitor disease activity and response to treatments.
Other blood tests: To evaluate overall health and make additional diagnoses, a rheumatologist may perform further tests to assess kidney function, electrolyte levels, liver function, thyroid function, muscle markers, autoimmune indicators, and infection markers. Other specialised tests for rheumatoid arthritis may be considered.
X-rays (plain radiographs): X-ray imaging may not detect early symptoms or changes associated with rheumatoid arthritis (RA), but it remains a standard method for diagnosis and monitoring of the disease. While joint space narrowing and bone erosions visible on X-rays are more suggestive of advanced RA, these features are typically absent or subtle in the early stages of the illness.
Magnetic resonance imaging (MRI) and ultrasonography: These techniques can aid in diagnosing rheumatoid arthritis in its early stages and are used to evaluate the severity of this condition and the extent of joint damage.
Computed Tomography (CT) Scan: This imaging method helps identify bone erosion and joint injury that may not be apparent on conventional X-rays by providing detailed images of joints and surrounding tissues.
Positron Emission Tomography (PET) Scan: Although less commonly used, PET scans can detect inflammation throughout the body and may help assess disease activity or identify systemic involvement.
Bone Scan: Helps identify areas of active inflammation or joint damage, especially in early stages when X-rays may appear normal.
Dual-energy X-ray Absorptiometry (DEXA): It is primarily used to assess bone density. This test is crucial for RA patients who are at a high risk of osteoporosis due to chronic inflammation and corticosteroid use.
Joint aspiration: The process of removing fluid from the area surrounding a joint is called joint aspiration. A syringe and needle are needed for this procedure. This is frequently done to reduce edema or to obtain fluid for examination in order to identify a joint issue or condition. To lessen pain, a local anaesthetic may be used.
Nodule biopsy: By examining under a microscope, tiny tissue samples are collected. This aids in the detection of cancer and other cellular abnormalities.
Stages of Rheumatoid Arthritis
Rheumatoid arthritis (RA) typically progresses through four distinct stages, each marked by worsening inflammation and joint involvement. According to the American College of Rheumatology (ACR), these stages range from early synovial inflammation to advanced joint deformity and loss of function. Understanding these stages is essential for timely diagnosis, appropriate treatment planning, and prevention of long-term disability in patients with RA.
The 4 stages of rheumatoid arthritis are:
- Stage 1: In early-stage rheumatoid arthritis, inflammation begins in the synovial tissue surrounding the joints. Patients may experience mild joint pain, stiffness, and swelling. X-rays at this stage typically do not show any bone damage, as structural changes have not yet occurred.
- Stage 2: At this point, the damaged joints' cartilage is beginning to deteriorate because of inflammation. Although joint abnormalities are not yet evident, X-rays may show symptoms such as subchondral bone degradation and periarticular osteoporosis. Reduced mobility, stiffness, and increased joint pain are possible symptoms.
- Stage 3: At this point, the inflammation becomes severe enough that it seriously damages the bone and cartilage. X-rays typically reveal periarticular osteoporosis, cartilage and bone loss, as well as joint abnormalities. Patients may have noticeable joint deformities, restricted joint function, and severe discomfort.
- Stage 4: At this advanced stage, active inflammation subsides, but joint damage continues to progress. There is evidence of bony or fibrous ankylosis, where joints become fused along with the structural damage seen in Stage 3. This leads to significant loss of joint function, deformity, and disability.
Rheumatoid Arthritis Differential Diagnosis
Differential diagnosis is crucial, since the symptoms of rheumatoid arthritis (RA) can resemble those of many other illnesses. The following disorders are frequently considered:
- Osteoarthritis: This condition often affects the distal interphalangeal (DIP) joints, the small joints located at the tips of the fingers, which are typically not involved in rheumatoid arthritis (RA). Unlike RA, it tends to cause new bone growth rather than significant joint inflammation, and it is less likely to produce widespread symptoms throughout the body.
- Psoriatic arthritis: It can present with joint pain and swelling similar to rheumatoid arthritis and is often associated with a history of psoriasis.
- Systemic lupus erythematosus: This condition can resemble rheumatoid arthritis, presenting with multiple joint inflammation and systemic symptoms, often accompanied by skin lesions or involvement of other organs.
- Sjogren syndrome: This condition can cause joint pain and swelling that resemble those seen in rheumatoid arthritis. Additionally, patients often experience symptoms such as dry eyes and dry mouth, which are characteristic features indicating the involvement of the moisture-producing glands.
- Polymyalgia rheumatica: It is taken into consideration when elderly patients exhibit proximal muscle discomfort and stiffness, particularly in the shoulders and hips. To initiate the correct treatment and prevent any adverse consequences, early identification is crucial.
- Chronic gouty arthritis: This condition is characterized by acute, episodic arthritis that commonly affects the first metatarsophalangeal joint (big toe). Diagnosis is confirmed by identifying urate crystals in the synovial fluid, which helps distinguish it from other types of arthritis.
- Calcium pyrophosphate deposition disease: This disorder often affects major joints, such as the knees, hips, or shoulders, and manifests as either acute or chronic arthritis. The patient's daily activities and quality of life may be significantly impacted by the pain, swelling, and decreased mobility that can result from inflammation in these joints.
Rheumatoid Arthritis Goals of Treatment
The overall treatment goals of rheumatoid arthritis are to improve the patient’s quality of life and prevent permanent joint damage. Rheumatoid arthritis goals of treatment include:
- The primary goal of rheumatoid arthritis is to relieve pain and prevent, slow, or stop joint and organ damage.
- To decrease inflammation and swelling.
- To improve the ability to take part in daily activities.
Treatments of rheumatoid arthritis can help reduce joint inflammation, alleviate pain, slow or halt joint degeneration, minimize disability, and enable individuals to remain as active as possible. Below are the treatment options available for rheumatoid arthritis:
- Nonpharmacological treatment
- Pharmacological treatment
- Surgical procedures
Nonpharmacological management
- Patient Education: Rheumatoid Arthritis (RA) involves patient education for proper management. Patients need to be informed about the characteristics of the disease, including its progressive and chronic nature, available treatments, the significance of taking their medications as prescribed, and lifestyle modifications that can enhance their response to treatment. Providing patients with more information enhances treatment outcomes, reduces long-term complications, and enhances self-management.
- Physical and occupational therapy: This therapy helps improve joint mobility, reduce pain, and enhance daily functioning in patients with rheumatoid arthritis. When combined with medication, they offer a comprehensive approach to disease management.
- Lifestyle modifications: Making lifestyle modifications is crucial for managing rheumatoid arthritis (RA) effectively, as it can help to decrease symptoms and improve overall health. Major changes such as eating a healthy diet, exercising frequently, efficiently handling stress, avoiding smoking, getting sufficient sleep, and limiting alcohol consumption.
Pharmacological treatment
Many of the medications prescribed for rheumatoid arthritis (RA) are designed to reduce inflammation and pain while also slowing or preventing joint damage. These may include:
- Disease-modifying antirheumatic drugs (DMARDs): These are the first-line treatment for rheumatoid arthritis and are also used to manage other inflammatory arthritic conditions. They act by modifying the immune system to prevent joint damage, reduce inflammation, and improve long-term disease outcomes.
- Corticosteroids: These can halt joint deterioration, reduce inflammation, and offer some pain relief. Since these are strong medications with potential adverse effects, the rheumatologist will prescribe the lowest effective dosage to achieve the intended effect.
- Biologic response modifiers (Tumour necrosis factor (TNF) inhibitors): These are a class of drugs used to treat inflammatory and autoimmune diseases, particularly those targeting TNF (Tumour Necrosis Factor). TNF, a pro-inflammatory protein implicated in the illness process, is blocked by them. These medications help people with the condition experience less inflammation, fewer symptoms, and a slower rate of disease progression by blocking TNF activity.
- Targeted synthetic DMARDs (Janus Kinase (JAK) Inhibitors): The class of medications known as targeted synthetic disease-modifying antirheumatic drugs (DMARDs), or Janus Kinase (JAK) inhibitors, is used to manage inflammatory and autoimmune conditions such as rheumatoid arthritis (RA). To modify the immune response, they function by blocking Janus kinases, which are enzymes involved in the signaling pathways of several cytokines.
- Nonsteroidal Anti-inflammatory Drugs (NSAIDs): Nonsteroidal anti-inflammatory drugs are frequently used in the management of rheumatoid arthritis (RA) to relieve pain and reduce inflammation. They are often used as a starting treatment, either alone or in combination with other medications. While effective for symptom control, NSAIDs do not modify the progression of illness or prevent joint damage.
- Interleukin 6 Inhibitors: These are a class of medications used in treating rheumatoid arthritis (RA) that work by blocking IL-6, a pro-inflammatory cytokine involved in joint inflammation and damage. These agents are especially beneficial for patients who don't respond well to TNF inhibitors or conventional synthetic disease-modifying antirheumatic drugs (csDMARDs).
Surgical procedures
- Synovectomy: A surgical procedure that involves the excision of the inflamed synovial lining of a joint. It is performed to relieve pain and swelling and may help to stop or slow the progression of joint damage.
- Total joint replacement (Arthroplasty): It is a surgical technique used to address severe joint abnormalities and destruction in rheumatoid arthritis (RA). Prosthetic implants are used to replace damaged joint components, aiming to reduce discomfort and improve mobility. Due to its effects on mobility and quality of life, hip and knee replacements are the most prevalent.
- Arthrodesis (Joint fusion): This is a surgical technique that permanently fuses 2 bones in a joint, thereby reducing discomfort and increasing joint stability. To manage severe arthritis, it is often considered when other therapies, such as medication or physical therapy, are insufficient. Weight-bearing joints, including the ankle, foot, and wrist, as well as minor joints in the fingers and toes, are frequently the sites of this surgery.
Rheumatoid Arthritis Prognosis
The prognosis of rheumatoid arthritis (RA) is influenced by adherence to treatment and the timing of therapy initiation. RA is a chronic (long-term) and progressive disease with no cure, leading to increased morbidity, disability, and mortality. Most patients experience recurrent flare-ups, and without treatment, outcomes are poor.
Early therapy within six months can improve joint function and reduce disease activity, although mortality rates are similar to those of those treated later. Still, both groups fare better than untreated patients. Within ten years, around 40% of RA patients develop functional disability.
RA also increases the risk of other severe conditions, including cardiovascular disease, lung disease, and certain cancers, contributing to premature mortality.
Frequently Asked Questions (FAQs) on Rheumatoid Arthritis (RA)
Is rheumatoid arthritis hereditary?
Rheumatoid arthritis (RA) is not directly hereditary, but genetics can play a role in increasing the risk of the disease. Having a family member with RA may raise your chances of developing the condition, but it does not guarantee you will get it. Environmental factors, immune system function, and lifestyle choices also contribute significantly to the development of RA.
How to prevent rheumatoid arthritis?
Rheumatoid arthritis (RA) cannot be entirely prevented, but specific lifestyle changes can reduce the risk. Maintaining a healthy weight, exercising regularly, avoiding smoking, and following an anti-inflammatory diet may help. Limiting exposure to environmental toxins and managing infections early may also be beneficial. Early awareness is key, especially for those with a family history of RA.
Is rheumatoid arthritis dangerous?
Rheumatoid arthritis can cause severe and irreversible joint damage if it is not treated promptly or is not adequately managed. This could involve the degeneration of the cartilage that cushions and shields the ends of bones in a joint, as well as erosion of neighboring bone. Over time, joint deformity, reduced mobility, and chronic pain resulting from this injury may have a substantial effect on an individual's quality of life.
What is the main cause of rheumatoid arthritis?
In rheumatoid arthritis (RA), an autoimmune condition, the body's immune system mistakenly targets the joint lining, resulting in stiffness, discomfort, and inflammation. The onset of RA is believed to be caused by environmental factors and genetic predisposition, while the precise reason is unknown.
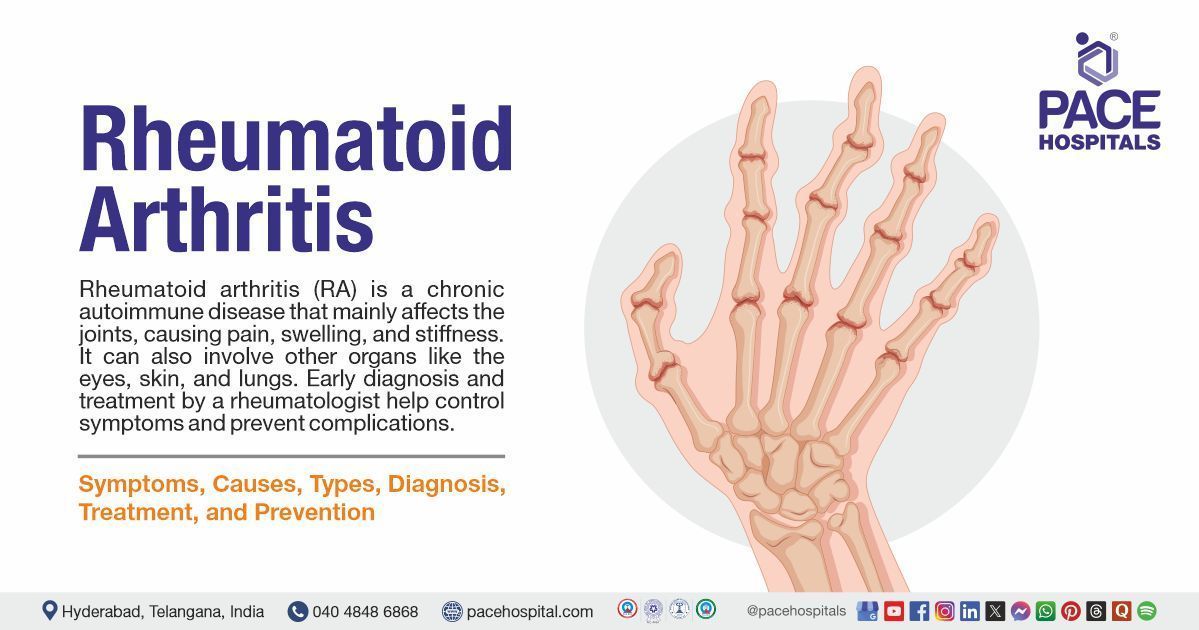
What is rheumatoid arthritis?
Rheumatoid arthritis (RA) is a chronic (long-lasting) autoimmune disease in which the immune system mistakenly (accidentally) targets the joints, resulting in inflammation, pain, and stiffness. It primarily affects the hands and feet, although it can also damage other joints and organs.
What are the symptoms of rheumatoid arthritis?
Joint pain, swelling, and stiffness are some common symptoms of rheumatoid arthritis (RA), particularly in the small joints of the hands and feet. The symptoms typically worsen in the morning or after periods of inactivity, and they are usually symmetrical. Low-grade fever, exhaustion, and inadvertent weight loss are among the symptoms that people with RA may have. Other organs may occasionally be affected by illness, which could result in complications such as involvement of the heart or lungs.
Can you get pregnant with rheumatoid arthritis?
Yes, women with RA can become pregnant and can have safe pregnancies, but it is essential to manage rheumatoid arthritis (RA) properly both before and throughout pregnancy. Some women may have flare-ups during pregnancy, while others may see improvements in their RA symptoms. Managing RA during pregnancy is challenging due to limited treatment options. However, some medications have been found to be safe, allowing for continued control of the disease.
Does rheumatoid arthritis show up on the X-ray?
X-rays can reveal rheumatoid arthritis (RA), because they are more helpful in tracking the disease's course than in diagnosing it early. Although RA is active in its early phases, X-rays may reveal no abnormalities. However, when the illness worsens, X-rays may reveal joint degeneration, including bone loss, narrowing of the joint space, and erosions.
How many types of rheumatoid arthritis are there?
Rheumatoid arthritis (RA) comes in three primary forms: juvenile idiopathic arthritis (JIA), seropositive RA, and seronegative RA. Whereas seronegative RA is diagnosed even in the absence of these antibodies, seropositive RA is identified by the presence of specific antibodies in the blood. The type of RA that affects youngsters is called JIA.
Is rheumatoid arthritis an autoimmune disorder?
Yes, rheumatoid arthritis (RA) is an autoimmune disease. In this instance, the body's immune system unintentionally targets its healthy tissues, mainly the joint lining. The impacted joints become inflamed, painful, and stiff because of this attack.
Can rheumatoid arthritis affect vision?
Rheumatoid arthritis (RA) can indeed impair vision, and it is an inflammatory condition that may cause inflammation in various parts of the body, including the eyes. With symptoms ranging from minor dryness to more serious difficulties, including vision loss, eye problems are common in patients with RA.
Can I live an everyday life with RA?
Yes, with proper treatment and support, many people with rheumatoid arthritis (RA) can live a relatively active life. Although RA can affect daily routines, modern medications and healthy lifestyle choices help manage symptoms and slow disease progression. Early diagnosis and consistent care are crucial to maintaining a high quality of life.
Can rheumatoid arthritis go away on its own?
No, Rheumatoid arthritis (RA) typically doesn't resolve on its own. Because it is chronic, it persists for a prolonged period. It is unlikely to be a lasting cure, although some patients may experience periods of remission during which their symptoms subside or disappear. To control symptoms, avoid joint damage, and maybe achieve remission, early and appropriate treatment is essential.