Arthroplasty Surgery Hospital in Hyderabad, India
PACE Hospitals is recognized as one of the best hospitals for arthroplasty (Joint replacement) in Hyderabad, Telangana, India. Our expert orthopedic team specializes in advanced arthroplasty procedures, including knee replacement, hip replacement, shoulder replacement, and ankle replacement surgeries. Using modern surgical techniques and cutting-edge technology, we treat conditions like osteoarthritis, rheumatoid arthritis, joint degeneration, and severe trauma with precision and care.
Book an Appointment for
Arthroplasty Surgery
Arthroplasty (Joint Replacement ) Online Appointment
Thank you for contacting us. We will get back to you as soon as possible. Kindly save these contact details in your contacts to receive calls and messages:-
Appointment Desk: 04048486868
WhatsApp: 8977889778
Regards,
PACE Hospitals
HITEC City and Madeenaguda
Hyderabad, Telangana, India.
Oops, there was an error sending your message. Please try again later. Kindly save these contact details in your contacts to receive calls and messages:-
Appointment Desk: 04048486868
WhatsApp: 8977889778
Regards,
PACE Hospitals
HITEC City and Madeenaguda
Hyderabad, Telangana, India.
Why Choose PACE Hospitals for Arthroplasty?
State-of-the-Art Operation Theatres & Advanced Diagnostic Imaging
Team of the Best Orthopedic and Arthroplasty Surgeons in Hyderabad
Post-surgery care tailored physiotherapy and rehabilitation
Affordable Arthroplasty Surgery Cost in Hyderabad with Insurance & Cashless Options
What is Arthroplasty Surgery?
Arthroplasty is a surgical technique that is used to replace a damaged joint with an artificial prosthesis composed of ceramic, plastic, or metal parts to restore its function. Patients with osteoarthritis, rheumatoid arthritis, osteonecrosis, or traumatic injuries who experience severe joint pain and disability are the primary candidates for this procedure, particularly if non-surgical measures like medication, physical therapy, or injections have not been effective. Orthopedic surgeons, specialists in musculoskeletal disorders, perform arthroplasty.
Arthroplasty meaning
"Arthroplasty" comes from the Greek words "arthro," which means joint, and "plasty," which means “molding” or “formation”. The idea of arthroplasty first appeared in the 19th century when surgeons were looking for alternatives to amputation for joint disease. Rather than removing the limb, early procedures used excision or interposition techniques to restore joint function. The word "arthroplasty" itself conveys the intention to reshape or reconstruct damaged joints, reflecting the evolution of the procedure from limb removal to reconstructive joint surgery.
Arthroplasty Types
There are several types of arthroplasty that are developed to the degree of joint involvement and patient-specific parameters to maximize clinical results and enhance quality of life. Below are the types of arthroplasty:
Total joint arthroplasty
Also known as total joint replacement, it involves using prosthetic components to replace both joint’s articular surfaces. Common examples include:
- Total knee arthroplasty (TKA): It includes the replacement of the knee's tibial and femoral components.
- Total hip arthroplasty (THA): It includes the replacement of both the femoral head and acetabulum.
- Total ankle arthroplasty: It includes the replacement of the distal tibia and talar surfaces.
- Total shoulder arthroplasty: It includes the replacement of the humeral head and the glenoid cavity.
Hemiarthroplasty (Partial joint replacement)
It is usually used when damage is restricted to one side of the joint, and only one particular surface is replaced. Common types include:
- Hip hemiarthroplasty: Replacing just the femoral head while keeping the acetabulum unchanged.
- Unipolar: There is movement between the solid prosthesis and the acetabulum.
- Bipolar: The prosthesis permits mobility within the prosthesis as well as at the acetabulum.
- Shoulder hemiarthroplasty: It includes only replacing the humeral head.
Resurfacing arthroplasty
- In order to preserve more native bone, the damaged joint surface is cut and covered with a smooth metal covering. It is usually done on the hip (hip resurfacing), but it can also be done on the knee and shoulder.
Resection arthroplasty
- It includes the removal of the joint surface without the use of prosthetic parts. For example, the girdlestone procedure, which is a hip resection arthroplasty, is usually performed as a salvage procedure.
Spinal disc arthroplasty
- To preserve motion at the spinal segment, a degenerated intervertebral disc is replaced with an artificial one.
Other joint replacements
- It is also possible to perform arthroplasty on less commonly used joints like elbow replacement, wrist replacement, and finger joint replacement.
Revision arthroplasty
- It is done when a previous arthroplasty fails because of loosening, infection, or wear and needs replacement or repair of the prosthetic components.
Arthroplasty Indications
The main indications for arthroplasty are end-stage joint damage that, generally resulting from the failure of conservative treatments, leading to severe pain, reduced quality of life, and functional impairment. The key indications of arthroplasty include the following:
- Severe joint pain and functional limitation: Even with the best conservative treatment (e.g., medications, physical therapy, activity modification), persistent joint pain, stiffness, and loss of function substantially reduce everyday activities and quality of life.
- Advanced joint disease: The most common indication is osteoarthritis, particularly in the knee and hip. When they cause severe joint damage and symptoms, other types of arthritis (like rheumatoid arthritis and post-traumatic arthritis) may also require arthroplasty.
- Joint deformity and instability: Significant joint instability, deformity, or misalignment that is not manageable or correctable with less invasive techniques.
- Failure of conservative treatments: When non-surgical options (medication, injections, physical therapy, assistive devices) fail to provide sufficient relief, arthroplasty is considered.
- Fractures involving the joint: Joint replacement is preferable to internal fixation for the treatment of some fractures, particularly displaced femoral neck fractures in older adults.
- Loss of joint mobility: Marked restriction of range of motion that impacts essential functions and independence.
- Other indications: Joint replacement may be necessary in certain cases of avascular necrosis (osteonecrosis), congenital or developmental joint disorders, and unsuccessful prior joint surgeries (revision arthroplasty).
Arthroplasty Contraindications
Before proceeding with surgery, several absolute and relative contraindications to arthroplasty must be taken into consideration. Understanding these contraindications lowers the chance of complications during and after surgery. They include the following:
Absolute contraindications
- Active local or systemic infection: The high risk of prosthetic infection makes it absolutely contraindicated for ongoing infections in the joint (septic arthritis), surrounding tissues (cellulitis), or distant sites (bacteremia or sepsis).
- Active deep vein thrombosis (DVT) or pulmonary embolism (PE): Surgery may dislodge thrombi and result in potentially fatal complications. Hence, it needs to be delayed until acute DVT or PE is treated, and the patient is stabilized.
- Uncontrolled medical comorbidities: Severe medical conditions that prevent anesthesia or surgery, like end-stage renal disease that necessitates hemodialysis, severe chronic obstructive pulmonary disease, advanced liver cirrhosis (Child-Pugh C), or decompensated heart failure.
- Untreated immunodeficiency: Untreated immunodeficiencies, such as uncontrolled HIV (CD4+ count <200), are absolute contraindications because they greatly increase the risk of infection.
- Severe malnutrition or uncontrolled diabetes: Before surgery, severe malnutrition (serum albumin <3 g/dL, transferrin <200 mg/dL) and uncontrolled diabetes (HbA1c >8%) must be treated because they increase the risk of infection and poor wound healing.
- Severe peripheral vascular disease: Safe surgery is not possible due to advanced vascular compromise in the affected limb.
Relative contraindications
- Poor bone quality: Although recent research indicates osteoporosis is not always an absolute contraindication, particularly with cemented implants, severe osteoporosis or poor bone stock may make implant fixation more difficult.
- Morbid obesity: Higher BMIs, particularly those over 50, are related to a higher risk of implant failure and complications; obesity is listed as a contraindication by some implant manufacturers, though this is not always the case and needs to be individualized for each patient.
- Previous joint infection: A history of infection in the surgical joint raises the chance of recurrence and necessitates careful assessment and risk-benefit analysis.
- Severe neurological or muscular disorders: Successful outcomes may be prevented by conditions that affect joint stability or rehabilitation potential, such as Charcot arthropathy or severe neuromuscular disease.
- Lack of surgical expertise or inadequate facilities: Lack of surgical experience or lack of ability to carry out required concurrent procedures are relative contraindications for certain procedures (such as patellofemoral arthroplasty).
Other considerations
- Patient non-compliance or unrealistic expectations: Patients with high expectations or those who are unable or unwilling to follow postoperative rehabilitation guidelines may not be good candidates for arthroplasty.
Arthroplasty Benefits
Numerous studies have shown how arthroplasty improves mobility, pain management, and overall quality of life. The main advantages of arthroplasty are as follows:
- Pain relief: Significant pain relief is the main advantage of arthroplasty, or joint replacement surgery, particularly for patients with osteoarthritis.
- Improved functional activity and mobility: Patients can regain mobility and participate in every day and recreational activities after having an arthroplasty, which increases functional activity. Several months following surgery, there will be a noticeable improvement in walking speed and overall gait function.
- Enhanced quality of life: After having an arthroplasty, patients report better quality of life because they can carry out daily tasks more independently and with less discomfort.
- Reduction in anxiety and psychological distress: After surgery, anxiety levels are considerably decreased, which usually improves psychological health.
- Decreased need for assistance: Following surgery, patients become more independent as they need less assistance with everyday tasks.
- Early rehabilitation and shorter hospital stay: Modern methods and procedures, such as clinical care pathways and anterior approach hip arthroplasty, are related to early rehabilitation, less pain, and shorter hospital stays.
- Cost-effectiveness: Over the course of the patient's life, total hip and knee replacements are very cost-effective surgeries that offer significant health benefits in comparison to their expenses.
- Patient safety and optimized care: When multidisciplinary care pathways are used for arthroplasty, patient safety is increased, care is standardized, and complications like unnecessary ICU stays and blood transfusions are reduced.
Arthroplasty Steps
Arthroscopy procedure steps include the following:
Before the procedure
- In addition to a thorough medical history, the doctor usually performs a complete physical examination to ensure patients' good health before going through the surgical procedure, which may include blood tests or additional diagnostic tests.
- The patients will have to do a signature on a consent form authorizing the doctors to perform the surgery. Patients should carefully read the form; if there are any questions, they can ask the doctors.
- Patients need to inform the doctor if they are sensitive to or allergic to any medications, tape, latex, or anesthetic agents (local and general).
- Patients need to inform the doctor about every medication (prescription and over the counter) and herbal supplements they are taking.
- Patients must inform their doctor if they have a history of bleeding disorders or are using any anticoagulant (blood-thinning) medications, aspirin, or other blood-clotting inhibitors. Certain medications may be required to be discontinued prior to the surgery.
- Patients who are pregnant or suspect they are pregnant need to inform their doctor.
- Patients are informed not to drink or eat anything from the night before their procedure.
- Patients need to look and arrange for someone to assist them around the house for a week or two once they are discharged from the hospital.
During the procedure
- Arthroscopy surgery is usually performed while patients are asleep under general anesthesia. The anesthesiologist will discuss this with the patients earlier.
- Patients will be asked to take off their garments and provided a gown to wear.
- An intravenous (IV) line can be started in the patient's arm or hand.
- Patients are positioned on the operating table, and a urinary catheter is inserted.
- In case of excessive hair at the surgical site, it may be trimmed.
- The anaesthesiologist will monitor the blood pressure, heart rate, and other vital signs during the procedure.
- The skin around the surgical site will be cleaned with an antiseptic solution.
- The surgeon will create an incision in the joint area.
- The surgeon will remove the damaged surfaces of the joint and resurface it with the prosthesis. The prosthesis is composed of metal and plastic. The most common type of artificial prosthesis is the cemented prosthesis. Uncemented prostheses are no longer routinely used. A cemented prosthesis is secured to the bone with surgical cement. An uncemented prosthesis has a porous surface that allows the bone to develop and connect to the prosthesis. Sometimes, both types are used to replace a knee.
- The incision will be closed using stitches or surgical staples.
- A drain may be inserted into the incision site to remove fluid. A sterile bandage or dressing will be done.
After the procedure
- Following surgery, patients will be brought to the recovery room for observation. Patients will be moved to their hospital room once their blood pressure, pulse, and respiration have stabilized, and they are alert. A few days’ stay in the hospital is normally required for arthroscopy surgery.
- Following surgery, it is essential to start moving the new joint. A physical therapist will visit with patients shortly after surgery to plan an exercise program for them.
- Physical therapy may begin with the use of a continuous passive motion (CPM) machine. While patients are lying in bed, this machine moves the new joint through its full range of motion.
- Pain will be managed with medicines so that patients can participate in the activity. Patients will be provided with an exercise schedule to follow while in the hospital and after discharge.
- Patients will be discharged and sent home or to a rehabilitation facility. In any instance, the doctor will arrange for continued physical therapy until patients regain muscular strength and range of motion.
Arthroplasty Complications
Like any major surgical procedure, arthroplasty has a risk of complications that can impact long-term results as well as short-term recovery. Following are some of the complications of the arthroplasty procedure:
- Infection: There is a considerable risk of postoperative infection, which includes deep periprosthetic joint infection as well as superficial wound infection. Infection is more prevalent in some populations, such as those with rheumatoid arthritis, and may necessitate revision surgery or long-term antibiotics.
- Venous thromboembolism (VTE): The most common systemic medical complication following arthroplasty is venous thromboembolism, which includes pulmonary embolism and deep vein thrombosis. This risk is increased by pre-existing comorbidities, which can be life-threatening if not detected and treated immediately.
- Dislocation: One significant complication is joint dislocation, particularly following total hip replacement. It causes discomfort and instability and frequently necessitates reduction or additional surgery. Patients with rheumatoid arthritis and those with spinal disorders that impair alignment are at a higher risk.
- Periprosthetic fracture: During or after surgery, fractures may occur around the implant. These fractures are linked to higher morbidity and may necessitate revision arthroplasty or additional fixation.
- Implant loosening or failure: Over time, aseptic loosening and mechanical failure of the prosthesis may occur. This may result in discomfort, diminished functionality, and the need for revision surgery.
- Wound complications: After the arthroplasty procedure, there have been reports of wound infection, wound dehiscence, and delayed wound healing. These issues may require additional care and lengthen hospital stays.
- Nerve or vascular injury: During surgery, damage to the blood vessels or nerves may cause haematoma formation, bleeding, or sensory or motor impairments. These are less frequent but potentially dangerous side effects.
- Joint stiffness: After surgery, joint stiffness or decreased range of motion may occur. The function may be limited, and additional procedures, like manipulation under anaesthesia, may occasionally be necessary.
- Revision surgery: Infection, dislocation, or mechanical failure may necessitate an early revision. Compared to primary procedures, revision surgeries are riskier and more complicated.
Arthroplasty Recovery
During the first six weeks following an arthroplasty, most patients report improved function and less pain than they did prior to surgery. Recovery is characterized by a progressive decrease in pain and an improvement in function and quality of life. Although the intensity and schedule can vary, early mobilization and physical therapy are essential. Most of the patients can resume their regular activities, including driving and working, in six weeks, and they frequently need fewer assistive devices and pain relievers. By six to eight months after surgery, full recovery of physical functioning usually reaches about 80% of that of healthy individuals.
Questions that the patients can ask the healthcare team about arthroplasty?
- When can I go home?
- When do I need to see my doctor again?
- What kind of pain can I expect?
- When can I go back to my regular activities?
- What is the expected recovery time?
- What precautions should I take?
- What problems can occur after arthroplasty surgery?
- Will I require physical therapy after surgery, and for how long?
- How do I expect my knee to look over time?
- How long will my recovery take, and what kind of assistance will I require throughout that time?
- Are there any specific exercises I should avoid while recovering?
- Do I need any further treatment?
Difference between Arthrodesis and Arthroplasty
Arthrodesis vs arthroplasty
Two different surgical techniques, arthroplasty, and arthrodesis, are used to treat severe joint pathology, especially when there is advanced arthritis, deformity, or instability. Numerous factors, such as the joint involved, the patient's level of activity, and the desired functional outcome, affect the choice between these procedures. Below are the parameters that help in differentiating arthrodesis and arthroplasty:
| Parameters | Arthrodesis | Arthroplasty |
|---|---|---|
| Definition | It is defined as the surgical fusion of a joint, eliminating all the movement. | It is defined as surgically replacing or reconstructing a joint to maintain or restore motion. |
| Common indications | Severe pain, deformity (often in small joints: ankle, thumb, wrist, foot) or instability. | Joint damage (commonly in large joints: knee, hip, sometimes ankle/wrist) or advanced arthritis |
| Procedure | Joint cartilage is removed, and bones are fixed until fusion takes place. | Damaged joint surfaces are removed, and prosthetic parts are positioned. |
| Goal | Eliminating motion relieves pain and stabilizes joints. | Reduction of pain while preserving or regaining joint mobility. |
| Function | It may restrict joint-moving activities, usually recommended for small or low-demand joints. | Better functional results for high-demand joints (knee, hip); more activities can be started again. |
| Mobility outcome | Loss of movement at the fused joint; nearby joints may experience compensatory motion. | Improves function in day-to-day activities by maintaining or restoring joint movement. |
| Long-term outcomes | Long-lasting pain relief, but at the expense of joint mobility, arthritis may develop in nearby joints. | Good function and pain relief; the risk of prosthesis wear or loosening over time. |
Difference between Shoulder Arthroscopy and Arthroplasty
Shoulder Arthroscopy vs Arthroplasty
The functions of shoulder arthroscopy and arthroplasty in the treatment of shoulder pathology are distinct. In comparison with arthroplasty, arthroscopy is a minimally invasive procedure that is frequently used for rotator cuff repair, treatment of impingement, and for diagnostic purposes. It offers significant improvements in pain and function, even in elderly patients, and is less expensive and requires a quicker recovery.
Although arthroplasty, which includes anatomic and reverse total shoulder replacement, offers dependable pain relief and functional improvements, it is usually saved for patients with advanced joint diseases like severe osteoarthritis or irreparable rotator cuff tears. However, it is more invasive and has a higher risk of complications.
Comparative studies show that arthroplasty is preferred for patients with advanced degenerative changes or to those whose previous repairs have failed, while arthroscopic rotator cuff repair is typically more cost-effective and should be considered first when feasible.
Arthroplasty Cost in Hyderabad, Telangana, India
The cost of arthroplasty (joint replacement surgery) in Hyderabad generally ranges from ₹1,10,000 to ₹3,50,000 and above (approximately US $1,325 – US $4,215).
The exact price depends on factors such as the type of joint being replaced (knee, hip, shoulder), the extent of joint damage, implant type (standard or premium), surgical technique (conventional or minimally invasive), surgeon experience, hospital infrastructure, and availability of cashless insurance, TPA corporate tie-ups, and medical insurance support wherever applicable.
Cost Breakdown According to Type of Arthroplasty Surgery
- Total Knee Replacement (Single Knee) – ₹1,10,000 – ₹2,00,000 (US $1,325 – US $2,410)
- Total Knee Replacement (Both Knees) – ₹2,20,000 – ₹3,50,000 (US $2,650 – US $4,215)
- Partial Knee Replacement / Unicondylar Knee Replacement – ₹1,20,000 – ₹2,20,000 (US $1,445 – US $2,650)
- Hip Arthroplasty – Total Hip Replacement /Total Hip Arthroplasty – ₹1,50,000 – ₹3,00,000 (US $1,805 – US $3,610)
- Hemiarthroplasty (Half Hip Replacement) – ₹1,20,000 – ₹2,00,000 (US $1,445 – US $2,410)
- Shoulder Arthroplasty (Total Shoulder Replacement) – ₹1,50,000 – ₹3,00,000 (US $1,805 – US $3,610)
- Reverse Shoulder Arthroplasty – ₹2,00,000 – ₹3,50,000 (US $2,410 – US $4,215)
Frequently Asked Questions (FAQs) on Arthroplasty
What is total joint arthroplasty?
Total joint arthroplasty is a surgical procedure that involves replacing all the surfaces of an arthritic or damaged joint with prostheses to decrease pain and restore function. The most often replaced joints in this procedure are the hip and knee.
Which Is the best hospital for Arthroplasty in Hyderabad, Telangana, India?
PACE Hospitals, Hyderabad, is recognised as one of the leading centres for arthroplasty and advanced joint reconstruction.
We deal complicated cases guided by expert orthopaedic and joint replacement surgeons by using modern techniques such as minimally invasive approaches, computer-assisted alignment, and advanced prosthetic implants for long-lasting joint function.
We are equipped with highly advanced state-of-the-art operation theatres, infection-controlled environments, dedicated physiotherapy units, and comprehensive post-operative rehabilitation programs, PACE Hospitals provides safe, precise, and highly successful arthroplasty outcomes.
Patients also benefit from cashless insurance, TPA tie-ups, and full assistance for medical insurance documentation.
How long do artificial joints typically last?
Although longevity varies depending on the patient's weight, activity level, and implant type, modern joint implants typically last 15 to 20 years or longer. Durability is continuously increased by developments in implant materials and surgical methods.
Are there activity restrictions after arthroplasty?
High-impact sports and activities that could strain the joint or cause dislocation should be avoided, especially in the early postoperative phase, but patients are encouraged to return to low-impact activities like walking, cycling, or swimming.
What joints can be treated with arthroplasty?
Depending on the patient's requirements and the degree of joint damage, the hip, knee, shoulder, ankle, and occasionally smaller joints like the wrist or spine are replaced.
How successful is arthroplasty in the long term?
In the long run, arthroplasty is very successful; total hip and knee replacements have prosthesis survival rates of over 94% at 10 years and roughly 92–94% at 25–30 years. After a total knee replacement, the majority of patients report long-lasting pain relief and function improvement, with a revision rate of less than 5% within ten years. Although some procedures, such as patellofemoral arthroplasty, have lower 10-year survival rates (roughly 76%), major joint arthroplasty generally provides patients with long-lasting results.
What Is the cost of Arthroplasty in Hyderabad, Telangana, India?
At PACE Hospitals, the cost of arthroplasty typically ranges from ₹1,10,000 to ₹3,20,000 and above (approximately US $1,325 – US $3,855), depending on:
- Joint involved (knee, hip, shoulder)
- Type of replacement (total, partial, reverse, or hemiarthroplasty)
- Implant material and brand (standard, high-flex, ceramic, titanium, etc.)
- Complexity of joint damage or deformity
- Duration of hospital stay and rehabilitation needs
- Surgeon expertise and advanced technology used
Basic joint replacement procedures fall at the lower end of the range, while complex reconstructions needing premium implants or advanced techniques fall toward the higher end.
After clinical assessment, imaging (X-ray/MRI/CT), and pre-operative evaluation, our orthopaedic team provides a personalised surgery plan along with an accurate cost estimate based on your condition and treatment requirements.
What is excision arthroplasty?
In an excision arthroplasty, sometimes referred to as a resection arthroplasty, a joint is surgically removed entirely or in part, with no artificial implant placed. Scar tissue fills the empty space, allowing for some mobility and pain relief. When alternative reconstructive procedures are not feasible, this technique is frequently employed as a salvage option for severe joint infections or failed joint replacements.
What is reverse shoulder arthroplasty?
Reverse shoulder arthroplasty is a surgical procedure in which the normal ball-and-socket structure of the shoulder joint is inverted. A concave "socket" is positioned on the humerus (upper arm bone), and a convex "ball" is attached to the glenoid (shoulder blade). This design improves shoulder function and lessens pain in patients with severe rotator cuff injuries or arthropathy by allowing the deltoid muscle to compensate for a deficient or torn rotator cuff.
Can a person do heavy walking after ankle arthroplasty?
Most patients who have had ankle arthroplasty can resume regular walking and low-impact activities after their rehabilitation is finished, which usually happens three to six months after the procedure. However, to prolong the implant's lifespan and avoid complications, heavy walking, and high-impact, repetitive activities are typically discouraged. Running and tasks that repeatedly put a lot of strain on the ankle joint need to be avoided.
What is the role of rehabilitation after arthroplasty?
Rehabilitation is necessary to regain range of motion, strength, and flexibility. Functional outcomes are greatly enhanced, and complications are decreased with early and structured physical therapy that involves muscle activation and balance exercises.
Is it normal to experience pain after arthroplasty, and how is it managed?
Early postoperative pain and discomfort are to be expected, but they are typically effectively managed with medicine, ice, and physical therapy. Severe or chronic pain needs to be assessed for possible complications.
Do all patients experience the same level of improvement after arthroplasty?
Although the majority of patients experience notable reductions in pain and enhanced functionality, results may differ. Even patients with less favorable profiles generally report better quality of life after surgery. However, factors like obesity, bilateral versus unilateral procedures, and pre-existing comorbidities may influence the extent of improvement.
Is arthroplasty a major or minor surgery?
Because arthroplasty, including total joint replacement, involves invasive orthopedic procedures, necessitates spinal or general anesthesia, and significantly modifies normal anatomy, it is categorized as major surgery. Hip, knee, ankle, and shoulder arthroplasty are among the most frequently performed major surgical procedures.
What is the difference between arthroplasty and replacement?
The surgical replacement of a joint with an artificial material is known as arthroplasty, and the terms "arthroplasty" and "joint replacement" are used interchangeably in the medical literature. Whereas partial arthroplasty only replaces a portion of the joint, total arthroplasty replaces all joint surfaces.
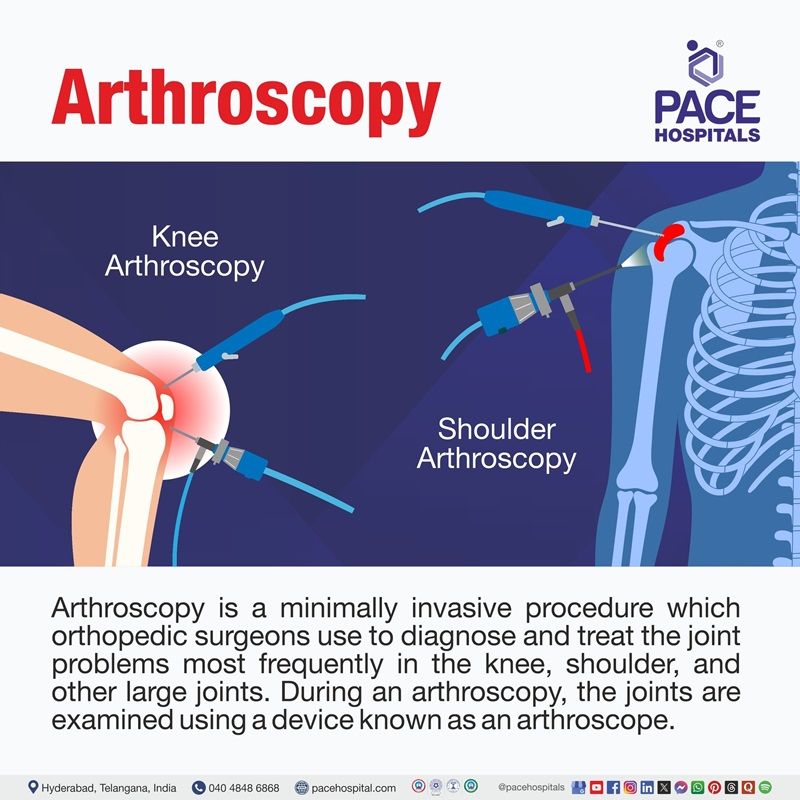
What is the difference between arthroscopy and arthroplasty?
While arthroplasty is an open surgical procedure that replaces or reconstructs the joint to restore function and alleviate pain, arthroscopy is a minimally invasive surgical procedure that uses a small camera and instruments to diagnose and treat joint problems without replacing the joint. Whereas arthroplasty includes the implantation of prosthetic components, arthroscopy maintains the original joint.




