Osteoarthritis: Symptoms, Types, Causes, Risk Factors, Complications
Pace Hospitals
Osteoarthritis definition
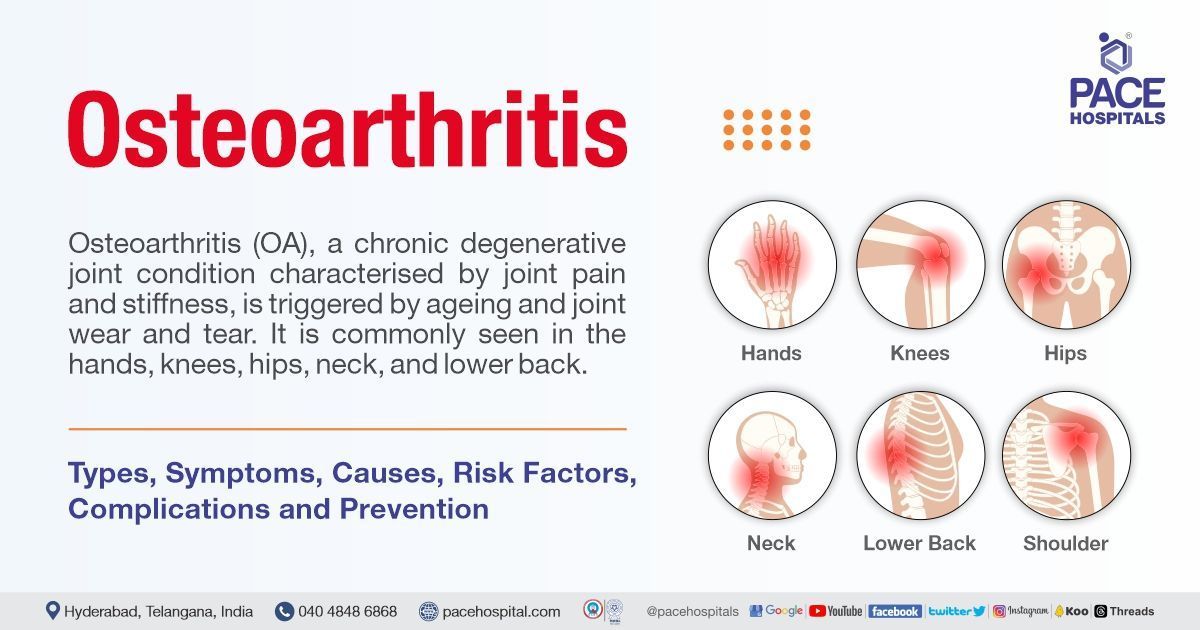
Osteoarthritis (OA), well-known as degenerative joint disease, is a common form of arthritis that damages the tissue surrounding the joint. This condition, commonly characterised by joint pain and stiffness, is triggered due to ageing and joint wear and tear.
What is osteoarthritis?
Osteoarthritis meaning
Osteoarthritis (OA) is a long-lasting joint condition that primarily occurs when the cartilage wears and tears away, which in turn causes the bones within the joint to rub together. The cartilage acts as a cushion and protects the ends of the bones. Osteoarthritis is commonly seen in older people. Clinical features of osteoarthritis include joint pain, stiffness, swelling, and loss of mobility.
Osteoarthritis is commonly seen in the hands, knees, hips, neck, and lower back. There is no permanent cure for osteoarthritis except pain management, physical exercises, and lifestyle modifications.
Global incidence of osteoarthritis
About 3.3 to 3.6% of people worldwide suffer from OA. It ranks as the 11th most disabling disease in the world, causing moderate to severe disability in 4.3 crore individuals. 60% of those with osteoarthritis are female, and 73% are older than 55. Of those, 60% are thought to be symptomatic. Around the world, 24 crore adults are thought to suffer from osteoarthritis symptoms. It affects females more often than males.
There were 52.8 crore osteoarthritis sufferers worldwide in 2019, an increase of 113% since 1990. The knee is the frequently affected joint, with a prevalence of 365 million, followed by the hip and the hand. Osteoarthritis affects 34.4 crore people, with severity levels (moderate or severe) that could benefit from rehabilitation.
Prevalence of osteoarthritis in India
With the prevalence of 22% to 39% in India, osteoarthritis is the most common joint disease and the second most prevalent rheumatology condition. Women are more likely than men to have OA; however, as people get older, the risk rises significantly. In India, the number of people with OA grew from about 2.3 crore in 1990 to 6.2 crore in 2019.
Types of osteoarthritis
Osteoarthritis is commonly of two types:
- Primary osteoarthritis
- Secondary osteoarthritis
Primary osteoarthritis: Primary osteoarthritis is the most common type of osteoarthritis associated with age, obesity, anatomical factors, female gender, and muscle weakness. It is a generalised arthritis that especially occurs in the fingers, hips, knees, toes, thumbs, and spine.
Secondary osteoarthritis: Secondary arthritis is associated with a pre-existing abnormality. It can be seen in younger people. The conditions that trigger this type include congenital joint disorders, injury or trauma, infectious arthritis, inflammatory arthritis, metabolic disorders, osteoporosis, hemoglobinopathy, Ehlers-Danlos syndrome, and more.
Osteoarthritis classification
The sites where osteoarthritis tends to occur are as follows:
- Knees (osteoarthritis knee or knee osteoarthritis)
- Hands (osteoarthritis hands)
- Hips (osteoarthritis hip)
- Neck (cervical osteoarthritis)
- Lower back (osteoarthritis of the spine or lumbar osteoarthritis)
Osteoarthritis grading
There are four stages of osteoarthritis:
- Stage 0 (normal): The knee joint doesn't show any symptoms in this stage. Henceforth, no treatment is required.
- Stage 1 (minor): Minor spurs and bony growths are often seen in this stage. This stage doesn't show any pain or discomfort. Patients are advised to do exercises going forward.
- Stage 2 (mild): In this stage, individuals experience minor pain and stiffness. Henceforth, different therapies are suggested to treat the pain, stiffness, and tenderness.
- Stage 3 (moderate): In this stage, the cartilage is damaged, and the individual shows frequent pain when walking, running, or bending. In addition to this, joint swelling and stiffness are also seen. Henceforth, patients are suggested for corticosteroid injections and pain relievers with different supportive therapies.
- Stage 4 (severe): In this stage, the individual experiences severe pain and major symptoms. The cartilage is completely damaged due to a lack of synovial fluid. Henceforth, the patient is suggested for osteoarthritis surgery.
Osteoarthritis symptoms
Osteoarthritis signs and symptoms are as follows:
- Joint pain
- Stiffness that lasts less than 30 minutes in the morning or after relaxation
- Limitation of movement
- Muscle weakness
- Balance-related problems (joint instability)
- Swelling or inflammation around the joints
- Joint deformities that could decrease the range of movements
- Popping or clicking sounds on the movement of joints
- Tenderness or discomfort upon touch at the affected site, and more
Osteoarthritis causes
The etiology of osteoarthritis includes:
- Being overweight
- Repetitive or overuse of the joints
- Trauma or injuries to the joints, ligaments, or cartilage
- Joint abnormalities or malformations
- Poor posture
- Sporting activities or jobs involve lifting, climbing, or twisting of the joints for longer periods
- Wear and tear of cartilage due to ageing
- Bone sours and infections to the joints, etc.
Osteoarthritis risk factors
The risk factors for osteoarthritis are as follows:
- Ageing: Age-related loss in the body's cells and tissue's capacity to maintain homeostasis, particularly under stress, is the cause of many conditions, including osteoarthritis (OA). Unusual or excessive mechanical stresses contribute to the development of OA.
- Female gender: A higher production of bone-eroding cells is correlated with decreasing oestrogen levels, which can result from menopause. In addition to this, exosomes generated from synovial fluid have a significant impact on the pathogenesis of OA. These differently expressed female miRNAs may also be oestrogen-responsive and participate in TLR [toll-like receptor] signalling during the development of OA.
- Obesity: Obesity-related joint overloading, which results in the degeneration of articular cartilage, had been assumed to be the primary cause of OA.
- Anatomical factors: Anatomical factors such as bone and joint deformities could cause osteoarthritis.
- Muscle weakness: A gradual decrease in peri articular muscle mass and function impacts joint stability and health. Ageing is irreversibly accompanied by muscle wasting, which is more recently been shown in OA patients.
- Predisposing or pre-existing abnormalities: Abnormalities such as infectious arthritis, congenital joint disorders, osteopetrosis, inflammatory arthritis, avascular necrosis, osteochondritis dissecans, Paget disease, hemoglobinopathy, Ehlers-Danlos syndrome, or Marfan syndrome increase the risk of osteoarthritis.
- Injury or fractures or overuse (occupation/sports activities/trauma): Following a cartilage injury, the collagen matrix gets damaged, which prompts chondrocytes to multiply and organise into clusters. As a result of a phenotypic transition to hypertrophic chondrocytes, cartilage growths ossify and develop into osteophytes. More collagen matrix damage causes chondrocytes to apoptosis, thus leading to osteoarthritis.
- Genetics: Variations in genes such as cartilage extracellular matrix structural genes (COL2A1 genes), bone density genes, chondrocyte cell signalling genes (FRZB genes), and inflammatory cytokine genes (IL-1R1 genes) increase the risk of osteoarthritis.
- Musculoskeletal abnormalities: Musculoskeletal conditions that affect joints, bones, and muscles, such as osteoporosis, sarcopenia, etc., increase the risk of osteoarthritis.
- Metabolic disorders: Metabolic disorders such as hemochromatosis and Wilson's disease trigger the risk of osteoarthritis.
Complications of osteoarthritis
Osteoarthritis complications are as follows:
- Sleep disturbances: Caused due to the pain.
- Reduced ability: Decreased ability to perform the activities.
- Increased body weight: Weight gain due to a lack of interest in physical exercise participation. This might lead to heart disease, hypertension and diabetes.
- Depression and anxiety: The osteoarthritis symptoms directly negatively affect the individual's mental health, resulting in depression and anxiety.
In addition to this, some more complications might arise due to osteoarthritis, including:
- Deterioration of ligaments and tendons.
- Bleeding or infections at the affected site.
- Osteonecrosis (bone death).
- Stress fractures.
- Pinched (compressed) nerves.
- Problems with walking.
- Distorted joint.
- Restricted joint range of motion.
- Radiculopathies (injury or damage to the nerve roots), etc.
Osteoarthritis diagnosis
The osteoarthritis investigations include:
- Thorough history taking and physical examination.
- Blood tests
- CBC (complete blood count)
- ESR (erythrocyte sedimentation rate)
- Rheumatoid factor
- ANA (anti-nuclear antibody)
- WBC (white blood cell count)
- X-Ray
- Joint aspiration
- Ultrasound
- MRI scan (magnetic resonance imaging)
Osteoarthritis treatment
Management of osteoarthritis includes several approaches, such as:
- Medical management of osteoarthritis (osteoarthritis medications)
- NSAIDs (non-steroidal anti-inflammatory medications)
- Intra articular corticosteroid injections
- Dietary and vitamin supplements
- Anti-depressants
- Topical pain relievers, etc.
- Physical therapy (physiotherapy for osteoarthritis)
- Assistive or supportive management
- Specially designed footwear or insoles
- Crutches or Canes or sticks
- Leg braces (knee brace for osteoarthritis)
- Splints
- Supportive dressings
- Orthotics, etc.
- Weight loss exercises, exercises for osteoarthritis (osteoarthritis knee exercises), yoga, and heat therapy
- Electric nerve stimulation
- Creative visualisation to relieve stress and depression
- Surgical management of osteoarthritis
- Arthroscopic surgery
- Osteotomy
- Joint fusion (arthrodesis)
- Joint replacement surgery (arthroplasty or total joint replacement)
Osteoarthritis prevention
The following modifiable factors can prevent osteoarthritis:
- Being physically active
- Maintaining a healthy weight
- Protecting the joints from injuries due to repetitive use, overuse, or trauma
- Managing blood sugar levels
- Choosing a healthy lifestyle
- Taking a balanced diet that is rich in healthy fats and vitamin D
- Taking supplements for vitamin-D deficiency
- Maintaining good posture
- Reducing the workload on the joints, etc.
Osteoarthritis vs rheumatoid arthritis | Difference between osteoarthritis and rheumatoid arthritis
Osteoarthritis is the degenerative joint disease characterised by wear and tear of cartilage, whereas rheumatoid arthritis is an autoimmune disorder that affects the whole body.
| Parameters | Osteoarthritis | Rheumatoid arthritis |
|---|---|---|
| Age | Usually seen in older adults> 40 years of age | Commonly seen in people around the age of 20 years |
| Causes | Ageing, obesity and some external factors that raise pressure on the joints | The exact cause is not known |
| Site of occurrence | Knee, hips, spine, neck, and hands | Hands, feet, eyes, lungs, heart, hips, elbows, knees, and feet |
| level of severity | Worsen gradually | Worsen within a few weeks from onset |
| Inflammation | It is a secondary symptom | It is a primary symptom |
| Morning stiffness | Less than one hour | More than one hour |
| Involvement | Monoarticular disease | Polyarticular disease |
| Laboratory findings | ESR, CPR, and anti-CCP are elevated | No such elevations |
| Immunotherapy | Not required | Required |
Osteoporosis vs osteoarthritis | Difference between osteoporosis and osteoarthritis
Osteoarthritis is a degenerative joint disease characterised by wear and tear of cartilage, whereas osteoporosis is a condition where the bone tissue breaks due to low bone density.
| Parameters | Osteoporosis | Osteoarthritis |
|---|---|---|
| Characterisation | Characterised by brittleness and weakness of bones due to low bone mass | Characterised by inflammation and deterioration of the joints |
| Risk factors | Age, sex, hormonal disorders, low BMI, genetics, smoking, alcohol consumption | Age, sex, injuries, genetics, overuse of the joints, obesity, metabolic disorders, and bone deformities |
| Signs and symptoms | Stooped posture, back pain, compression fractures, etc. | Joint pain, tenderness, stiffness, and inflammation |
| Treatment | Bisphosphonates, hormonal therapy and lifestyle modifications | NSAIDs, pain relievers, supportive therapies, osteotomy, arthroscopy and joint replacement |
| Involvement | Affects all the bones | Affects the weight-bearing bones |
| Site of occurrence | Hip, joint and spine | Knee, hips, spine, neck, and hands |
| Nature | It can be entirely prevented | Some types can’t be prevented |
Share on
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868
Appointment request - health articles
Recent Articles