Dysphagia Treatment | Diagnosis & Cost
PACE Hospitals is the best hospital for dysphagia treatment in Hyderabad, India, offering advanced care for swallowing difficulties. Our experts manage esophageal dysphagia using diagnostics like endoscopy and manometry, with treatments ranging from dietary guidance and therapy to medications and minimally invasive procedures, ensuring safe swallowing and improved quality of life.
Book an Appointment for Dysphagia Treatment
Dysphagia Treatment Online Appointment
Thank you for contacting us. We will get back to you as soon as possible. Kindly save these contact details in your contacts to receive calls and messages:-
Appointment Desk: 04048486868
WhatsApp: 8977889778
Regards,
PACE Hospitals
HITEC City and Madeenaguda
Hyderabad, Telangana, India.
Oops, there was an error sending your message. Please try again later. Kindly save these contact details in your contacts to receive calls and messages:-
Appointment Desk: 04048486868
WhatsApp: 8977889778
Regards,
PACE Hospitals
HITEC City and Madeenaguda
Hyderabad, Telangana, India.
Why Choose PACE Hospitals for Dysphagia Treatment?

Advanced Diagnostic Facilities: Endoscopy, High-Resolution Manometry, pH Monitoring & Biopsy for accurate Esophagitis detection
Expert Gastroenterologist in Hyderabad dedicated to comprehensive dysphagia care
Minimally invasive approaches for severe Esophagitis treatment, including endoscopic therapy, laparoscopic surgery, balloon dilation, radiofrequency ablation
Affordable & Transparent Esophagitis Treatment at PACE Hospitals with Insurance & Cashless Options
Dysphagia Diagnosis
Diagnosis of dysphagia depends on factors such as the patient's medical history, presenting symptoms, and physical examination, which help the gastroenterologist to diagnose and treat esophageal dysphagia. Neurologists or ENT specialists may be involved in diagnosing and treating oropharyngeal dysphagia. Speech-language pathologists (SLPs) play a crucial role in assessing and treating swallowing disorders. These specialists consider the following before selecting the appropriate diagnostic tests for dysphagia.
- Medical history
- Physical examination
Medical history
When evaluating a patient for dysphagia, the medical history focuses on the onset, duration, and progression of swallowing difficulties, as well as whether the problem occurs with solids, liquids, or both. Gastroenterologists ask about associated dysphagia symptoms such as coughing, choking, nasal regurgitation, voice changes, weight loss, and recurrent chest infections, which may indicate aspiration or underlying disease.
A thorough review of past medical history is essential, particularly for neurological conditions like stroke, Parkinson’s disease, or dementia, as well as any history of head and neck cancer, surgery, or radiation. Medication use is reviewed, especially drugs that can cause dry mouth or sedation. Lifestyle factors, such as smoking, alcohol consumption, and dietary habits, are also relevant, along with any family history of neurological or gastrointestinal disorders, as these may increase the risk or contribute to the underlying cause of dysphagia.
Physical examination
The physical examination for diagnosing dysphagia includes a careful check of the mouth, neck, larynx, and oropharynx. It also involves a neurological exam to identify the cause of swallowing difficulty. Also, assessment of the patient’s general appearance and nutritional status, looking for signs of weight loss or dehydration. When the neck is palpated, lumps or lymphadenopathy may be found, and a respiratory examination may indicate chronic lung abnormalities or signs of aspiration. These results help identify the source of dysphagia and determine whether additional research is necessary.
Diagnostic Evaluation for Dysphagia
Depending on the medical history and physical examination, the gastroenterologist may recommend diagnostic testing to confirm dysphagia. The following tests are frequently used in the diagnostic process:
- Laboratory test
- Imaging studies and instrumental evaluation
Laboratory test
There is no single laboratory test that definitively diagnoses dysphagia causes. But certain blood tests may be used to investigate possible underlying causes or complications, especially when neurological or systemic diseases are suspected. These laboratory tests involve:
- Complete blood count (CBC)
- Thyroid function studies
- Vitamin B-12
- Creatine kinase
Complete blood count: CBC measures the red blood cells (RBC), white blood cells (WBC), and platelets. It is used in the evaluation of dysphagia to detect infection, inflammation, or anemia, which can be indicated in underlying systemic illness, malignancy, or inflammatory process contributing to swallowing difficulties.
Thyroid function studies: Hormones like thyroxine and TSH are measured by this test. It is recommended to investigate for thyroid dysfunction (hypothyroidism or hyperthyroidism) or structural abnormalities (thyroid cancer or goitre) that could cause or worsen dysphagia by altering the structure or muscle function of the neck.
Serum vitamin B-12: Serum vitamin B-12 levels are measured with a blood test. A deficiency in vitamin B-12 can cause neurological issues. This may result in neurogenic swallowing problems. So, checking B-12 levels is important when evaluating patients with dysphagia.
Creatine kinase: This test measures levels of the muscle enzyme creatine kinase. It is used to screen for muscle diseases (myopathies) that may present with dysphagia, as elevated creatine kinase can suggest an underlying neuromuscular cause of impaired swallowing.
Imaging studies and instrumental evaluation
Imaging investigations and instrumental examinations are important for diagnosing and characterising dysphagia. These approaches are useful for determining the types, location, and cause of swallowing difficulty.
Imaging investigations and instrumental evaluation include the following: Imaging studies and Instrumental evaluation include:
- Bedside swallowing assessment
- Barium swallow (esophagram)
- Fiberoptic Endoscopic Evaluation of Swallow (FEES)
- Upper endoscopy
- Video fluoroscopic Swallow Study (VFSS)
- Pharyngoscopy
- 24-hour pH impedance testing or wireless pH testing
- Esophageal manometry
- pH monitoring
- Computed tomography (CT) scan or
- Magnetic resonance imaging (MRI)
Bedside swallowing assessment: A bedside swallowing assessment is a clinical test performed at the patient’s bedside to screen for dysphagia by evaluating swallowing ability and aspiration risk without the use of instrumentation. The patient swallows various food and liquid consistencies while monitoring for signs such as coughing, choking, wet or gurgling voice quality, drooling, or difficulty managing secretions. This test helps identify individuals who are at risk of dysphagia or aspiration and may require further instrumental assessment or dietary modifications. While useful for initial screening and guiding management decisions, but cannot fully assess deeper swallowing phases or silent aspiration.
Barium swallow (esophagram): The barium swallow test is a key diagnostic imaging study used to evaluate oesophagal dysphagia. Performed by a radiologist, barium liquid is swallowed by the patient, which coats the lining of the oesophagus and allows for real-time fluoroscopic visualization of the swallowing process. It reveals anatomical abnormalities of the esophagus, helping to identify structural issues such as strictures, rings, tumors, diverticula, and hiatal hernias, as well as motility disorders like achalasia.
The barium swallow also provides information about the functional integrity of the pharynx and upper esophagus, capturing any delays or abnormalities in bolus transit. While invaluable in detecting both morphologic and functional causes of dysphagia, it is rarely used as a stand-alone test and is usually complemented by other investigations such as endoscopy or esophageal manometry for a complete diagnostic assessment.
Fiberoptic Endoscopic Evaluation of Swallow (FEES): The Fiberoptic Endoscopic Evaluation of Swallowing (FEES) is a diagnostic procedure used to assess swallowing difficulties. This test helps identify problems such as aspiration (food or liquid entering the airway), residue remaining in the throat after swallowing, or structural and functional abnormalities of the swallowing mechanism.
Upper endoscopy: Upper endoscopy is a key diagnostic procedure for patients with dysphagia, especially when esophageal causes are suspected. Upper endoscopy allows direct visualization of the esophagus, stomach, and the first part of the small intestine. This examination enables gastroenterologists to identify structural abnormalities such as esophageal strictures, rings, tumors, inflammation (esophagitis), and ulcers. Additionally, tissue sample (biopsies), made possible by upper endoscopy, is essential for the diagnosis of diseases like cancer, infections, and eosinophilic oesophagitis.
Videofluoroscopic Swallowing Study (VFSS): The videofluoroscopic swallowing study is considered the gold standard in diagnosing oropharyngeal dysphagia. This specialized imaging test uses real-time X-ray fluoroscopy to visualize the movement of the mouth, pharynx, larynx, and esophagus during swallowing, as the patient consumes barium-containing substances. VFSS enables gastroenterologists to evaluate all four phases of swallowing, detecting structural and functional abnormalities such as aspiration, penetration, delayed swallowing reflex, insufficient laryngeal closure, reduced epiglottic inversion, and residue in the pharynx after swallowing.
Pharyngoscopy: Pharyngoscopy is an endoscopic procedure that allows direct visualisation of the pharynx and larynx. Clinicians can examine the mucosal surfaces, detect structural abnormalities such as tumors, strictures, inflammation, or foreign bodies, and assess the function of the vocal cords and surrounding tissues during swallowing. Pharyngoscopy can also help identify signs of aspiration, pooling of secretions, or impaired movement of the pharyngeal muscles. This procedure is useful when oropharyngeal causes of dysphagia are suspected and can guide further management or the need for biopsy and additional investigations.
24-hour pH impedance testing or wireless pH testing: This is a diagnostic procedure that measures both acid and non-acid reflux from the stomach into the esophagus over a full day, which can help evaluate swallowing difficulties (dysphagia) related to reflux disease. This tube remains for 24 hours while the patient goes about their normal activities and meals. The sensors detect changes in pH (acid levels) and impedance (movement of liquid, gas, or mixed contents), providing detailed information about the frequency, type, and height of reflux episodes.
This helps to determine whether gastroesophageal reflux, which can cause esophageal irritation, strictures, or motility problems, is contributing to a patient’s dysphagia, making the 24-hour pH impedance test a valuable tool in assessing reflux-related swallowing disorders.
Esophageal manometry: This diagnostic procedure checks how well the esophagus moves and works. It is often used to find out why someone has dysphagia, which is difficulty swallowing. The test can identify motility disorders, such as achalasia or esophageal spasm, which can lead to dysphagia. By providing detailed information about esophageal muscle activity, esophageal manometry helps pinpoint functional abnormalities contributing to swallowing problems and guides appropriate treatment.
pH monitoring: Esophageal pH monitoring checks if acid reflux is causing swallowing problems. A thin tube is placed in your esophagus for 24 hours to measure acid levels while you record your symptoms. This helps doctors see if acid irritation or muscle spasms from reflux are making it hard for you to swallow, so they can choose the right treatment.
Computed tomography (CT) scan: When structural or anatomical abnormalities are detected, a CT scan might help evaluate dysphagia. Finding tumors, masses, or lymphadenopathy that might be compressing or invading the oesophagus or throat might be aided by CT imaging of the chest and neck. It is also useful for assessing complications such as abscesses, fistulas, or evidence of aspiration pneumonia. In cases of suspected malignancy, CT scans provide detailed information about the extent of disease and involvement of surrounding tissues, which is important for staging and treatment planning.
Magnetic resonance imaging (MRI): In dysphagia assessment, MRI is especially effective for visualizing the soft tissues of the oropharynx, larynx, and upper esophagus. It is mostly recommended when soft tissue tumors, neurological involvement, congenital deformities, or infiltrative processes that cannot be sufficiently evaluated by other imaging abnormalities are suspected. When structural or neural reasons for dysphagia are suspected, MRI is useful for a thorough evaluation since it may rule out cancers, show the extent of tumor invasion, and detect neurological or soft tissue diseases.
Stages of Dysphagia
Dysphagia can be staged and classified based on the location of the swallowing impairment, the phase of swallowing affected, and the severity of the symptoms. There are 4 stages of dysphagia such as oral preparatory stage, the oral (propulsive) stage, the pharyngeal stage, and the esophageal stage.
Dysphagia Differential Diagnosis
Differential diagnosis for dysphagia is a list of possible medical conditions that can make swallowing difficult and have similar symptoms. The causes of dysphagia can be grouped into three main categories: structural (mechanical), neuromuscular, and functional disorders. These affect the oropharyngeal (mouth and throat) or esophageal (food pipe) stages of swallowing. Common conditions to consider include:
Common conditions considered include:
- Achalasia: It is a condition characterised by impaired relaxation of the lower esophageal sphincter, leading to difficulty with the passage of food into the stomach.
- Dermatomyositis: An inflammatory myopathy that can affect swallowing muscles, causing oropharyngeal dysphagia.
- Myasthenia Gravis: It is a neuromuscular junction disorder leading to fatigable weakness, often affecting swallowing.
- Eosinophilic esophagitis: Chronic allergic/immune condition causing inflammation, rings, and strictures in the esophagus, leading to dysphagia.
- Esophageal malignancies (Esophageal cancer): This can cause progressive obstruction as the tumor grows, resulting in dysphagia to solids and then liquids.
- Esophageal webs and rings: These are thin, membranous folds of tissue that partially narrow the esophagus, causing intermittent difficulty swallowing solid foods.
- Gastroesophageal reflux disease (GERD): This is a chronic acid reflux that can cause inflammation, strictures, and scarring, leading to dysphagia.
- Hiatal hernia: This condition occurs when part of the stomach herniates through the diaphragm, which can lead to mechanical obstruction or impaired peristalsis and cause dysphagia.
- Multiple sclerosis: This is a demyelinating disease that can impair central nervous control of swallowing.
- Parkinson's disease: Neurodegenerative disorder frequently associated with oropharyngeal motor dysfunction and swallowing difficulties.
Dysphagia Treatment Goals
The overall goals of treatment for dysphagia are to improve swallowing safety and efficiency, maintain adequate nutrition and hydration, and enhance the individual’s quality of life. Dysphagia treatment goals include:
The primary goal is to ensure safe and effective swallowing to prevent aspiration, choking, and related complications such as pneumonia.
- To maintain or restore the patient’s ability to eat and drink orally.
- To minimise complications such as malnutrition, dehydration, and respiratory illness.
- To improve the patient’s ability to participate in daily activities involving eating and drinking, thereby supporting social engagement and well-being.
Dysphagia treatments are designed to enhance swallowing safety, enhance nutritional condition, and reduce the risk of complications such as aspiration and pneumonia. The major objective is to compensate for persistent deficiencies or restore as much normal swallowing function as possible so that people may continue to eat and drink enough water and engage fully in everyday activities. Treatment options for dysphagia include:
- Non-pharmacological treatment
- Pharmacological treatment
- Surgical interventions
Non-pharmacological treatment
This focuses on improving swallowing safety, efficiency, and patient quality of life without depending on medications or surgery. The most widely recommended and evidence-based approaches include:
- Lifestyle and behavioural changes: Adjusting eating habits such as eating smaller, more frequent meals, cutting food into small pieces, thoroughly chewing, eating slowly, and avoiding foods or textures that trigger symptoms can make swallowing easier. Thickening liquids and modifying food consistency (e.g., pureed or soft diets) are key interventions to prevent aspiration and support adequate nutrition. Changing the posture or position of the head while swallowing.
- Swallowing exercises: Targeted exercises and rehabilitation techniques help strengthen the muscles used in swallowing, retrain swallowing coordination, and promote safer and more efficient food transit. These may include oral motor exercises, easy swallow, and other techniques provided by speech-language pathologists.
- Enteral feeding (Feeding tube): For patients who are unable to maintain adequate nutrition and hydration by mouth or who are at ongoing risk of aspiration, temporary or permanent feeding tubes (nasogastric or gastrostomy tubes) can ensure nutritional support while minimising risks associated with oral feeding.
- Patient education: Educating patients and caregivers about safe swallowing practices, recommended food and liquid textures, proper posture, and behavioural strategies is essential for self-management and prevention of complications. Speech-language pathologists or multidisciplinary teams often support education.
Pharmacological treatment
This is personalized to each patient's specific situation and helps to enhance swallowing function, reduce symptoms, and avoid complications like aspiration or malnutrition. Important pharmaceutical interventions consist of:
- Botulinum toxin and muscle relaxants: These are used to help relax overly tight or spastic muscles in the esophagus. This is especially useful in conditions like achalasia or esophageal spasms, where the muscles fail to relax properly and block the passage of food.
- Proton pump inhibitors (PPIs) and H2-receptor blockers: These are commonly given when dysphagia is caused by gastroesophageal reflux disease (GERD). These drugs lower stomach acid, allowing the esophagus to heal from irritation and improving swallowing.
- Antibiotics: Antibiotics are prescribed if dysphagia is due to an infection of the throat, mouth, or esophagus. Treating the infection can relieve inflammation and restore normal swallowing.
- Corticosteroids: These drugs are used when an allergic reaction, such as eosinophilic esophagitis (EoE), causes swelling and narrowing of the esophagus. These medicines reduce inflammation and help improve swallowing.
- Other medications for neurological disorders: These are sometimes given to manage the symptoms of conditions like Parkinson’s disease or myasthenia gravis, which can impair the nerves and muscles involved in swallowing. These treatments aim to improve muscle control and coordination during swallowing.
Surgical interventions
Surgery is considered when conservative measures fail to restore safe and adequate oral intake or when life-threatening aspiration or obstructive pathology is present. The choice of surgical procedure depends on the cause and severity of dysphagia, as well as patient factors and overall goals of care.
- Peroral endoscopic myotomy (POEM)
- Esophageal stent placement
- Stretching the constricted esophageal segments with dilation
- Surgery to remove an esophageal blockage, such as a tumor
Peroral endoscopic myotomy (POEM): A minimally invasive endoscopic technique used to treat achalasia and other esophageal motility disorders. In the POEM, the inner circular muscle of the esophagus is cut, allowing easier passage of food into the stomach by relieving the abnormal tightness at the lower esophageal sphincter.
Esophageal stent placement: Self-expandable esophageal stents are used most commonly for palliative treatment of malignant dysphagia, where a tumor or malignancy is causing obstruction. Stents can also be considered for refractory benign esophageal strictures that do not respond to dilation. This method quickly restores the ability to swallow solids and liquids by re-establishing esophageal patency, and is especially valuable in patient’s ineligible for surgery or other therapies.
Stretching the constricted esophageal segments with dilation: Esophageal dilation is a procedure used to dilate a narrowed area of the esophagus that makes swallowing difficult (dysphagia). Narrowing of the esophagus (called a stricture) can happen because of scarring from acid reflux, radiation therapy, surgery, inflammation, or certain diseases.
Surgery to remove an esophageal blockage, such as a tumor: Surgical resection may be indicated when a discrete lesion, such as a benign or malignant tumour, is causing obstruction and the patient is a surgical candidate. This approach aims to provide a definitive cure for benign blockages or to improve swallowing and quality of life in selected cases of cancer when endoscopic therapies are insufficient or not feasible.
Dysphagia Prognosis
The prognosis of dysphagia depends on its underlying cause, severity, the patient’s age, and how early the condition is diagnosed and treated.
- In cases such as post-stroke dysphagia, function may gradually return over time, often within 3 weeks to 6 months, but recovery duration can extend beyond that in some individuals.
- For mechanical or structural issues, such as strictures or achalasia, prognosis improves markedly with timely surgical or endoscopic intervention.
- When dysphagia stems from progressive neurological diseases, for example, ALS or Parkinson’s, the outlook may be more guarded, and long-term management is often needed.
Dysphagia Treatment Cost in Hyderabad, India
The cost of Dysphagia Treatment in Hyderabad generally ranges from ₹9,000 to ₹45,000 (approximately US $110 – US $545).
The exact dysphagia treatment cost varies depending on factors such as the underlying cause (neuromuscular, structural, motility disorder, GERD-related), the diagnostic tests required (endoscopy, barium swallow, manometry), whether medical therapy or endoscopic intervention is needed, surgeon/gastroenterologist expertise, and the hospital facilities chosen — including cashless treatment options, TPA corporate tie-ups, and assistance with medical insurance approvals wherever applicable.
Cost Breakdown According to Type of Dysphagia Treatment / Evaluation
- Basic Evaluation & Medical Management – ₹9,000 – ₹15,000 (US $110 – US $180)
- Diagnostic Endoscopy / Barium Swallow / Manometry – ₹15,000 – ₹25,000 (US $180 – US $305)
- Endoscopic Dilatation (for strictures) – ₹22,000 – ₹35,000 (US $265 – US $425)
- Complex / Recurrent Dysphagia Management (GERD, spasms, neurological issues) – ₹30,000 – ₹45,000 (US $360 – US $545)
Frequently Asked Questions (FAQs) on Dysphagia Treatment
What are dysphagia symptoms?
Symptoms of dysphagia include difficulty swallowing, coughing or choking during meals, sensation of food sticking in the throat or chest, drooling, unexplained weight loss, recurrent pneumonia, and changes in voice quality after eating or drinking.
Which Is the best hospital for Dysphagia Treatment in Hyderabad, India?
PACE Hospitals, Hyderabad is regarded as one of the most comprehensive centres for diagnosing and treating dysphagia, covering both structural and neurological swallowing disorders.
Our expert team of gastroenterologists, ENT specialists, neurologists, and speech-swallow therapists provides precise, minimally invasive, and evidence-based care tailored to each patient.
With advanced endoscopy suites, high-resolution manometry systems, complete swallowing-assessment facilities, and dedicated post-treatment rehabilitation, PACE Hospitals ensures accurate diagnosis, effective treatment, and improved swallowing function — supported by cashless facility options, TPA corporate tie-ups, and assistance with medical insurance processing for eligible patients.
Can dysphagia affect speech?
Yes, dysphagia can affect speech because both swallowing and speech share nerves and muscles in the mouth and throat. Conditions causing dysphagia, such as stroke or neurological disorders, often result in speech problems, including hoarseness, dysarthria, or nasal speech. The impaired muscle control affecting swallowing can also disrupt speech articulation.
Does GERD cause dysphagia?
Yes, Gastroesophageal reflux disease (GERD) can cause dysphagia by damaging the esophagus lining or causing esophageal spasms and strictures. Chronic acid reflux leads to inflammation or narrowing that physically obstructs the food passage, resulting in difficulty swallowing.
Is dysphagia congenital?
Dysphagia can sometimes be congenital, which means a person is born with it. This usually happens if there are problems with the structure or function of the mouth, throat, or esophagus from birth. Examples include cleft palate or certain birth defects affecting the nerves or muscles used for swallowing. Studies revealed that congenital dysphagia is less common than acquired forms; it does occur, especially in children with developmental or anatomical issues.
What Is the cost of Dysphagia Treatment at PACE Hospitals, Hyderabad?
At PACE Hospitals, Hyderabad, the cost of Dysphagia Treatment typically ranges from ₹9,000 to ₹40,000 and above (approximately US $110 – US $485). However, the final cost varies depending on:
- Type of underlying swallowing disorder
- Diagnostic tests required (endoscopy, barium swallow, manometry)
- Whether medical therapy or endoscopic intervention is required
- Severity and complexity of symptoms
- Surgeon/gastroenterologist expertise
- Additional supportive care such as speech-swallow therapy
- Need for ongoing follow-up or repeat interventions
For basic evaluations, the cost falls at the lower end, whereas advanced endoscopic treatments or complex swallowing disorders fall toward the higher end.
After a thorough clinical assessment and swallowing evaluation, our specialists will provide a personalized treatment plan and a detailed, transparent cost estimate based on your condition.
Is dysphagia curable?
Dysphagia is sometimes curable, but this depends on the cause and type of swallowing difficulty. After tests to assess swallowing and examine the oesophagus, the exact type of dysphagia can usually be identified.
In many cases, dysphagia can be improved with treatment, even if a complete cure is not always possible. Treatment options may include speech and language therapy to learn safer swallowing techniques and changes in food or liquid consistency to make swallowing easier.
When swallowing is more severely affected, alternative feeding methods such as tube feeding may be required. If dysphagia is caused by a narrowing of the oesophagus, procedures or surgery to widen the passage or place a stent (a plastic or metal tube) may help. Early evaluation and appropriate treatment can significantly improve swallowing and quality of life.
What is dysphagiaa and what are its causes?
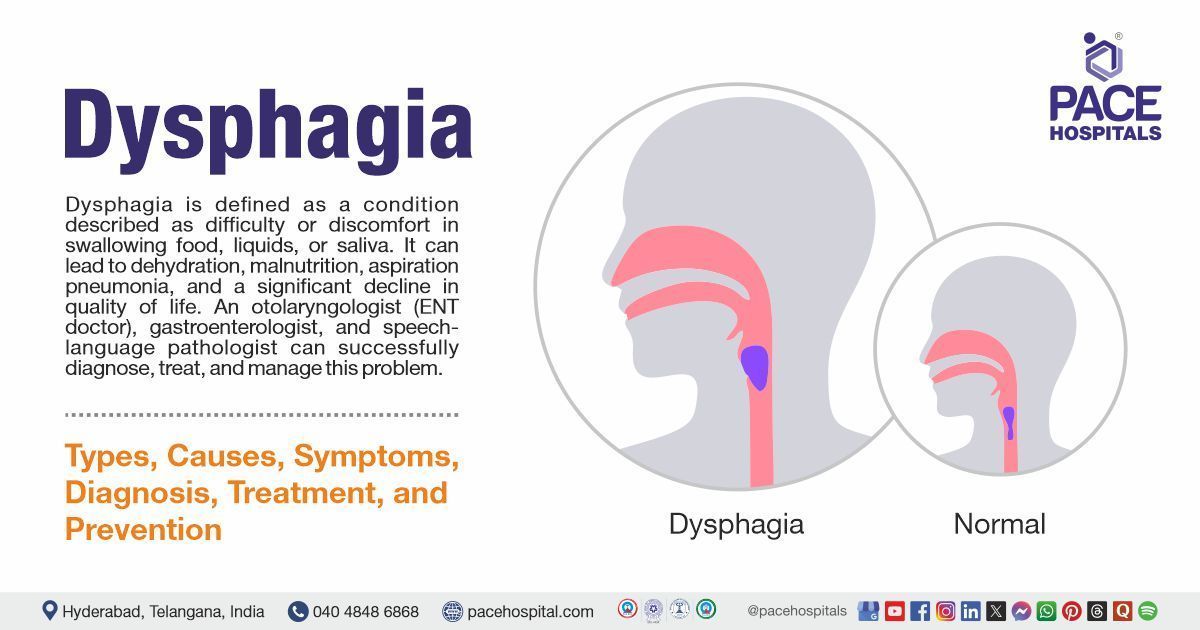
Dysphagia is defined as difficulty swallowing, affecting the movement of food or liquid from the mouth to the stomach. Causes include neurological disorders (stroke, Parkinson’s), structural abnormalities (tumours, strictures), esophageal motility disorders, and inflammatory conditions such as GERD.
Is dysphagia a disability?
Yes, dysphagia or swallowing can be classified as disability since it can have a significant impact on one's ability to eat, drink, and maintain proper nutrition, which can lower quality of life and perhaps cause health issues. The WHO recognises Dysphagia as a medical disability. It can be associated with various conditions, including neurological disorders, muscular, and physical abnormalities.
How does dysphagia occur?
When the natural swallowing process is disrupted, dysphagia develops due to neurological impairment, structural lesions, muscular disorders, or inflammation. This disruption can affect the oral, pharyngeal, or esophageal phases of swallowing, leading to difficulty moving food or liquids safely to the stomach.
What to eat with dysphagia?
Individuals with dysphagia are frequently encouraged to consume soft, moist, and pureed foods, as well as thickened drinks, to reduce the risk of aspiration and choking. Dietary changes are customised based on swallowing assessments and may include avoiding dry, hard meals.
Is dysphagia a pressure effect on the larynx?
Dysphagia is not usually caused by pressure on the larynx. It results from neuromuscular, structural, or motility disorders affecting the swallowing pathway. However, external compression from tumors or masses near the larynx or esophagus can cause dysphagia by narrowing or obstructing the passage.
What is the oropharyngeal phase of dysphagia?
Oropharyngeal phase dysphagia is difficulty or inability to initiate swallowing due to dysfunction in the mouth or throat (oropharynx). It causes symptoms like coughing during swallowing, food sticking in the throat, drooling, and nasal regurgitation. This phase involves impaired muscle function or sensory loss, making it hard to move food safely from the mouth into the esophagus. If left untreated, it can cause complications such as aspiration pneumonia and weight loss.
What type of stroke causes dysphagia?
Dysphagia commonly results from strokes affecting the brain regions that control swallowing muscles, primarily ischemic strokes in the brainstem or cortical areas. Such strokes impair swallowing coordination, leading to oropharyngeal dysphagia. Central nervous system damage from stroke is a major cause of swallowing difficulties.
Can gas cause dysphagia?
Gas is not the direct cause of dysphagia. Excess gas and bloating, on the other hand, can cause abdominal discomfort and reflux symptoms, which may mimic or worsen swallowing difficulties. Dysphagia typically stems from structural or neurological issues rather than from gas.
How common is dysphagia?
Dysphagia is relatively frequent, especially among older adults. It affects 2% to 16% of the general population, with higher prevalence among stroke survivors (more than 30%), people with neurological disorders, and elderly adults in nursing facilities. The prevalence varies depending on the cause, age, and health problems.
Can post-nasal drip cause dysphagia?
Yes, postnasal drip can cause dysphagia (difficulty swallowing) by irritating the throat, swelling it, or giving the sensation of mucus buildup in the throat. This excess mucus can lead to discomfort or a feeling of a lump, sometimes impairing normal swallowing. Postnasal drip is often linked to sinus infections, allergies, or rhinitis, which can cause throat inflammation contributing to swallowing difficulties.