Dysphagia - Symptoms, Causes, Diagnosis, Treatment & Prevention
PACE Hospitals
Overview | Prevalence | Types | Causes | Risk Factors | Symptoms | Complications | Diagnosis | Treatment | Prevention | Odynophagia vs Dysphagia | FAQs | When to consult a Doctor
Dysphagia definition
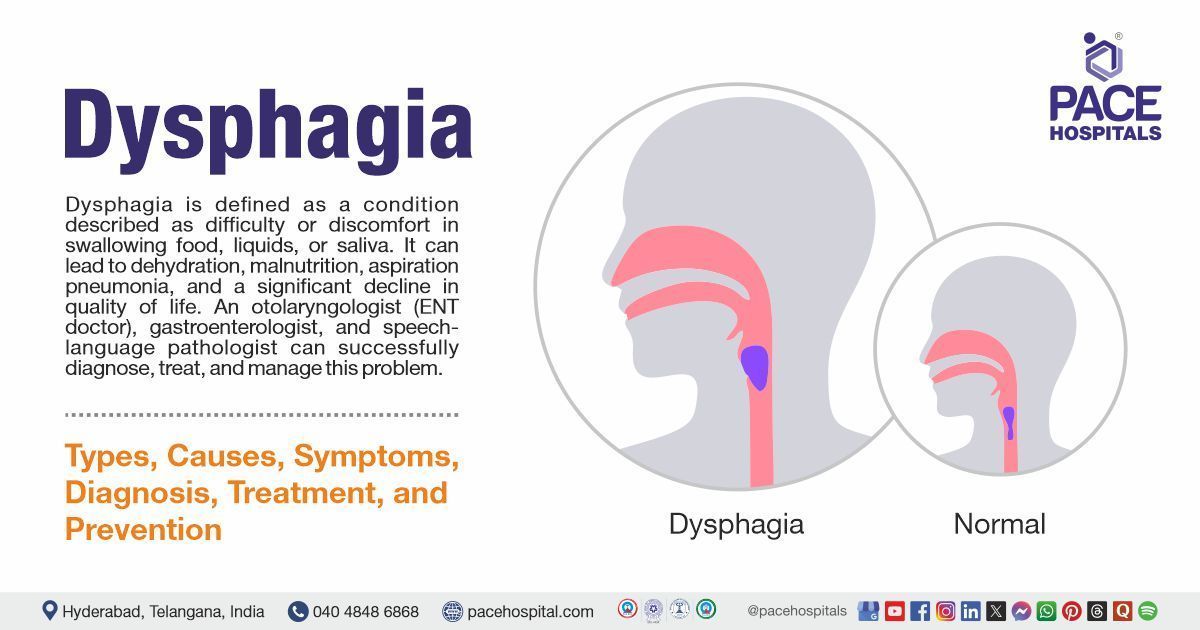
Dysphagia is defined as a condition described as difficulty or discomfort in swallowing food, liquids, or saliva. Dysphagia can be accompanied by various symptoms, which include pain while swallowing, choking or coughing when eating, or feeling as though food is lodged in the chest or throat, backflow of food, unexplained weight loss, and recurrent chest infections or pneumonia.
The main causes of dysphagia involve a combination of neurological disorders, structural abnormalities of the esophagus or throat, muscle weakness, or damage from medical conditions, surgery, or medications. If left untreated, dysphagia can lead to major complications such as dehydration, malnutrition, aspiration pneumonia, and a significant decline in quality of life. These complications can cause serious illness, hospitalisation, and in severe cases, death.
A gastroenterologist, otolaryngologist (ENT doctor), and speech-language pathologist can successfully diagnose, treat, and manage the problem, ensuring proper healing and avoiding complications.
Dysphagia meaning
Dysphagia is derived from two Greek words. The term dysphagia means:
- “Dys” meaning “difficulty” or “bad” in swallowing
- ‘Phagia’ meaning ‘to eat’ or “to swallow” in Greek. It indicates difficulty in swallowing food after chewing in the mouth.
Dysphagia Prevalence
Prevalence of dysphagia Worldwide
Dysphagia affects about 20% of the general population and up to 50–66% of people over 60, with women being more commonly affected than men. It is more frequent in older adults and those with conditions like stroke, Alzheimer’s disease, or ALS. In younger individuals, it’s often linked to systemic illnesses such as autoimmune diseases, GERD, or eosinophilic esophagitis. Despite its high prevalence, only about half of those with dysphagia report their symptoms to a doctor.
Prevalence of dysphagia in India
Studies from India show that dysphagia is common, especially among stroke patients, with prevalence rates around 47.7%. A high incidence (11.1% - 87.5%) was observed in stroke patients. In older adults and hospital settings, about 17-20% report swallowing difficulties. While statistics on the general population are limited, dysphagia is regarded as a significant health concern in high-risk populations such as the elderly and those with neurological problems.
Types of Dysphagia
Depending on the location of the swallowing difficulties, dysphagia can be classified into two main categories.
Types of dysphagia are as follows:
- Oropharyngeal dysphagia (high dysphagia)
- Esophageal dysphagia (low dysphagia)
Other subtypes include:
- Esophagogastric dysphagia
- Paraesophageal dysphagia
- Functional dysphagia
Oropharyngeal dysphagia
This type involves trouble starting a swallow, often because of issues in the mouth or throat. It usually comes from neurological or muscular disorders that impact the swallowing muscles.
Esophageal dysphagia
This type occurs when there is a problem in the esophagus (the tube that carries food from the throat to the stomach), such as a blockage, narrowing, or motility disorder.
Esophagogastric dysphagia
Esophagogastric dysphagia is difficulty swallowing caused by problems at the junction between the esophagus and the stomach. It occurs when food cannot pass smoothly from the lower esophageal sphincter (LES) into the stomach. This may be due to muscle dysfunction (like achalasia) or physical blockages such as strictures or tumors. Patients often feel like food is stuck behind the lower part of the chest (sternum).
Paraesophageal dysphagia
Paraesophageal dysphagia results from external pressure or infiltration on the esophageal wall, rather than a problem inside the esophagus itself. This pressure can narrow or obstruct the esophagus, and in severe cases, may also affect how well the esophagus moves food. Causes include mass lesions or nearby structural abnormalities.
Functional dysphagia
Functional dysphagia is difficulty swallowing with no physical blockage or major movement disorder found on medical tests. It is diagnosed when all other causes are ruled out. The problem is thought to be related to nerve sensitivity or how the brain processes swallowing.
Dysphagia Causes
Dysphagia results from different underlying medical conditions that interfere with the normal functioning of swallowing. The causes can be temporary, e.g., infection or swelling, or more chronic, e.g., muscle, nerve or esophageal damage. Knowing the reason behind the swallowing issue is important for selecting proper therapy and the prevention of complications.
The main 4 causes of dysphagia are:
- Neurologic problems
- Structural abnormalities
- Problems with motility
- Allergies that affect swallowing
Neurologic problems: Neurological problems are a major cause of dysphagia and occur when the nerves that control the muscles of swallowing are damaged or diseased. Conditions such as stroke, amyotrophic lateral sclerosis (ALS), Parkinson’s disease, myasthenia gravis, and polymyositis can weaken or incoordinate the muscles of the mouth, throat, and esophagus, making swallowing difficult or unsafe.
These nerves can also be damaged by head and neck trauma or surgery. Even hyperactive and underactive thyroid conditions can impact swallowing-related nerve function. Coughing during swallowing or nasal regurgitation are common symptoms of neurologic dysphagia, which may need specialized assessment and treatment.
Structural abnormalities: Structural abnormalities refer to physical changes in the esophagus that block or narrow the passageway, making it difficult for food to move through. This can include strictures (narrowing) from scarring, chronic inflammation, or tumors, as well as benign or cancerous growths. Esophageal diverticula, such as Zenker’s diverticulum, are pouch-like pockets that trap food and can cause regurgitation or choking. Some individuals are born with anatomical differences that predispose them to dysphagia, but most structural issues develop over time due to disease, injury, or chronic irritation.
Problems with motility: Esophageal motility disorders occur when the muscles of the esophagus do not contract in a coordinated way to move food from the throat to the stomach. Normally, swallowing triggers a wave-like movement (peristalsis) that pushes food downward, and rings of muscle called sphincters at the top and bottom of the esophagus open and close at the right times.
In motility disorders such as achalasia, when the lower esophageal sphincter is not relaxed, food cannot pass into the stomach. In distal esophageal spasm and jackhammer esophagus, abnormal or overly strong contractions can cause pain, chest discomfort, and food to come back up. These problems can also arise after surgery on the esophagus or from having a breathing tube, but sometimes the exact cause is unknown.
Allergies that affect swallowing: Eosinophilic esophagitis is a chronic allergic condition where eosinophils (a type of white blood cell) build up in the esophagus, causing inflammation, swelling, and narrowing. This can lead to rings, strictures, and food getting stuck, which may require emergency care. It’s more common in people with allergies or asthma, and symptoms include difficulty swallowing, chest pain, and, in children, food refusal or poor growth.
Dysphagia Risk Factors
While anyone can develop dysphagia, some people are more likely to experience it due to certain factors. These risk factors either affect the swallowing mechanism directly or make the body more vulnerable to conditions that impair swallowing.
The following are the risk factors of dysphagia:
- Older age
- Neurological conditions
- Male gender
- History of pneumonia
- Comorbidities and impaired functionality
- Malnutrition and poor muscle strength
- Lifestyle factors
- Certain medications
Older age: Ageing is strongly associated with dysphagia risk. As people age, muscle strength and coordination decline, saliva production may decrease, and there is a higher prevalence of neurological diseases and comorbidities, all of which impair the swallowing mechanism.
Neurological conditions: Disorders such as stroke, Parkinson’s disease, amyotrophic lateral sclerosis (ALS), and other neurodegenerative or neuromuscular diseases can damage the nerves and muscles involved in swallowing. For example, stroke, especially right-sided or haemorrhagic, can disrupt the brain’s control of swallowing, leading to oropharyngeal dysphagia.
Male gender: Men may have a higher risk, possibly due to higher rates of risk factors like smoking, alcohol use, and certain medical conditions.
History of pneumonia: Often caused by aspiration (food or liquid entering the lungs), which can also damage the lungs and throat, increasing the risk of further aspiration and swallowing problems.
Comorbidities and impaired functionality: Multiple chronic conditions (such as respiratory disease, diabetes, or cardiovascular disease), frailty, and reduced physical function are all linked to higher dysphagia risk. These conditions can weaken the muscles and coordination needed for safe swallowing.
Malnutrition and poor muscle strength: Malnutrition and low body mass index (BMI) cause the muscles, particularly the swallowing muscles, to deteriorate. The body's capacity to maintain and repair tissues is further compromised by poor nutritional condition, which raises the risk of dysphagia.
Lifestyle factors: Lifestyle factors such as smoking and chronic drinking can raise the risk of dysphagia. Smoking harms the mucosa of the oropharynx and esophagus, weakens muscle function, and increases the chances of cancers that block the swallowing pathway. Drinking too much alcohol can lead to chronic irritation, inflammation, and nerve damage, all of which can disrupt the swallowing process.
Certain medications: Antipsychotics, antiepileptic drugs, antidepressants, and narcotic painkillers are among the medications that are linked to a higher incidence of dysphagia. These medications have the potential to impair swallowing by affecting nerve and muscle function or by producing dry mouth.
Dysphagia Symptoms
Dysphagia is a swallowing disorder that can impair eating, drinking, and quality of life. The ability to swallow securely and efficiently, as well as different related symptoms, are critical in determining this condition. It is very important to recognize these symptoms for timely diagnosis and effective management.
Signs and symptoms of dysphagia include the following:
- Sensation of food getting stuck
- Odynophagia
- Coughing or Choking
- Regurgitation
- Nasal regurgitation
- Hoarseness
- Shortness of breath
- Chest pain
- Persistent sore throat
- Reflux or heartburn
- Vomiting
Sensation of food getting stuck: This sensation results from dysphagia, which interferes with food's usual passage along the swallowing pathway. Food or liquid may stall or become stuck because of nerve issues, muscle weakness, or constriction or obstruction in the oesophagus or throat.
Odynophagia: Pain happens when the lining or muscles of the throat or esophagus are inflamed, irritated, or injured. This can accompany dysphagia but is a separate symptom indicating possible infection, injury, or severe inflammation.
Coughing or choking: Normally, the airway closes tightly during swallowing to prevent food or liquid from entering the windpipe. In dysphagia, especially oropharyngeal dysphagia, weak or poorly coordinated muscles fail to protect the airway, allowing food or liquid to enter the trachea. This triggers a cough or choking as a protective reflex.
Regurgitation: This happens when food or liquid comes back to the mouth or throat after swallowing, without nausea or vomiting. If it tastes like what the individual just ate, it suggests a swallowing problem; if it’s sour or bitter, it may be from the stomach, indicating GERD.
Nasal regurgitation: When swallowed, food or liquid retraces and flows into the nose. This occurs if the nasopharynx fails to shut correctly, and it can be a sign of an issue with the nerves that enable the muscles of the soft palate or throat.
Hoarseness: Food or liquid entering the larynx (voice box) or sitting in the throat can change the sound of the voice, making it hoarse, “wet,” or gurgly after eating or drinking. This is a subtle sign of aspiration risk.
Shortness of breath: When food or liquid accidentally enters the airway (aspiration), it can cause coughing, choking, and a feeling of breathlessness. Chronic aspiration can lead to lung irritation or pneumonia, which also causes shortness of breath.
Chest pain: Dysphagia from esophageal causes (like spasms, strictures, or blockages) can make swallowing painful and feel like pressure or pain in the chest. This can mimic heart problems but is due to difficulty moving food down the esophagus.
Persistent sore throat: Food or liquid pooling in the throat or repeated coughing and throat clearing from impaired swallowing can irritate the throat, causing ongoing soreness.
Reflux or heartburn: When swallowing doesn’t work properly, food and stomach acid may come back up into the esophagus or throat. This reflux can cause a burning sensation and is often seen in people with esophageal dysphagia or underlying GERD.
Vomiting: If the esophagus is blocked or not moving properly, swallowed food can back up, and the body may respond by vomiting. This happens more with mechanical obstructions or severe motility problems.

Complications of Dysphagia
Swallowing difficulties caused by dysphagia can have significant effects on nutrition, hydration, and respiratory health. If left untreated, dysphagia can develop into major complications that impair overall health and quality of life.
The following are the possible problems of dysphagia:
- Aspiration pneumonia
- Malnutrition and dehydration
- Food impaction
Aspiration pneumonia: Food or liquids may accidentally enter the airway (aspiration) instead of the esophagus, which leads to lung infections such as aspiration pneumonia. This is a significant complication and can be life-threatening, especially in older adults or those with weakened immune systems.
Malnutrition and dehydration: Eating and drinking can be challenging or uncomfortable for those with dysphagia. People may eventually consume fewer meals or avoid drinking particular liquids, which could result in inadequate consumption of water, protein, calories, and vitamins. This can make it harder to recover after sickness or surgery by causing weight loss, loss of muscle weakness, and a compromised immune system.
Food impaction: This occurs when food becomes stuck in the esophagus due to impaired swallowing or esophageal motility. Acute symptoms include salivation, chest pain, difficulty swallowing, and respiratory trouble if aspiration occurs. Food impaction raises the risk of aspiration pneumonia and esophageal damage.
Dysphagia Diagnosis
A thorough evaluation is necessary to diagnose dysphagia in order to identify the underlying reasons and determine the areas of the swallowing process that are impacted. A proper diagnosis is essential for directing an appropriate course of treatment and preventing complications.
The dysphagia diagnostic tests usually include:
- Medical history
- Physical examination
- Laboratory test
- Blood test
- Imaging studies and instrumental evaluation
- Bedside swallowing assessment
- Barium swallow (esophagram)
- Fiberoptic Endoscopic Evaluation of Swallowing (FEES)
- Upper endoscopy (EGD)
- Video fluoroscopic Swallow Study (VFSS)
- Pharyngoscopy
- 24-hour pH impedance testing or wireless pH testing
- Esophageal manometry
- pH monitoring
- Computed tomography or magnetic resonance imaging
Dysphagia Treatment
Treatment of dysphagia depends on the cause, severity of the disease, and which part of the swallowing process is impacted. The main goals of treating dysphagia are to make swallowing easier and more efficient, ensure proper nutrition and hydration, and prevent complications.
The following may be used to treat dysphagia:
- Non-pharmacological treatment
- Pharmacological treatment
- Surgical interventions
Non-pharmacological treatment
- Swallowing therapy
- Exercises for larynx closure that build laryngeal muscles
- Exercises to strengthen and increase the mobility of the tongue
- Exercises for lip closure that improve lip strength and mobility
- Dietary Modification and Behavioral Changes
- Feeding tube
Pharmacological treatment
- Botulinum toxin injections and other muscle relaxants can help relax specific esophageal muscles.
- Antibiotics
- Proton pump inhibitors and H2 receptor antagonists
- Corticosteroids
- Additional drugs to lessen the symptoms of a neurologic disorder
Surgical intervention
- Peroral endoscopic myotomy (POEM)
- Esophageal stent placement
- Stretching the constricted esophageal segments with dilation
- Surgery to remove an esophageal blockage, such as a tumor
Why Choose PACE Hospitals?
Expert Super Specialist Doctors
Advanced Diagnostics & Treatment
Affordable & Transparent Care
24x7 Emergency & ICU Support

Dysphagia Prevention
While not all cases of dysphagia can be prevented since many are due to stroke, neurological diseases, or cancer, some general measures can reduce the risk or severity of dysphagia, especially in vulnerable people like the elderly or those with chronic illnesses:
- Maintaining oral hygiene
- Performing swallowing muscle exercises
- Early screening
- Improving diet and fluid intake
- Avoiding smoking and drinking
- Adjusting posture
- Preventing aspiration
- Regular screening in high-risk groups
Maintaining oral hygiene: Regularizing dental check-ups and proper oral hygiene are important for preventing infections, tooth loss, and gum disease, all of which can contribute to swallowing problems, especially in older adults.
Performing swallowing muscle exercises: Regular swallowing exercises improve the strength and coordination of the oral and oropharyngeal muscles, allowing for easier swallowing. These exercises help to prevent muscle atrophy and maintain swallowing function, reducing the likelihood of dysphagia onset.
Early screening: Early detection of swallowing difficulties through routine screening in high-risk groups allows for timely intervention. This can prevent the progression of mild swallowing problems into clinically significant dysphagia and prevent complications such as aspiration pneumonia and malnutrition.
Improving diet and fluid intake: Modification of food and liquid textures (e.g., using thickened fluids or pureed foods) can make swallowing safer for at-risk individuals by slowing bolus transit and reducing the risk of aspiration. Nutritional adaptations, such as high-calorie and high-protein diets, also support overall muscle health and function.
Avoiding smoking and drinking: Both can increase the risk of cancers and chronic inflammation in the mouth and throat, which may lead to dysphagia.
Adjusting posture: Adjusting body posture during swallowing (e.g., chin tuck, upright sitting) can optimise the mechanics of swallowing and protect the airway. These compensatory strategies reduce the risk of food or liquid entering the airway and causing aspiration.
Preventing aspiration: For at-risk individuals (elderly, those with neurological disorders), using proper positioning during meals (upright posture), modifying food textures, and supervised feeding can help prevent aspiration and subsequent dysphagia.
Regular screening in high-risk groups: Elderly individuals, people with neurological diseases, and those with a history of head and neck cancer need to be regularly screened for swallowing difficulties to allow for early intervention.
Difference Between Odynophagia and Dysphagia
Odynophagia vs Dysphagia
Odynophagia refers to pain during swallowing, while dysphagia refers to difficulty in swallowing. Recognizing the differences between the two helps in determining the cause, the patient's condition, and the proper treatment. The main differences between odynophagia and dysphagia are as follows:
| Parameters | Odynophagia | Dysphagia |
|---|---|---|
| Definition | Painful swallowing: pain experienced during the act of swallowing. | Difficulty swallowing: an abnormal delay or problem in the movement of food or liquid from the mouth to the stomach. |
| Symptoms | Sharp, burning, or aching pain when swallowing. | Sensation of food or liquid being stuck, delayed, or not passing normally. |
| Pain | Always associated with pain | It may or may not be painful |
| Causes | Infections (viral, bacterial, fungal esophagitis), inflammation (reflux esophagitis), trauma, caustic ingestion, and some medications. | Neurological disorders (stroke, Parkinson’s), structural lesions (tumors, strictures), motility disorders (achalasia), inflammation, infections. |
| Associated risks | Can lead to reduced oral intake due to pain, risk of weight loss and dehydration. | Aspiration pneumonia, malnutrition, dehydration, and social isolation. |
| Location focus | Usually esophageal or oropharyngeal mucosal injury. | It can involve nerves, muscles, or structural abnormalities throughout the swallowing pathway. |
| Treatment | Treat underlying cause: antibiotics, anti-inflammatories, pain management, treating infection or injury | Depends on underlying cause: swallowing therapy, dietary modifications, medical or surgical interventions |
Frequently Asked Questions (FAQs) on Dysphagia
How to cure dysphagia?
Management of dysphagia depends on its cause. Treatments may include swallowing therapy, dietary modifications, medications for reflux or motility disorders, esophageal dilation, or surgery for structural lesions. In some cases, especially those due to neurological disease, dysphagia may not be fully curable but can be managed to improve swallowing safety and nutrition.
What is a dysphagia diet?
A dysphagia diet consists of foods and liquids modified in texture and consistency to facilitate safer swallowing. Levels range from pureed foods and thickened liquids to soft, easy-to-chew foods. The specific diet is tailored to the severity and type of swallowing difficulty.
What causes dysphagia in the elderly?
Dysphagia in the elderly is frequently brought on by neurological conditions (stroke, Parkinson's disease), age-related muscle weakness, esophageal motility problems, anatomical abnormalities (tumours, strictures), and decreased salivary flow. These factors can impair the coordination and strength needed for effective swallowing.
What are the causes of dysphagia in children?
Difficulty in swallowing or dysphagia is not uncommon in children of all age groups. These include congenital anatomic anomalies such esophageal webs and rings, oesophagitis, esophageal strictures, and esophageal motility problems. Rare causes of dysphagia in children include esophageal tumours and external constriction of the oesophagus by vascular rings.
How to treat dysphagia naturally?
Managing dysphagia naturally includes swallowing exercises, postural adjustments (such as chin-tuck), slow eating, and modifying food textures. A speech-language pathologist often guides these strategies. Medical evaluation is essential, as some causes require specific medical or surgical interventions beyond natural or behavioural approaches.
What are dysarthria and dysphagia?
Dysarthria is a disorder of neuromotor control that results from abnormalities in accuracy, speed, or duration needed for controlling speech, leading to poor articulation and slurred speech. Dysphagia is difficulty swallowing, affecting the safe and efficient movement of food or liquid from the mouth to the stomach. Both conditions may result from neurological diseases or injuries.
Can dysphagia cause weight loss?
Dysphagia can lead to weight loss due to reduced oral intake, malnutrition, and dehydration. Difficulty swallowing may cause individuals to avoid eating or drinking, resulting in insufficient caloric and fluid intake, which can have significant health consequences if not addressed promptly.
Can a sore throat cause dysphagia?
A sore throat, usually brought on by diseases like tonsillitis or pharyngitis, might temporarily impair one's ability to swallow. It may be painful or difficult to swallow due to pain and swelling in the throat, but this normally goes away when the underlying infection or inflammation gets better.
How long does dysphagia last?
Dysphagia's duration varies depending on its cause. Acute cases, like infections, can go away in a few days or weeks. In order to preserve nutrition and avoid consequences, chronic or progressive causes, like neurological disorders, may last for a long time and need proper medical management.
What is the difference between achalasia and dysphagia?
Dysphagia is a symptom describing difficulty swallowing, regardless of cause. Achalasia is a specific esophageal motility disorder interpreted by impairment in relaxation of the lower esophageal sphincter and loss of esophageal peristalsis, resulting in dysphagia for both solids and liquids.
What is dysphagia grading?
Grading of dysphagia is a system used to classify the severity of swallowing difficulty, often ranges from grade 0 (no dysphagia) to grade 4 (unable to swallow even saliva). Grading helps guide proper management and monitor response to treatment.
Describe dysphagia pathophysiology?
A disturbance in the normal swallowing process, such as a neurological impairment, muscle dysfunction, anatomical abnormalities, or obstruction, results in dysphagia. Ineffective or delayed passage of food or liquid from the mouth to the stomach might result from its effects on the pharyngeal, esophageal, or oral phases.
What are the exercises for dysphagia?
Dysphagia exercises are therapeutic activities designed to retrain and strengthen the swallowing muscles in order to promote swallowing safety and lower the risk of aspiration or choking. These exercises, guided by speech-language pathologists, may include larynx closure exercises, tongue strengthening, and lip closure exercises. Swallowing retraining is particularly beneficial for individuals with dysphagia due to neurological disorders or after throat surgery.
What is dysphagia lusoria?
Dysphagia lusoria is a condition where difficulty swallowing (dysphagia) is caused by compression of the esophagus from an abnormally routed blood vessel, most commonly an aberrant right subclavian artery. This artery originates from the left side of the aortic arch and passes behind the esophagus to reach the right arm, thereby compressing the esophagus and causing swallowing difficulties.
When to consult a doctor for dysphagia?
Consult a doctor for dysphagia if swallowing difficulties persist for several days, get worse, or make eating and drinking difficult. Signs that need attention include:
- Food or liquid getting stuck
- Frequent choking or coughing
- Painful swallowing
- Unexplained weight loss
- Chest infections caused by aspiration
If these symptoms continue, it is important to consult a dysphagia specialist who can evaluate the cause and recommend the right treatment plan. Seek emergency medical attention if you experience slurred speech, facial paralysis, or drooping, which could suggest a stroke. A general care physician, ENT specialist, or gastroenterologist can provide the best dysphagia treatment to control the disease and prevent complications.
Share on
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868
Appointment request - health articles
Recent Articles