Wilson’s Disease Symptoms, Causes, Prevention, and Treatment
Pace Hospitals
Wilson’s disease is a genetic disorder which predominantly affects liver, basal ganglia of the brain and eyes due to its characteristic element of copper accumulation in the body, arising from impaired copper breakdown. It is a pretty rare ailment, considering its occurrence in 1 of 30,000 individuals.
In medical terminology, Wilson’s disease is also known as progressive hepatolenticular degeneration or hepatolenticular degeneration. This ailment falls under the category of autosomal recessive disorders, as it is an inherited trait or condition from parent to child.
Wilson’s disease give rise to mixed symptoms pertaining to hepatic (related to liver) and neurological (related to brain) which include yellowish skin and eyes (jaundice) ascites (buildup of fluid in stomach) vomiting, muscle stiffness, tremors, hallucinations etc.
A limited amount of copper from food is essential for the body to remain healthy, but excess of it can be toxic and can give rise to organ damage. With early diagnosis and timely treatment, many manifestations of the disease can be managed and reversed. If left untreated, it can be life-threatening and cause severe disability and even death in almost all instances. Therefore, a multidisciplinary team consists of gastroenterologists and hepatologists neurologists, psychiatrists, should work in tandem to manage the disease.
Wilson’s disease definition
Wilson’s disease is defined as a rare inherited disorder that affects the body function to remove excess copper from the body, eventually leading to its accumulation in vital organs such as liver, brain, eyes, and other organs. While conventional, traces of copper from diet are essential for normal bodily function. Excess of it can be fatal.
Wilson’s disease meaning
Wilson’s disease: in a crude way to put – is a genetic condition of excessive accumulation of copper in the body, declining the health of the patient.
Wilson’s disease is named after the famous British neurologist Dr. Samuel Alexander Kinnier Wilson, who identified this disease with his eminent work. One of the world’s greatest neurologists, Dr Wilson worked at the National Hospital for the Paralyzed and Epileptic and later at Kings’ College Hospital, in London, United Kingdom.
Dr Wilson’s most important work - entitled ‘‘Progressive lenticular degeneration, a familial nervous disease associated with liver cirrhosis’’ was published in 1912 in the English scientific journal “Brain” and simultaneously in Revue Neurologique, in the same year in French. In the research papers, he analyzed 12 clinical cases, regarding the same disease he was describing. His thesis and paper, on progressive lenticular degeneration, made him famous as a young physician.
Progressive hepatolenticular degeneration meaning
Progressive hepatolenticular degeneration is the combination of three words.
- ‘Progressive’ is derived from the French term’ progressif’ and is used to describe concepts of ’advancement’ or ‘going forward’ etc.
- ‘Hepato’- the term ‘hepato’ is derived from the Greek word ‘hepak’ which means’ liver’.
- ‘Lenticular’- the term ‘lenticular’ is derived from the Latin word ‘lenticularis’ which means ‘lentil shaped’.
- ‘Degeneration’- the term ‘degeneration’ is a French word which means ‘loss’ or ‘impairment’.
Wilson’s disease is so-called progressive hepatolenticular degeneration because it gradually deteriorates hepatocytes (liver cells) as well as the lenticular nucleus, which is an important structure in the basal ganglia of the brain that control emotions and motivation.
Prevalence of Wilson’s disease
A 2024 study demonstrated that there are 3 crore cases of Wilson’s disease worldwide by the beginning of new millennium. It could be asserted due to the advent of advanced and improved methods such as the widespread availability of cheaper molecular genetic diagnostic methods for the diagnosis of Wilson’s disease could increase the prevalence. Also, increased awareness of Wilson’s disease, could be argued in the development of the disease.
With a carrier frequency of 1 in every 90 individuals, this disease affects 1 in 30,000 people globally. Due to the rising number of consanguineous marriages (marriage between two blood related individuals), Wilson’s disease is more common in certain communities. Both men and women have similar effects. While the typical age range for this disorder's appearance is four to forty years old, cases have been reported in individuals as old as 70 years and children as young as 3 years old.
Prevalence of Wilson’s disease in India
There has been hypothesis that the prevalence of Wilson’s disease in India may exceed the prevalence rates seen in the West, i.e 1 in 30,000 to 1 in 100,000.
Several case series from India implies that Wilson’s disease might be more common than previously believed. P.C271X is the frequently found mutation in ATP7B gene in Indian population.
A 2021 study demonstrated that nearly 50% of cases of Wilson’s disease in India have a positive family history, and consanguinity (blood relation) is common among them. It also emphasizes that men are more prone to Wilson’s disease in the Indian population.
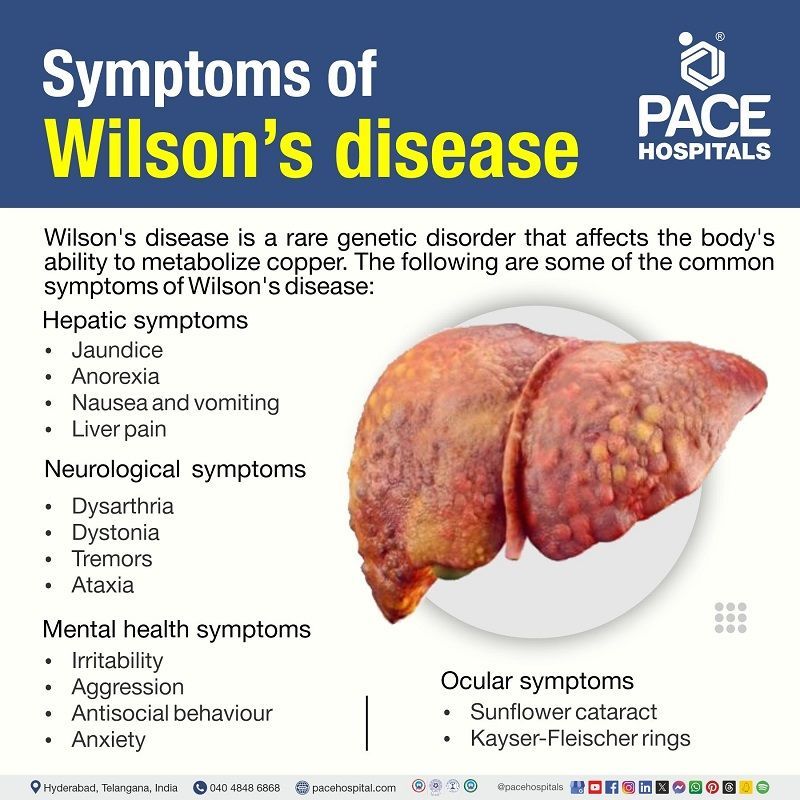
Wilson’s disease symptoms
Since Wilson’s disease is an inherited phenomenon where people usually are born with the disorder. Prior to the accumulation of copper in the liver, brain, and other organs, the symptoms of this disease may not be manifested.
In some patients, symptoms of this disease cannot be spotted unless they are diagnosed and managed. The symptoms of this disease may vary and are related to hepatic system nervous system, eyes, mental illness, and other organs.
Hepatic symptoms (symptoms related to liver)
Wilson’s disease patients may experience hepatitis-like symptoms, or inflammation of the liver. These symptoms can occasionally appear in patients experiencing acute liver failure. These symptoms could consist of:
- Jaundice (Yellowish discoloration of eyes and skin)
- Anorexia (poor appetite)
- Nausea and vomiting
- Liver pain
- Dark urine
- Pale stools (lightening of stool colour)
Only after developing problems from cirrhosis (permanent damage to liver) and chronic liver disease, some individuals with Wilson’s disease exhibit symptoms. Some of these symptoms are:
- Fatigue (feeling tired or weak)
- Weight loss without effort
- Bloating (A buildup of gas in the stomach)
- Oedema (swelling of legs)
- Itchy skin
Neurological symptoms
Neurological symptoms of Wilson’s disease are appears during the progression of the disease. The Wilson's disease neurological symptoms could include:
- Dysarthria (weakness in the muscles used for speech)
- Dystonia (unwanted muscle movements)
- Tremors (shaking usually from physical weakness, or disease)
- Choreoathetosis (unwanted movements of fingers and toes)
- Ataxia (Impaired balance or coordination)
- Cognition difficulties (difficulty in thinking, communication, understanding or memory)
Mental health symptoms
Adult Wilson’s disease sufferers frequently experience psychiatric manifestations. At initial stages of the disease 25% of patients may have psychiatric symptoms, in the later stages of the disease almost every adult patient may experience them. Symptoms may include:
- Irritability
- Aggression
- Antisocial behaviour
- Anxiety
- Depression
Ocular symptoms (symptoms related to eyes)
In addition to being essential for diagnosis, the visual symptoms are also important for tracking treatment response. The characteristic signs of Wilson's disease eyes, include:
- Sunflower cataract (clouding of lens in anterior capsule of the eye)
- Kayser-Fleischer (KF) rings (type of brown or grey coloured rings that encircle the cornea of the eye)
Other symptoms
Other body regions may be affected by Wilson’s disease, which can result in symptoms or health issues like:
- Anaemia (low levels of haemoglobin and red blood cells)
- Arthritis (joint pain)
- Cardiomyopathy (condition that affects heart muscle)
- Renal tubular acidosis (inability of kidneys to remove waste) and kidney stones
- Azure lunula (Also called blue nails or Wilson's disease nails. Characterized by a blue discoloration of the lunula)
Apart from symptomatic Wilson's disease, there is a manifestation of asymptomatic Wilson's disease which presents neither hepatic nor any of the major symptoms. Herein, an asymptomatic adult patient with Wilson's disease can be detected only through genetic analysis.
Wilson’s disease causes
Wilson’s disease pathophysiology
Wilson’s disease is brought on by one of the many mutations (change in DNA sequence of a cell) in the ATP7B gene on chromosome 13, which control the protein transporter that in charge of removing extra copper from the body and dumping it into bile.
- Copper metabolism in a healthy body: Copper is a necessary element for the bodily maintenance, mainly as a cofactor for enzymes such as cytochrome c, ceruloplasmin, oxidase, etc. Sometimes in the case of a copper overload in a healthy body, the ATP7A enzyme releases copper into the portal vein to the liver where it gets bonded to ceruloplasmin which in turn released into the bloodstream. The excess copper is secreted into bile.
- The role of ATP7B: The binding of ceruloplasmin to copper is overseen by ATP7B. In the case of patients suffering from Wilson’s Disease, due to the mutation of ATP7B, the gene remains dysfunctional. It causes copper accumulation in the liver.
- Unbounded copper: Increased copper level in the liver causes oxidative damage, resulting in various hepatic disorders and the release of unbounded copper. This unbounded copper precipitates particularly in the kidneys, brain, and eyes. Being overexposed to copper triggers the production of free radicals, which deteriorate essential proteins and fats. Early alterations due to excess copper occur in the parts of the cell such as nucleus, peroxisomes and mitochondria.
- The aftermath: The unbounded copper deposition in the brain is mainly concentrated around the basal ganglia, putamen, and globus pallidus (also called lenticular nucleus), damaging the neurocognitive processes and producing neuropsychiatric symptoms of the Wilson’s disease.
Autosomal recessive inheritance pattern
Autosomal recessive inheritance is the passage of a genetic trait or condition from parent to kid. When a child receives one copy of each parent’s mutant (changed) gene, a genetic disease might develop. The parents of a kid with an autosomal recessive disease are usually not carriers of the condition. Unaffected parents are referred to as carriers, since they each have one copy of the mutant gene and can pass it on to their children.
Wilson’s disease risk factors
A person’s risk of developing Wilson’s disease may increase if there is a family history of the disease, particularly if a first-degree relative such as a parent, sibling, or child has the illness.
Wilson’s disease affects both the genders equally.
Complications of Wilson’s disease
Wilson’s disease, if left untreated, it produces life-threatening complications such as the following. In case of severe cases, the complications may also could lead to death.
- Liver cirrhosis (permanent liver damage)
- Hepatocellular carcinoma (liver cancer)
- Kidney damage (kidneys are considered damaged when they are unable to filter blood efficiently)
- Encephalopathy (brain dysfunction)
- Variceal bleeding (bleeding from expanded blood vessels, mainly in esophagus and stomach)
- Hepatorenal syndrome (kidney damage that occur with advanced liver damage)
- Neuropsychiatric manifestations (mental disorders that occur due to brain malfunction, ex: irritability, aggression etc.)
Prevention of Wilson’s disease
Wilson’s disease cannot be prevented. To determine whether the present or future offspring are susceptible to the illness, genetic counselling may be helpful.
Wilson’s disease diagnosis
The diagnosis of Wilson’s disease is still a challenge, as there is no single test which provides an accuracy of 100%. Due to its unique transmission mode, Wilson’s disease is seen more often in siblings than in consecutive generations and was reported only in offspring.
When symptoms of Wilson’s disease are observed, or if a family member has been diagnosed with the illness, suspicion should be raised. The doctor, after seeking all the medical and family history, diagnose Wilson’s disease by physical examination, eye examination and other tests,
Physical examination
The doctor may investigate abnormal liver signs such as:
- Oedema (swelling of legs)
- Ascites (tenderness of stomach)
- Jaundice (yellowish discolouration of eyes and skin)
- Hepatomegaly or splenomegaly (enlarged liver or spleen)
- Pale skin
Eye examination
- Slit lamp examination: This test uses a special dye to detect kaiser-Fleischer rings. Kayser-Fleischer rings (a type of brown or grey coloured rings that encircle the cornea of the eye) are the unique feature of Wilson’s disease.
Blood tests
- Complete blood picture
- Liver function tests
- Ceruloplasmin (protein that carry protein into blood) test
- Total copper in blood
- 24-hour urine collection test (to evaluate the amount of copper excreted)
Wilson’s disease radiology
- Computed tomography (CT scan)
- Magnetic resonance imaging (MRI scan)
Other tests
- Liver biopsy
- Electrocardiogram (ECG)
- Genetic testing
Wilson’s disease treatment
There is no permanent cure for Wilson’s disease, nevertheless treating the disorder for lifetime improvise quality of life, life expectancy and clinical presentations related to liver and brain.
Pharmacological treatment (treatment using medicine) of Wilson’s disease
- Chelating agents
- Antioxidants
- Zinc
- Anticholinergics
- GABA antagonists
Nonpharmacological treatment of Wilson’s disease
- Getting vaccination against hepatitis A and hepatitis B
- Consuming diet rich in vitamin B6 and zinc
- Copper levels of water should be tested and consumed if water for households is coming through copper pipes.
- Foods to avoid with Wilson’s disease
Since it is impossible to accomplish copper stability through diet because every food contains some amount of copper in it, nevertheless it is immensely suggested that foods rich in copper should be consumed with in the limits. Some of the foods that are to be avoided include:
- Shellfish
- Mushroom
- Nuts
- Chocolates
- Raisins
Other treatment strategies
- Physiotherapy
- Speech therapy
- Occupational therapy
- Liver transplant
- Transjugular intrahepatic portosystemic shunt (TIPS)
Future treatments for Wilson’s disease
Studies have demonstrated quite promising results in the interventional treatment of Wilson’s disease. They include:
- Gene therapy
- Molecular therapy
- Cell therapy
FAQs - Frequently Asked Questions on Wilson’s disease
What is Wilson’s disease?
Wilson’s disease is an unusual genetic inherited condition which is passed on from parents to offsprings due to impaired copper excretion out of the body. This phenomenon cause accumulation of copper in vital organs such as brain, liver, and eyes, eventually causing noxious affects.
For a healthy body, limited amounts of copper from meals are essential. However, excess copper is poisonous.
How to treat Wilson’s disease?
Since Wilson’s disease is a progressive disorder and has a scarcity of specific therapeutic interventions, it may be life threatening if left untreated. A multidisciplinary team consisting of a pathologist, radiologist, internist, neurologist, gastroenterologist, geneticist, nurse practitioner, and dietician etc will work in tandem to manage the disease effectively.
Can Wilson’s disease be cured?
No. Wilson’s disease cannot be permanently cured. However, Wilson’s disease patient can improve life neurological expectancy and quality of life by lifelong treatment with medications and other interventional treatments.
What is the gold standard test for Wilson's disease?
Despite other diagnostic tests available for Wilson’s disease, liver biopsy remains standard test to diagnose Wilson’s disease to evaluate copper levels. A copper content of more than 250 µg/g in dry liver tissues is considered positive for Wilson’s disease.
Who are more prone to get Wilson's disease?
Individuals who have a family history of Wilson’s disease are more likely to develop the condition themselves, particularly if a parent, sibling, or child in their first degree is affected. In most cases, signs of Wilson’s illness appear in people between the ages of five and forty. Nevertheless, certain individuals have symptoms at an earlier or later age. Early signs of Wilson’s disorder may appear in persons over 70 years old as well as in newborns as early as 9 months.
Is Wilson’s disease dominant or recessive?
Wilson’s disease is an autosomal recessive disorder that involves a single gene mutation. Usually, the carriers of the mutant gene, do not apparently show any symptoms. Although autosomal-recessive disorders rarely appear in successive generations, they may develop in communities with a significantly elevated carrier frequency of Wilson’s disease.
What is Wilson’s disease life expectancy?
Studies have demonstrated that, individuals with Wilson’s disease who receive quality care have an excellent recovery. Patients who receive appropriate treatment and an early diagnosis have a life expectancy comparable to that of the general population. Furthermore, treatment improves these people's quality of life (QOL) in addition to extending their lives.
At what age Wilson's disease is usually diagnosed?
The onset of symptoms of Wilson’s disease is not age specific. However, in most cases, symptoms are usually said to appear between the ages of 5 to 35 years. A 2023 study demonstrated that this disease had been diagnosed in children as young as 3 years and older persons who aged 70 years.
Does Wilson’s disease cause eye problems?
Yes, Wilson’s disease does give rise to eye problems. The two most prevalent ocular (related to eyes) conditions found in patients with Wilson’s disease are sunflower cataracts (clouding of lens in the anterior capsule of the eye) and Kayser-Fleischer rings (type of brown or grey colored rings that encircle the cornea of the eye). Additional ocular symptoms could affect the retina (innermost, light sensitive layer of the eye) the visual systems, or the movement of the eyes.
Can Wilson’s disease affect organs other than liver, brain, and eyes?
Yes. Wilson’s disease does affect organs other than liver, brain, and eyes. Patients diagnosed with Wilson’s disease may also have manifestations (symptoms) related to cardiac (heart) system, endocrine (hormonal) system, kidneys, skin, and lipomas (non-cancerous tumor) may also present at times.
Is Wilson's disease painful?
Yes. Wilson’s disease has painful manifestations such as abdominal pain, headache, and osteoarthritis (pain in joints such as knee, hips, and spine joints etc.)
Share on
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868