Endoscopic Submucosal Dissection (ESD) - Procedure & Cost
Dept. of Gastroenterology at PACE Hospitals, is equipped with advanced Third-Space Endoscopy, The SpyGlass® Direct Visualization System and Laparoscopic surgery equipment to perform complex and supra-major precancerous and cancerous conditions of gastrointestinal (GI) tract.
Our team of the Best Medical Gastroenterologist in Hyderabad, Telangana, India; are having extensive experience in performing endoscopic Resection and third space endoscopy techniques such as peroral endoscopic myotomy (POEM), endoscopic submucosal dissection (ESD), endoscopic mucosal resection (EMR) and submucosal tunneling endoscopic resection (STER) to treat conditions of achalasia cardia, Barrett’s esophagus etc.
Request an Appointment for ESD Procedure
ESD Procedure - appointment
Endoscopic Submucosal Dissection meaning
Etymologically, endoscopic describes the process or the usage of
endoscopy
(endo – “within” and scopy – “to see” in Greek). Submucosal dissection describes the process of cutting at the level of submucosa.
What is Endoscopic Submucosal Dissection Procedure?
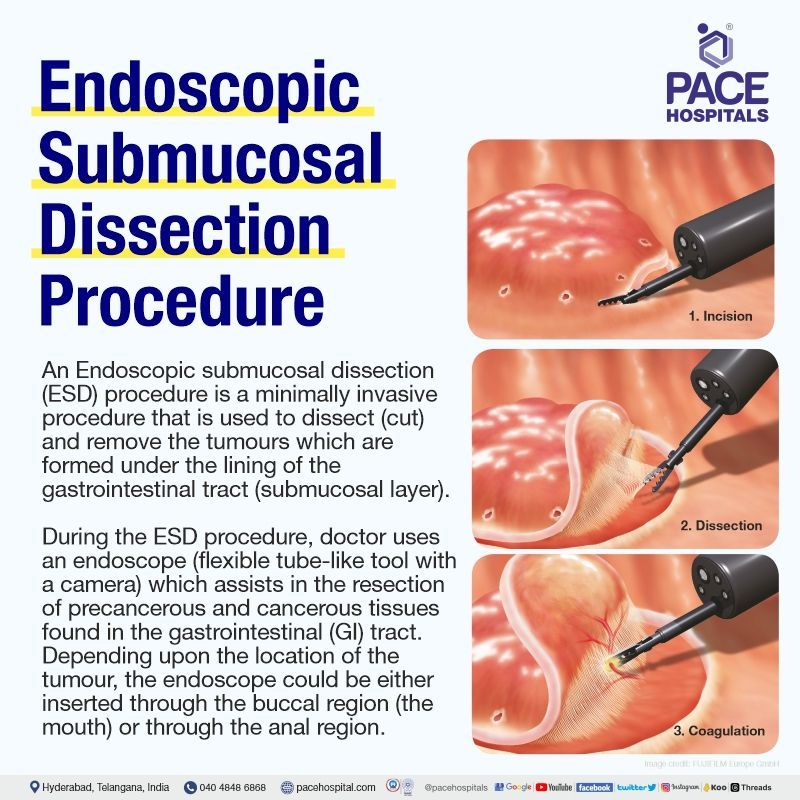
An Endoscopic submucosal dissection (ESD) procedure is a minimally invasive procedure that is used to dissect (cut) and remove the tumours which are formed under the lining of the gastrointestinal tract (submucosal layer).
During the ESD procedure, the doctor uses an endoscope (flexible tube-like tool with a camera) which assists in the resection of precancerous and cancerous tissues found in the gastrointestinal (GI) tract. Depending upon the location of the tumour, the endoscope could be either inserted through the buccal region (the mouth) or through the anal region.
It is important to note that since the complete removal of these tumours through other methods could prove difficult, ESD procedure could be a final solution as the formation of these tumours is at close quarters with the GI muscle tissue.
Due to the complexity of the procedure, accompanied by its rare occurrence, it is important for the patients to opt for a competent gastroenterologist doctors who are also skilled in interventional endoscopy, as general endoscopists may not be able to perform it.
Indications for Endoscopic Submucosal Dissection (ESD) Procedure
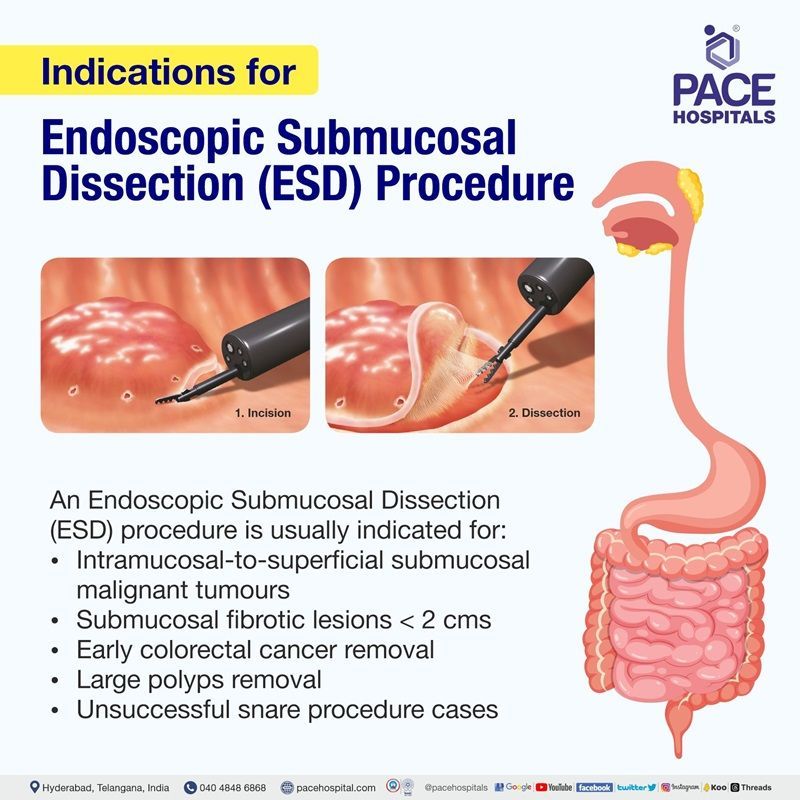
Development of endoscopic submucosal dissection (ESD) technique is specialised procedure to resect larger tumours apart from obtaining higher rates of en-bloc resection than that of endoscopic mucosal resection. Endoscopic Submucosal Dissection (ESD) procedure is generally indicated for the following:
- Malignant tumours that are diagnosed with intramucosal-to-superficial submucosal invasion.
- Submucosal fibrotic lesions (< 2 cm) that cannot be removed by endoscopic mucosal resection.
- Cases where a snare is unlikely to enable a successful en-bloc resection with endoscopic mucosal resection. Snare is a surgical tool to extract polyps/tumours.
- Removal of early colorectal cancer, large polyps and any lesions without transanal access in patients avoiding major surgical resection.
Which types of doctors can successfully execute the Endoscopic Submucosal Dissection (ESD) procedure?
Medical gastroenterologists or surgical gastroenterologists who are also skilled in interventional endoscopy are usually the first preferred choice. Nevertheless, surgical oncologists and endoscopists with experience in interventional endoscopy could also be consulted.
Need for specialised training and the learning curve
Endoscopic Submucosal Dissection (ESD) procedure is a technically demanding procedure which requires substantial training to achieve competence; inadequate training compromises both patient safety and technical outcomes.
- A research series demonstrated the effect of experience and competence of the surgeons who performed ESD procedures on porcine models (live pigs). Post-surgery, it was detected that the rate of perforation was 22%, mostly attributable to participants with less experience in ESD technique. This study suggests the significant risk the patient may undertake when the ESD procedure is performed by inadequately trained personnel.
Preparation for the Endoscopic Submucosal Dissection Procedure
Before the gastroenterologist prescribes an endoscopic submucosal dissection (ESD) technique, the patient undergoes a thorough physical and clinical examinations. The gastroenterologist understands the previous medical issues both by performing these examinations and by imploring the patients about their previous major medical problems such as diabetes, hypertension, pregnancy etc.
In addition, current medications, especially the use of antiplatelet and anticoagulation agents and the presence of any allergic history of the patient, must be provided to the gastroenterologist.
Before the Endoscopic Submucosal Dissection (ESD) procedure
The doctor examines the patient thoroughly, and only after absolute necessity endoscopic submucosal dissection technique is prescribed. Either the gastroenterologist or any personnel from the team thoroughly explains the procedure before obtaining written consent.
- The patient will be kept on fast for at least 6 hours before the examination.
- Only a low-fibre diet (i.e. no grains, nuts) is suggested for at least three days before the ESD procedure (especially if it is a colonic ESD procedure), patient should only use a low-fibre diet.
- On the day of examination, the patient is allowed to consume only clear fluid.
- The ESD team may prescribe laxatives to clean out the bowels without which ESD procedure cannot proceed.
- In case of adverse effects of laxatives (severe sweating, palpitation, vomiting, dizziness, and abdominal pain), the ESD personnel must be at once consulted.
- Any valuables, especially any metallic belongings or jewellery, must not be brought to the hospital.
- The patient must be accompanied by an adult relative or friend when leaving the hospital.
- The patient must refrain from indulging in alcohol, smoking or any drug abuse before the procedure.
During the Endoscopic Submucosal Dissection (ESD) procedure
- The patient is escorted into the endoscopy theatre.
- Depending on the patient’s condition, before the procedure, he/she may be administered intravenous sedation, which helps alleviate any anxiety and discomfort.
- To achieve numbness, local anaesthetic may be sprayed on the throat.
- A plastic mouth guard may be placed in the buccal cavity (mouth) of the patient. It facilitates the insertion of an endoscope by the doctor.
- As the patient lies on his/her left side, a flexible endoscope will be passed through the mouth down to the gastrointestinal tract for upper endoscopy or inserted through the anus up to the large bowel for lower endoscopy to perform the examination.
- The patient is under close monitoring during the procedure.
- Patients may feel bloated and/or experience abdominal distension during the procedure. It is a normal feeling.
After the Endoscopic Submucosal Dissection (ESD) procedure
- The patient should remain fasted until anaesthesia has worn off. The efficacy of local anaesthesia could vary, but usually, it could be between 1–2 hours.
- Fasting is necessary as the throat muscles could be still in a paralysis state, and any ingestion of food/beverages could result in choking.
- The patient should avoid operating heavy machinery, especially in case of intravenous sedation. Similarly, alert activities such as driving for the rest and signing legal documents must be avoided.
- For any discomfort after the procedure or any question about the examination result or the following drug treatment, the patient may consult either the gastroenterologist or anyone in their team.
- Care is taken to minimise risk during the ESD procedure, but in cases of any occult bleeding or passing large amounts of blood, severe abdominal pain, or fever, medical consultation must be at once sought.
Principle of the Endoscopic Submucosal Dissection technique
To understand the principle of endoscopic submucosal dissection technique, the division of the wall of the gastrointestinal tract must be understood. The mucosa and muscle are the principal layers existing in the wall of the gastrointestinal tract, which are attached by a loose connective tissue submucosa. It is within this submucosal tissue that gastric submucosal tumours and mesenchymal origin-stromal tumours originate.
Most people with early gastric cancer do not exhibit any noticeable symptoms. If gastric cancer screening is performed correctly, it is possible to discover the disease at an early stage. Unfortunately, people are frequently diagnosed with advanced stomach cancer because they were not checked for the disease.
Not just the discovery of the tumour but endoscopic submucosal dissection procedure also assists in removing it. Developed from an endoscopic resection (EMR) technique, the execution of ESD procedure is done in three steps:
- Injection of hypertonic saline-epinephrine (HSE) fluid into the submucosal layer to elevate the tumour.
- Pre-cutting the surrounding submucosal tissue of the tumour
- Dissecting the connective tissue of the submucosal layer beneath the tumour.
Rising the spatial altitude of gastric cancers and any other polyps by lifting them up through injecting fluid underneath them for the process of clear dissection is the prime principle of endoscopic submucosal dissection.
Contraindications of Endoscopic Submucosal Dissection technique
The Endoscopic Submucosal Dissection (ESD) procedure is not done in the following:
- If there is a lymph node or at least a suspicion of lymph node in the area of dissection.
- If biopsy of the lesion was performed. Biopsy could result in fibrosis at the site, which may tamper the results of ESD procedure (false positive). In case of biopsy, ESD procedure must also be done before the onset of fibrosis.
- The non lifting sign - the lesion fails to elevate above the surrounding mucosa even after submucosal injection underneath it. It could be due to the invasion of lesion into the submucosa.
- Coagulopathy (issues in clotting of blood). In case there is any accidental perforation or bleeding, patients suffering with coagulopathy could lose large amount of blood.
- Patients suffering from any severe cardiopulmonary comorbidities or any other contraindications which applies to standard endoscopy are also contraindicated in ESD procedure.
Considerations of a gastroenterologist to reduce the risks and complications during the Endoscopic Submucosal Dissection (ESD) procedure
Being one of the most complicated endoscopic procedures, endoscopic submucosal dissection involves incising (cutting) the mucosa (soft tissue lining the body's canals) and directly dissecting the submucosal layer after injection. It is one of the reasons for its scarcity, and therefore, it is necessary that the patients must opt for the best gastroenterologists skilled in interventional endoscopy rather than approaching mere general endoscopists.
Perforation risks
Despite being the expert, at times, interventional gastroenterologists do face difficulty in executing the task safely due to the depth of technical difficulties it could create and the risks accompanying the procedure. Although being 2-6% in previous reports, perforation is one of the most common surgical complications. Perforation is a medical term to describe the hole (aperture) that develops through the wall of a body organ.
Careful selection and dissection of submucosal fibres
Good visualisation of the submucosal tissue is necessary to reduce the risks of perforation. Countertraction is a very useful method to make good visualisation during the dissection of submucosal fibres. There are various devices and methods to achieve countertraction, such as:
- Transparent hood
- Clip with thread method
- Grasper method
- R-scope
Although these methods effectively apply countertraction to the tissue, their rarity could be attributed to their complicated process. Gastroenterologists update themselves periodically on the current scientific trends.
A novel ESD technique was developed using the intragastric lifting method with a re-opening clip device which executes safer, easier, and less time-consuming ESD compared to the previous methods. By using this method, even general endoscopists may also be able to perform a safe ESD procedure.
Maintenance of submucosal fluid cushion
Gastroenterologists undertake various measures to even minimise the already abysmal perforation rates. By creating an adequate submucosal fluid cushion (SFC) between the lesion and the muscle layer, the risk of perforation can be prevented.
While submucosal injection of normal saline can be administered to obtain the effect, it has got its limitations of being rapidly absorbed, greatly limiting the duration of the window of gastroenterologists for endoscopic submucosal dissection technique. The other methods include:
- Glycerol injection: This hypertonic solution contains 10% glycerol and 5% fructose in a normal saline solution, providing a long-lasting SFC than that of normal saline. It is also cheap and readily available.
- Hyaluronic acid: This thick viscous substance is widely found in connective tissues and has approved indications for intra-articular injections treating osteoarthritis. Studies demonstrate its superlative efficacious nature when compared to other submucosal injection solutions available. Since it is costlier, hyaluronic acid is utilised only in severe fibrosis and other organ cases (e.g., oesophagus, colorectal).
Implementation of the best electrosurgical knives
While it is necessary to use the accustomed knife, it is also important to choose devices that suit the situation of treatment. Interventional gastroenterologist prefers to utilise the knives which have improved safety, such as IT knife, Hook knife, Flex knife etc.
The mucosectome is one such electrosurgical device that has been newly developed for ESD. Since the top of this device turns freely, it greatly assists the cutting wire in facing the proper direction. A Japanese study demonstrated its efficacy with no perforations and only minor bleeding in 9.8% of patients. Mucosectome can execute safer, easier, and less time-consuming ESD compared to previous methods. By using this device, general endoscopists may also be able to carry out ESD safely.
Difference between ESD and EMR Procedure
Endoscopic Submucosal Dissection vs Endoscopic Mucosal Resection
Although both Endoscopic Submucosal Dissection (ESD) and Endoscopic Mucosal Resection (EMR) procedure are used to locate and remove any early gastric cancers, lesions and polyps found in the gastrointestinal canal, there are certain differences which signify the efficacy of ESD procedure over the EMR procedure. Few of them are:
| Parameter | Endoscopic Submucosal Dissection (ESD) | Endoscopic Mucosal Resection (EMR) |
|---|---|---|
| Definition | Injecting the submucosal layer with fluid or gel to dissect the plane and lift a lesion. Once a lesion is raised, it can be cut, reducing the perforation risk. | Resecting a lesion with a variety of techniques (suction, lift, underwater). Usually, the division plane is within the submucosa and often is not as precise. |
| The extent of submucosal cutting | Deeper division of the tissues within the submucosal layer | Superficial cutting |
| Recurrence rate | Approximately 1% | 6-10% but can be higher if lesions are removed in a piecemeal fashion |
| Size limitations | Lesions of 2-3 cm diameter, occupying less than two-thirds of the oesophageal lumen | At most, 2-3 cm diameter and less than one-third the circumference of the oesophageal lumen |
| Duration | More time consuming | Less time consuming |
| Extent of sedation | As procedure duration could be longer, often the ESD team prefers general anaesthesia | EMR can often be performed under moderate sedation |
| Post operative hospitalisation | Since ESD carries a higher risk of bleeding complications an overnight observation may be necessary | Majority of the EMR procedures can be done in ambulatory setting |
Risk of complications in Endoscopic Submucosal Dissection technique
The Endoscopic Submucosal Dissection (ESD) procedure is technically demanding, which may cause a high frequency of complications, especially perforation and post-operative bleeding (delayed bleeding). The risk factors for perforation and post-operative bleeding during and after ESD technique of gastric neoplasms are:
- The location of the tumour: It is widely accepted that the lower part of the stomach is easily approached and manipulated by endoscopy, as endoscopic haemostasis can be easily performed for bleeding located in the lower part of the stomach when compared with that in the upper part of the stomach.
- Operation time: Long operation time could risk higher chances of perforation during the ESD procedure. It could be due to: Tumour-related factors - dependent on the indication criteria for ESD procedures and Endoscopist-related factors - dependent on the experience of the personnel.
- Bacterial translocation: Bacteraemia could result from bacterial translocation of endogenous microbial flora through the injured mucosa into the bloodstream during the procedure. Also, a longer procedure time could lead to an increased risk of mucosal injuries and a high incidence of infection.
Complications of Endoscopic Submucosal Dissection technique
Endoscopic submucosal dissection technique is associated with various complications, most importantly, bleeding and perforation, amongst others.
Perforation
Most of the perforations occur during the ESD procedure, ranging from 1.2% to 5.2% for gastric endoscopic submucosal dissection. Gastric perforation is higher in both the upper and middle thirds of the stomach when compared with the lower third of the stomach. It could be due to the thinner gastric wall in the former two locations than in the latter.
Bleeding
Bleeding complications could be:
- Immediate (intraoperative) bleeding: happen during the procedure
- Delayed bleeding: occurs after the procedure.
In immediate bleeding, management plays a critical role. Since the diameter of the submucosal arteries in both the upper and middle thirds of the stomach is higher, it is common to expect a higher level of significant immediate bleeding in these parts when compared to the lower third of the stomach.
Delayed bleeding after ESD procedure could range from 0%-15.6%. It was found that delayed bleeding after the ESD procedure occurred more frequently in the lower and middle thirds of the stomach, which could be due to antral peristaltic activity and the alkaline effect of bile juice reflux. Antram is the lower part of the stomach. Peristalsis is the wavy movement generated in the gut to push the food down to the next compartment of the alimentary canal.
Other complications
The complications include:
- Stenosis - muscles in part of the stomach enlarge, narrowing the passage of the stomach into the intestine.
- Aspiration pneumonia - abnormal entry of fluids into the lower respiratory tract. It is usually seen in the ESD procedure executed in patients who are under deep sedation with no tracheal intubation.
- Air embolism (blockage of blood supply in a blood vessel due to air bubbles) and deep vein thrombosis (blood clot in a deep vein, especially in the legs.) may occur, but their numbers are insignificant.
ESD Mat Testing Procedure
In an open surgery traction can be easily applied with the use of second arm. As ESD procedure is not an open surgery, the inability of generating a traction poses a prime drawback.
To help generate the traction, various methods have been proposed and developed such as the clip-with-line method, the percutaneous traction method, the sinker-assisted method, the external forceps method, the internal-traction methods among various others.
The magnetic anchor technique (MAT) is one such method of generating traction.
Magnetic anchor guided - endoscopic submucosal dissection or the ESD MAT testing procedure demonstrated its potential benefits when compared to various other current traction methods.
This ESD MAT testing procedure does not interfere with any of the endoscopic procedures, unlike the double channel and outer-route methods. Unlike the percutaneous traction, clip-with-line, and sinker-assisted methods, the dynamic traction provided by ESD MAT testing procedure can change the direction of retraction through the movement of external magnet.
Necessity of endoscopic submucosal dissection over other endoscopies
To examine the gastrointestinal organs, an endoscopy is performed with an endoscope - a long, thin tube that contains a small camera which is inserted into the body through the mouth or anus. Usually done as an outpatient procedure, it is prescribed to the patient only after a thorough examination by the doctor who notices a pattern of symptoms.
When people think of endoscopy, they typically think of a screening examination such as a colonoscopy for cancer surveillance etc. Nevertheless, endoscopies have evolved for a variety of indications, such as gastrointestinal bleeding and gastroesophageal reflux. In the earlier days, when endoscopy was still in infancy, the endoscopists could only view the anomaly (polyps, tumours etc.) as the devices lacked the technical harness and equipment. Of late, along with diagnostic uses, interventional/therapeutic uses are also incorporated into endoscopic procedures.
Despite the advancement of various endoscopic techniques, such as:
- Strip biopsy
- Endoscopic resection with local injection of hypertonic saline-epinephrine solution (ERHSE)
- Endoscopic double snare polypectomy (EDSP)
- Cap-assisted endoscopic mucosal resection
Endoscopic submucosal dissection (ESD) always has the edge over its predecessors and contemporaries as it is:
- Not restricted by the limited resectable specimen size imposed by the calibre of a snare or cap attachment, therefore, ESD can be used for lesions larger than 2 cm in diameter that were resectable within a single specimen, no cases of incomplete resections, which could risk local recurrences/infections.
Endoscopic Submucosal Dissection (ESD) Cost in Hyderabad, India
The
cost of Endoscopic Submucosal Dissection (ESD) in Hyderabad generally ranges from ₹1,00,000 to ₹1,75,000 (approximately US $1,210 – US $2,120). The exact ESD price varies depending on factors such as the size and location of the lesion, presence of fibrosis, whether advanced knives or hybrid techniques are required, surgeon/endoscopist expertise, and the hospital facilities chosen — including cashless treatment options, TPA corporate tie-ups, and assistance with medical insurance approvals wherever applicable.
Cost Breakdown According to Type of Procedure
- Small Lesion ESD (< 2 cm) – ₹1,00,000 – ₹1,25,000 (US $1,210 – US $1,510)
- Medium Lesion ESD (2–4 cm) – ₹1,25,000 – ₹1,50,000 (US $1,510 – US $1,815)
- Large / Difficult Lesion ESD (> 4 cm) – ₹1,50,000 – ₹1,75,000 (US $1,815 – US $2,120)
FAQs on Endoscopic Submucosal Dissection (ESD) Procedure
How much does Endoscopic Submucosal Dissection cost in India?
Endoscopic submucosal dissection cost in India, range varies from ₹ 1,25,000 to ₹ 1,50,000 (Rupees one lakh twenty-five thousand to one lakh fifty thousand). However, cost of Endoscopic Submucosal Dissection (ESD) Procedure in India vary in different private hospitals in different cities.