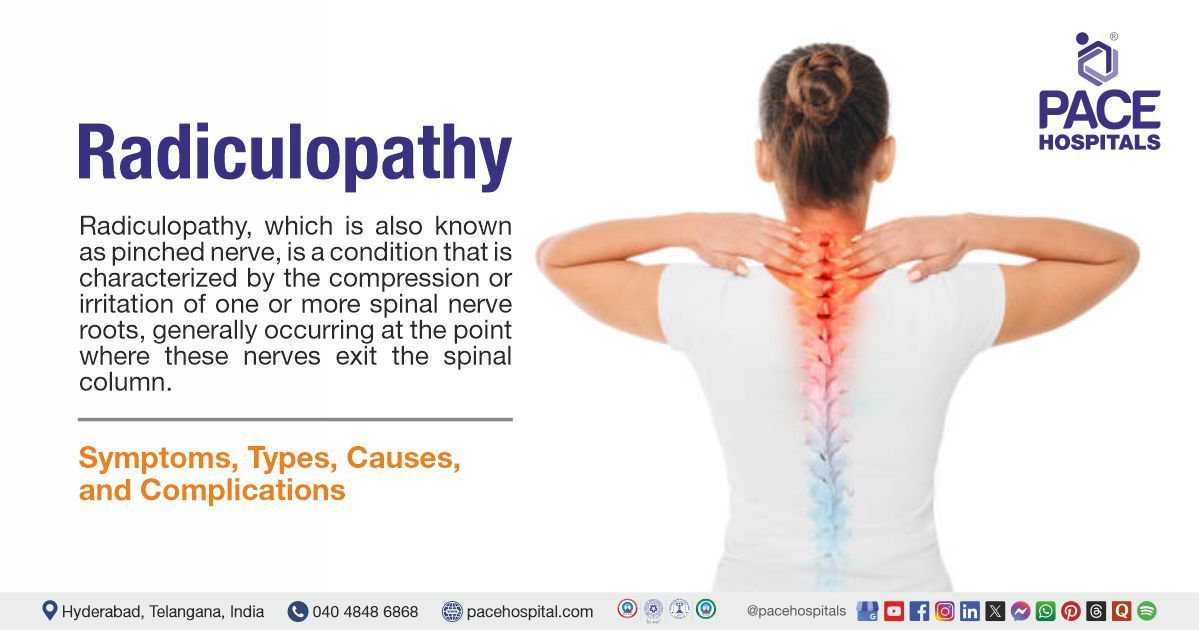
Radiculopathy – Symptoms, Causes, Types, Diagnosis, and Treatment
PACE Hospitals
Written by: Editorial Team
Medically reviewed by: Dr. U L Sandeep Varma - Consultant Brain (Neuro) and Spine Surgeon
Radiculopathy definition
Radiculopathy, which is also known as pinched nerve, is a condition which is characterized by the compression or irritation of one or more spinal nerve roots, generally occurring at the point where these nerves exit the spinal column. It can affect any individual and is the result of disc degeneration, disc herniation, or other trauma. Arthritis, herniated disc, spondylosis, and bone spurs are some of the causes of radiculopathy. It is primarily of three types: cervical radiculopathy, lumbar radiculopathy, and thoracic radiculopathy. Numbness or tingling sensation in the arms, weakness in the arms, pain in the arms, legs, or shoulders are some of the symptoms of radiculopathy. Neurosurgeons and orthopedic specialists can treat radiculopathy.
Radiculopathy meaning
The term "radiculopathy" is derived from two words
The term "radiculo" is derived from the Latin word “radix” which means "root".
The term "pathy" is derived from the Greek word “patheia” which means "suffering".
Together, it means "the suffering of the nerve root".
Radiculopathy Prevalence
Radiculopathy prevalence worldwide
The prevalence of cervical radiculopathy varies, ranging from 1.21 to 5.8 per 1,000 people. The prevalence rates for males and females have been reported as 1.14 percent and 1.31 percent respectively. Lumbar radiculopathy is more common than cervical radiculopathy, with a prevalence of 3 to 5 percent of the population.
Radiculopathy prevalence in India
A study conducted in Chennai estimated that cervical radiculopathy was diagnosed in 30 percent of the patients with neck pain, with males experiencing it more frequently than females. The prevalence of lumbar radiculopathy among adults in a rural Indian setting was estimated to be 12 percent.
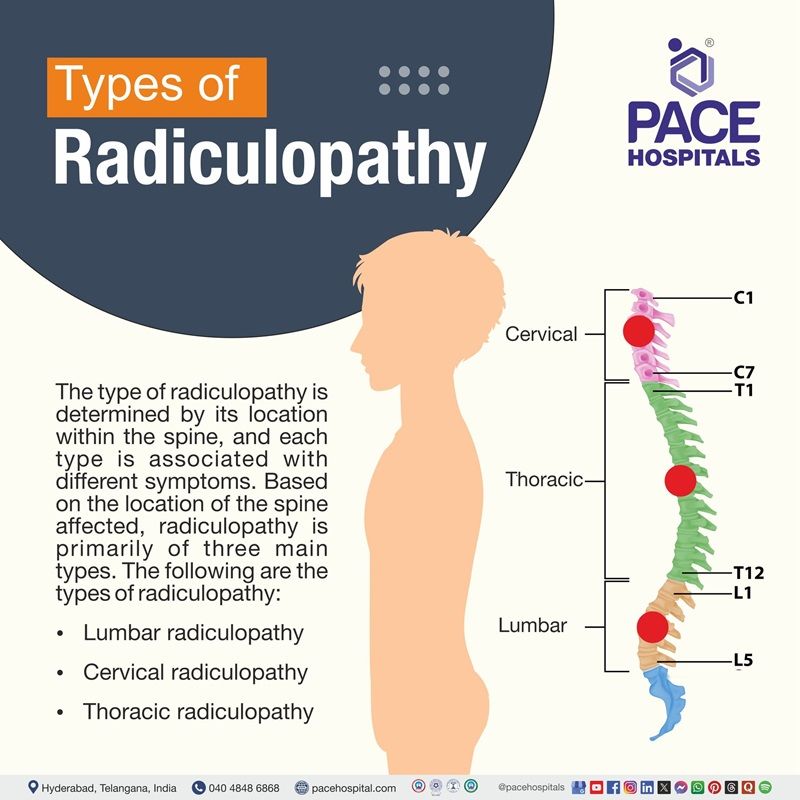
Types of Radiculopathy
The type of radiculopathy is determined by its location within the spine, and each type is associated with different symptoms. Based on the location of spine affected, radiculopathy is primarily of three main types. The following are the types of radiculopathy:
Lumbar radiculopathy
This type of radiculopathy occurs in the lower back, and it is also known as sciatica, as the nerve roots which make up the sciatic nerve are often involved. Sciatica is a type of lumbar radiculopathy which produces pain that starts in the lower back and shoots down one or both legs. In radiculopathy, the lower back is the most affected part.
Cervical radiculopathy
It describes a compressed nerve root in the neck (cervical spine). It occurs when a nerve in the neck area is compressed or irritated at the point where it leaves the spinal cord. This can result in shoulder pain, and muscle weakness and numbness which travels down the arm into the hand.
Thoracic radiculopathy
This type of radiculopathy refers to the compressed nerve root in the thoracic area of the spine, which is the upper back. This is the least common type of radiculopathy, and the symptoms follow a dermatomal (specific area of skin that receives sensory input from a single spinal nerve) distribution. It causes pain and numbness which wraps around to the front of body.
Radiculopathy Causes
There are various causes of radiculopathy, some involve spinal injury, and others are caused by the development of spinal conditions. The majority of these etiologies lead to changes in the structure of the spine, leading to loss of nerve space. A number of issues related to disc degeneration are the most common causes of radiculopathy. The following are some of the additional causes of radiculopathy:
Bone spurs
These are bony overgrowths which develop in the vertebrae. The excess bone when present in the area of spine can invade on space needed by the surrounding spinal nerves. This invasion may cause the spinal nerves to get pinched.
Osteoarthritis
This is the most common type of arthritis affecting the spine. It can weaken the joints and vertebrae, making the spine vulnerable to injuries such as compression fractures.
Spondylolisthesis
It is spinal instability, which involves slipping of a vertebral body forward and onto the vertebrae below, resulting in misalignment of the spine. It causes radiculopathy by narrowing the spinal canal and exerting pressure on the exiting nerve roots.
Spinal stenosis
It is the narrowing of the spinal column which causes pressure on the spinal cord or narrowing of neural foramina (openings in the spine) where the spinal nerves exit the spinal column.
Scoliosis
It is a condition where the spine curves abnormally, often to the sideways. This abnormal curvature puts pressure on the nerve roots, making them compressed or irritated as they exit the spinal cord.
Subluxation or misalignment
It is the misalignment or partial dislocation of the vertebrae. This misalignment causes pressure on the nerve roots as they exit the spinal column through the foramina.
Spinal tumors
Tumors can contribute to the development of radiculopathy by pressing on the spine, causing nerve irritation.
Cervical Radiculopathy Causes
Cervical radiculopathy is caused by degenerative changes which occur in the spine with increasing age. The following are the causes of cervical radiculopathy:
- Degenerative changes: With increasing age, the discs in the spine lose height and lose water content, begin to dry out, and become stiffer. This causes collapse of disc spaces and loss of disc space height and as the discs lose height, the vertebrae move closer together. As a result, in response to the collapsed disc, the body forms more bone called bone spurs. These bone spurs result in stiffening of the spine and narrow the foramen and pinch the nerve root.
- Herniated disc: When the jelly-like core (nucleus) of the disc pushes against its outer ring, the disc herniates. When this herniated disc bulges out towards the spinal canal, it exerts pressure on the sensitive nerve root, resulting in pain and weakness in the area the nerve supplies.
Lumbar radiculopathy causes
Increasing age, injury, poor posture, obesity and other issues can cause problems in the lower back. These problems can then irritate nerve roots. The following are some of the causes of lumbar radiculopathy:
- Disc damage in the lumbar spine: The disc that is damaged can exert pressure on the spine and nearby nerve roots, causing nerve compression.
- Degeneration from wear and tear, and aging: With increasing age and from wear and tear the openings in the vertebrae get narrow and these narrowed openings press on nerve roots as they leave the spinal canal.
- Unstable spine: When the vertebrae slip forward or because of the poor body posture, a pressure is exerted on the spine causing nerve compression.
Thoracic radiculopathy causes
Because of compression or irritation of the thoracic spinal nerve roots, thoracic radiculopathy may develop. The following are the causes of thoracic radiculopathy:
- Disc herniation or bulging: The bulging of the soft inner material of the thoracic intervertebral disc because of tears or weakness in the outer disc layer can cause thoracic radiculopathy. This bulging compresses or irritates the nearby thoracic spinal nerve roots as they exit the spinal canal through the intervertebral foramina.
- Degenerative spine changes: These degenerative changes through mechanical compression and irritation of the thoracic spinal nerve roots can cause thoracic radiculopathy.
- Foraminal stenosis: The narrowing of intervertebral foramina which are the openings through which spinal nerve roots exit the spinal canal causes compression and irritation of these nerve roots. This narrowing can decrease the space available for the nerves, increasing mechanical pressure, which disrupts normal nerve function and results in radicular symptoms.
- Trauma: History of fractures or injury may cause nerve root irritation or compression, thereby causing thoracic radiculopathy.
Radiculopathy Symptoms
The symptoms of radiculopathy are shaped by various factors, one of which is type. The type of radiculopathy is determined by its location within the spine, and each type is associated with different symptoms. The following are the symptoms of radiculopathy:
- Sharp pain in the back, arms, legs or shoulders which may worsen with even simple activities such as coughing or sneezing.
- Weakness or loss of reflexes in the arms or legs
- Numbness of the skin, “pins or needles” or other abnormal sensations in the arms or legs.
Cervical Radiculopathy Symptoms
The symptoms of cervical radiculopathy vary based on the severity of the condition. The common symptom of cervical radiculopathy includes:
- Neck pain
- Shoulder and back pain
- Weakness or numbness
- Reduced range of motion
In severe cases, the patient may lose dexterity of hands and tends to drop things.
Thoracic Radiculopathy Symptoms
The symptoms of thoracic radiculopathy may vary from patient to patient. The following are some of the common symptoms of thoracic radiculopathy:
- Chest pain
- Torso pain (discomfort in the abdominal region, which lies between the chest and pelvis)
- Burning nerve pain, which is felt in the rib cage, down the sides of the body, in the abdomen
- Numbness or tingling sensation in the areas affected.
Lumbar Radiculopathy Symptoms
A number of symptoms may develop when a nerve is compressed and/or irritated in the lumbar spine. Bgh67ghgut most of the symptoms will affect the lower body and worsen during or after extended periods of standing or sitting. The following are some of the symptoms of radiculopathy:
- Lower back pain
- Sciatic nerve pain
- Hip pain
- Foot pain
- Pain in the buttocks
- Numbness and weakness in the legs
- Tingling sensation in back and legs
- Reflex changes
- Bowel or bladder issues
Radiculopathy Risk Factors
Risk factor can be anything which can increase the likelihood of developing the disease. The following are some of the risk factors of radiculopathy:
- Family history: It increases the risk of radiculopathy through several mechanisms. Many studies have indicated that having a family history of disc related lower back pain increases the risk of lower back pain by four times.
- Having other spine disorders: Having a history of spine disorder can increase the risk of radiculopathy. History of herniated discs, degenerative diseases, puts pressure on the nerve roots and can lead to radiculopathy.
- Performing strenuous activities: Strenuous activities such as heavy lifting, repetitive motions can injure the spine and lead to conditions such as herniated disc or bone spurs which can directly cause radiculopathy.
- Sports: Sports which involve high loads can injure the spine and can increase the risk of radiculopathy because of repetitive strain, sudden impacts and spine misalignment.
Cervical Radiculopathy Risk Factors
The following are the risk factors of cervical radiculopathy:
- Age: With increasing age, the natural degeneration of spinal discs and bones can increase the risk of cervical radiculopathy. Though cervical radiculopathy can occur at any age, it is most commonly seen in the 50 – 54 years of age group.
- Female gender: Some factors such as muscle activity and posture can contribute to the increased risk of radiculopathy in females. In females, higher muscle activity in the neck and shoulder muscles during activities like standing or sitting without back support can increase strain, which could potentially contribute to a higher risk of cervical radiculopathy.
- White race: In white individual’s factors such as genetic predisposition, lifestyle and socioeconomic status increases the risk of developing cervical radiculopathy.
- Military involvement: In military works such as heavy lifting, repetitive motions, and spinal injuries from combat or training activities can potentially increase the risk of cervical radiculopathy.
- Heavy manual labor: Because of repetitive strain, forceful movements, and sustained postures which compress or irritate nerve roots in the neck can increase the risk of cervical radiculopathy.
- Smoking: It can increase the risk of cervical radiculopathy by mechanisms such as impairing blood flow, hindering tissue healing, and accelerating disc degeneration, which can lead to nerve root compression and pain.
- Driving: During driving, prolonged static postures, vibrations, and repetitive movements can strain the neck, compress or irritate nerve roots, ultimately leading to cervical radiculopathy.
- Previous history of cervical or lumbar radiculopathy: A previous history of cervical radiculopathy can increase the risk of recurrence due to factors such as increased spinal degeneration and previous episode of radiculopathy where the nerve root were damaged, can cause those nerves more susceptible to future injury.
Lumbar Radiculopathy Risk Factors
The following are the risk factors of lumbar radiculopathy:
- Driving occupation: Long-term driving with prolonged static postures and repetitive movements strain the spine, compress or irritate nerve roots, ultimately leading to lumbar radiculopathy.
- Lifting heavy weight: Frequent heavy lifting combined with bending exerts excessive pressure on the intervertebral discs and facet joints in the lumbar spine. This can cause disc degeneration or cause disc herniation, which compresses the adjacent nerve roots, causing radiculopathy.
- Heavy industry work: The industrial work includes repetitive lifting and carrying of loads multiple times per day. This repetitive mechanical loading can increase the risk of intervertebral disc degeneration and herniation, which ultimately causes lumbar radiculopathy.
- Smoking: It can increase the risk of lumbar radiculopathy by mechanisms such as impairing blood flow, hindering tissue healing, and accelerating disc degeneration, which can lead to nerve root compression and pain.
- Overweight: Extra weight can put extra pressure on the spine, thereby causing compression of nerve roots and causing lumbar radiculopathy.
- Sedentary lifestyle: a Lifestyle that includes prolonged sitting places can put extra pressure on the lumbar intervertebral discs, reducing their flexibility and strength over time. This can increase the likelihood of disc herniation, which compresses lumbar nerve roots, causing radiculopathy.
- Multiple pregnancies: This can increase the risk of lumbar radiculopathy through several biomechanical and physiological changes such as increased mechanical load and altered posture, disc compression and degeneration. All this can affect the lumbar spine and nerve roots, ultimately causing lumbar radiculopathy.
Thoracic Radiculopathy Risk Factors
The following are the risk factors of thoracic radiculopathy:
- Overweight: Due to obesity or increased body weight the increased mechanical stress from can cause disc deterioration resulting in disc herniation or bulging more likely to occur which then compress thoracic nerve roots.
- Sedentary lifestyle: This lifestyle can reduce the spine’s ability to maintain healthy disc hydration and nutrition. Because of dehydration and poor nutrition, it causes disc degeneration and facet joint arthritis, which ultimately cause nerve root irritation or compression in the thoracic spine.
- Muscle spasm: The spasm of back muscle causes the muscles to contract tightly and can compress or irritate the adjacent nerve roots by increasing pressure on the spinal structures, ultimately leading to thoracic radiculopathy.
- Trauma to the spine: Any injury to the spine or fracture can increase the risk of thoracic radiculopathy development.
- Bone spurs: The bony growths of Bone spurs can increase the risk of thoracic radiculopathy by narrowing the intervertebral foramina which are the openings through which thoracic spinal nerve roots exit the spinal canal.
Radiculopathy Complications
When left untreated, radiculopathy can progress to chronic pain and can lead to various other complications. These complications depend on the location of the pinched nerve and patient’s medical history. The following are some of the potential complications of radiculopathy:
- Muscle atrophy: In radiculopathy, the compression of nerve roots causes denervation of the muscles. This disrupts the neural drive, causing muscles to weaken and results in atrophy over time.
- Difficulty in walking or moving: Radiculopathy can result in difficulty in walking because of several factors related to nerve root compression or damage. When a nerve root is compressed, it causes inflammation and irritation. This inflammation results in symptoms such as pain, numbness, tingling, and weakness in the affected limbs. These symptoms impair motor function, making it difficult to walk normally.
- Severe lumbar radiculopathy: This is one of the major complications of radiculopathy, which occurs through the compression or irritation of nerve roots in the lumbar spine. This compression causes severe pain, numbness, tingling, and muscle weakness in the affected areas where the pain often radiates down the leg, following the path of the sciatic nerve, which is commonly involved in lumbar radiculopathy, particularly at the L4-5 and L5-S1 levels.
- Weight gain: Radiculopathy does not directly cause weight gain, but factors such as reduced mobility because of pain, side effects from medications and metabolic changes from chronic inflammation can cause weight gain.
- Muscle loss: In radiculopathy the compression of nerve roots disrupts nerve signals to the muscles, this disruption causes muscles to weaken and over time leads to muscle atrophy and eventually muscle loss.
- Depression: Radiculopathy overtime when left untreated can cause depression. This depression may occur from chronic pain (disrupts daily life and reduces quality of life) and disability and reduced mobility, which increases psychological distress.
- Chronic pain: Nerve compression causes inflammation and irritation of nerve roots in the spine, eventually resulting in pain which radiates along the nerve path. Chronic inflammation causes chronic pain.
- Cauda equina syndrome: This one of the major complications of radiculopathy which results when a bundle of nerve roots at the bottom of the spinal cord, which are compressed, causing neurological symptoms, such as bowel and bladder dysfunction, and lower extremity weakness.
Radiculopathy Diagnosis
The diagnosis of radiculopathy usually includes several steps to identify the condition and to determine the affected root. The following are the steps involved in the diagnosis of radiculopathy:
Initial evaluation
- Medical history
- Physical examination
Diagnostic tests
- Imaging studies
- X-ray
- Computed tomography (CT) scan
- Magnetic resonance imaging (MRI)
- Electrodiagnostic tests
- Electromyography
- Nerve conduction studies
Radiculopathy Treatment
Radiculopathy is typically managed by a multidisciplinary team that may include neurologists, neurosurgeons, orthopedic surgeons, physical therapists, and primary care physicians. The treatment of radiculopathy depends on the location affected and the cause of the underlying conditions. Generally, non-surgical treatment is preferred first. The following are the steps involved in treating radiculopathy:
Non-surgical treatment
- Medications
- Non-steroidal anti-inflammatory drugs
- Opioids
- Muscle relaxants
- Physical therapy
- Lifestyle changes
- Weight management
- Posture improvement
- Steroid injections
- Alternative therapies
Surgical treatment
- Anterior cervical diskectomy and fusion (ACDF)
- Artificial disc replacement
- Posterior cervical laminoforaminotomy
Lumbar Radiculopathy Treatment
The first line of treatment for lumbar radiculopathy is usually conservative and includes nonsteroidal anti-inflammatory drugs (NSAIDs), physical therapy, patient education, and advice to stay active. Individualized exercise and pain management are prioritized during the acute phase, and in certain situations, oral corticosteroids or antidepressants may be taken into consideration. Options like spinal manipulative therapy or epidural steroid injections may be used if symptoms continue, especially in subacute or chronic stages. Surgery, like a discectomy, is only used when conservative treatment is ineffective or there are significant neurological impairments. Unless there are warning signs or the condition does not improve with standard care, routine imaging is not advised.
Cervical Radiculopathy Treatment
The most common conservative treatment for cervical radiculopathy includes patient education, advice to stay active, manual therapy, supervised exercise, and the short-term administration of NSAIDs for extreme pain. Surgery is only advised in cases of severe or ongoing symptoms or neurological deficits; traction and exercise-manual therapy combinations are also advised. Since many patients get better without surgery, conservative treatment is typically chosen when quick pain relief or functional recovery is required.
Thoracic Radiculopathy Treatment
Conservative treatments for thoracic radiculopathy usually include physical therapy, spinal extension exercises, and analgesic drugs (such as NSAIDs). For pain relief, intercostal nerve blocks are an option, and the majority of patients report feeling better after using these non-invasive techniques. When conservative management fails or when there are progressive neurological deficits, surgery is the only option.
Why Choose PACE Hospitals?
Expert Super Specialist Doctors
Advanced Diagnostics & Treatment
Affordable & Transparent Care
24x7 Emergency & ICU Support
Radiculopathy Prevention
Radiculopathy cannot always be prevented, but there are few measures which help in reducing the risk of development of radiculopathy. The following are some of the measures which help in preventing radiculopathy:
- Staying physically active: Being physically active can help in preventing radiculopathy by strengthening the muscles which support the spine, by improving flexibility and promoting healthy posture, which can reduce nerve compression and the risk of injury.
- Maintaining body weight: Excess body weight can put extra pressure on the spine, causing herniated discs or spinal osteoarthritis, which can compress nerve roots and cause radiculopathy. Maintaining ideal body mass index (BMI) helps in reducing the strain and pressure on the spine.
- Maintaining good posture and heavy lifting techniques: By maintaining good posture and by following proper heavy lifting techniques, can reduce strain on the spine and nerves, promoting proper alignment, and minimizing the risk of nerve compression
- Smoking cessation: It can help in preventing radiculopathy by improving circulation, reducing inflammation, and enhancing the body's ability to heal, which are negatively impacted by smoking.
- Managing stress: Stress management can reduce muscle tension, promoting better posture, and encourage regular exercise, which can all mitigate the risk of nerve compression and spinal problems.
Difference between Myelopathy and Radiculopathy
Myelopathy vs Radiculopathy
Both myelopathy and radiculopathy are related to the nerve’s problems in the spine, but they differ in their location. Myelopathy involves the spinal cord itself whereas radiculopathy affects the nerve roots as they exit the spinal cord. The following are some of the parameters that differentiate between myelopathy and radiculopathy:
| Parameters | Myelopathy | Radiculopathy |
|---|---|---|
| Definition | It is an injury to the spinal cord which is caused by severe compression which may occur as a result of spinal stenosis, degeneration, auto immune disorders, disc herniation or any other trauma. | It results from compression generally on an individual nerve root, which occurs when a nerve or nerves along the spine become pinched. |
| Symptoms | Tingling, numbness, weakness, pain in the lower back, neck, arm, or leg, abnormal or increased reflexes, difficulty in walking, poor balance, loss of bowel or bladder function are some of the symptoms of myelopathy. | Pain that radiates down the arm or leg, limb weakness and decreased reflexes are some of the symptoms of radiculopathy. |
| Causes | Disc herniations, bone spurs, arthritis, spinal degeneration from aging, spinal stenosis, spinal injury, infection and inflammation are some of the causes of myelopathy. | Herniated discs, bone spurs and arthritis are some of the common causes of radiculopathy. |
| Treatment | Spinal decompression surgery, discectomy, laminectomy, spinal fusion, foraminotomy, disc replacement surgery are some of the surgical treatment options available for myelopathy. | Over-the-counter pain medications, physical therapy, discectomy, spinal fusion and disc replacement are the treatment options available. |
Lumbar radiculopathy vs Sciatica
Lumbar radiculopathy and sciatica are both closely related conditions which are often used interchangeably but have different meanings. Lumbar radiculopathy refers to the compression of nerve root or irritation in the lower back, while sciatica is the pain which travels along the sciatic nerve, a nerve that originates from the lower back and extends down the leg. The following are some of the key parameters that differentiate between lumbar radiculopathy and sciatica:
| Parameters | Lumbar radiculopathy | Sciatica |
|---|---|---|
| Definition | This type of radiculopathy occurs in the lower back, and it is also known as sciatica as the nerve roots which make up the sciatic nerve are often involved. | It is a condition which is characterized by pain within the sciatic nerve distribution or an associated lumbosacral nerve root. |
| Causes | Damage to disc in the lumbar spine, degeneration from wear and tear, and aging and unstable spine are some of the causes of lumbar radiculopathy. | Herniated discs or bulging lumbar intervertebral disc are the common causes of sciatica. |
| Symptoms | Shooting pain in the lower back, pain, numbness, or muscle weaknesss which travels into the buttocks, hip, groin, or leg are some of the symptoms. | Unilateral pain in the lumbar spine; a common characteristic is pain radiating to the ipsilateral affected extremity. Patients may also feel pain or a burning sensation with accompanying paresthesia deep in the buttocks. |
| Treatment | Treatment includes over the counter medications, steroid shots into the lower back, physical therapy and weight loss. | Treatment usually includes oral nonsteroidal anti-inflammatory drugs, NSAIDs, opioid and nonopioid analgesics, muscle relaxants, anticonvulsants. |
Frequently Asked Questions (FAQs) on Radiculopathy
Is radiculopathy curable?
Radiculopathy is treatable, but the majority of the cases of radiculopathy are managed effectively with nonsurgical treatments such as medications, physical therapy, and lifestyle modifications. Surgery may be necessary in severe cases to relieve from nerve compression. This condition may not always be considered curable, especially for degenerative causes.
What are the treatment options for radiculopathy?
The treatment of radiculopathy involves conservative methods and may progress to more invasive procedures when required. Initially conservative treatment such use of medications, use of steroid injections, physical therapy and lifestyle modifications are employed to treat radiculopathy. When conservative treatment is ineffective minimally invasive procedures such as anterior cervical diskectomy and fusion (ACDF), artificial disc replacement, and posterior cervical laminoforaminotomy are recommended.
How does weight loss help in treating radiculopathy?
Excess body weight puts extra pressure on the spine and joints, thereby causing nerve compression and leading to radiculopathy symptoms. Losing weight and maintaining body weight can help in reducing this pressure, potentially reducing pain and discomfort. Weight loss can also increase the mobility and physical activity of the patient, which helps in reducing the strain on the affected nerves.
What is the role of nerve root injections in treating radiculopathy?
These injections are composed of corticosteroids and local anesthetics. While corticosteroids reduce inflammation around the nerve root, local anesthetics provide immediate pain relief. These are generally recommended after conservative treatments or non-surgical treatment such as drug therapy and physical therapy have failed to manage pain effectively.
What are the differences between radiculopathy and neuropathy?
Radiculopathy is a condition which is characterized by the compression or irritation of one or more spinal nerve roots, generally occurring at the point where these nerves exit the spinal column. While neuropathy refers to damage or dysfunction of peripheral nerves themselves, that are nerves outside the brain and spinal cord. This damage occurs along the peripheral nerves anywhere in the body, beyond the spinal nerve roots.
How is radiculopathy diagnosed?
Diagnosis of radiculopathy involves a combination of patient history, physical examination, and diagnostic tests. The diagnostic approach begins with gathering detailed medical history to understand symptoms, prior conditions, and lifestyle factors. A physical examination assesses muscle strength, reflexes, and sensory function. Imaging studies are performed such as X-rays, computed tomography (CT) scan, or magnetic resonance imaging (MRI) to visualize nerve root compression or other structural abnormalities.
What is Lasegue’s sign in diagnosis of radiculopathy?
This test is also known as the straight leg raise (SLR) test, it is a clinical test that is used to diagnose radiculopathy, especially lumbosacral nerve root irritation caused by disc herniation. During this test the patient lies in a supine position (on their back) with the knee fully extended. Then the examiner lifts the patient's leg by flexing hip while keeping the knee straight. When the patient experiences radicular pain, the test is positive.
What is sensory testing in diagnosis of radiculopathy?
In this test simple bedside tests such as assessing touch sensitivity with monofilament, pain perception with a pinprick, and temperature sensitivity are performed. They help in identifying nerve root involvement by detecting sensory disturbances, such as increased or decreased sensitivity.
What is the role of electromyography in diagnosing radiculopathy?
This test plays an important role in the diagnosis of radiculopathy. It can evaluate the electrical activity of the skeletal muscle and nerves which control them and also helps in identification of abnormalities which may indicate nerve root involvement.
What is the role of nerve conduction study in diagnosing radiculopathy?
Despite lower utility, these tests are an important part of electrodiagnostic tests in the radiculopathy diagnosis. These tests can evaluate the strength of electrical signals and can detect abnormalities which can be useful in ruling out other conditions that might mimic radiculopathy, such as peripheral neuropathy.
What is the role of NSAIDS in treating radiculopathy?
These drugs are commonly used to manage pain and inflammation, and they act by inhibiting the cyclooxygenase (COX) enzymes that are involved in the production of prostaglandins which cause pain and inflammation.
What is the role of steroid injections in treating radiculopathy?
These injections play a significant role in treating radiculopathy, especially for treating radicular pain which is associated with spinal conditions such as herniated discs and spinal stenosis. They provide moderate short-term relief from radicular pain, particularly in the lumbar area.
What is the difference between cervical spondylosis and cervical radiculopathy?
Cervical spondylosis is a term for age-related wear and tear which affects the spinal discs and vertebrae in the neck (cervical spine) and is often described as arthritis of the neck. Neck pain, stiffness, headaches, and sometimes a grinding sensation when moving the neck are some of the symptoms of cervical spondylosis.
Whereas cervical radiculopathy describes a compressed nerve root in the neck (cervical spine). It occurs when a nerve in the neck is compressed or irritated at the point where it leaves the spinal cord.
When to consult a doctor for radiculopathy
Consult a doctor for Radiculopathy when neck, back, arm, or leg pain, along with numbness, tingling, or weakness, does not improve with rest or starts interfering with daily activities. This condition occurs when a nerve in the spine is compressed or irritated, and early treatment can assist in symptom management and the avoidance of chronic issues.
Key warning signs include:
- Persistent neck, back, or leg pain
- Numbness, tingling, or weakness radiating into arms or legs.
- Pain that worsens with specific movements or activities
- Difficulty lifting objects, walking, or performing routine tasks
- Loss of bowel control (in severe cases)
If these symptoms persist, a radiculopathy specialist or a neurologist can perform tests and recommend treatment. In urgent cases—such as sudden weakness, severe pain, or bladder/bowel issues—emergency medical care is essential.
Share on
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868