Dengue Fever - Symptoms, Causes, Diagnosis and Treatment
PACE Hospitals
People with weakened immune systems as well as those with a second or subsequent dengue infection are believed to be at greater risk for developing dengue hemorrhagic fever.
Dengue fever is a painful, debilitating mosquito-borne disease caused by any one of four closely related dengue viruses. These viruses are related to the viruses that cause West Nile infection and yellow fever.
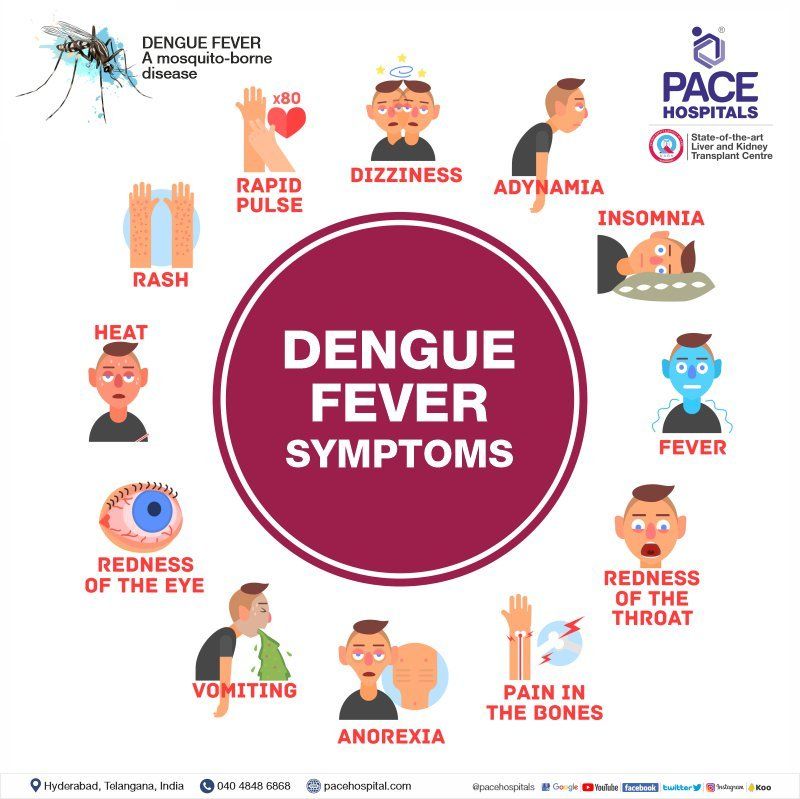
Dengue Fever Symptoms
Signs and symptoms, which usually begin four to six days after infection and last for up to 10 days, may include:
- Sudden, high fever (105 degree)
- Severe headaches
- Pain behind the eyes
- Severe joint and muscle pain
- Fatigue
- Nausea & Vomiting
- Diarrhoea
- Skin rash, which appears two to five days after the onset of fever
- Mild bleeding (such a nose bleed, bleeding gums, or easy bruising)
Sometimes, dengue fever symptoms are mild and can be mistaken for those of the flu or another viral infection. Younger children and people who have never had the infection before tend to have milder cases than older children and adults.
However, serious problems can develop. These include dengue hemorrhagic fever, a rare complication characterized by high fever, damage to lymph and blood vessels, bleeding from the nose and gums, enlargement of the liver, and failure of the circulatory system. The symptoms may progress to massive bleeding, shock, and death. This is called dengue shock syndrome (DSS).
People with weakened immune systems as well as those with a second or subsequent dengue infection are believed to be at greater risk for developing dengue haemorrhagic fever.
Causes of Dengue Fever
Dengue fever is caused by one of four dengue viruses (DENV). Transmission of these viruses to humans happens through the bites of an infected mosquito. The most common types of mosquitoes responsible for spreading dengue fever are Aedes aegypti and Aedes albopictus mosquitoes.
These mosquitoes are widely found in tropical and subtropical regions, including Southeast Asia, the western Pacific islands, Latin America, and Africa. When an infected mosquito bites a person, the virus initially enters the bloodstream, targets the liver, and then propagates to other organs. It replicates there and impairs the liver's functioning, accumulating toxins in the blood, resulting in fever, muscle pain, headache, and rash. If not managed, its severity may cause liver failure.
Dengue Hemorrhagic Fever
Dengue haemorrhagic fever is a severe and fatal condition of patent suffering from dengue fever. The patient may develop dengue hemorrhagic fever symptoms that include pain in the abdomen, persistent vomiting, change in body temperature from fever to hypothermia, irritability, confusion, and haemorrhagic manifestations. The patient might show early signs of shock, including weak pulse, restlessness, and cold clammy skin.
Abnormal haemostasis and plasma leakage are the pathological cause of the occurrence of haemorrhagic dengue fever. The plasma leakage is due to the cytokine-mediated increased vascular permeability.
Vascular permeability is defined as the ability of blood vessels to regulate the bidirectional flow of molecules and immune cells up to a particular size and to prevent the extravasation of larger molecules. In normal circumstances, molecules lesser than 40 kDa can pass through, whereas molecules such as albumin (66 kDa) and transferrin (80 kDa) retain. In case of disease conditions, such as inflammation or allergy, molecules of 2,000 kDa may extravasate, resulting in plasma leakage.
Dengue haemorrhagic fever is mainly observed in children and infants. Epidemiological studies reported, dengue haemorrhagic fever occurs, especially in children with a secondary infection with a dengue virus or infected with different serotypes from their primary (initial) dengue infection. In infants, they acquire dengue antibodies from the mother and experience dengue infection.
As per World Health Organization (WHO) criteria, the following are the criteria defined for dengue hemorrhagic fever.
- Presence of any haemorrhagic manifestation
- Thrombocytopenia (decrease in platelet count; <100,000 cells/mm3)
- Increased body temperature or recent history of fever (lasting for 2–7 days)
- Evidence of increased vascular permeability
Dengue Hemorrhagic Fever in Pregnancy
Dengue hemorrhagic fever is a serious complication of dengue fever and is more likely to be seen in pregnant women than non-pregnant. This might be due to changes in immunologic, physiologic, endocrinologic and metabolic changes during pregnancy that increase the risk of having infections.
Most pregnant women are more likely to infect in the third trimester. Placental injury and possible vertical transmission of the virus occur as a result of increased vascular permeability and endothelial leakage in dengue hemorrhagic fever. During the first trimesters, spontaneous abortion and in the third trimester, premature birth and severe and prolonged bleeding after surgical births are serious complications.
Dengue Shock Syndrome
Dengue shock syndrome is a serious complication of dengue infection that has a high death rate. Secondary infection with a different viral serotype causes severe dengue.
The exact cause of the dengue shock syndrome is still under research; however, scientists proposed the following theory:
- Dengue shock syndrome is caused by abnormal and increased host immune responses, specifically the development of cross-reactive antibodies of the dengue virus, which further exacerbates the infection.
- The cross-reactive antibodies which are formed during the primary dengue virus infection have no neutralising action.
- The dengue virus and non-neutralising antibodies produce viral-antibody complexes upon subsequent infection by a different serotype, leading to more cells being infected with the dengue virus, resulting in a severe form of dengue.
- This is known as antibody-dependent enhancement, and it is thought to have a role in the pathophysiology of shock.
- Patients suffering from severe dengue die as a result of progressively worsening shock and multiorgan failure.
7 warning signs of dengue fever
Center for disease control and prevention (CDC) has published 7 warning signs of dengue fever as per the World Health Organization guidelines 2009, as mentioned below:
- Pain in the abdomen or tenderness
- Continuous vomiting
- Ascites or pleural effusion
- Bleeding of the mucosa
- Fatigue or tiredness
- Enlargement of liver greater than 2 cm
- Increased Hematocrit values in the blood along with rapid drop in platelet count
Diagnosis of Dengue Fever
Doctors can diagnose dengue infection with a blood test to check for the virus or antibodies to it. If you become sick after travelling or living near to people those already having dengue infection, let your doctor know. This will allow your doctor to evaluate the possibility that your symptoms were caused by a dengue infection.
Doctors may suggest a combination of blood tests and imaging tests to diagnose dengue fever infection, because the body’s immune response to the virus is complex and dynamic. The dengue infection is difficult to diagnose without laboratory and radiology tests because initially symptoms may be the same as other diseases, such as malaria. Tests may include:
- Complete blood count (CBC or CBP) - to check the platelet count typical of the later stages of the illness and to detect the decrease in hematocrit, hemoglobin, and red blood cell (RBC) count (evidence of anemia) that would occur with blood loss associated with severe dengue fever.
- Dengue Serology Test (Dengue IgG & IgM) - to detect antibodies produced by the immune system when a person has been exposed to the virus; these tests are most effective when performed at least 4 days after exposure in both primary and secondary infections.
- Dengue Virus Antigen Detection (NS1) - to confirm Dengue viral infection. This test is useful to diagnose early dengue infection and can be conducted within 1-2 days following Dengue infection.
In case of severe symptoms Doctors may suggest other blood test and radiology imaging test to know the spread of dengue infection to other organs, these may include:
- Liver function tests (LFT) - to detect mild elevations in serum bilirubin, elevated transaminases and derangements in serum albumin caused by Aedes mosquito's virus hepatotoxic effects that can aslo lead to acute liver failure, with fatal outcomes.
- Renal Function Test (RFT) - to check the elevation of the serum creatinine level that may cause variety of renal diseases such as Acute renal failure, acute tubular necrosis, hemolytic uremic syndrome, hypotension, rhabdomyolysis, proteinuria, glomerulopathy, nephrotic syndrome or hemolysis.
- ECG - to check the heart electrical disturbances. In many patients ECG abnormalities observed mainly sinus bradyarrhythmias, ventricular asystole, sinus tachyarrhythmias, supraventricular tachycardia (SVT) and ST- and T-wave changes due to electrolyte abnormalities of potassium, calcium, magnesium caused by dengue infection.
- Ultrasound abdomen (USG) – to check the conditions like serositis, fluid in abdomen, edema of the gallbladder, pericholecystic fluid, ascites (buildup of fluid in spaces within your abdomen) mainly caused by dengue fever infection.
- Chest X-ray - to check the pleural effusion (the build-up of excess fluid between the layers of the pleura (the tissues that line the lungs and the chest)), pericardial effusion (the buildup of the fluid in the saclike double-layered structure around the heart called as pericardium) caused by dengue fever infection.
- D-dimer – to check D-dimer value in the blood, D-dimer is a protein fragment made when a blood clot dissolves in your body. Dengue fever infection can increase the D-dimer levels in the blood and that can result pain in body, sharp chest pain, high fever, trouble breathing and changes in skin color of your arm or leg.
- 2D echocardiography (2D Echo) - to check the damage to heart muscles. Severe dengue fever affects the heart structurally and functionally. Cardiac complications secondary to dengue virus infection vary from self-limiting arrhythmias to severe myocardial infarction, leading to hypotension, pulmonary edema, and cardiogenic shock.
- A fibrinogen test - to check fibrinogen levels, Fibrinogen is a blood protein made in liver and helps blood clotting. Low fibrinogen may make it difficult for blood to clot. In case of complicated dengue hemorrhagic fever patients have tendency of excessive bleeding, doctor may go for this test to check your fibrinogen levels.
- Fibrin degradation products blood test
- to check the FDP levels, Fibrin degradation products (FDPs) are the substances left behind when clots dissolve in the blood. Increased FDPs may be a sign of primary or secondary fibrinolysis (clot-dissolving activity) due to dengue hemorrhagic fever.
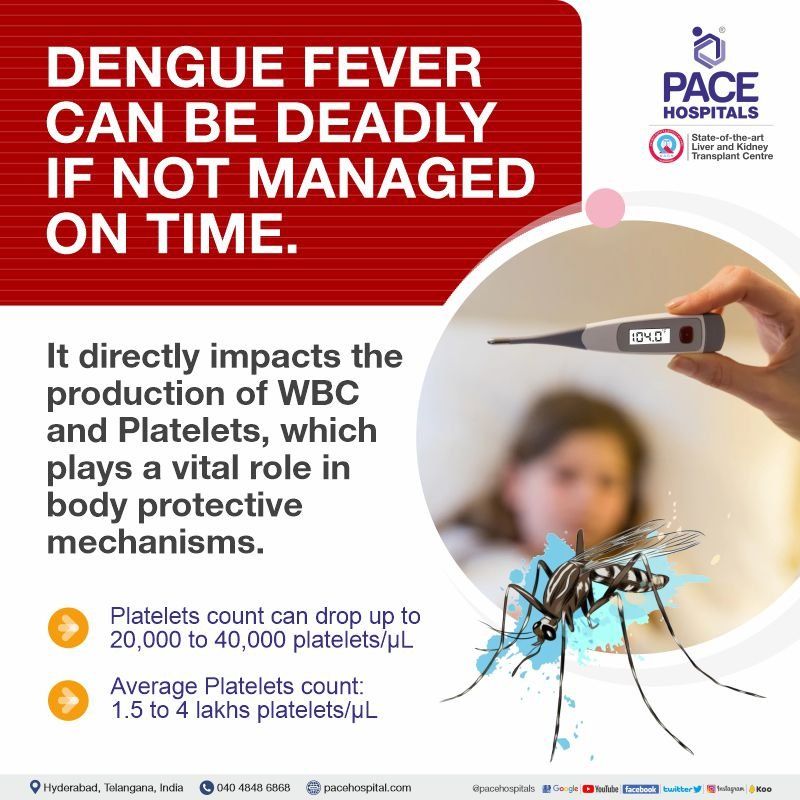
How Dengue Impact the production of White Blood Cell (WBC) & Platelets?
Dengue infection is mainly spread through the bite of a virus-infected Aedes Aegypti mosquito. The virus enters the body when the mosquito bites and begins to spread. The drop in platelets is caused by a condition called "thrombocytopenia", through direct suppression of the bone marrow or an autoimmune reaction and antibodies pushed into place. Although the dengue virus does not destroy platelets, it can trigger complications that impair platelet count and function.
Platelet loss can be recorded in many underlying conditions. A healthy person is estimated to have 1,50,000 - 4,50,000 platelets / μL. When infected with the dengue virus, platelet counts can reach minimal levels, may be less than 40,000 platelets / μL. In some cases, you can witness the decline within a day. This usually occurs at the peak of infection, during a fever of 3-4 days. Comorbidities, immunity, and age can also exacerbate platelet loss.
If necessary, regular blood transfusions can increase the platelet count. In addition to these remedies, one of the best ways to improve your platelet count is to include foods that help with recovery in your diet. Including papaya leaf extract, green leafy vegetables, fruits, iron-rich foods, foods rich in vitamin C and vitamin K, and supplements can increase and stabilize healthy platelet counts during infection.
Dengue Fever Treatment
There is no specific medicine to treat dengue infection. If you think you may have dengue fever, you should rest, drink plenty of fluids. A doctor should be seen immediately if you have symptoms such as decreased urination, dry mouth or lips, lethargy or confusion, cold or
sticky hands and feet.
Over-the-counter (OTC) medicine paracetamol can help reduce muscle pain and fever. Antiplatelet drugs should not be taken in dengue fever without doctor's advice. But if you have dengue fever, you should not take any medicines other than paracetamol without a doctor's advice to avoid the risk of complications of dengue haemorrhage fever.
If you start feeling unwell in the first 24 hours after the fever subsides, you should go to the hospital or consult doctor immediately to be checked for dengue fever complications.
Dengue Hemorrhagic Fever Treatment
There is no specific treatment available for the treatment of dengue hemorrhagic fever. In patients with hemorrhagic dengue fever, there will be a loss of electrolytes or fluids in the body. To sustain euvolemia (normal volume of blood or fluids), patients with dengue hemorrhagic fever require rigorous treatment with avoidance of overhydration (which can cause acute respiratory distress syndrome) and hypovolemia (which can cause shock). Urine production and hemoconcentration can be used to measure intravascular volume.
Why Choose PACE Hospitals?
Expert Super Specialist Doctors
Advanced Diagnostics & Treatment
Affordable & Transparent Care
24x7 Emergency & ICU Support
Dengue Fever Prevention
Preventing mosquito bites and avoiding endemic areas are the primary ways to avoid getting dengue virus.
Preventative measures
- Using bed nets during the day.
- Using window curtains sprayed with mild insecticides.
- Using creams that repel mosquitoes and contain DEET, IR3535,
- Using coils to keep mosquitoes away.
- Developing the routine of dressing in long sleeves and long pants.
Biological Control
- Fish: Using natural larvicidal fish and introducing viviparous fish species, such as Poecilia reticulata, into enclosed water bodies, like huge water tanks or open freshwater wells.
- Predatory copepods: Utilizing tiny freshwater crustaceans as efficient predators, especially in settings designed for containers.
- Endosymbiotic control: using Wolbachia-infected mosquitoes, which show a decreased vulnerability to DENV infection in comparison to Aegypti mosquitoes of the wild type
Chemical Control
- In large breeding containers, use larvicidal sprays.
- Using formulations based on oil as they prevent evaporation
- Employing pesticides, such as pyrethroids (bioresmethrin and cypermethrin) and organophosphorus compounds (fenitrothion and malathion).
Environmental measures
- Locating and removing pest and mosquito breeding grounds.
- Keeping the sunshades and rooftops in good condition.
- Properly covering water that has been stored in pots, buckets, and other containers.
Frequently Asked Questions (FAQs) on Dengue Fever
Is dengue contagious?
No, dengue is not contagious though it is caused by a viral pathogen (virus); hence it cannot be spread from one infected person to another. The primary transmission route to the human is through a bite of an infected mosquito (Aedes aegypti or Aedes albopictus). However, in certain instances, such as blood transfusions or organ transplantations from a dengue-infected person, the virus can transmit to a healthy person from an infected person.
Is itching a symptom of dengue?
Yes, itching is a symptom of dengue, and it may appear in the recovery phase that occurs after the critical phase of 24 to 48 hours, and which is attributed to the next 48 to 72 hours. During this recovery phase, patients may feel well, and their symptoms are relieved and might feel itchy.
What to eat in dengue fever?
Food rich in lean protein and low carbohydrates is preferred over high-fat, spicy and fibre-content food as it is difficult to digest.
Diet (vegetables and fruits) rich in vitamin C (oranges, papaya, green leafy vegetables, etc.), vitamin K (sprouts, broccoli, etc.), vitamin D (Salmon fish, Cod liver oil, eggs, etc.), vitamin E (wheat germ Oil, almonds, sunflower seeds), iron (beans, cereals, etc) and zinc (beans and nuts) are recommended.
Fluids play a vital role in the overall management of dengue fever, as the patient needs to stay hydrated due to loss of electrolytes.
What precautions should be taken in dengue?
In any person affected with dengue, one must take precautions in order to curb its spread. In the first week of virus infection, the dengue virus is found in the affected person’s blood. When a mosquito bites an infected person, the viral agent enters and infects the bitten mosquito; thereby, the infected mosquito can spread the virus to a healthy person through bites.
Therefore, the following are the precautions that one should take if any person or their family are affected to prevent the virus spread:
- Wearing long sleeves (shirt/pants), thereby covering the complete body
- Usage of Environmental Protection Agency (EPA)-registered insect repellents (DEET, IR3535, etc.)
- Wiping out stagnant water to prevent mosquito breeding.
- Usage of mosquito repellents
- Closing the water-filled tubs with lids
What to eat in dengue to increase platelets?
Some of the foods that can increase the platelet count during dengue fever are:
- Fruits: Citrus fruits like oranges, lemons, and grapefruits, strawberries, raspberries, kiwi, tomatoes are good sources of vitamin C, which essentially support the production of Platelets.
- Vegetables: Vegetables, including broccoli, spinach, and kale, are a high source of vitamin K that supports the production of platelets in the body. Other vegetables include Beetroot, Carrot and bell peppers.
- Nuts and seeds: Nuts & seeds are a rich source of vitamin E, antioxidants and healthy fats, which supports the production of platelets. Some beneficial nuts and seeds are walnuts, almonds, sunflowers and flax seeds.
- Whole grains: It is a rich vitamin B source, which helps increase platelet counts. Also, its fibre property helps in better digestion and absorption of nutrients. Some good whole grains include brown rice, oats and Quinoa.
- Dairy products & Protein-rich diets: They provide overall health benefits in increasing platelet counts. Some excellent dairy products and proteins are milk, yoghurt, cheese, fish, beans, and lentils.
In addition to eating these foods, staying hydrated and getting plenty of rest is essential.
What does Dengue IgM positive mean?
Dengue IgM positive: Patients with a positive IgM test result are classified as having recent dengue virus infection. Negative IgM: Patients with negative IgM results before day 8-10 of illness and absent or negative NS-1 or NAAT results are considered unconfirmed cases.
If only dengue IgG is positive that indicates patients had dengue infection in the past.
Can dengue cause death?
Severe cases of dengue fever can cause death in addition to shock and internal bleeding. Pregnant women and newborns/ infants are at high risk of developing severe dengue. Among people affected with dengue, 5% (one in 20 affected members) have a risk of severe dengue and patients affected for the second time have more chances of severe dengue.
Can you get dengue twice?
Yes, a person can get dengue fever twice, as there are four different variants of the dengue virus. When a person is infected with one variant, the patient develops antibodies against that specific viral organism. However, if any of the other three variants had bitten the same person, the antibodies produced that does show any impact, and the patient would be at high risk of severe dengue.
When will the platelet count increase in dengue fever?
In most cases, the platelet count in dengue will increase around day 7 of the illness. However, the platelet count can take up to 10 days to return to normal. Sometimes, the platelet count may not return to normal even after ten days.
It is important to note that this is just a general timeline, and the actual timing of the platelet count changes may vary from person to person, which could be based on:
- The severity of the infection
- Patient's age and overall health
- Whether the patient has had dengue before
How long does dengue fever last?
The signs of dengue fever typically last for 2–7 days. Most people will recover after about a week. However, some people may develop severe dengue, which can be life-threatening.
Dengue fever Timelines:
- Day 1-4: At the beginning of dengue fever, the initial signs manifest with fever, joint & muscle pain, headache, vomiting and rash. ·
- Day 5-7: Dengue fever breaks between 5–7 days, but other symptoms may worsen and indicate severe, life-threatening complications. ·
- Day 8-10: During these days, the symptoms start improving, and even most patients would recover completely.
Why platelets decrease in dengue fever?
There are many reasons why platelets decrease in dengue. Some of the common causes include:
- Bone marrow suppression: The direct attack of the dengue virus on the bone marrow, where Platelets are produced, can impair its productivity.
- Increased consumption of platelets: Increased risk of bleeding during dengue fever may increase the consumption of platelets, which are essentially required for blood clotting in the body.
What is the Dengue mosquito life cycle?
The dengue mosquito life cycle involves two phases: one is an aquatic phase (eggs, larvae, pupae), and the other is a terrestrial phase (adults). Female mosquitoes of Aedes aegypti and Ae. albopictus) lay their eggs on the inside walls of containers with water. The eggs hatch into larvae when water level rises, submerging the eggs. The water level could rise by any means, such as rain or people filling the water. The larvae feed on microorganisms, particulate organic matter (POM). The larvae shed their skins 3 times and develop first to fourth instars. The 4th instar larva turns into pupa. Pupae do not feed and grow to form adult mosquitos. The total life cycle lasts 8–10 days at room temperature, depending on the feeding level.
Share on
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868