Malaria Symptoms, Causes, Types, Risk Factors, Complications & Prevention
Pace Hospitals
Malaria definition
Malaria is caused by a protozoan parasite named Plasmodium, and it is spread by the Anopheles (female) mosquito that causes acute life-threatening disease. It is a major worldwide health concern where immunocompromised persons, children, and pregnant women have the highest morbidity and mortality rates.
Every year, 200 crore people, including 12.5 crore travelers, are at risk of malaria, with an annual death count of 15 to 27 lakhs. As per the World Malaria Report, a mean of 24.6 crore malaria cases with a death count of 6.22 lakhs deaths were reported in 2020 and 2021.
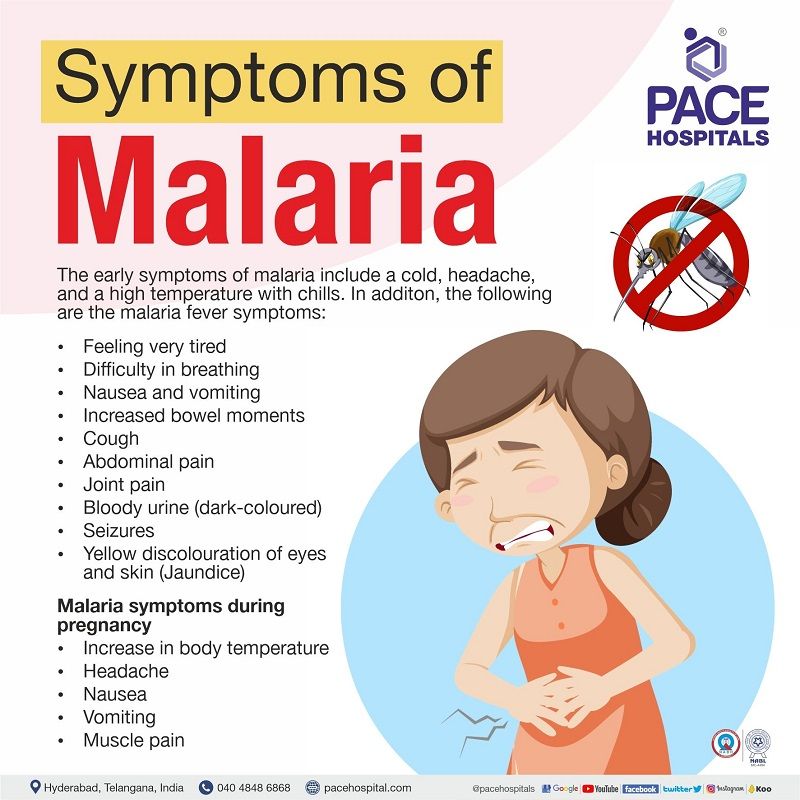
Malaria symptoms
The malaria fever symptoms usually appear within two weeks (10–14 days) from the day of infection by a Plasmodium-infected mosquito (malaria vector). The early symptoms of malaria include a cold, headache, and a high temperature with chills. Some people, especially those who have previously been infected with malaria, may experience only minor symptoms.
The following are the malaria fever symptoms:
- Feeling very tired
- Difficulty in breathing
- Nausea and vomiting
- Increased bowel moments
- Cough
- Abdominal pain
- Joint pain
- Bloody urine (dark-coloured)
- Seizures
- Yellow discolouration of eyes and skin (Jaundice)
These are some common malaria symptoms during pregnancy:
- Increase in body temperature
- Headache
- Nausea
- Vomiting
- Muscle pain
Malaria in Pregnancy
Severe malarial illness is three times more common in pregnant women in comparison to non-pregnant women, and the maternal death rate from severe malaria is close to 50%. Miscarriage, intrauterine death, early birth, poor birth weight, and neonatal death are all linked to this disease. The highest prevalence of infection seems to occur in the second trimester, indicating the necessity for antepartum care (care for healthy pregnancies) as part of efforts to prevent and treat malaria.
One of the major causes of malaria disease in pregnancy is Plasmodiumfalciparum, which is transmitted through the placenta and is a major contributor to maternal and infant deaths. Lack of antibodies to certain pregnancy-specific variant surface antigens (VAR2CSA protein), explains some of the increased vulnerability to malaria during pregnancy.
Risk factors of Malaria Disease
Living in or travelling to regions where malaria is prevalent is the highest risk of contracting the illness. The level of risk is determined by regional efforts to combat malaria, seasonal variations in malaria cases, and the precautions to avoid mosquito bites. These are some common risk factors of malaria disease:
- Staying near to old ponds and lakes
- Visiting unhygienic localities
- Mosquito prone areas
The following are at high risk of having malaria disease:
- Infants and children (less than five years)
- Pregnant women
- Nonimmune civilian and military travellers
- Disease-naive populations
- HIV or AIDS-infected patients
Types of Malaria Disease
The types of malaria fever are based on the subspecies of the malaria parasite. There are usually five types of malaria parasite, such as:
- Plasmodium falciparum (P. falciparum)
- Plasmodium vivax (P. vivax)
- Plasmodium ovale (P. ovale)
- Plasmodium malariae (P. malariae)
- Plasmodium knowlesi (P. knowlesi)
Causes of Malaria Disease
The causing agent of malaria is Plasmodium (protozoan). The malaria incubation (time taken to initiate symptoms) period varies between different subspecies of Plasmodium (P) as follows:
- P. falciparum: 8 to 11 days
- P. vivax: 8 to 17 days
- P. ovale: 10 to 17 days
- P. malariae: 18 to 40 days
- P. knowlesi: 9 to 12 days
When the causative agent of malaria (Anopheles-malaria mosquito) infects (bites) a healthy person, the Plasmodium sporozoites are transferred from the mosquito's saliva into the capillary bed of the host (the human). The incubation period can range from 7 to 30 days, depending on the type of malaria parasite. The parasite will reach the liver within hours, undergoing further cycles and replicating before being released into the host's circulatory system, starting a cascade of malarial symptoms.
- The sporozoite invades the liver cells within one hour, multiplies there, and then leaves as a merozoite to infect the rest of the body.
- This merozoite invades new healthy blood cells (erythrocytes) and infects the blood cells, forming trophozoites.
- These trophozoites in the red blood cells replicate and form schizonts that disrupt erythrocyte cell membrane integrity, which further undergo a phagocytosis process by the spleen.
- The spleen's ability to phagocytose (engulfing) infected blood cells aids in infection clearance, but also causes severe anaemia and a folic acid deficit.
Complications of Malaria Disease
Severe malaria can cause complications within hours to days from the initiation of symptoms, such as:
- Cerebral malaria
- Severe anaemia
- Decrease in blood sugar levels
- Pulmonary oedema
- Acute renal failure
Complications of Malaria in Pregnancy
Malaria complications in pregnancy include low birth weight (LBW) due to intrauterine growth restriction, premature labour, or both, which has been linked to increased infant mortality. In addition to LBW, the following are the complications of malaria:
- Maternal anaemia
- Miscarriage
- Stillbirths
- Congenital malaria
Pregnant women are particularly vulnerable to malaria's devastating effects on anaemia, which might lead to the following:
- Congestive heart failure
- Foetal death
- Maternal mortality from haemorrhage during delivery
Complications of Malaria in Pediatrics
Children with pre-existing health conditions, such as anaemia, malnutrition, and immunocompromised states, have a higher risk of death. Malaria with severe or complex symptoms includes
- Breathing problems
- Decrease in blood sugar levels
- Increase aminotransferases levels
- Severe anaemia (less than 5mg/dL)
- Increase parasitaemia (more than 5%–10% infected erythrocytes)
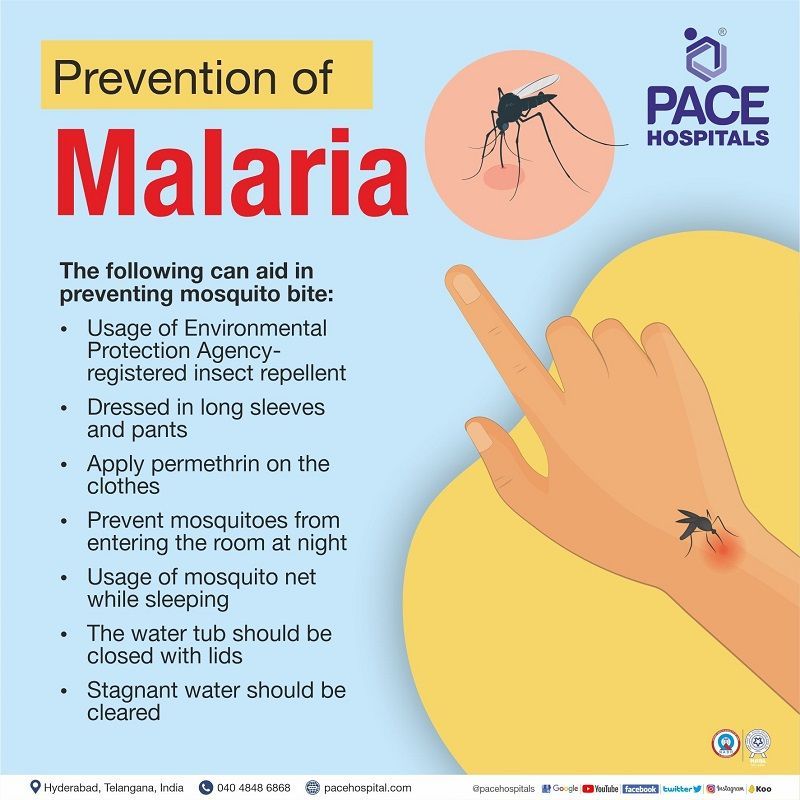
Prevention of Malaria Disease
Prevention and control of malaria disease include intake of anti-malarial medications and taking precautions to avoid being infected by mosquitoes. These are some common measures to prevent malaria disease:
- Usage of Environmental Protection Agency-registered insect repellent
- Dressed in long sleeves and pants
- Apply permethrin on the clothes
- Prevent mosquitoes from entering the room at night
- Usage of mosquito net while sleeping
- The water tub should be closed with lids
- Stagnant water should be cleared
Prevention of malaria during pregnancy
There are two main methods used to prevent malaria in pregnant women:
- Provision of insecticide-treated bed nets
- Intermittent presumptive treatment (IPT)
- After 20 weeks of pregnancy, IPT refers to the administration of two or more doses of chemoprophylaxis given to lower the subclinical malarial load
Malaria diagnosis
The general physician (GP) will examine the patient's signs and symptoms of malaria in addition to inquiring about the patient's travel history, such as:
- Recently visited places
- How far did the patient travel and return back
- Intake of any prophylactic medication (travel-related prevention)
Post that, the general physician may prescribe one of the following diagnostic tests (malaria test) to detect the presence of malaria pathogen, and it's kind. The diagnosis of malaria in pregnancy is similar to that of non-pregnant.
- Microscopy
- Rapid Diagnostic Test
- Serology
Malaria treatment
Combination therapy is used to treat both the hepatic and erythrocytic types. The treatment includes synthetic forms of quinine (aminoquinolines) and in combination with antiprotozoals (in quinine resistance patients). The treatment choice is based on Plasmodium species, pregnancy status, patient’s age, and regional anti-malarial susceptibility.
However, due to foetal teratogenicity (foetal abnormalities) and/or haemolytic reaction, few quinine derivatives are contraindicated in patients with pregnancy andGlucose-6-phosphate dehydrogenase deficiency.
Treatment of malaria in Pregnancy
- Uncomplicated malaria: In uncomplicated malaria, the obstetrician must weigh the benefits of parasite clearance over the risks to the developing foetus adverse effects from the drugs. The World Health Organization (WHO) suggests treating uncomplicated malaria in pregnancy with a combination of quinine and macrolide antibiotics.
- Severe malaria: The WHO advises quinine or antiprotozoalsto be given intravenously (IV) in the first trimester, or antiprotozoalsgiven IV in the second and third trimesters as quinine (IV) is contraindicated in second and third trimesters due to the presence of recurrent hypoglycaemia (low blood sugar) events.
Difference between Malaria disease and Yellow fever
Mosquitoes are responsible for the spread of malaria and yellow fever. In addition, the following are the differences:
| Element | Malaria | Yellow fever |
|---|---|---|
| Definition | Serious disease caused by a protozoan agent | Serious disease caused by a viral agent |
| Source organism | Caused by Plasmodium | Caused by Flavivirus |
| Vaccination | RTS, S/AS01 (only for P. falciparum) | Yellow fever vaccine |
| Vector | Female Anopheles mosquito | Aedes or Haemagogus species |
| Symptoms | Periodic fever, severe chills and heavy sweating | Fever, chills, low back pain, and Encephalopathy |
| Incubation period | 10-15 days | 3-7 days |
| Mode of transmission | Vector-borne, Blood transfusion, Organ transplantation | Vector-borne, Blood transfusion, Organ transplantation |
| Medication | Combination of synthetic forms of antimalarial and antiprotozoals | No oral medication is available, Supportive care and hydration |
Difference between Malaria disease and Viral fever
Malaria is a severe condition caused by a specific organism, whereas viral fever is caused by various viruses. Some other differences between the two are as follows:
| Element | Malaria | Viral fever |
|---|---|---|
| Definition | Serious disease caused by a protozoan agent | Common disease caused due to viral agents |
| Vector | Female Anopheles mosquito | Aedes aegypti mosquito (dengue), Dog (Rabies), etc |
| Symptoms | Periodic fever, severe chills and heavy sweating | Low-grade fever, dehydration, loss of appetite, cough, etc |
| Mode of transmission | Vector-borne, Blood transfusion, Organ transplantation | Airborne, Waterborne, Sexual transmission, Blood transfusion, Placental transfusion |
| Medication | Combination of synthetic forms of antimalarial and antiprotozoals | Antiviral agents, Antipyretics |
Difference between Malaria disease and Typhoid
Malaria and typhoid are potentially fatal diseases. Both have been linked to anaemia and gastrointestinal problems. The following are some further distinctions between the two:
| Element | Malaria | Typhoid |
|---|---|---|
| Definition | Serious disease caused by a protozoan agent | Acute systemic illness caused by gram-negative-bacterium |
| Source organism | Plasmodium | Salmonella Typhi |
| Symptoms | Periodic fever, severe chills and heavy sweating | Fever, diarrhoea, maculopapular rash, dry cough, enlargement of spleen and liver |
| Incubation period | 10-15 days | 6-30 days (7-14 days on average) |
| Types | 5 types - P. falciparum, P. vivax, P. ovale, P. malariae, P. knowlesi | 2 types - Salmonella Typhi 1, Salmonella Typhi 2 |
| Mode of transmission | Vector-borne, Blood transfusion, Organ transplantation | Orofecal route (disease-causing organisms that exist in faeces to pass from one infected person to another healthy person when they are ingested. |
| Vaccination | RTS, S/AS01 (only for P. falciparum) | Ty21a, ViCPS |
Difference between Malaria disease and Dengue
The bite of a mosquito spreads both malaria and dengue. Both of these infections are frequent in tropical and subtropical areas and are major contributors to the global burden of disease and death.
| Element | Malaria | Dengue |
|---|---|---|
| Definition | Serious disease caused by a protozoan agent | Serious disease caused by a viral agent |
| Source organism | Plasmodium | Flavivirus |
| Vector | Female Anopheles mosquito | Aedes aegypti mosquito |
| Symptoms | Periodic fever, severe chills and heavy sweating | Sudden fever, rashes, itching, low WBC count |
| Types | 5 types - P. falciparum, P. vivax, P. ovale, P. malariae, P. knowlesi | 4 types - DENV 1, DENV 2, DENV 3, DENV 4 |
| Incubation period | 10 – 15 days | 3-14 days |
| Mode of transmission | Vector-borne, Blood transfusion, Organ transplantation | Vector-borne, Blood transfusion, Organ transplantation |
| Vaccination | RTS, S/AS01 (only for P. falciparum) | CYD-TDV |
Frequently asked questions
Share on
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868